Abstract
Medical practice exposes physicians to numerous stressors, leading to high rates of psychological distress and burnout, a problem that begins during medical school. Scientific evidence suggests that promoting compassion among physicians could improve their well-being and promote patient-centered care. However, the mechanisms underlying these benefits remain unclear. This study aimed to examine the mediators and moderators of changes in psychological distress and well-being following Compassion Cultivation Training (CCT) among medical students. A randomized controlled trial with 40 medical students assigned to an 8-week CCT program or a waitlist control group was conducted. Participants were assessed at pre-intervention, post-intervention, and a 2-month follow-up on measures of psychological distress, well-being, mindfulness, compassion, emotion regulation, and burnout. Results indicated that CCT led to significant reductions in stress and anxiety immediately after the program, mediated by improvements in emotion regulation and mindfulness skills. Gender moderated changes in stress, anxiety, depression, and well-being at post-intervention, with women benefiting more than men, though these differences were not sustained at follow-up. In conclusion, this study contributes to the growing body of literature on the benefits of compassion training in healthcare and provides insights into the mechanisms through which compassion could support physicians and medical students.
Keywords: Compassion, Medical students, Distress, Well-being, Mediation, Moderation
Subject terms: Human behaviour, Medical ethics, Quality of life, Health policy
Introduction
Medical practice is subjected to physical and emotional stressors not only from witnessing the suffering of patients and their families, but also from the healthcare environment itself. These stressors include demanding workloads1, long working hours2, and increasing administrative demands3. These challenges can interfere with physicians’ personal values and convictions4.
Such stressors have been linked to higher rates of psychological distress and burnout among healthcare professionals5. Anxiety and depression are common among doctors6, and burnout is highly prevalent in the medical profession7. Alarmingly, these issues begin during medical school, where students experience high levels of anxiety and depression8, as well as higher rates of suicide and burnout compared to the general population9.
Poor mental health also leads to increased medical errors10 and suboptimal patient outcomes11. Chronic stress and burnout lead to decreased job satisfaction and diminished personal accomplishment, undermining the sense of fulfillment and purpose that physicians derive from their work12. Furthermore, this situation negatively impacts work-life balance, as exhausted and emotionally drained physicians struggle to engage with their families and communities13. Additionally, these adverse mental health outcomes lead to greater dehumanization while decreasing empathy14 and compassionate care15. As medical training progresses, students often become more frustrated and emotionally distant from patients, experience rising levels of cynicism, and become less empathetic and compassionate16. However, part of the solution lies precisely in enhancing compassion and empathy.
Compassion serves as a cornerstone of medical practice and remains a core value within healthcare organizations17. Several medical associations incorporate compassion into their codes of ethics, highlighting the significance of compassionate patient care. The significance of compassion in enhancing the overall quality of care is garnering increasing attention from various stakeholders in healthcare18. Nevertheless, evidence suggests that patients often receive insufficient compassionate care, despite its recognized importance19.
Fortunately, scientific evidence suggests that compassion can be trained. The so-called Compassion-Based Programs (CBP) have been shown to reduce psychological distress while enhancing core skills in compassionate care, such as mindfulness, common humanity or emotional regulation20,21. Although most CBP studies have focused on the general population, these programs have also shown promising results in healthcare workers22,23. Promoting compassion among physicians and medical students could potentially improve both their psychological well-being and their ability to provide patient-centered care. Self-compassion fosters resilience by encouraging a balanced perspective on negative experiences, reducing the effects of self-criticism, and promoting emotional regulation, which in turn enhances overall mental health and well-being24. Additionally, self-compassion is a key mechanism of change across diverse outcomes (e.g., stress, depression, anxiety, burnout, and well-being) and populations (e.g., students, professionals, patients, etc.)25. In a recent study, CBP showed significant improvements in compassion skills while reducing psychological distress in undergraduate medical students26. Specifically, the study found significant improvements in self-compassion, mindfulness, and emotion regulation, along with a significant decrease in stress, anxiety, and burnout. A systematic review of educational interventions and their impact on empathy and compassion among undergraduate medical students, highlighted the importance of sustainable programs, rather than single training activities, in cultivating compassion among undergraduate medical students16.
Although the benefits of compassion on psychological distress and well-being in physicians and medical students have been previously documented, the mechanisms of change underlying these benefits remain insufficiently elucidated20,27, and we still do not know how compassion heals physicians. Compassion programs seem to target a set of transdiagnostic mechanisms common to different psychopathologies, such as attentional control, emotional regulation, common-humanity, kindness, or empathy28,29. Furthermore, a recent systematic review identified gender, emotion regulation, quality of life, and burnout as significant predictor of physician compassion30. Similarly, self-compassion, resilience and optimism significantly influence the decrease in depression and perceived stress among nursing and medical students31.
For all the above, the general aim of the study is to examine the mediators and moderators of change of Compassion Cultivation Training (CCT) in a sample of medical students. Based on previous studies29–31, we hypothesized that changes in psychological distress (i.e., stress, anxiety, and depression) and well-being in medical students, both after the CCT and at 2-month follow-up, would be mediated by changes in mindfulness, compassion, emotion regulation, and burnout-related variables. Finally, we also explored baseline potential moderators of change, including demographics (i.e., age, gender, education, marital status, and nationality) and meditation experience (i.e., prior meditation experience yes/no; currently meditation yes/no; and months of previous meditation experience).
Methods
Study design
The present study analyzes the mechanisms of change from a previously published pilot Randomized Controlled Trial (RCT) that examined the effects of an online Compassion Cultivation Training on psychological outcomes in a sample of medical students. The study design has been fully described elsewhere26, in compliance with CONSORT guidelines. Participants were randomly assigned to either the Compassion Cultivation Training (CCT) group or a Waitlist (WL) control group. Those in the CCT group were evaluated at three points: before the intervention, after the intervention, and at a 2-month follow-up. The WL group underwent assessments at corresponding times: pre-waitlist, post-waitlist, and follow-up waitlist, after which they received the CCT program. Participation was voluntary, with written informed consent obtained from all legal-age participants. All methods were carried out in accordance with relevant guidelines and regulations. The study protocol was pre-registered at ClinicalTrials.gov (ID: NCT04690452), and approved by the CEIm Hospital Clínico San Carlos ethics committee (associated hospital of the Complutense University of Madrid) prior to participant recruitment (Ref. 20/742-EC_X).
Participants
Sample size was determined for the original study using G *Power software v. 3.1 (https://www.psychologie.hhu.de/arbeitsgruppen/allgemeine-psychologie-und-arbeitspsychologie/gpower), with a final sample of 40 participants: 18 participants in CCT experimental group, and 22 in WL. Eligibility criteria included being a medical student enrolled at the university, providing written informed consent, having access to the internet for CCT sessions and assessments, and committing to attend the program. Exclusion criteria were a diagnosis of a severe mental disorder in an active phase (e.g., schizophrenia, bipolar disorder), being under the influence of alcohol or substances during sessions (as determined by the CCT instructor), withdrawing before starting the intervention, or participating in another meditation program during the study.
Participants had a mean age of 23.4 (SD = 5.59), 92.5% were women, and 60% were single. The 35% had prior meditation experience, 27.5% currently practice meditation, with a mean of 8 months of prior meditation experience (SD = 18.69). No significant differences between CCT and WL were found in age (t(38) = − 0.27, p = .79), gender (χ2(1) = 0.18, p = .67), nationality (χ2(1) = 0.18, p = .67), marital status (χ2(1) = 1.36, p = .24), or prior meditation experience (χ2(1) = 0.04, p = .84).
Procedure and program description
Compassion Cultivation Training is an 8-week secular meditation program designed to cultivate compassion and empathy towards oneself and others, aiming to reduce psychological distress and enhance well-being. It was developed at Stanford University’s Center for Compassion and Altruism Research and Education, integrating insights from psychology, neuroscience, and contemplative practice. Table 1 shows the contents of the CCT program, which was taught by a certified instructor. The program consists of weekly 2-hour online group sessions featuring instruction, discussions, practical exercises, and guided meditations. Participants also engaged in 30 min of daily home practice using pre-recorded audio files and a workbook for daily practice.
Table 1.
Compassion cultivation training protocol.
| Session | Contents |
|---|---|
| 1 - Settling and focusing the mind | Introduction to breath-focused meditation to calm and focus the mind, forming the foundation for subsequent practices. |
| 2 - Loving-kindness and compassion for a loved one | Recognizing and feeling love and compassion through meditation and practical exercises, focusing on warmth, tenderness, and concern. |
| 3 - Compassion for oneself | Developing self-acceptance, non-judgment, and caring in self-relations, forming the basis for compassion towards others. |
| 4 - Loving-kindness for oneself | Fostering warmth, appreciation, joy, and gratitude towards oneself, complementing self-acceptance with self-appreciation. |
| 5 - Common humanity and appreciation of others | Building compassion for others by recognizing shared humanity and the interconnectedness of all people. |
| 6 - Cultivating compassion for others | Extending compassion progressively from loved ones to neutral individuals, difficult persons, and all beings. |
| 7 - Active compassion practice | Engaging in “tonglen” practice, visualizing taking away others’ suffering and giving them beneficial qualities. |
| 8 - Integrated practice | Combining core elements from all six steps into a daily integrated compassion meditation practice. |
Participants were invited to join the study through the university’s official website. Eligible individuals were informed about the study and provided written informed consent. They completed online assessments before the program (pre-intervention), after the program (post-intervention), and at two-month follow-up. Randomization was performed after the baseline assessment to preserve adequate allocation concealment. Participants received course credits and a book as a reward for their participation.
Measures
The online assessment comprised a set of scales evaluating domains related to compassion practice, including:
Psychological distress
Measured using the Depression Anxiety Stress Scale (DASS-2132,33, a 21-item scale assessing depression, anxiety, and stress. Each item is rated on a three-point Likert scale (0 = “not applicable” to 3 = “very applicable”). Higher scores indicate greater symptom severity. In this study, the DASS-21 total score had a Cronbach’s α of 0.85.
Psychological well-being
Evaluated using the Pemberton Happiness Index (PHI34, an 11-item scale measuring remembered well-being. Each item is rated on a ten-point scale (1 = “totally disagree” to 10 = “totally agree”), with higher scores indicating greater well-being. The PHI had a Cronbach’s α of 0.95 in this study.
Self-compassion
Measured using the Self-Compassion Scale-Short Form (SCS35,36, a 12-item self-report scale that includes three factors: self-kindness, common humanity, and mindful self-compassion. Each item is rated on a five-point scale (1 = “almost never” to 5 = “almost always”), with higher scores indicating greater self-compassion. The SCS had a Cronbach’s α of 0.90 in this study.
Compassion to others
Assessed using the Compassion Scale Pommier (CSP37, a 24-item self-report scale rated on a five-point Likert scale (1 = “almost never” to 5 = “almost always”). This study used the total score, with higher scores indicating greater compassion towards others. The CSP had a Cronbach’s α of 0.83 in this study.
Empathy
Measured using the Interpersonal Reactivity Index (IRI38,39, a 28-item self-report scale for assessing empathy towards others. This study only used the Empathic Concern subscale. Each item is rated on a five-point Likert scale (1 = “It doesn’t describe me well” to 5 = “It describes me well”), with higher scores indicating higher empathy levels. The IRI had a Cronbach’s α of 0.76 in this study.
Mindfulness
Assessed using the Five Facet Mindfulness Questionnaire – Short Form (FFMQ40,41, a 20-item self-report scale that evaluates five mindfulness facets: observing, describing, acting with awareness, non-judgment of inner experience, and non-reactivity to inner experience. Each item is rated on a five-point Likert scale (1 = “almost never” to 5 = “almost always”), with higher scores indicating greater mindfulness. The FFMQ total score had a Cronbach’s α of 0.83 in this study.
Emotion regulation
Measured using the Difficulties in Emotion Regulation Scale (DERS42,43, a 28-item self-report scale assessing five types of emotion regulation difficulties: emotional inattention, emotional confusion, emotional rejection, emotional life interference, and emotional lack of control. Items are rated on a five-point Likert scale (1 = “almost never” to 5 = “almost always”), with higher scores indicating greater difficulties in emotion regulation. The DERS had a Cronbach’s α of 0.95 in this study.
Academic burnout
Evaluated using the Maslach Burnout Inventory-Student Survey (MBI44, a 15-item self-report scale assessing three factors: emotional exhaustion, cynicism, and academic effectiveness. Items are scored on a seven-point frequency scale (0 = never to 6 = every day), with higher scores indicating higher levels of burnout. The MBI had a Cronbach’s α of 0.75 in this study.
Resilience
Measured using the Brief Resilience Scale (BRS45,46, a 5-item self-report measure rated on a scale from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicate greater resilience. The BRS had a Cronbach’s α of 0.86 in this study.
Data analysis plan
Following CONSORT guidelines47, Intention-To-Treat analyses were conducted using Maximum Likelihood estimation. A total of 6.1% of construct-level missing data were found. Little’s MCAR test showed that missing data were completely at random (MCAR; χ2(632) = 225.26, p = .99).
Mediation and moderation analyses were carried out. Mediators are variables that help explain how or why a particular effect occurs. In our study, mediators are the mechanisms (such as self-compassion or mindfulness skills) through which CCT leads to changes in outcomes (psychological distress and well-being). Moderators, on the other hand, are variables that influence the strength or direction of the relationship between the CCT and the outcomes. For example, a moderator might determine whether the effect of CCT is stronger for one group of people (e.g., women) compared to another group (e.g., men). Understanding both mediators and moderators helps clarify not only if CCT works, but also how and for whom it works best.
Multiple mediation analyses (i.e., more than one mediator simultaneously) were performed to examine whether the changes in psychological distress (i.e., stress, anxiety, and depression) and well-being in medical students, both after the CCT and at the 2-month follow-up, were mediated by changes in mindfulness, compassion, emotion regulation, and burnout-related variables. Following similar studies in the field48, mediations were carried out using simple change scores, introducing pre-intervention outcomes and mediator scores as covariates in the models to minimize variance in the outcomes49. We computed mediation models to examine whether changes in the mechanisms along the intervention (t1-t0 mediators) predicted changes in psychological distress and wellbeing after the intervention (t1-t0 outcomes: post-intervention mediators of change), and the maintenance of these changes at follow-up (t2-t0 outcomes: follow-up mediators of change).
The group was used as the predictor “X” (i.e., WL [0] and CCT [1]), psychological distress and well-being as the outcomes “Y” (i.e., stress, anxiety, depression, and well-being), and changes in mechanisms as the mediators “M” (i.e., mindfulness, compassion, emotion regulation, and burnout-related variables). Specifically, four multiple mediation models were carried out, one for each family of mediators: mindfulness-related variables (i.e., observing, describing, acting with awareness, non-judging, and non-reactivity), compassion-related variables (i.e., self-kindness, common humanity, mindful self-compassion, compassion to others, and empathic concern), emotion regulation variables (i.e., emotional inattention, confusion, rejection, interference, and lack of control), and burnout-related variables (i.e., exhaustion, cynicism, academic effectiveness, and resilience). Unstandardized regression coefficients (b) were computed for the different paths in the mediation models: path a (prediction X on M), path b (prediction of M on Y), path c (total prediction of X on Y), and path c’ (direct prediction of X on Y controlling M). The indirect effects of X on Y through M were computed as the path a and path b product (ab). Bias-corrected 95% Confidence Intervals (CI) were computed for indirect effects using bootstrap calculation (5,000 samples), as well as R2 effect size for significant models.
Finally, moderation analyses were carried out to examine whether the relationship between the intervention (X: WL vs. CCT) and psychological distress and well-being outcomes (Y) were moderated by different baseline variables (W), including demographics (i.e., age, gender, marital status, and nationality) and meditation experience (i.e., prior meditation experience yes/no; currently practicing meditation yes/no; and months of previous meditation experience). Pre-intervention scores were used as covariates in the models. Simple slopes were tested to probe the interactions using the Johnson-Neyman output with ± 1 Standard Deviation (SD), and continuous variables were mean-centered for construction of products. Bias-corrected 95% Confidence Intervals (CI) were computed for indirect effects using bootstrap calculation (5,000 samples) and R2 change was used as effect size in significant interactions.
Mediations and moderations were computed following Hayes´ (2018) technical recommendations using the PROCESS macro v. 3.4 (https://www.processmacro.org/index.html) at SPSS v. 25 software (https://www.ibm.com/es-es/products/spss-statistics).
Results
Post-intervention mediators of change
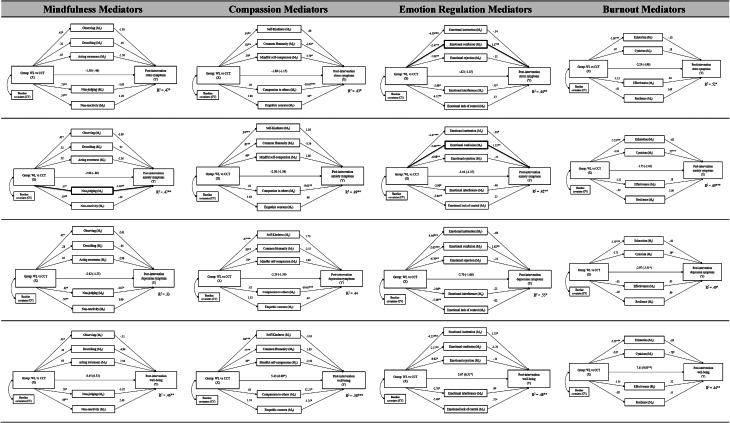
Table 2 presents the descriptive statistics for both groups across the different time points for all the measures used. Multiple mediation models of post-intervention changes in psychological distress and well-being are shown in Table 3.
Table 2.
Descriptive statistics (Mean [M] and Standard Deviation [SD]) for both groups (i.e., Compassion Cultivation training [CCT] group or a Waitlist control group [WL]) across the different time points (i.e., pre-intervention, post-intervention, and follow-up) for all the measures used in the study.
| CCT | WL | |||||
|---|---|---|---|---|---|---|
| Measure | Pre | Post | Follow | Pre | Post | Follow |
| DASS-Stress | 8.83 (3.31) | 6.24 (2.94) | 7.85 (2.97) | 7.45 (2.84) | 7.38 (4.24) | 7.93 (3.29) |
| DASS-Anxiety | 5.33 (4.35) | 3.51 (4.33) | 3.06 (2.92) | 3.95 (3.27) | 4.82 (4.31) | 4.93 (3.94) |
| DASS-Depression | 4.72 (3.44) | 3.32 (4.51) | 3.28 (3.18) | 4.59 (4.36) | 5.40 (5.97) | 4.35 (4.16) |
| PHI-Well-Being | 79.39 (19.06) | 87.64 (13.17) | 86.91 (13.74) | 75.14 (21.3) | 77.84 (19.59) | 79.22 (18.17) |
| FFMQ-Observing | 3.76 (0.70) | 4.19 (0.76) | 4.32 (0.82) | 3.19 (0.66) | 3.17 (0.84) | 3.23 (0.75) |
| FFMQ-Describing | 3.40 (0.81) | 3.66 (0.70) | 3.93 (1.31) | 3.31 (1.03) | 3.22 (0.98) | 3.39 (0.96) |
| FFMQ-Acting Awareness | 2.81 (1.11) | 3.18 (0.86) | 3.27 (0.99) | 2.88 (0.80) | 2.96 (0.80) | 2.81 (1.00) |
| FFMQ-Non-judging | 3.01 (0.93) | 3.79 (0.96) | 3.54 (0.68) | 3.11 (1.09) | 3.08 (0.94) | 3.22 (1.01) |
| FFMQ-Non-reactivity | 2.83 (0.70) | 3.41 (0.65) | 3.29 (0.68) | 3.01 (0.75) | 2.90 (0.68) | 3.07 (0.80) |
| SCS-Self-kindness | 2.89 (1.05) | 3.63 (0.83) | 3.61 (0.90) | 2.88 (0.93) | 2.81 (1.00) | 2.83 (1.06) |
| SCS-Common Humanity | 2.81 (0.86) | 3.63 (0.96) | 3.44 (0.77) | 2.82 (0.94) | 2.90 (0.93) | 3.06 (0.83) |
| SCS-Mindful self-compassion | 2.71 (0.94) | 3.28 (1.04) | 2.96 (1.00) | 2.93 (1.01) | 2.93 (1.00) | 2.86 (0.89) |
| CS-Compassion to others | 4.35 (0.39) | 4.32 (0.45) | 4.34 (0.43) | 4.33 (0.37) | 4.26 (0.41) | 4.26 (0.52) |
| IRI-Empathic concern | 29.06 (4.11) | 30.80 (3.62) | 30.34 (3.50) | 29.32 (3.11) | 29.04 (3.08) | 28.60 (3.58) |
| DERS- Inattention | 8.72 (3.48) | 6.56 (4.11) | 7.36 (3.34) | 8.68 (3.83) | 10.41 (3.90) | 10.17 (3.64) |
| DERS- Confusion | 9.33 (3.82) | 6.66 (1.89) | 7.32 (2.87) | 8.27 (2.80) | 9.14 (2.60) | 8.53 (2.82) |
| DERS- Rejection | 21.33 (8.85) | 13.20 (10.28) | 16.07 (7.55) | 20.59 (9.12) | 19.35 (8.85) | 19.33 (7.52) |
| DERS- Interference | 13.83 (4.00) | 10.42 (4.61) | 13.27 (4.03) | 13.68 (5.33) | 13.06 (4.50) | 13.29 (4.74) |
| DERS- Lack of Control | 22.72 (9.65) | 15.80 (6.23) | 17.59 (8.14) | 20.14 (9.76) | 20.44 (9.11) | 20.43 (7.00) |
| MBI-Exhaustion | 24.11 (5.87) | 24.12 (5.39) | 24.67 (6.04) | 23.95 (7.75) | 25.24 (7.20) | 24.60 (6.65) |
| MBI-Cynicism | 7.83 (7.53) | 7.58 (10.01) | 6.25 (7.05) | 4.00 (4.71) | 5.25 (6.43) | 4.84 (5.40) |
| MBI-Effectiveness | 20.33 (6.17) | 15.54 (5.67) | 15.44 (4.59) | 18.64 (7.10) | 19.39 (6.20) | 17.81 (5.23) |
| BRS-Resilience | 3.05 (0.74) | 3.15 (0.67) | 3.50 (1.11) | 3.01 (0.94) | 3.10 (0.84) | 3.15 (0.95) |
Table 3.
Post-intervention multiple mediation models of stress (1st row), anxiety (2nd row), depression (3rd row), and well-being (4th raw). The paths show the unstandardized regression coefficients, and the path c is provided in brackets. Significant indirect effects are shown in bold. Note: * p < .05; ** p < .01; and *** p < .001.
First, in the case of stress symptoms, the a-path was significant for some mindfulness facets (i.e., where the CCT predicted improvements in observing, non-judging, and non-reactivity), for self-compassion variables (i.e., where the CCT predicted improvements in self-kindness, common humanity, and mindful self-compassion), for all emotion regulation mediators (i.e., where the CCT predicted reductions in all the emotion regulation difficulties), and for emotional exhaustion in academic life. The b-path was significant for some compassion variables (i.e., common humanity, mindful self-compassion, and compassion to others), as well as for some emotion regulation variables (i.e., emotional confusion and interference), suggesting that improvements in these mediators predicted reductions in stress symptoms. However, the only significant indirect effect was found for emotional confusion (ab = -2.88; S.E. = 1.53; 95% CI [-5.99, − .14]): the CCT predicted significant reductions in emotional confusion, which in turn significantly predicted reductions in stress symptoms. The direct and total effects (c’-path and c-path) were nonsignificant for all the models, suggesting that the effect of CCT on stress symptoms was entirely mediated by changes in emotional confusion. This model explained 44% of the variance in stress reduction after the program.
Second, in the case of anxiety symptoms, the a-path showed a similar pattern to stress symptoms. The b-path was significant for non-judging of inner experience, compassion to others, a couple of emotion regulation difficulties (i.e., emotional inattention and confusion), and cynicism towards their academic life. However, the only significant indirect effects were found for non-judging of inner experience (ab = 2.54; S.E. = 1.82; 95% CI [.09, 6.62]) and emotional confusion (ab = -3.50; S.E. = 1.89; 95% CI [-7.42, − .18]): improvements in non-judging of inner experience and emotional confusion after the CCT predicted reductions in anxiety symptoms. The direct and total effects (c’-path and c-path) were nonsignificant for all the models, suggesting that the effects of CCT on anxiety symptoms were entirely mediated by changes in non-judging of inner experience and emotional confusion. These models explained 47% and 42% (respectively) of the variance in anxiety changes after the program.
Third, in the case of depression symptoms, the a-path showed a similar pattern to stress and anxiety symptoms. However, the b-path was only significant for describing one’s experiences with words. Furthermore, none of the indirect effects were significant (p > .05), suggesting that not significant mediators for depression were identified. The direct and total effects (c’-path and c-path) were nonsignificant for all the models.
Finally, in the case of psychological well-being, the a-path showed a similar pattern to psychological distress variables. However, the b-path was significant only for the ability to describe one’s experiences with words and for self-kindness. Furthermore, none of the indirect effects were significant (p > .05), suggesting that not significant mediators for well-being were identified. The total effects (c-path) were significant for compassion, emotion regulation, and burnout models.
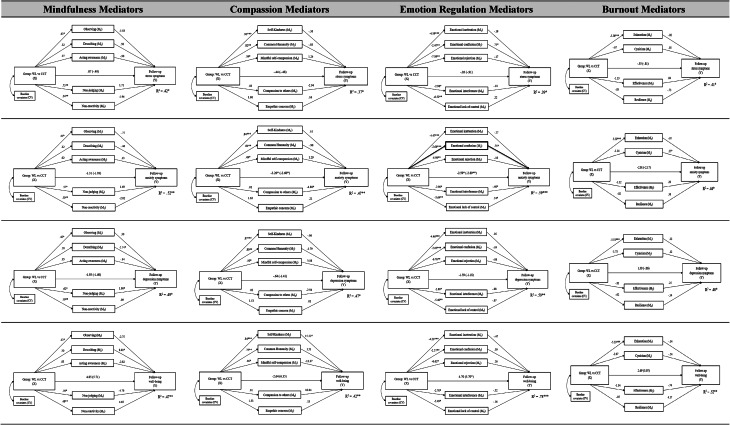
Follow-up mediators of change
Multiple mediation models of follow-up changes in psychological distress and well-being are shown in Table 4. The a-path showed similar results to those found at post-intervention mediations: the a-path was significant for some mindfulness facets (i.e., observing, non-judging, and non-reactivity), for self-compassion variables (i.e., self-kindness, common humanity, and mindful self-compassion), for all the emotion regulation difficulties, and for emotional exhaustion in academic life. However, most of the significant b-paths at post-intervention were no longer significant at follow-up: (1) no significant b-paths were found for stress symptoms at follow-up; (2) compassion to others, emotional confusion, emotional interference, and cynicism significantly predicted anxiety symptoms at follow-up; (3) describing and non-judging facets of mindfulness significantly predicted depression symptoms at follow-up; and (4) describing and self-kind changes significantly predicted psychological well-being at follow-up. However, the only significant indirect effect was found for emotional confusion mediating anxiety symptoms (ab = -2.00; S.E. = 0.97; 95% CI [-4.09, − 0.28]): the CCT predicted significant post-intervention reductions in emotional confusion, which in turn significantly predicted reductions in stress symptoms at follow-up. This model explained 59% of the variance in anxiety reduction at follow-up.
Table 4.
Follow-up multiple mediation models of stress (1st row), anxiety (2nd row), depression (3rd row), and well-being (4th raw). The paths show the unstandardized regression coefficients, and the path c is provided in brackets. Significant indirect effects are shown in bold. Note: * p < .05; ** p < .01; and *** p < .001.
Moderations
The interaction term was not statistically significant for almost all moderators (p > .05), which means that the effects of the interventions on psychological distress and well-being were not explained by confounding variables moderating the results (see Table 5). The only significant moderator was gender for all the outcomes at post-intervention: stress (-8.47 [-13.13, -4.09]), anxiety (-23.15 [-27.15, -19.25]), depression (-20.78 [-28.58, -13.03]), and well-being (32.35 [19.81, 44.41]). Overall, the results suggest that the CCT was more effective for women than for men at post intervention, however these differences vanished at follow-up (where gender did not significantly moderate the relationship).
Table 5.
Moderation models. Unstandardized regression coefficients (b) and 95% confidence intervals (CI) of the interaction term are presented. Pre-intervention outcomes scores were included as covariates in the models.
| Post-intervention changes | Follow-up changes | |||||||
|---|---|---|---|---|---|---|---|---|
| Stress | Anxiety | Depression | Well-being | Stress | Anxiety | Depression | Well-being | |
| Age | 0.12 (-0.31, 1.20) | 0.34 (-0.05, 1.44) | 0.29 (-0.18, 1.36) | − 0.62 (-2.89, 1.21) | − 0.18 (-0.76, 0.49) | − 0.12 (-0.48, 0.74) | − 0.02 (-0.75, 0.55) | 0.59 (-0.62, 4.41) |
| Gender | -8.47 (-13.13, -4.09) | -23.15 (-27,15, -19.25) | -20.78 (-28.58, -13.03) | 32.35 (19.81, 44,41) | -4.88 (-10.04, 0.31) | -3.11 (-6.28, 0.06) | -1.08 (-3.19, 0.96) | 0.86 (-7.73, 8.97) |
| Nationality | 3.07 (-1.37, 8.29) | 2.03 (-2.61, 6.39) | 0.98 (-4.89, 6.60) | -2.38 (-4.76, 1.99) | 1.36 (-2.13, 4.53) | − 0.27 (-4.87, 3.04) | 1.55 (-0.99, 4.71) | -14.16 (-44.47, 16.15) |
| Marital status | -1.36 (-6.12, 3.51) | 4.26 (-1.07, 10.63) | 4.39 (-2.14, 11.90) | -3.42 (-16.89, 9.61) | 3.02 (-1.19, 7.22) | 0.85 (-3.43, 4.73) | 2.04 (-2.04, 5.87) | -5.05 (-17.32, 6.89) |
| Meditation experience | ||||||||
| Priori experience | − 0.81 (-5.43, 4.82) | -2.49 (-8.47, 3.49) | -2.02 (-9.01, 3.87) | 9.35 (-1.33, 20.67) | -1.26 (-4.93, 2.84) | 1.69 (-2.02, 5.48) | − 0.26 (-4,22, 3.73) | 3.69 (-10.21, 18.49) |
| Currently meditation | -3.10 (-7.72, 2,13) | -2.88 (-8.96, 2.27) | -2.36 (-10.79, 4,61) | 9.29 (-0.36, 20.24) | -2.56 (-6.41, 2.11) | 1.98 (-2.15, 6.01) | 0.07 (-4.76, 4.91) | -1.89 (-16.68, 11.92) |
| Time (months) | − 0.04 (-0.29, 0.22) | − 0.05 (-0.51, 0.11) | − 0.03 (-0.57, 0.16) | 0.29 (-0.13, 1.29) | − 0.07 (-0.37, 0.10) | 0.09 (-0.34, 0.28) | 0.02 (-0.33, 0.17) | − 0.05 (-0.48, 1.40) |
Significant values are in bold.
Discusion
Medical practice exposes physicians to numerous stressors, leading to high rates of psychological distress and burnout, a problem that begins during medical school. Fortunately, scientific evidence suggests that promoting compassion among physicians and medical students could improve both their psychological well-being and their ability to provide patient-centered care. However, we still do not know the mechanisms of change underlying these benefits. Therefore, the aim of this study was to examine the mediators and moderators of change in psychological distress and well-being following Compassion Cultivation Training among medical students. We hypothesized that improvements in mindfulness, compassion, emotion regulation, and burnout-related variables would mediate the effects of CCT on psychological distress and well-being. Additionally, we explored demographic factors and prior meditation experience as potential moderators of changes.
The main results of this study were that CCT (compared to the WL) led to significant reductions in stress and anxiety immediately after the program, primarily mediated by improvements in emotion regulation (specifically emotional confusion) and mindfulness (specifically non-judging of inner experience). However, these results vanished at the 2-month follow-up, with emotional confusion being the only mediator that maintained its influence on anxiety symptoms at follow-up. Additionally, gender was the only significant moderator of changes in stress, anxiety, depression, and well-being, with women benefitted more from the compassion training than men, although these differences were not sustained at follow-up. These results contribute to the existing literature on the effects of CCT on medical students23,26, expanding the evidence on the mechanisms of change of compassionate practices to the specific case of healthcare professionals22.
Our results showed that reductions in stress and anxiety symptoms post-intervention were significantly mediated by decreases in emotional confusion, one of the key components of emotional regulation42. Difficulties in identifying and describing emotional experiences have been linked to a range of affective disorders51, so improving the recognition and clarity of their emotional states is a crucial skill for medical students. Meditation-based programs have shown to improve emotional clarity in the general population52, which we now extend to compassion training in medical students. This finding aligns with previous studies highlighting the role of emotion regulation in managing stress and anxiety, and especially in the case of university students53. Studies have shown that improving emotion regulation can reduce psychological distress among healthcare professionals54, whereas difficulties in emotion regulation predict empathy and patient-centeredness in medical students55. Therefore, interventions and trainings targeting emotional clarity in physicians and medical students can be crucial in distress managing and compassionate patient care, providing tools to handle the inherent stressors of their profession. Interestingly, the reduction in anxiety symptoms mediated by emotional confusion was maintained at the 2-month follow-up, highlighting the enduring impact of CCT on emotional regulation skills, which is crucial for long-term mental health56.
Our study also found that CCT led to reductions in anxiety symptoms through improvements in non-judging of inner experience, a critical component of mindfulness57. Non-judgmental awareness allows medical students to observe their thoughts and emotions without getting entangled in them, assuming the stance of an impartial observer free from judgments or labels58. This is consistent with previous research suggesting that the more you judge the worse you feel and how a judgmental attitude towards one’s inner experience predicts anxiety59. Additionally, nonjudging of inner experience has been shown to predict internalizing distress60, being a fundamental target of medical training to support overall mental health and resilience in the face of academic and professional challenges.
Contrary to our initial hypotheses, we did not find significant mediators for the changes in depression symptoms and psychological well-being. This finding may suggest that the mechanisms through which CCT improves depression and well-being in medical students might be more complex and not solely attributable to psychological variables. For instance, previous studies have found that depression in medical students can be influenced by workload, long working hours, and administrative demands, as well as a mix of academic and healthcare stressors, as students are exposed not only to difficult exams but also to potentially traumatic experiences such as performing surgeries, dealing with critically ill patients, and witnessing deaths61. Surprisingly, none of the compassion and empathy mechanisms significantly mediated the changes in psychological distress and well-being28,29, which might suggest that compassion is an outcome of these programs and not necessarily a mechanism driving mental health improvements. Additionally, only one mechanism continued to have significant effects at the two-month follow-up (i.e., emotional confusion mediating anxiety symptoms), which might suggest the need to integrate compassion practice as part of the ongoing training for physicians and medical students, providing opportunities for ongoing practice and reinforcement over time. There could also be methodological limitations explaining the absence of some important mechanisms, such as the small sample size of the study or the types of measures used. Future research should explore additional mediators, such as social support and external stressors, recognizing the role of contextual and social variables in mental health62,63. This will help us better understand the pathways through which compassion exerts its positive effects.
Finally, we also found that gender significantly moderated the effects of CCT on changes in stress, anxiety, depression, and well-being, with women benefiting more from the compassion training than men. This finding is consistent with previous research suggesting gender differences in response to psychological interventions, where with women often reporting greater benefits64. Similarly, gender has emerged as a significant moderator of the association between self-compassion and emotional reactivity, with this relationship being stronger for women than for men65. Self-identified men have shown significantly higher levels of self-compassion than self-identified women66, with women demonstrating greater potential for improvements in interventions aimed at enhancing compassion. Furthermore, men’s poorer response to CCT might be partly due to lower levels of commitment to the groups and lower levels of compatibility with the other group members (primarily females). Future studies should explore tailored approaches to maximize the effectiveness compassion training for different genders, introducing gender-specific components to enhance engagement and outcomes for medical students.
This study has several limitations that should be acknowledged. First, the sample size was moderate and predominantly female, which limits the generalizability of the findings. The lower enrollment of male participants in our study reflects the gender distribution within health care careers67, where female students often outnumber their male counterparts. Furthermore, previous research suggests that women are generally more likely than men to participate in psychological interventions related to mental health and well-being68 .This highlights the importance of further research exploring how compassion programs can be tailored to better engage male participants. Second, the reliance on self-report measures may introduce response biases, which could be addressed through additional methodological considerations, and future research could incorporate behavioral and experimental tasks69. Third, the nature of CCT prevents participants from being blinded to the intervention, which could lead to social desirability effects. Future studies should replicate our results with an active control condition (e.g., a relaxation program) and explore additional mechanisms (e.g., social support, workload, personal values alignment, etc.), in order to provide a more comprehensive understanding of how compassion training heals physicians and medical students. Finally, the lack of sustained significant changes and mediators at follow-up may suggest the potential value of incorporating maintenance sessions throughout the academic year to reinforce the intervention’s effects and support the ongoing meditation practice. Future studies should consider adopting longer longitudinal designs (e.g., one-year follow-up) to assess the durability of CCT outcomes over time, exploring the role of continued meditation practice as a mediator of long-term effects.
Despite these limitations, the study has certain strengths, including the use of a randomized controlled trial design with a waitlist control group, the use of a well-validated and standardized compassion program, the inclusion of a follow-up assessment to analyze the maintenance of the mechanisms over time, the assessment of multiple potential mediators and moderators based on previous studies and empirical models, the use of robust mathematical models to test mechanisms (such as multiple mediation models controlling for covariates at baseline, compared to simple mediations), and the dual approach in which we examine not only reductions in psychological distress but also improvements in well-being as two independent yet related dimensions. For all the above, we believe that the results of this study contribute to the growing body of literature on the benefits of compassion training in healthcare settings and provide valuable insights into the specific mechanisms through which compassion exerts its effects. The findings highlight the importance of integrating compassion training into medical education to enhance emotional regulation skills, which could contribute to better mental health and professional performance, ultimately improving the humanization of healthcare.
Acknowledgements
This research was supported by Cátedra de Humanización de la Asistencia Sanitaria (VIU), Fundación ASISA and Proyecto HUCI.
Author contributions
SR and BR contributed equally to this work and share first authorship. PR and BR designed the study. BR recruited participants. PR and SR analyzed the data. SR, BR, and PR wrote the manuscript. SR and PR review the manuscript. PR supervised the project.
Data availability
The data that support the findings of this study are available from the corresponding author upon request.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sara Rodriguez-Moreno and Blanca Rojas contributed equally to this work.
References
- 1.Shah, M. K. et al. Prevalence of and factors associated with nurse burnout in the US. JAMA Netw. Open.4, e2036469–e2036469 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wasson, R., Barratt, C. & Mindfulness, W. O. & undefined. Effects of mindfulness-based interventions on self-compassion in health care professionals: a meta-analysis. SpringerRS Wasson, C Barratt, WH O’BrienMindfulness, 2020•Springer 11, 1914–1934 (2020). (2020). [DOI] [PMC free article] [PubMed]
- 3.Rao, S. K. et al. The impact of administrative burden on academic physicians: results of a hospital-wide physician survey. Acad. Med.92, 237–243 (2017). [DOI] [PubMed] [Google Scholar]
- 4.O’Dowd, E. et al. Stress, coping, and psychological resilience among physicians. BMC Health Serv. Res.18, 730 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.West, C., Dyrbye, L. & Shanafelt, T. Physician burnout: contributors, consequences and solutions. J. Intern. Med.283, 516–529 (2018). [DOI] [PubMed] [Google Scholar]
- 6.Hardy, P. et al. Comparison of burnout, anxiety and depressive syndromes in hospital psychiatrists and other physicians: results from the ESTEM study. Psychiatry Res.284, 112662 (2020). [DOI] [PubMed] [Google Scholar]
- 7.Shanafelt, T. et al. (ed, D.) Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin. Proc.94 1681–1694 (2019). [DOI] [PubMed] [Google Scholar]
- 8.Maser, B., Danilewitz, M., Guérin, E., Findlay, L. & Frank, E. Medical student psychological distress and mental illness relative to the general population: a Canadian cross-sectional survey. Acad. Med.94, 1781–1791 (2019). [DOI] [PubMed] [Google Scholar]
- 9.Dyrbye, L. N. et al. Burnout and suicidal ideation among U.S. medical students. Ann. Intern. Med.149, 334–341 (2008). [DOI] [PubMed] [Google Scholar]
- 10.Kelm, Z., Womer, J., Walter, J. K. & Feudtner, C. Interventions to cultivate physician empathy: a systematic review. BMC Med. Educ.14, 219 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shanafelt, T. D., Bradley, K. A., Wipf, J. E. & Back, A. L. Burnout and self-reported patient care in an internal medicine residency program. Ann. Intern. Med.136, 358–367 (2002). [DOI] [PubMed] [Google Scholar]
- 12.West, C. P., Dyrbye, L. N., Erwin, P. J. & Shanafelt, T. D. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet388, 2272–2281 (2016). [DOI] [PubMed] [Google Scholar]
- 13.Shanafelt, T. D. et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin. Proc. 90, 1600–1613 (2015). [DOI] [PubMed]
- 14.Dzeng, E. et al. Moral distress amongst American physician trainees regarding futile treatments at the end of life: a qualitative study. J. Gen. Intern. Med.31, 93–99 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sinclair, S. et al. What is the state of compassion education? A systematic review of compassion training in health care. Acad. Med.96, 1057 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Menezes, P., Guraya, S. Y. & Guraya, S. S. A systematic review of educational interventions and their impact on empathy and compassion of undergraduate medical students. Front. Med.8, 758377 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marshman, C., Allen, J., Ling, D. & Brand, G. It’s very values driven’: a qualitative systematic review of the meaning of compassion according to healthcare professionals. J. Clin. Nurs.33, 1647–1665 (2024). [DOI] [PubMed] [Google Scholar]
- 18.Malenfant, S., Jaggi, P., Hayden, K. A. & Sinclair, S. Compassion in healthcare: an updated scoping review of the literature. BMC Palliat. Care. 21, 1–28 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sinclair, S., Russell, L. B., Hack, T. F., Kondejewski, J. & Sawatzky, R. Measuring compassion in healthcare: a comprehensive and critical review. Patient10, 389–405 (2017). [DOI] [PubMed] [Google Scholar]
- 20.Kirby, J. N., Tellegen, C. L. & Steindl, S. R. A Meta-analysis of compassion-based interventions: current state of knowledge and future directions. Behav. Ther.48, 778–792 (2017). [DOI] [PubMed] [Google Scholar]
- 21.Roca, P., Diez, G., McNally, R. J. & Vazquez, C. The impact of compassion meditation training on psychological variables: a network perspective. Mindfulness (N Y). 12, 873–888 (2021). [Google Scholar]
- 22.Scarlet, J., Altmeyer, N., Knier, S. & Harpin, R. E. The effects of compassion cultivation training (CCT) on health-care workers. Clin. Psychol.21, 116–124 (2017). [Google Scholar]
- 23.Weingartner, L. A., Sawning, S., Shaw, M. A. & Klein, J. B. Compassion cultivation training promotes medical student wellness and enhanced clinical care. BMC Med. Educ.19, 139 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Germer, C. K. & Neff, K. D. Self-Compassion in Clinical Practice. J. Clin. Psychol.69, 856–867 (2013). [DOI] [PubMed] [Google Scholar]
- 25.Maloney, S. et al. Target mechanisms of mindfulness-based programmes and practices: a scoping review. BMJ Ment Heal27, (2024). [DOI] [PMC free article] [PubMed]
- 26.Rojas, B., Catalan, E., Diez, G. & Roca, P. A compassion-based program to reduce psychological distress in medical students: a pilot randomized clinical trial. PLoS One. 18, e0287388 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Van Dam, N. T. et al. Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspect. Psychol. Sci.13, 36–61 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roca, P., Vazquez, C., Diez, G., Brito-Pons, G. & McNally, R. J. Not all types of meditation are the same: mediators of change in mindfulness and compassion meditation interventions. J. Affect. Disord. 283, 354–362 (2021). [DOI] [PubMed] [Google Scholar]
- 29.Roca, P., Vazquez, C., Diez, G. & McNally, R. J. How do mindfulness and compassion programs improve mental health and well-being? The role of attentional processing of emotional information. J. Behav. Ther. Exp. Psychiatry. 81, 101895 (2023). [DOI] [PubMed] [Google Scholar]
- 30.Pavlova, A., Wang, C. X. Y., Boggiss, A. L., O’Callaghan, A. & Consedine, N. S. Predictors of physician compassion, empathy, and related constructs: a systematic review. J. Gen. Intern. Med.10.1007/s11606-021-07055-2 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao, F. F., Yang, L., Ma, J. P. & Qin, Z. J. Path analysis of the association between self-compassion and depressive symptoms among nursing and medical students: a cross-sectional survey. BMC Nurs.21, 1–11 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lovibond, P. F. & Lovibond, S. H. The structure of negative emotional states: comparison of the Depression anxiety stress scales (DASS) with the Beck Depression and anxiety inventories. Behav. Res. Ther.33, 335–343 (1995). [DOI] [PubMed] [Google Scholar]
- 33.Daza, P., Novy, D. M., Stanley, M. A. & Averill, P. The depression anxiety stress scale-21: Spanish translation and validation with a hispanic sample. J. Psychopathol. Behav. Assess.24, 195–205 (2002). [Google Scholar]
- 34.Vázquez, C., Duque, A. & Hervás, G. Satisfaction with life scale in a representative sample of Spanish adults: validation and normative data. Span. J. Psychol.16, 1–15 (2013). [DOI] [PubMed] [Google Scholar]
- 35.Raes, F., Pommier, E., Neff, K. D. & Van Gucht, D. Construction and factorial validation of a short form of the Self-compassion Scale. Clin. Psychol. Psychother.18, 250–255 (2011). [DOI] [PubMed] [Google Scholar]
- 36.Garcia-Campayo, J. et al. Validation of the Spanish versions of the long (26 items) and short (12 items) forms of the Self-Compassion Scale (SCS). Health Qual. Life Outcomes. 12, 1–9 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pommier, E. & Neff, K. D. Tóth-Király, I. The development and validation of the compassion scale. Assessment27, 21–39 (2020). [DOI] [PubMed] [Google Scholar]
- 38.Davis, M. H. A multidimensional approach to individual differences in empathy. Cat Sel. Doc. Psychol.10, 85 (1980). [Google Scholar]
- 39.Fernández, A. M., Dufey, M. & Kramp, U. Testing the psychometric properties of the interpersonal reactivity index (IRI) in Chile. (2011). 10.1027/1015-5759/a000065 27, 179–185. [DOI]
- 40.Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J. & Toney, L. Using self-report assessment methods to explore facets of mindfulness. Assessment13, 27–45 (2006). [DOI] [PubMed] [Google Scholar]
- 41.Cebolla, A. et al. Psychometric properties of the Spanish validation of the five facets of Mindfulness Questionnaire (FFMQ). Eur. J. Psychiatry. 26, 118–126 (2012). [Google Scholar]
- 42.Gratz, K. L. & Roemer, L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the difficulties in emotion regulation scale. J. Psychopathol. Behav. Assess.26, 41–54 (2004). [Google Scholar]
- 43.Hervás, G. Adaptación Al Castellano De Un instrumento para evaluar El Estilo Rumiativo. Rev. Psicopatología Y Psicol. Clínica. 13, 111–121 (2008). [Google Scholar]
- 44.Galán, F., Sanmartín, A., Polo, J. & Giner, L. Burnout risk in medical students in Spain using the Maslach burnout inventory-student survey. Int. Arch. Occup. Environ. Health. 84, 453–459 (2011). [DOI] [PubMed] [Google Scholar]
- 45.Smith, B. W. et al. The brief resilience scale: assessing the ability to bounce back. Int. J. Behav. Med.15, 194–200 (2008). [DOI] [PubMed] [Google Scholar]
- 46.Rodríguez-Rey, R., Alonso-Tapia, J. & Hernansaiz-Garrido, H. Reliability and validity of the brief resilience scale (BRS) Spanish version. Psychol. Assess.28, e101 (2016). [DOI] [PubMed] [Google Scholar]
- 47.Moher, D. et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. Int. J. Surg.10, 28–55 (2012). [DOI] [PubMed] [Google Scholar]
- 48.Schotanus-Dijkstra, M., Pieterse, M. E., Drossaert, C. H. C., Walburg, J. A. & Bohlmeijer, E. T. Possible mechanisms in a multicomponent email guided positive psychology intervention to improve mental well-being, anxiety and depression: a multiple mediation model. J. Posit. Psychol.14, 141–155 (2019). [Google Scholar]
- 49.Tabachnick, B. G., Fidell, L. S. & Ullman, J. Using multivariate statistics title: Using multivariate statistics (Vol.5)Pearson,. (2007).
- 50.Hayes, A. F. Introduction to Mediation, Moderation, and Conditional: A regression-based Approach Process Analysis (The Guilford Press, 2018).
- 51.Vine, V. & Aldao, A. Impaired emotional clarity and psychopathology: A transdiagnostic deficit with symptom-specific pathways through emotion regulation. (2014). 10.1521/jscp.2014.33.4.319 33, 319–342. [DOI]
- 52.Cooper, D., Yap, K. & Batalha, L. Mindfulness-based interventions and their effects on emotional clarity: a systematic review and meta-analysis. J. Affect. Disord. 235, 265–276 (2018). [DOI] [PubMed] [Google Scholar]
- 53.Naser, S. G., Parviz, P., Seifollah, A. & Mohammad, N. Effectiveness of emotion regulation training on reduction of anxiety. Heal Educ. Heal Promot. 3, 5–13 (2015). [Google Scholar]
- 54.Krasner, M. S. et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA302, 1284–1293 (2009). [DOI] [PubMed] [Google Scholar]
- 55.Ardenghi, S., Russo, S., Bani, M., Rampoldi, G. & Strepparava, M. G. The role of difficulties in emotion regulation in predicting empathy and patient-centeredness in pre-clinical medical students: a cross-sectional study. Psychol. Health Med.28, 1215–1229 (2023). [DOI] [PubMed] [Google Scholar]
- 56.Voltmer, E., Rosta, J., Aasland, O. G. & Spahn, C. Study-related health and behavior patterns of medical students: a longitudinal study. Med. Teach.32, (2010). [DOI] [PubMed]
- 57.Mattes, J. Systematic review and meta-analysis of correlates of FFMQ mindfulness facets. Front. Psychol.10, 445667 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kabat-Zinn, J. & Hanh, T. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illnessDelta,. (2009).
- 59.Barcaccia, B. et al. The more you judge the worse you feel. A judgemental attitude towards one’s inner experience predicts depression and anxiety. Pers. Individ Dif.138, 33–39 (2019). [Google Scholar]
- 60.Hsu, T. & Forestell, C. A. Mindfulness, depression, and emotional eating: the moderating role of nonjudging of inner experience. Appetite160, 105089 (2021). [DOI] [PubMed] [Google Scholar]
- 61.Rotenstein, L. S. et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA316, 2214–2236 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rodriguez-Moreno, S. et al. Initial effectiveness evaluation of the Unified Protocol for transdiagnostic treatment of emotional disorders for homeless women. https://doi org (2022). 46, 506–528 [DOI] [PubMed]
- 63.Rodriguez-Moreno, S., Vázquez, J. J., Roca, P. & Panadero, S. Differences in stressful life events between men and women experiencing homelessness. J. Community Psychol.49, 375–389 (2021). [DOI] [PubMed] [Google Scholar]
- 64.Ogrodniczuk, J. S. Men, women, and their outcome in psychotherapy. Psychother. Res.16, 453–462 (2006). [Google Scholar]
- 65.Helminen, E. C., Scheer, J. R. & Felver, J. C. Gender differences in the associations between mindfulness, self-compassion, and perceived stress reactivity. Mindfulness (N Y). 12, 2173–2183 (2021). [Google Scholar]
- 66.Yarnell, L. M., Neff, K. D., Davidson, O. A. & Mullarkey, M. Gender differences in self-compassion: examining the role of gender role orientation. Mindfulness (N Y). 10, 1136–1152 (2019). [Google Scholar]
- 67.Adams, T. L. Gender and feminization in health care professions. Sociol. Compass.4, 454–465 (2010). [Google Scholar]
- 68.Seaton, C. L. et al. Men’s mental health promotion interventions: a scoping review. Am. J. Mens Health11, 1823–1837 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Roca, P. & Vazquez, C. Brief meditation trainings improve performance in the emotional attentional blink. Mindfulness (N Y). 11, 1613–1622 (2020). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon request.