Abstract
BACKGROUND:
The Stepped Care Model (SCM) is an evidence-based treatment approach that tailors treatment intensity based on patients’ health status, aiming to achieve the most positive treatment outcomes with the least intensive and cost-effective interventions. Currently, the effectiveness of the Stepped Care Model in postoperative rehabilitation for TKA (Total Knee Arthroplasty) patients has not been reported.
OBJECTIVE:
The present study aimed to investigate whether the stepped care model could improve early-stage self-report quality of life and knee function after total knee arthroplasty via a prospective randomized controlled design.
METHODS:
It was a mono-center, parallel-group, open-label, prospective randomized controlled study. Patients who aging from 60–75 years old as well as underwent unilateral primary total knee arthroplasty due to end-stage knee osteoarthritis between 2020.06 to 2022.02 were enrolled. Participants were randomized and arranged into two groups in a 1:1 allocation. The control group was given traditional rehabilitation guidance, while the stepped care model group was given continued stepped care. Hospital for special surgery knee score, daily living ability (ADL), knee flexion range, and adverse events at 1, 3, and 6 months after total knee arthroplasty were recorded.
RESULTS:
88 patients proceeded to the final analysis. There was no significant difference of age, gender, length of stay, BMI, and educational level between the two groups at the baseline. After specific stepped care model interventions, patients showed significant improvements in HHS in 1 month (85.00 (82.25, 86.00) vs. 80.00 (75.00, 83.00), 0.001), 3 months (88.00 (86.00, 92.00) vs. 83.00 (76.75, 85.00), 0.001), and 6 months (93.00 (90.25, 98.00) vs. 88.00 (84.25, 91.75), 0.001) when compared with the control group. Similar results were also found in both daily living ability and knee flexion angle measurements. No adverse event was observed during the follow-up.
CONCLUSION:
The present study found that the stepped care model intervention significantly improved early-stage knee function and self-reported life quality after total knee arthroplasty due to knee osteoarthritis. Female patients and those less than 70 years old benefit more from the stepped care model intervention after total knee arthroplasty.
Keywords: Stepped care model, total knee arthroplasty, randomized controlled trail, knee function, life quality
1. Introduction
Total knee arthroplasty (TKA) stands as the most efficacious remedy for end-stage knee osteoarthritis, a condition witnessing a surge in incidence alongside the global aging demographic [1]. In the United States alone, approximately 680,000 TKAs are performed annually, with projections estimating a rise to 3.48 million procedures by 2030 [2, 3]. However, akin to the heterogeneous disease progression and long-term prognosis of knee osteoarthritis, patient-specific factors closely influence the outcome of TKA [4, 5, 6]. Consequently, patient-reported satisfaction post-TKA lags behind other elective joint surgeries, such as total hip arthroplasty. Even after ruling out peri-prosthetic infection and implant-related issues like malalignment or oversizing, around 10% of patients endure persistent knee pain and restricted range of motion due to unspecified causes [7, 8]. It has been hypothesized that insufficient functional exercise, weak muscle strength, cognitive impairment, or psychological disorders may underlie the dissatisfaction experienced by these patients post-TKA [9]. Although a definitive standard therapy remains elusive, studies suggest that preoperative and postoperative physical therapy education provided by dedicated rehabilitation teams could mitigate the time taken to achieve functional milestones and reduce the risk of unfavorable outcomes following TKA [10, 11].
The stepped Care Model (SCM) is an evidence-based treatment model to take different intensities of treatment in different stages according to the health status of patients in order to achieve the most positive treatment effect by providing the lowest intensity, cost-effective intervention [12]. Briefly, SCM starts with low-intensity treatment, and if patients do not achieve the desired treatment effect after each stage of intervention, a higher level of intensity intervention would carry out. SCM is mostly used in foreign primary care systems, focusing on behavioral health and psychological problems, such as depression, anxiety disorders, eating disorders, drug abuse, musculoskeletal pain, and somatoform disorders [13, 14, 15, 16]. At present, the efficiency of SCM on postoperative rehabilitation in TKA patients has not yet been reported. Consequently, the present study aimed to investigate whether SCM could improve early-stage self-report quality of life and knee function after total knee arthroplasty via a prospective randomized controlled design.
2. Materials and methods
2.1. Study design
This mono-center, parallel-group, open-label, prospective randomized controlled study was conducted in the department of Orthopaedic, Guangdong Provincial Peoples’ Hospital, Southern Medical University. Our research was carried out following the ethical guidelines outlined in the Declaration of Helsinki and received approval from our hospital’s institutional review board (KY2020-643-01). Consent forms were duly signed by all participants, and the study has been registered with the Chinese Clinical Trial Registry Center.
2.2. Inclusion and exclusion criteria
Patients who aging from 60–75 years old as well as underwent unilateral primary total knee arthroplasty due to end-stage knee osteoarthritis in our department between 2020.06 to 2022.02 were enrolled in the present study. We excluded patients who: (1) with severe collateral ligament impairment or bone defect which needed constrained implants, metal augments, or rods. (2) with a previous history of surgery, trauma, neuromuscular diseases, extra-articular deformity, or infection in the operated lower limb. (3) with cognition impairment. (4) were pregnant or lactating. (5) were unwilling to participate. During the follow-up, patients fulfilling the following criteria were also excluded: (1) diagnosed with the postoperative periprosthetic joint infection, periprosthetic fracture, or venous thromboembolism. (2) lost to follow-up. (3) demanded to withdraw from the study. (4) readmission for other diseases.
2.3. Randomization and SCM intervention
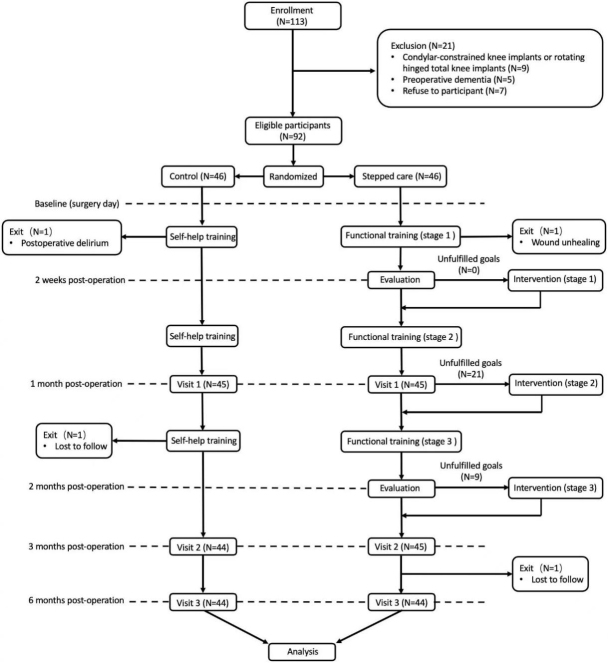
After giving consent, eligible participants were randomized and arranged into two groups in a 1:1 allocation. Trained outcome assessors and data collectors were blinded to group allocation throughout the study. The control group was given traditional rehabilitation guidance [17], while the SCM group was given continued stepped care (Fig. 1). Details of our SCM rehabilitation protocol for patients who underwent TKA were shown in Table 2. Firstly, rehabilitation protocols and stage goals regarding different postoperative periods were set. Our trained staff contacted patients in the SCM group at each time point of stage goal evaluation via telephone follow-up or on-site consultation. SCM interventions are needed if patients were unable to fulfill any stage of rehabilitation goals.
Figure 1.
92 patients were randomly divided into two groups: control group ( 46) and SCM group ( 46). Four patients exited during the study.
Table 2.
Details of our stepped care model for patients underwent total knee arthroplasty
| Stage I (1–2 weeks post-operation) | Stage II (2–4 weeks post-operation) | Stage III (4–8 weeks post-operation) | |
|---|---|---|---|
| Functional training |
|
Stage I
|
Stage II
|
| Rehabilitation goals |
|
|
|
| Interventions(if needed) |
|
|
|
2.4. Outcome measures
The primary outcome is the Hospital for Special Surgery Knee Score (HSS) at 30 days post-operation, which was assessed by blinded assessors during a face-to-face assessment at the clinic visit. Secondary outcomes include HSS at 3 and 6 months after TKA, daily living ability (ADL) and knee flexion range at 1, 3, and 6 months after TKA, as well as adverse complications including periprosthetic fracture, periprosthetic joint infection, and deep vein thrombosis, etc. Post hoc subgroup analysis was conducted regarding patients’ age, gender, and education.
2.5. Sample size
An observational study conducted in China reported that the 6-month HSS score in the SCM group and control group were 79.54 4.27 and 85.21 6.35, respectively [17]. Using G Power 3.1 software, with the effect size setting as 1.047 ( 0.01, 1 0.95), the estimated sample size was 70. The final number of participants was set as 88 regarding the 20% drop-out rate.
2.6. Statistical analysis
Mean standard deviation or median with interquartile range were used to represent continuous data. Percentages (count) were employed for presenting categorical data Demographic data and clinical outcomes were summarized and compared using bivariate tests (student T test, Mann–Whitney U, 2, or Fisher’s exact tests). A -value of 0.05 was considered to be significant. SPSS 20.0 (SPSS Headquarters, Chicago, IL, USA) and SAS 9.4 (SAS Institute Cary, NC, USA) were used to carry out the statistical analysis.
3. Results
3.1. Demographic data
As depicted in Fig. 1, the present study included a total of 92 eligible patients, with an equal distribution of 46 patients in each group At the end of the 6 months follow-up of the last participants, 4 patients were exited, two were lost to follow-up, one for postoperative delirium and another one was due to wound unhealing. 88 patients (10 males and 78 females) proceeded to the final analysis. There were no notable distinctions observed in terms of age, gender, duration of stay, BMI, and educational attainment between the two groups (Table 1). In the first week after TKA, baseline clinical outcomes including ADL, HHS, and knee flexion angle were comparable between the control and SCM groups. In the SCM group, all the patients fulfilled the stage goal 1 after the functional training. But 21 and 9 patients were unable to reach the requirements of stage goals 2 and 3, respectively. Consequently, stage-specific SCM interventions (Table 2) were initiated in those patients.
Table 1.
Demographic data and baseline clinical outcomes
| Items | SCM group ( 44) | Control ggroup ( 44) | value |
|---|---|---|---|
| Age (years), mean (SD) | 66.7 6.1 | 68.1 7.2 | 0.330 |
| Gender (male), (%) | 4 (9.1%) | 6 (13.6%) | 0.739 |
| Educational level, (%) | 0.590 | ||
| Primary school | 32 (72.7%) | 27 (61.4%) | |
| Junior high school | 7 (15.9%) | 8 (18.2%) | |
| Senior high school | 4 (9.1%) | 6 (13.6%) | |
| College | 1 (2.3%) | 3 (6.9%) | |
| BMI (kg/m2), mean (SD) | 26.04 3.105 | 25.39 3.068 | 0.320 |
| Length of stay (days), mean (SD) | 5.93 2.731 | 5.50 2.074 | 0.406 |
| ADL, median (quartile) | 65.00 (60.00, 73.75) | 67.50 (61.25, 75.00) | 0.644 |
| HSS score, median (quartile) | 67.00 (56.25, 68.00) | 67.00 (60.00, 67.00) | 0.689 |
| Knee flexion (∘), median (quartile) | 95.50 (87.50, 98.00) | 95.00 (90.00, 97.88) | 0.634 |
3.2. Clinical outcomes
After specific SCM interventions, patients showed significant improvements in HHS in 1 month (85.00 (82.25, 86.00) vs. 80.00 (75.00, 83.00), 0.001), 3 months (88.00 (86.00, 92.00) vs. 83.00 (76.75, 85.00), 0.001), and 6 months (93.00 (90.25, 98.00) vs. 88.00 (84.25, 91.75), 0.001) when compared with the control group. As shown in Fig. 2, similar results were also found in both ADL and knee flexion angle measurements. No adverse event was observed during the follow-up.
Figure 2.
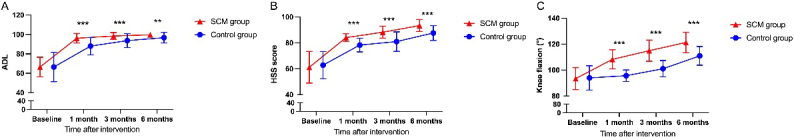
ADL, HSS and knee flexion in patients between SCM group and Control group. Segments with significant statistical differences (*: 0.05) between the groups were marked with asterisks.
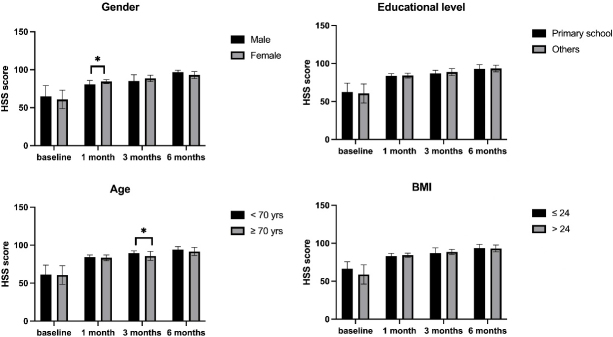
As for post Hoc analysis, female and younger patients trended to be benefited more from the SCM interventions. Illustrated by Fig. 3, there were significantly higher one-month HHS score in the female patients ( 0.05) and higher three-month HHS score in patients 70 years old ( 0.05).
Figure 3.
Post Hoc analysis in patients after SCM. Error bars denote the standard deviation of each group. Segments with significant statistical differences (*: 0.05) between the groups were marked with asterisks.
4. Discussion
In the present study, we found that the SCM intervention significantly improved the early-stage knee function and self-reported life quality after TKA due to knee osteoarthritis, when compared with the traditional rehabilitation guidance group. In the meanwhile, no adverse event was observed during the follow-up. Besides, our study also suggested that the SCM intervention is more effective in female patients and those less than 70 years old. Although the application of SCM in postoperative TKA rehabilitation has not yet been reported previously, our results were consistent with another study that focus on postoperative recovery in gynecological patients [18].
Although early postoperative rehabilitation exercise for TKA patients has been widely accepted, the optimal postoperative rehabilitation protocol doesn’t reach a consensus [19]. Under the background of fast-track surgery, the length of hospital stay for TKA patients has been decreased to 5.5 days in Australia and 6.6 days in the UK, which however led to insufficient in-hospital rehabilitation and patient education [20]. Patients encounter many problems during postoperative functional exercises, such as exercise-induced pain and fatigue, lack of understanding of exercise intensity, fear of exercise-related injury, and depression due to delayed function recovery [21]. There are also certain risks due to excessive exercise, such as wound dehiscence and falls, which indicates the requirement of professional guidance and assistance from healthcare providers after discharge.
Throughout the SCM, it is important to inform patients and service providers of the steps and progress and ensure that patients are actively involved in care and treatment options and decisions [22]. Consequently, SCM provides patients with a more comfortable care experience, and appropriate functional recovery expectation also gives patients confidence during the rehabilitation [23]. As the prognosis of TKA is closely related to patients’ psychological factors (such as trait anxiety) and functional exercises [24], we suggested that the timely and effective communication between the patients and our SCM team is one of the reasons for better recovery than the control group.
SCM provides interventions ranging from low intensity to high intensity for different stages of different patients [25]. These interventions combine individual, social, and structural psychological health factors, which can provide appropriate and accurate services according to individual needs change over time [26]. In our study, SCM provided specific rehabilitation advice according to patients’ feedback at each visit, and the detailed instruments in our study were partially referred to the Enhanced Recovery After Surgery Society recommendations for total joint replacement [27]. Compared to the control group, humanistic care is emphasized in addition to functional rehabilitation in the SCM group, which allows patients to recover both physically and mentally.
We acknowledge the limitations of our study, including the restricted sample size. Therefore, it is imperative to conduct a more extensive, multi-center, and long-term investigation in order to reinforce the validity of our findings. Besides, the bias of self-reported knee function and life quality is inevitable due to the varied pain thresholds and different educational levels of the participants. Lastly, image data such as CT/MRI were not evaluated in the present study.
5. Conclusion
The present study found that the SCM intervention significantly improved the early-stage knee function and self-reported life quality after TKA due to knee osteoarthritis when compared with the traditional rehabilitation guidance group. Female patients and those less than 70 years old benefit more from the SCM intervention after TKA.
Ethical approval
The present study was approved by the institutional review board of Guangdong Provincial People’s Hospital (KY2020-643-01).
Consent to participate and publication
Signed informed consents were obtained from all the participants.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author (13826039304@163.com) on reasonable request.
Author contributions
XH, HJ: Conceptualization, methodology, writing original draft preparation. PL, ZL: Investigation, software, statistical analysis. RZ: Reviewing and editing, funding acquisition, supervision. All authors read and approved the final manuscript.
Funding
This work was supported by the Medical Scientific Research Foundation of Guangdong Province of China (A2021038), Guangdong Basic and Applied Basic Research Foundation (2022A1515011103) and (2021A1515110458), as well as NSFC Incubation Program of GDPH (KY012021163).
Acknowledgments
Not applicable.
Conflict of interest
The authors have no conflicts of interest.
References
- [1]. Giorgino R, Albano D, Fusco S, Peretti GM, Mangiavini L, Messina C. Knee Osteoarthritis: Epidemiology, Pathogenesis, and Mesenchymal Stem Cells: What Else Is New? An Update. Int J Mol Sci. 2023; 24(7): 6405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2]. Davila CI, Recai TM, Abraham MM, et al. Rehabilitation protocols following total knee arthroplasty: a review of study designs and outcome measures. Ann Transl Med. 2019; 7(Suppl 7): S255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007; 89(4): 780-785. [DOI] [PubMed] [Google Scholar]
- [4]. Wu R, Ma Y, Yang Y, Li M, Zheng Q, Fu G. A clinical model for predicting knee replacement in early-stage knee osteoarthritis: data from osteoarthritis initiative. Clin Rheumatol. 2022; 41(4): 1199-1210. [DOI] [PubMed] [Google Scholar]
- [5]. Wu R, Ma Y, Li M, et al. Baseline Knee Pain Predicts Long-Term Response of Intra-Articular Steroid Injection in Symptomatic Knee Osteoarthritis: Data from OAI. Cartilage. 2023; 14(2): 144-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Wu R, Fu G, Li M, et al. Contralateral advanced radiographic knee osteoarthritis predicts radiographic progression and future arthroplasty in ipsilateral knee with early-stage osteoarthritis. Clin Rheumatol. 2022; 41(10): 3151-3157. [DOI] [PubMed] [Google Scholar]
- [7]. Holm B, Kristensen MT, Bencke J, Husted H, Kehlet H, Bandholm T. Loss of knee-extension strength is related to knee swelling after total knee arthroplasty. Arch Phys Med Rehab. 2010; 91(11): 1770-1776. [DOI] [PubMed] [Google Scholar]
- [8]. Dutta S, Ambade R, Wankhade D, Agrawal P. Rehabilitation Techniques Before and After Total Knee Arthroplasty for a Better Quality of Life. Cureus J Med Science. 2024; 16(2): e54877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Cheuy VA, Foran J, Paxton RJ, Bade MJ, Zeni JA, Stevens-Lapsley JE. Arthrofibrosis Associated With Total Knee Arthroplasty. J Arthroplasty. 2017; 32(8): 2604-2611. [DOI] [PubMed] [Google Scholar]
- [10]. Barker KL, Room J, Knight R, et al. Outpatient physiotherapy versus home-based rehabilitation for patients at risk of poor outcomes after knee arthroplasty: CORKA RCT. Health Technol Asses. 2020; 24(65): 1-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11]. Soeters R, White PB, Murray-Weir M, Koltsov J, Alexiades MM, Ranawat AS. Preoperative Physical Therapy Education Reduces Time to Meet Functional Milestones After Total Joint Arthroplasty. Clin Orthop Relat R. 2018; 476(1): 40-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12]. Roddy MK, Pfammatter AF, Mayberry LS. Optimizing adaptive stepped-care interventions to change adults’ health behaviors: A systematic review. J Clin Transl Sci. 2023; 7(1): e190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13]. Do MT, Nguyen TT, Tran H. Preliminary results of adapting the stepped care model for depression management in Vietnam. Front Psychiatry. 2022; 13: 922911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14]. Smink AJ, Dekker J, Vliet VT, et al. Health care use of patients with osteoarthritis of the hip or knee after implementation of a stepped-care strategy: an observational study. Arthrit Care Res. 2014; 66(6): 817-827. [DOI] [PubMed] [Google Scholar]
- [15]. Damush TM, Kroenke K, Bair MJ, et al. Pain self-management training increases self-efficacy, self-management behaviours and pain and depression outcomes. Eur J Pain. 2016; 20(7): 1070-1078. [DOI] [PubMed] [Google Scholar]
- [16]. Lowe B, Piontek K, Daubmann A, et al. Effectiveness of a Stepped, Collaborative, and Coordinated Health Care Network for Somatoform Disorders (Sofu-Net): A Controlled Cluster Cohort Study. Psychosom Med. 2017; 79(9): 1016-1024. [DOI] [PubMed] [Google Scholar]
- [17]. Feng JE, Novikov D, Anoushiravani AA, Schwarzkopf R. Total knee arthroplasty: improving outcomes with a multidisciplinary approach. J Multidiscip Health 2018; 11: 63-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18]. Bouwsma E, Huirne J, van de Ven PM, et al. Effectiveness of an internet-based perioperative care programme to enhance postoperative recovery in gynaecological patients: cluster controlled trial with randomised stepped-wedge implementation. Bmj Open. 2018; 8(1): e017781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19]. Walsh M, Woodhouse LJ, Thomas SG, Finch E. Physical impairments and functional limitations: a comparison of individuals 1 year after total knee arthroplasty with control subjects. Phys Therapy. 1998; 78(3): 248-258. [DOI] [PubMed] [Google Scholar]
- [20]. Henderson KG, Wallis JA, Snowdon DA. Active physiotherapy interventions following total knee arthroplasty in the hospital and inpatient rehabilitation settings: a systematic review and meta-analysis. Physiotherapy. 2018; 104(1): 25-35. [DOI] [PubMed] [Google Scholar]
- [21]. Kline PW, Melanson EL, Sullivan WJ, et al. Improving Physical Activity Through Adjunct Telerehabilitation Following Total Knee Arthroplasty: Randomized Controlled Trial Protocol. Phys Therapy. 2019; 99(1): 37-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22]. Meuldijk D, Wuthrich VM. Stepped-care treatment of anxiety and depression in older adults: A narrative review. Aust J Rural Health. 2019; 27(4): 275-280. [DOI] [PubMed] [Google Scholar]
- [23]. Rollman BL, Belnap BH, Mazumdar S, et al. Telephone-Delivered Stepped Collaborative Care for Treating Anxiety in Primary Care: A Randomized Controlled Trial. J Gen Intern Med. 2017; 32(3): 245-255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24]. Rice DA, Kluger MT, McNair PJ, et al. Persistent postoperative pain after total knee arthroplasty: a prospective cohort study of potential risk factors. Brit J Anaesth. 2018; 121(4): 804-812. [DOI] [PubMed] [Google Scholar]
- [25]. Kongsted A, Kent P, Quicke JG, Skou ST, Hill JC. Risk-stratified and stepped models of care for back pain and osteoarthritis: are we heading towards a common model? Pain Rep 2020; 5(5): e843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26]. Maehder K, Lowe B, Harter M, Heddaeus D, Scherer M, Weigel A. Management of comorbid mental and somatic disorders in stepped care approaches in primary care: a systematic review. Fam Pract. 2019; 36(1): 38-52. [DOI] [PubMed] [Google Scholar]
- [27]. Wainwright TEA. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Acta Orthop. 2020; 91(3): 363. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author (13826039304@163.com) on reasonable request.