Abstract
BACKGROUND:
Breast cancer (BC) is one of the most common malignancies in women and imposes a significant health burden globally. According to data from the World Health Organization, the incidence of BC has been increasing steadily over the years. It has become one of the leading causes of cancer-related death among women worldwide.
OBJECTIVE:
This work was to evaluate the combined intervention effect of psychological care along with the use of ondansetron, dexamethasone, and promethazine hydrochloride in breast cancer (BC) patients undergoing chemotherapy, including their impact on nausea and vomiting control, quality of life (QoL), and psychological status.
METHODS:
64 BC patients undergoing chemotherapy were collected and randomly rolled into a control group (Group C) and an intervention group (Group I). Group C received ondansetron combined with routine psychological support and counseling therapy, while Group I received a combination of ondansetron, dexamethasone, promethazine hydrochloride, and psychological care therapy. Self-assessment scores for anxiety, QoL ratings, white blood cell counts, and incidence of adverse reactions were assessed and compared between the two groups.
RESULTS:
Group I showed better control of nausea and vomiting versus Group C ( 0.05). Marked improvements were also observed in the self-rating anxiety scale (SAS) scores, white blood cell counts, and nursing satisfaction in Group I versus Group C ( 0.05). Nevertheless, the two groups had no significant difference regarding QoL scores ( 0.05).
CONCLUSION:
the combination of psychological care with ondansetron, dexamethasone, and promethazine hydrochloride effectively controls nausea and vomiting symptoms in BC patients undergoing chemotherapy and provides higher levels of clinical nursing satisfaction.
Keywords: Chemotherapy for breast cancer, psychological nursing, ondansetron, dexamethasone, promethazine hydrochloride
1. Introduction
Breast cancer (BC) is one of the most common malignancies in women and imposes a significant health burden globally. According to data from the World Health Organization, the incidence of BC has been increasing steadily over the years. It has become one of the leading causes of cancer-related death among women worldwide [1, 2]. Common side symptoms of chemotherapy, such as nausea and vomiting, can indicate that the treatment is working by killing cancer cells and possibly getting rid of poisons. These side effects may increase patient compliance since patients frequently interpret them as proof of the effectiveness of their therapy. The progression of BC is complex, and early-stage lesions often lack obvious symptoms, leading to many patients being diagnosed at an advanced stage, which limits the effectiveness of treatment and overall survival rates. There are various treatment modalities available for BC, with surgery being the primary curative option. Treatment options for breast cancer include hormone therapy, radiation, chemotherapy, surgery, targeted therapy, immunotherapy, bone-directed therapy, and clinical trials. Patients and healthcare teams collaborate to choose the best course of action. Surgery aims to achieve local control and prevent distant metastasis by removing the tumor and surrounding lymph nodes. Lymph nodes must be removed during surgery to prevent cancer from spreading, stage the illness, plan therapy options, lessen tumor burden, enhance treatment effectiveness, and improve patient outcomes. This proactive strategy improves long-term survival rates, eradicates cancer cells, and stops the illness from progressing.
Nevertheless, even with successful surgical resection, there remains a high risk of recurrence and metastasis. This is primarily due to BC’s invasive and metastatic nature, where tiny residual cancer cells may disseminate to other sites and form distant metastases, even in cases where the tumor has been completely excised locally [3, 4]. Hence, to reduce postoperative recurrence and improve survival rates, surgical treatment often needs to be combined with adjuvant therapies, including chemotherapy.
Chemotherapy, as a conventional adjuvant treatment for BC, utilizes chemical drugs to kill or inhibit the growth and spread of cancer cells, aiming to eliminate postoperative residual cancer cells, reduce metastasis, and improve survival rates [5]. Nevertheless, the use of chemotherapy drugs is also accompanied by a range of adverse reactions, such as nausea, vomiting, hair loss, fatigue, and others, which have negative impacts on patients’ physical and psychological well-being. In comprehensive BC treatment, the importance of psychological nursing is gradually being recognized. A key component of comprehensive breast cancer treatment is psychological nursing, which addresses emotional distress, encourages coping mechanisms, facilitates communication, supports collaborative decision-making, builds resilience, and improves survivor support – all of which contribute to improved quality of life and general well-being. BC patients often experience psychological issues, including anxiety, depression, fear, and body image disturbances, during surgery and chemotherapy processes [6, 7, 8]. These psychological problems not only affect patients’ quality of life (QoL) and psychological health but may also hurt treatment compliance and efficacy. Hence, in the comprehensive treatment of BC, implementing intervention measures that incorporate psychological nursing is of significant importance in improving patients’ psychological well-being and coping abilities and enhancing treatment outcomes [9, 10].
2. Literature review
Adopting psychological nursing in BC patients has been widely studied and validated. As breast cancer patients progress through the treatment process, psychological nursing interventions are beneficial, valuable, and helpful in enhancing their psychological well-being, coping mechanisms, and overall quality of life. Through means such as psychological support, cognitive-behavioral therapy, psychological counseling, and psychoeducation, psychological nursing can effectively assist patients in dealing with psychological distress during surgery and chemotherapy, alleviate anxiety, depression, and other negative emotions, and enhance patients’ psychological adaptation and QoL. Cancer patients may substantially affect their appetite and quality of life from their food, digestive system, and physical fitness. Nutritional assistance and symptom management are necessary when treating treatments that alter taste, restrict appetite, and create discomfort in the digestive system. Furthermore, psychological nursing can facilitate communication and support between patients and their families, establish a positive social support network, and provide comprehensive patient support and care [11, 12, 13].
In terms of pharmacotherapy, ondansetron, dexamethasone, and promethazine hydrochloride are commonly utilized and widely applied drugs in clinical practice. Ondansetron is a targeted therapy drug that inhibits hormone receptors on BC cells, thereby blocking hormone signaling and suppressing tumor growth [14, 15]. Chemotherapy-induced nausea and vomiting can be avoided using ondansetron, a serotonin 5-HT3 receptor antagonist, which blocks serotonin receptors in the brain. Contrarily, hormone receptor-targeted treatments function by obstructing the signaling pathways of cancer cells. Dexamethasone, a glucocorticoid, possesses anti-inflammatory, immunosuppressive, and anti-allergic properties, making it helpful in alleviating chemotherapy-related side effects and improving patients’ QoL [16, 17]. Promethazine hydrochloride, an antipsychotic medication, exhibits sedative, anti-anxiety, and antiemetic effects, providing control over chemotherapy-induced nausea and vomiting [18]. This study aims to analyze the safety, efficacy, and effects of the selective serotonin 5-HT3 receptor antagonist ondansetron on cancer patients. Thirteen of the twenty-three clinical trials found through a search focused on ondansetron’s ability to prevent chemotherapy-induced nausea and vomiting (CINV). The results demonstrate that ondansetron efficiently treats CINV, pointing to a notable advancement in treating CINV in adult cancer patients [19]. The Efficient e-Healthcare Risk Prediction for Health Big Data, which focuses on Licensed Medical Practitioners, achieves an accuracy range of 73.98% in prediction analysis. It has improved execution time from 29.95% to 36.05%, monogenic score to 19%, density accuracy range to 39%, and prediction accuracy to 45.9% [20]. The study [21] examines the use of solar and wind power for electricity generation, as well as issues such as fluctuation, expenses, and scattered energy sources. Using Artificial Neural Network-Based Expert Systems, it forecasts plants’ responses to temperature, light, and humidity. Fertilizer is used in the agricultural production system once plant resources have been depleted and are needed for plant growth. The results show that an equal contribution of wind and solar energy to the 50%-50s in the analysis can explain 96.9% of the variance in plant growth and development dependent on input factors. Despite the extensive use of these drugs in BC treatment, there needs to be more research on their combined effects with psychological nursing interventions in BC surgical patients undergoing chemotherapy. Hence, this work aimed to investigate the intervention effects of combining ondansetron, dexamethasone, promethazine hydrochloride, and psychological nursing in BC surgical patients undergoing chemotherapy, aiming to provide more effective strategies and guidance for comprehensive treatment of BC patients.
3. Materials and methods
3.1. Research objects
64 patients diagnosed with BC through pathological confirmation from October 2020 to May 2022 at The First People’s Hospital of Lianyungang Oncology Department were recruited. The age of the patients ranged from 24 to 62 years, with an average age of 42.8 5.1 years. They were randomly assigned into two groups, with 32 patients in each Group. The control group (group C) received the combination of ondansetron and routine psychological support and counseling treatment. In contrast, the intervention group (Group I) received a combination of ondansetron, dexamethasone, and promethazine hydrochloride, along with psychological nursing treatment.
Inclusion criteria: (1) BC patients aged between 18 and 65 years; (2) Pathologically confirmed diagnosis of BC; (3) Patients who underwent BC surgical treatment; (4) Patients requiring chemotherapy treatment; (5) Patients having the ability to undergo psychological assessment and comply with the research requirements. Physical side effects, psychological discomfort, financial strain, treatment logistics, social isolation, fear of failing, body image problems, and long-term adverse effects are just a few of the difficulties that chemotherapy patients must deal with. Managing these difficulties and preserving well-being require coping mechanisms, knowledge, and practical assistance. Combining therapies during chemotherapy can assist patients with breast cancer in many ways, including better treatment results, less psychological distress, improved quality of life, long-term survivor support, and health advantages. They enhance mental well-being, immunological function, and treatment tolerance.
Exclusion criteria: (1) Patients with other organic diseases (such as severe heart disease and hepatic dysfunction) or mental disorders (such as severe depression and schizophrenia); (2) Patients previously treated with ondansetron, dexamethasone, or promethazine hydrochloride; (3) Patients who have undergone chemotherapy previously; (4) Patients with pre-existing gastrointestinal symptoms such as nausea and vomiting before chemotherapy. Common side effects of chemotherapy include nausea and vomiting, which can impact individual reactions, gastrointestinal irritation, healthy cells, delayed gastric emptying, anxiety, and stomach irritation. Anti-nausea drugs, supportive care, and lifestyle changes are all necessary for effective treatment.
The research objectives, procedures, precautions, and the study’s legitimacy were explicitly explained to the patients during the study. In addition, the study participants agreed to sign an informed consent form with the consent of their family members. The implementation of this work had obtained approval from the Hospital Ethics Association (Approval No.: XXXXX). It had been ensured that no harm would be caused to the patients during the study. Furthermore, the obtained research subjects and confidential data were strictly confidential and would only be utilized for research purposes, not for any other purposes.
3.2. Therapeutic methodologies
Both groups of patients received the TAC (cyclophosphamide pirarubicin docetaxel) chemotherapy regimen. Patients with breast cancer who get combined intervention regimens may react differently than those who receive chemotherapy alone because they gain from enhanced psychological support, symptom management, comprehensive care, empowerment, and social interaction. The dosage for each drug was cyclophosphamide: 500 mg/m2, pirarubicin: 40 mg/m2, docetaxel: 75 mg/m2. The experiment was initiated at the second chemotherapy cycle (21 days/cycle) for both groups, and all chemotherapy treatments were completed before noon.
-
(1)
Group C received an intravenous infusion of ondansetron 8 mg per dose 30 minutes before and after chemotherapy. Standard psychological support and counseling were as follows: i. Information provision and education: detailed information about BC, the chemotherapy process, and potential side effects was provided to patients to help them understand and cope with the changes and challenges during treatment. ii. Emotional support: Active listening to and understanding patients’ emotional experiences offered emotional support and comfort. Patients were encouraged to express their emotions, and space was provided for emotional release. iii. Psychological education: patients were provided with relevant psychological knowledge and skills, such as coping with anxiety and stress, positive thinking, and relaxation training, to enhance their psychological coping abilities. Positive thinking and relaxation techniques improve patients’ psychological coping mechanisms by lowering stress, encouraging emotional control, and building resilience. This method boosts optimism, enhances quality of life, and gives patients more control. iv. Psychological support groups: psychological support groups were organized for BC patients, providing a platform for communication and sharing, allowing patients to support and encourage each other, and reducing feelings of loneliness and anxiety. Activities that involve psychological intervention and support groups encourage communication, sharing of experiences, and emotional openness among members, fostering a caring atmosphere that helps people feel understood, accepted, and in control of their healing. Trained facilitators provide psychological support groups for people with breast cancer, which provide a secure, controlled setting for sharing experiences, offering private peer support, and providing tools, connections, and coping mechanisms to improve well-being.
-
(2)
Group I received an intravenous infusion of ondansetron 8 mg per dose, dexamethasone 10 mg per dose, and an intramuscular injection of promethazine hydrochloride 25 mg per dose, 30 minutes before and after chemotherapy. Psychological care was as follows: i. Preliminary assessment: patients were initially assessed by professional psychological care providers to understand their psychological status, needs, and issues and to establish a good communication and trust relationship. ii. Individualized intervention plan: based on the assessment results and individualized needs of the patients, a specific psychological care intervention plan was formulated. Through individualized treatment, promotion of well-being, and assurance of cultural sensitivity, customized psychological care interventions can save healthcare costs while improving mental health outcomes, coping mechanisms, and participation. Counseling, support groups, cognitive-behavioral therapy, mindfulness exercises, psychoeducation, spiritual support, and family involvement are some of the psychological interventions included in the integrated treatment approach for breast cancer surgery. These interventions are intended to enhance emotional well-being, lessen distress, and improve treatment outcomes. This plan should include goal setting, intervention methodologies, and frequency. iii. Emotional management and coping skills: through cognitive-behavioral therapy, psychological support, and psychological education, patients were assisted in learning emotional management and coping skills to deal with anxiety, depression, fear, and other negative emotions. Establishing quantifiable, realistic, relevant, and time-bound goals, choosing intervention strategies, coordinating activities with objectives, carrying out frequent evaluations, and being adaptable to changes are all components of a SMART strategy for breast cancer patients’ support. This method aids in the development of practical approaches to psychological problems. iv. Relaxation training: patients were taught relaxation techniques such as deep breathing and progressive muscle relaxation to help alleviate anxiety and stress and enhance their ability to relax. Psychological support groups for people with breast cancer aim to reduce anxiety and loneliness by offering a safe space for experience sharing, promoting empathy, and building relationships among members. These groups provide social contact, coping mechanisms, and emotional support to enhance general well-being before and after treatment. In addition to being side-effect-free, progressive muscle relaxation (PMR) is an efficacious cancer therapy technique that empowers patients and enhances overall well-being by lowering stress, anxiety, depression, pain, sleep quality, and coping abilities. v. Psychological support and active listening: a safe environment was provided, patients’ inner experiences were actively listened to, their needs and concerns were understood, and emotional support and encouragement were provided. vi. Psychological education and information provision: patients were provided with relevant information and education regarding the chemotherapy process, side effect management, nutritional guidance, and lifestyle adjustments to help them better cope with the challenges during chemotherapy. vii. Psychological intervention and support groups: psychological intervention activities and support groups were organized to provide opportunities for collective psychological education and communication and promote patient interaction and support.
After chemotherapy was completed, both groups successfully underwent observation for gastrointestinal reactions in patients’ post-chemotherapy. Patients are observed for gastrointestinal side effects following chemotherapy to evaluate response to treatment, control side effects, avoid problems, and offer continuous care. This aids in the smooth transition from active treatment to post-treatment survivability and assists medical professionals in identifying side effects and disease recurrence.
3.3. Observation indexes and evaluation standard
-
(1)
Nausea and vomiting symptoms were graded according to the standards set by the World Health Organization (WHO) (Tables 1 and 2). Nausea and vomiting Grade 0 was defined as complete response (CR), indicating complete relief. Grade I was defined as partial response (PR), indicating partial relief (Table 3). The treatment response rate was calculated as (CRPR) divided by the total number of patients multiplied by 100%.
-
(2)
The self-rating anxiety scale (SAS) questionnaire was employed to assess the anxiety levels of the two patient groups. One popular self-report tool for determining anxiety levels is the Self-Rating Anxiety Scale (SAS). It comprises numerically scored standardized questions encompassing cognitive, psychological, and physiological symptoms. SAS has been translated into several languages, is suited for clinical practice, research, and screening programs, and is simple to administer. The SAS is a commonly utilized tool for anxiety assessment, designed to evaluate an individual’s anxiety level over a specific period. It is a self-report scale consisting of 20 items, each describing emotions and experiences related to anxiety. Participants select the answer that best reflects their feelings for each item, and scores are calculated based on the chosen responses. The total score typically ranges from 20 to 80, with higher scores indicating higher levels of anxiety in individuals.
-
(3)
Adverse events were monitored and recorded according to the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0, a widely utilized standard for assessing drug toxicity. The Common Terminology Criteria for Adverse Events (CTCAE), developed by the National Cancer Institute, is a standardized system that helps with clinical decision-making, communication, safety monitoring, and comparative analysis between studies and treatments by classifying and comparing adverse events during cancer treatment. The CTCAE provides a standardized grading system for categorizing and comparing the severity of adverse events that may occur during the treatment process. It classifies adverse events into various grades regarding their severity, ranging from Grade I to Grade IV, with higher grades indicating more severe adverse events. The CTCAE 4.0 version includes multiple types of adverse events, each with corresponding descriptions and grading criteria.
-
(4)
The Functional Living Index–Emesis (FLIE) scale is used to evaluate patients’ QoL related to nausea and vomiting during chemotherapy. A proven instrument for assessing how chemotherapy-induced nausea and vomiting affect patients’ quality of life is the Functional Living index-emesis (FLIE) scale. It offers information on the efficacy of therapy and patients’ general well-being through its Feeling and Functioning subscales. It is frequently used to track symptoms and provide supportive care in clinical and research contexts. The scale consists of 14 items, covering aspects such as appetite, diet, digestive issues, physical strength, emotions, and social functioning. Each item has specific descriptions and rating options, and participants select the answer that best reflects their situation and score accordingly. The total score typically ranges from 0 to 140, with higher scores indicating better QoL. For the FLIE scale, a score greater than 108 indicates a relatively good QoL for patients with nausea and vomiting during chemotherapy. This suggests fewer diet, digestion, physical strength, emotions, and social functioning issues, with less impact on appetite and overall QoL.
-
(5)
After completion of the chemotherapy cycles, a survey questionnaire was distributed to all patients to assess their satisfaction with the nursing care during the chemotherapy process. The survey was completed, and detailed records were kept. The calculation equation for satisfaction rate is (the number of highly satisfied participants the number of generally satisfied participants) divided by the total number of respondents, multiplied by 100%.
Table 1.
Classification of nausea symptoms
| Symptom | Level | Definition |
|---|---|---|
| No nausea | 0 | Do not feel nausea |
| Mild nausea | I | A mild feeling of nausea without causing vomiting |
| Moderate nausea | II | Noticeable nausea but not frequent vomiting |
| Severe nausea | III | Severe nausea, often accompanied by vomiting. |
Table 2.
Classification of vomiting symptoms
| Symptom | Level | Definition |
|---|---|---|
| No vomiting | 0 | No vomiting occurs |
| A little vomiting | I | Vomiting occurs 1–2 times a day |
| Moderate vomiting | II | Vomiting occurs 3–5 times a day |
| Severe vomiting | III | Vomiting occurs six or more times a day |
Table 3.
Evaluation of curative effect
| Symptom | Definition | |
|---|---|---|
| Complete remission | CR | No vomiting |
| Partial remission | PR | Vomiting 1–2 times/day |
| Lightly controlled | MR | Vomiting 3–5 times/day |
| Invalid | F | Vomiting 5 times/day |
3.4. Statistical analysis
Using SPSS 20.0, continuous data were denoted as mean standard deviation and categorical data were analyzed using the chi-square test for statistical inference, described in percentages or rates. In statistical inference, categorical data are analyzed using the chi-squared test. Several criteria need to be taken into account for it to be effective: the data must be categorical, the observations must be independent, the sample size must be sufficient, the expected cell frequencies must ideally be greater than 5, random sampling must be used, no cells must have zero counts, the data must be organized in a contingency table format, and the assumptions’ validity must be evaluated. The continuous data followed a normal distribution and were analyzed using the -test. A significance level of 0.05 was considered statistically significant.
4. Results
4.1. Comparison of general data
In Table 4, the age, course of disease, affected side, and pathological type differed inconsiderably between the two groups ( 0.05), indicating comparability.
Table 4.
Comparison of general data
| General information | Group C ( 32) | Group I ( 32) | |
| Age (years old) | 42.6 3.5 | 42.9 3.7 | 3.564 |
| The course of disease (years) | 3.8 0.4 | 3.9 0.3 | 2.248 |
| Affected side (left/right) | 20/12 | 18/14 | 3.193 |
| Invasive ductal carcinoma | 26 | 24 | – |
| Invasive lobular carcinoma | 4 | 5 | – |
| Intraductal carcinoma | 2 | 3 | – |
4.2. The treatment efficiency of nausea and vomiting in two groups
In Fig. 1, after treatment, group C had a nausea control effective rate of 59.37% (19/32), while Group I had a rate of 81.25% (26/32). Group I demonstrated a drastically superior nausea control effective rate versus group C ( 0.05). Similarly, in Fig. 2, after treatment, group C had a vomiting control effective rate of 65.62% (21/32), while Group I had a rate of 84.37% (27/32), which was markedly superior to group C ( 0.05).
Figure 1.

Comparison of therapeutic effects of nausea.
Figure 2.
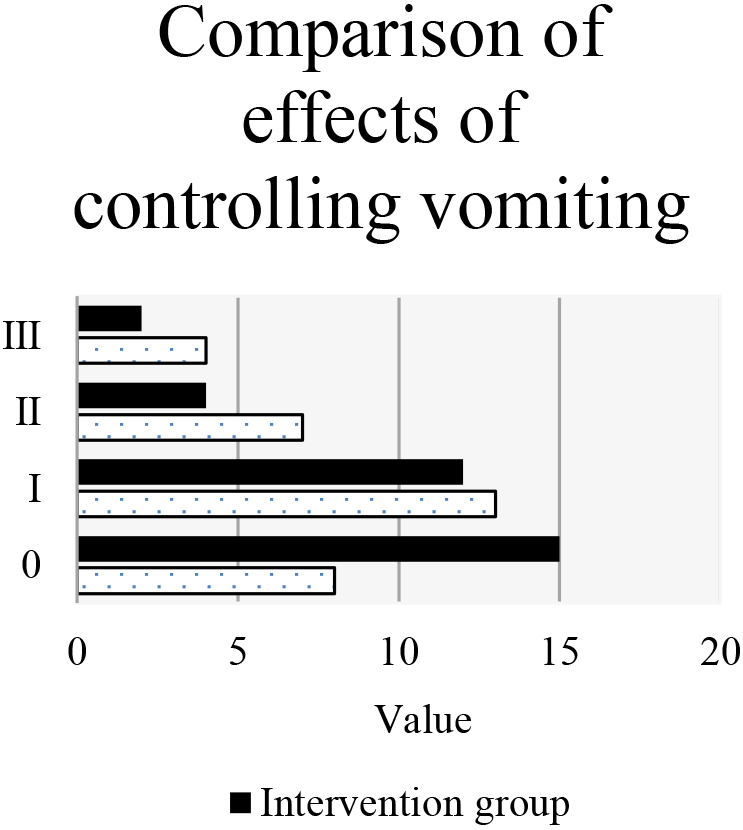
Comparison of therapeutic effects of vomiting.
4.3. The overall treatment response rate of the two groups
In Fig. 3, after treatment, group C had 7 cases with CR and 11 cases with PR, resulting in an overall treatment effective rate of 56.25% (18/32). On the other hand, Group I had 12 cases with CR and 13 cases with PR, resulting in an overall treatment effective rate of 78.12% (25/32). Group I demonstrated a higher overall treatment effective rate than group C ( 0.05).
Figure 3.

Comparison of overall treatment response rate.
4.4. Comparison of SAS scores
The management of symptoms, psychological health, adherence to therapy, patient involvement, and long-term symptom alleviation can all be improved by combining psychological nursing treatments with SAS scores. Relaxation methods, mindfulness-based stress reduction, and cognitive behavioral therapy assist patients in creating coping mechanisms, lessening the intensity of their symptoms, and enhancing their general quality of life. In Fig. 4, no significant difference was indicated in the SAS scores between Group C and Group I ( 0.05) before treatment. After treatment, the SAS score in Group C was 59.16 3.43, while in Group I, it was 51.33 3.25. Group I had a better SAS score than Group C, and the difference was substantial ( 0.05).
Figure 4.
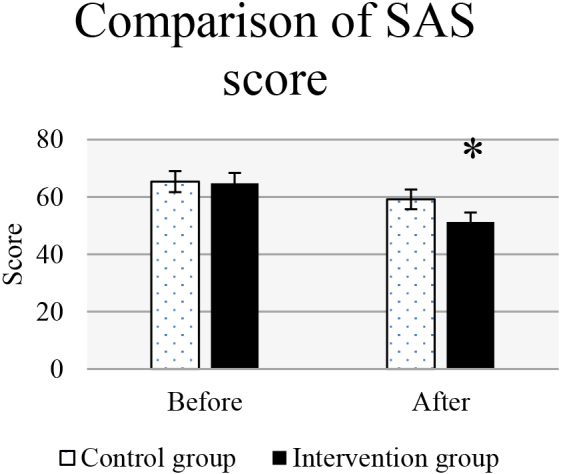
Comparison of SAS scores. Note: * 0.05 of SAS score vs. group C.
4.5. Comparison of white blood cell count
In Fig. 5, the white blood cell count differed inconsiderably between Group C and Group I ( 0.05) before treatment. After treatment, the white blood cell count in Group C was 2.58 1.26 (109/L), while in Group I, it was 3.76 1.31 (109/L). The white blood cell count in Group I was dramatically superior to that in Group C ( 0.05).
Figure 5.

Comparison of white blood cell count. Note: * 0.05 of white blood cell count vs. group C.
4.6. Comparison of adverse reactions
During the treatment process, adverse reactions experienced by the two groups of patients included dizziness, fatigue, insomnia, constipation, belching, and drowsiness. Fatigue and sleeplessness are common side effects of breast cancer therapy that have an impact on patient’s physical and mental health as well as their quality of life. Improving treatment experiences and long-term results requires addressing these side effects with supportive care and symptom management techniques. In Table 5, Group I had a markedly inferior incidence of dizziness (12.5%, 4/32) and constipation (15.62%, 5/32) versus Group C (21.87%, 7/32 and 31.25%, 10/32, respectively) ( 0.05). No grade III or IV reactions were observed in either Group. Regarding other adverse reactions, the differences were neglectable ( 0.05).
Table 5.
Comparison of adverse reactions
| Adverse reaction | Group C ( 32) | Group I ( 32) | ||||||
|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | I | II | III | IV | |
| Dizziness | 4 | 3 | 0 | 0 | 3 | 1 | 0 | 0 |
| Fatigue | 3 | 2 | 0 | 0 | 2 | 2 | 0 | 0 |
| Insomnia | 2 | 1 | 0 | 0 | 1 | 1 | 0 | 0 |
| Constipation | 6 | 4 | 0 | 0 | 3 | 2 | 0 | 0 |
| Hiccup | 3 | 1 | 0 | 0 | 1 | 1 | 0 | 0 |
| Somnolence | 2 | 1 | 0 | 0 | 2 | 1 | 0 | 0 |
4.7. Comparison of QoL scores
In Figs 6–7, the QoL for both groups of patients was assessed using the FLIE scale. In Group C, 24 cases (75%) scored above 108 points, while in Group I, 26 (81.25%) scored above 108. The difference was neglectable ( 0.05).
Figure 6.

Comparison of QoL scores in Group C.
Figure 7.
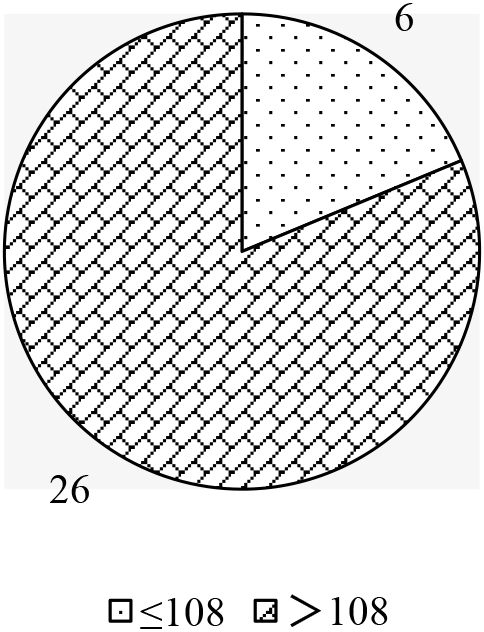
Comparison of QoL scores in Group I.
4.8. Comparison of nursing satisfaction
In Fig. 8, in terms of clinical nursing, in group C, 10 patients were delighted, 15 were generally satisfied, and 7 were dissatisfied. In contrast, 15 patients were delighted in Group I, 15 were typically happy, and 2 were dissatisfied. The nursing satisfaction rate in Group I (93.75%, 30/32) was considerably superior to that in Group C (78.12%, 25/32) ( 0.05).
Figure 8.

Comparison of nursing satisfaction.
5. Discussion
BC is a common malignancy, and combining chemotherapy with surgical treatment is a necessary choice to reduce recurrence and improve survival rates. Nevertheless, psychological issues during chemotherapy have adverse effects on patients’ mental health and QoL. This work aimed to explore the intervention effects of ondansetron, dexamethasone, and promethazine hydrochloride combined with psychological nursing in BC surgical patients undergoing chemotherapy to provide more effective strategies and guidance for the comprehensive treatment of BC and promote further advancements in BC therapy. To maximize therapeutic success, minimize toxicity, and enhance patient quality of life, breakthroughs in breast cancer treatment include personalized treatments, targeted immunotherapy, surgery, radiation therapy improvements, liquid biopsies, multidisciplinary care, and survivorship programs. 64 patients undergoing BC chemotherapy were enrolled and assigned to Group C. Group I. Group C received ondansetron combined with routine psychological support and counseling.
In contrast, Group I received ondansetron, dexamethasone, promethazine hydrochloride, and psychological nursing intervention. Psychological nursing is becoming more widely recognized because of its patient-centered care philosophy, emphasis on prevention and wellness, understanding the connection between mental and physical health, impact on treatment adherence and outcomes, and integration into primary care settings. Anxiety self-assessment scores, QoL scores, white blood cell counts, and occurrence of adverse reactions were assessed and compared between the two groups of patients.
The results indicated that during chemotherapy in BC surgical patients, the use of psychological nursing intervention combined with ondansetron, dexamethasone, and promethazine hydrochloride greatly enhanced the control rate of nausea and vomiting versus routine psychological support. Group I exhibited a notably superior treatment effectiveness rate for nausea and vomiting versus group C, suggesting that psychological nursing intervention has great clinical significance in the management of nausea and vomiting in BC patients undergoing chemotherapy. Gupta et al. (2021) [19] pointed out that cancer patients experience remarkable physiological and psychological effects from chemotherapy-induced nausea and vomiting. Severe symptoms can decrease patients’ QoL and may impede further treatment. The five significant forms of nausea and vomiting (acute, delayed, anticipatory, breakthrough, and refractory) require various treatment approaches. Despite extensive research and development of antiemetic drugs, the management of nausea and vomiting remains a significant challenge, with many unmet needs that require further attention and resolution. Nausea and vomiting are common side effects faced by chemotherapy patients, significantly impacting their QoL and treatment adherence. Through psychological nursing intervention, it is possible to effectively alleviate patients’ feelings of nausea and reduce the frequency of vomiting [23, 24]. In addition to assessing the control rate of nausea and vomiting, this work also observed the overall treatment effectiveness as an evaluation criterion. The results showed that Group I performed better than Group C regarding overall treatment effectiveness. This indicates that psychological nursing intervention not only improves patients’ symptoms of nausea and vomiting but may also have a positive impact on the efficacy of BC treatment. A possible explanation is that psychological nursing intervention can promote psychological stability in patients and enhance their confidence and adherence to treatment, thereby improving the overall treatment outcome [25, 26].
Ondansetron is primarily utilized for preventing chemotherapy-induced nausea and vomiting. By inhibiting the binding of neurokinin-1 (NK-1) receptors in the central and peripheral nervous systems, it reduces the stimulation of the chemoreceptor trigger zone by chemotherapy drugs, alleviating nausea and vomiting [27, 28]. Dexamethasone has anti-inflammatory, anti-allergic, and immunosuppressive effects. In the management of chemotherapy-induced nausea and vomiting (CINV), dexamethasone is often utilized in combination with other antiemetic drugs to enhance its antiemetic efficacy. Dexamethasone reduces nausea and vomiting by inhibiting inflammatory reactions and chemical releases. It also affects various receptors and pathways in the central nervous system, further alleviating nausea and vomiting symptoms [29]. Promethazine hydrochloride has sedative, anti-anxiety, and antiemetic effects. In the management of chemotherapy-induced nausea and vomiting, promethazine hydrochloride is commonly utilized as an adjuvant therapy. It alleviates nausea and vomiting symptoms by affecting the function of multiple neurotransmitter receptors, including dopamine and serotonin. Promethazine hydrochloride has been widely studied and applied in controlling nausea and vomiting, demonstrating specific therapeutic efficacy [30]. The combined use of these three drugs has a synergistic effect, allowing for more effective control of nausea and vomiting symptoms in BC chemotherapy patients.
Anxiety is one of the common psychological issues among BC patients during chemotherapy. In this work, before treatment, there were no considerable differences in the SAS scores between Group C and Group I, indicating that the two groups had similar initial levels of psychological status. Nevertheless, after treatment, the anxiety level (SAS score) of Group I was drastically inferior to that of Group C, indicating a marked alleviating effect of psychological nursing intervention on anxiety in BC chemotherapy patients. Psychological nursing interventions, through providing emotional support, coping strategies, and psychological education, help patients manage discomfort and stress during chemotherapy, enhance their psychological adaptation, and alleviate anxiety symptoms [31]. Currently, psychological education has become an effective tool for treating cancer patients and improving their psychological symptoms and QoL. Ghanbari et al. (2021) [32] conducted an experimental study investigating the impact of psychological education intervention on anxiety and self-esteem in cancer patients. The results demonstrated that psychological education intervention based on mobile adoptions played a crucial role in reducing anxiety and improving self-esteem in cancer patients.
Additionally, this work also observed that the white blood cell count of Group I was considerably superior to that of Group C. White blood cell count is a significant indicator of immune function, and for BC patients, maintaining immune system function is crucial for preventing infections and improving treatment outcomes. Psychological nursing interventions may improve white blood cell count by alleviating patients’ psychological stress and anxiety, thereby promoting the normal functioning of the immune system. This result further supports the positive role of psychological nursing in BC chemotherapy patients, benefiting their mental health and potentially exerting a positive influence on their overall physiological condition. Dizziness and constipation are common adverse reactions during BC chemotherapy. Dizziness may be associated with the impact of chemotherapy drugs on the central nervous system, while constipation may be related to the effects of chemotherapy drugs on intestinal function. The results indicated that psychological nursing interventions can effectively reduce the incidence of dizziness and constipation. Possible explanations are that psychological nursing interventions, by alleviating patients’ anxiety and stress and improving their emotional state, help relieve symptoms associated with dizziness and constipation. Patients’ well-being and treatment results are enhanced when they receive assistance in learning coping mechanisms and emotional regulation for anxiety and depression. In addition to improving quality of life and fostering social support and long-term psychological resilience, this also improves emotional resilience, lowers distress, increases treatment adherence, and facilitates communication. Additionally, psychological nursing interventions can provide nutritional guidance and lifestyle advice to help patients maintain healthy dietary and lifestyle habits, contributing to the alleviation of constipation symptoms.
Furthermore, neglectable differences were observed between the two groups regarding other adverse reactions in this work. This may be because psychological nursing interventions primarily target psychological issues during BC chemotherapy, and their impact on other adverse responses directly related to chemotherapy drugs may be limited. Nevertheless, further research is still needed to explore the potential effects of psychological nursing interventions on other adverse reactions. Based on the results of this work, Group I demonstrated significant advantages in terms of QoL scores and clinical nursing satisfaction for BC chemotherapy patients in certain aspects, which may be related to the medications utilized in Group I. Li et al. (2022) [33] evaluated the impact of psychological nursing interventions on inflammatory factors, negative emotions, and QoL in cancer patients. The patients who sought medical treatment at the Cancer Hospital of China Medical University were rolled into two groups according to the nursing approach. Group C received routine nursing care, while the experimental Group received appropriate psychological nursing interventions and routine care. Inflammatory factors (interleukin-6 (IL-6) and C-reactive protein (CRP)), negative emotions (self-rating depression scale (SDS) and SAS), and QoL (SF-36 questionnaire) were compared between the two groups. The results showed that the CRP, IL-6, SAS, and SDS differed slightly between the two groups before the intervention. After the intervention, patients in both groups showed improvement in bodily pain, physical limitations, vitality, emotional functioning, and overall health status. This indicates that psychological nursing intervention positively impacts inflammatory factors, negative emotions, and QoL in cancer patients. First, from the perspective of QoL scores, although both group C and group I achieved a certain level of scores (scores 108), a slight difference was indicated between the two groups. This suggests that the treatment provided in Group I did not significantly outperform Group C in overall QoL. This may be because the FLIE scale utilized to assess the QoL in BC chemotherapy patients may need to capture the advantages of Group I. Furthermore, the assessment of QoL is influenced by multiple factors, including psychological, social, and environmental factors. Nevertheless, this work only evaluated from the perspective of pharmacological intervention, which may have failed to reflect the advantages of Group I comprehensively. From the standpoint of clinical nursing satisfaction, Group I demonstrated notable advantages, with higher satisfaction in clinical nursing, which may be related to the medications utilized in Group I. In this work, Group I received medications such as ondansetron, dexamethasone, and promethazine hydrochloride, which not only have antiemetic effects but also alleviate other adverse reactions and provide more comprehensive nursing support. The combined use of these medications may provide patients with a better clinical nursing experience, positively influencing their satisfaction with nursing care. Through thorough analysis and evaluation of the efficacy and safety of these intervention measures, we can better understand the intervention effects of combining ondansetron, dexamethasone, and promethazine hydrochloride with psychological nursing in chemotherapy for BC patients. This will help provide more comprehensive and personalized treatment plans for clinical practice, improving the overall treatment outcomes and QoL for BC patients.
6. Conclusion
The purpose of this work was to evaluate the intervention effects of psychological nursing combined with ondansetron, dexamethasone, and promethazine hydrochloride on BC chemotherapy patients. The experiment found that this treatment regimen significantly improved nausea and vomiting control effectiveness in BC chemotherapy patients, mitigated some adverse reactions, and achieved high nursing satisfaction. Nevertheless, the limitations of this work include a relatively small sample size, which may affect the stability of the results. Further large-scale studies are still needed to confirm these findings. The assessment of QoL was solely conducted from the perspective of pharmacological intervention, failing to comprehensively reflect the advantages of Group I. Future research could adopt a multicenter and large-sample study design, incorporating more assessment tools and indicators, such as psychological, social, and environmental factors, to comprehensively evaluate the QoL and clinical nursing satisfaction of BC chemotherapy patients. In conclusion, the findings of this work have important clinical significance and value, providing references for clinical physicians in the management of nausea and vomiting and nursing care during BC chemotherapy.
Funding
The authors did not receive any funding.
Data availability
Statement: No datasets were generated or analyzed during the current study.
Code availability
Not applicable.
Author contributions
Xia Li is responsible for designing the framework, analyzing performance, validating the results, and writing the article. Lili Dong is responsible for collecting the information required for the framework, providing software, conducting critical reviews, and administering the process.
Conflict of interest
Authors do not have any conflicts.
References
- [1]. Hanker AB, Sudhan DR, Arteaga CL. Overcoming Endocrine Resistance in Breast Cancer. Cancer Cell. 2020. Apr 13; 37(4): 496-513. doi: 10.1016/j.ccell.2020.03.009. PMID: 32289273; PMCID: PMC7169993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2]. Burstein HJ, Curigliano G, Thürlimann B, Weber WP, Poortmans P, Regan MM, Senn HJ, Winer EP, Gnant M. Panelists of the St Gallen Consensus Conference. Customizing local and systemic therapies for women with early breast cancer: the St. Gallen International Consensus Guidelines for treatment of early breast cancer 2021. Ann Oncol. 2021. Oct; 32(10): 1216-1235. doi: 10.1016/j.annonc.2021.06.023. Epub 2021 Jul 6. PMID: 34242744; PMCID: PMC9906308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3]. Wilkinson L, Gathani T. Understanding breast cancer as a global health concern. Br J Radiol. 2022. Feb 1; 95(1130): 20211033. doi: 10.1259/bjr.20211033. Epub 2021 Dec 14. PMID: 34905391; PMCID: PMC8822551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Kashyap D, Pal D, Sharma R, Garg VK, Goel N, Koundal D, Zaguia A, Koundal S, Belay A. Global Increase in Breast Cancer Incidence: Risk Factors and Preventive Measures. Biomed Res Int. 2022. Apr 18; 2022: 9605439. doi: 10.1155/2022/9605439. PMID: 35480139; PMCID: PMC9038417. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [5]. Montemurro F, Nuzzolese I, Ponzone R. Neoadjuvant or adjuvant chemotherapy in early breast cancer? Expert Opin Pharmacother. 2020. Jun; 21(9): 1071-1082. doi: 10.1080/14656566.2020.1746273. Epub 2020 Apr 1. PMID: 32237920. [DOI] [PubMed] [Google Scholar]
- [6]. Iwamoto T, Kajiwara Y, Zhu Y, Iha S. Biomarkers of neoadjuvant/adjuvant chemotherapy for breast cancer. Chin Clin Oncol. 2020. Jun; 9(3): 27. doi: 10.21037/cco.2020.01.06. Epub 2020 Mar 13. PMID: 32192349. [DOI] [PubMed] [Google Scholar]
- [7]. Keenan TE, Tolaney SM. Role of Immunotherapy in Triple-Negative Breast Cancer. J Natl Compr Canc Netw. 2020. Apr; 18(4): 479-489. doi: 10.6004/jnccn.2020.7554. PMID: 32259782. [DOI] [PubMed] [Google Scholar]
- [8]. Provenzano E. Neoadjuvant Chemotherapy for Breast Cancer: Moving Beyond Pathological Complete Response in the Molecular Age. Acta Med Acad. 2021. Apr; 50(1): 88-109. doi: 10.5644/ama2006-124.328. PMID: 34075766. [DOI] [PubMed] [Google Scholar]
- [9]. Tsai PL, Kuo TT, Ku CH, Liao GS, Lin CK, Pan HH. Self-Esteem as a Predictor of Mental Adjustment in Patients with Breast Cancer. Int J Environ Res Public Health. 2021. Nov 29; 18(23): 12588. doi: 10.3390/ijerph182312588. PMID: 34886314; PMCID: PMC8656551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10]. Koç Z, Kaplan E, Tanrıverdi D. The effectiveness of telehealth programs on the mental health of women with breast cancer: A systematic review. J Telemed Telecare. 2022. Feb 2: 1357633X211069663. doi: 10.1177/1357633X211069663. Epub ahead of print. PMID: 35108131. [DOI] [PubMed] [Google Scholar]
- [11]. Alam MZB, Hia MS, Gidron Y, Al-Hakeem M. Mental health care of patients with breast cancer in Bangladesh. Lancet Psychiatry. 2021. Jan; 8(1): 18-19. doi: 10.1016/S2215-0366(20)30494-6. PMID: 33341163. [DOI] [PubMed] [Google Scholar]
- [12]. Zheng L, Jin Q. Roy adaptation model-based nursing diagnosis and implementation reduces the sense of shame and enhances nursing outcomes in female patients with breast cancer. Am J Transl Res. 2022. Aug 15; 14(8): 5520-5528. PMID: 36105053; PMCID: PMC9452335. [PMC free article] [PubMed] [Google Scholar]
- [13]. Hulett JM, Johnstone B, Millspaugh RJ, Millspaugh JJ. Personality and Spirituality as Predictors of Mental Health and Salivary Alpha-Amylase Activity in Breast Cancer Survivors. Oncol Nurs Forum. 2022. Jun 17; 49(4): 307-314. doi: 10.1188/22.ONF.307-314. PMID: 35788735. [DOI] [PubMed] [Google Scholar]
- [14]. Hsiung E, Celebioglu A, Emin Kilic M, Durgun E, Uyar T. Ondansetron/Cyclodextrin inclusion complex nanofibrous webs for potential orally fast-disintegrating antiemetic drug delivery. Int J Pharm. 2022. Jul 25; 623: 121921. doi: 10.1016/j.ijpharm.2022.121921. Epub 2022 Jun 15. PMID: 35714816. [DOI] [PubMed] [Google Scholar]
- [15]. Dey S, Chanu SM, Dev P, Borthakur M, Karim HMR, Yunus M. Antiemetic Efficacy of Palonosetron Compared with the Combination of Ondansetron and Dexamethasone for Prevention of Postoperative Nausea and Vomiting in Patients Undergoing Laparoscopic Gynaecological Surgery. Rom J Anaesth Intensive Care. 2022. Sep 25; 28(1): 19-24. doi: 10.2478/rjaic-2021-0003. PMID: 36846536; PMCID: PMC9949011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16]. Barden A, Phillips M, Mas E, Hill LM, Mowat I, Loh PS, Corcoran T, Mori TA. Effects of antiemetic doses of dexamethasone on plasma mediators of inflammation resolution and pain after surgery in women. Prostaglandins Other Lipid Mediat. 2020. Aug; 149: 106427. doi: 10.1016/j.prostaglandins.2020.106427. Epub 2020 Feb 19. PMID: 32084530. [DOI] [PubMed] [Google Scholar]
- [17]. Klag EA, Kuhlmann NA, Tramer JS, Franovic S, Muh SJ. Dexamethasone decreases postoperative opioid and antiemetic use in shoulder arthroplasty patients: a prospective, randomized controlled trial. J Shoulder Elbow Surg. 2021. Jul; 30(7): 1544-1552. doi: 10.1016/j.jse.2020.12.005. Epub 2021 Jan 22. PMID: 33486058. [DOI] [PubMed] [Google Scholar]
- [18]. Salama AH, Elmotasem H, Salama AAA. Nanotechnology based blended chitosan-pectin hybrid for safe and efficient consolidative antiemetic and neuro-protective effect of meclizine hydrochloride in chemotherapy induced emesis. Int J Pharm. 2020. Jun 30; 584: 119411. doi: 10.1016/j.ijpharm.2020.119411. Epub 2020 May 8. PMID: 32423876. [DOI] [PubMed] [Google Scholar]
- [19]. Ashour AM. The preventive effects of ondansetron on chemotherapy-induced nausea and vomiting in adult cancer patients: systematic review from ClinicalTrials. gov. Frontiers in Pharmacology, 2023; 14, 1310455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20]. Sathyaprakash P, Alagarsundaram P, Devarajan MV, Alkhayyat A, Poovendran P, Rani DR, Savitha V. Medical Practitioner-Centric Heterogeneous Network Powered Efficient E-Healthcare Risk Prediction On Health Big Data. International Journal of Cooperative Information Systems, 2024. [Google Scholar]
- [21]. Kumar PM, Kamruzzaman MM, Alfurhood BS, Hossain B, Nagarajan H, Sitaraman SR. Balanced Performance Merit On Wind and Solar Energy Contact With Clean Environment Enrichment. IEEE Journal of the Electron Devices Society, 2024. [Google Scholar]
- [22]. Gupta K, Walton R, Kataria SP. Chemotherapy-Induced Nausea and Vomiting: Pathogenesis, Recommendations, and New Trends. Cancer Treat Res Commun. 2021; 26: 100278. doi: 10.1016/j.ctarc.2020.100278. Epub 2020 Dec 11. PMIDs: 33360668. [DOI] [PubMed] [Google Scholar]
- [23]. Shirley M. Netupitant/Palonosetron: A Review in Chemotherapy-Induced Nausea and Vomiting. Drugs. 2021. Jul; 81(11): 1331-1342. doi: 10.1007/s40265-021-01558-2. Epub 2021 Jul 22. Erratum in: Drugs. 2021 Oct; 81(15): 1817. PMID: 34292534; PMCID: PMC8463343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24]. Toniolo J, Delaide V, Beloni P. Effectiveness of Inhaled Aromatherapy on Chemotherapy-Induced Nausea and Vomiting: A Systematic Review. J Altern Complement Med. 2021. Dec; 27(12): 1058-1069. doi: 10.1089/acm.2021.0067. Epub 2021 Jul 20. PMID: 34283916. [DOI] [PubMed] [Google Scholar]
- [25]. Nakamura ZM, Damone EM, Herrick HP, Nyrop KA, Deal AM, Brenizer AT, Muss HB. Anticipating mental health needs after chemotherapy in early-stage breast cancer using patient-reported symptom screening. Support Care Cancer. 2022. May; 30(5): 3933-3941. doi: 10.1007/s00520-022-06827-8. Epub 2022 Jan 19. PMID: 35044483; PMCID: PMC8957600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26]. Mou J, Zheng S. Effects of ADOPT-Based Breathing Training Combined with Continuous Nursing on Quality of Life, Mental Health, and Self-Efficacy in Lung Cancer Patients Undergoing Chemotherapy: Based on a Retrospective Cohort Study. Comput Math Methods Med. 2022. Apr 20; 2022: 4164771. doi: 10.1155/2022/4164771. PMID: 35495891; PMCID: PMC9046005. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [27]. Vimolchalao V, Sakdejayont S, Wongchanapai P, Sukprakun S, Angspatt P, Thawinwisan W, Chenaksara P, Sriuranpong V, Vinayanuwatikun C, Parinyanitikun N, Poovorawan N, Tanasanvimon S. The efficacy and safety of the addition of olanzapine to ondansetron and dexamethasone for prevention of chemotherapy-induced nausea and vomiting in patients receiving highly emetogenic chemotherapy. Int J Clin Oncol. 2020. Feb; 25(2): 396-402. doi: 10.1007/s10147-019-01570-3. Epub 2019 Nov 27. PMID: 31776732. [DOI] [PubMed] [Google Scholar]
- [28]. Ithimakin S, Theeratrakul P, Laocharoenkiat A, Nimmannit A, Akewanlop C, Soparattanapaisarn N, Techawattanawanna S, Korphaisarn K, Danchaivijitr P. Randomized, double-blind, placebo-controlled study of aprepitant versus two dosages of olanzapine with ondansetron plus dexamethasone for prevention of chemotherapy-induced nausea and vomiting in patients receiving high-emetogenic chemotherapy. Support Care Cancer. 2020. Nov; 28(11): 5335-5342. doi: 10.1007/s00520-020-05380-6. Epub 2020 Mar 4. PMID: 32128615. [DOI] [PubMed] [Google Scholar]
- [29]. Huang G, Huang J, Zhang Z, Xue C, Liu Y. Nivolumab plus gemcitabine, dexamethasone, and cisplatin chemotherapy induce durable complete remission in relapsed/refractory primary mediastinal B-cell lymphoma: a case report and literature review. J Int Med Res. 2020. Aug; 48(8): 300060520945075. doi: 10.1177/0300060520945075. PMID: 32783492; PMCID: PMC7425276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30]. Barney EZ, Fuller ME, Habib AS. Comparison of metoclopramide and promethazine for the treatment of postoperative nausea and vomiting in the post-anesthesia care unit: A retrospective database analysis. J Clin Anesth. 2020. Mar; 60: 47-48. doi: 10.1016/j.jclinane.2019.08.012. Epub 2019 Aug 20. PMID: 31442860. [DOI] [PubMed] [Google Scholar]
- [31]. Saraiva S, Bachmann M, Andrade M, Liria A. Bridging the mental health treatment gap: effects of a collaborative care intervention (matrix support) in the detection and treatment of mental disorders in a Brazilian city. Fam Med Community Health. 2020. Sep; 8(4): e000263. doi: 10.1136/fmch-2019-000263. PMID: 32958519; PMCID: PMC7507894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32]. Ghanbari E, Yektatalab S, Mehrabi M. Effects of Psychoeducational Interventions Using Mobile Apps and Mobile-Based Online Group Discussions on Anxiety and Self-Esteem in Women With Breast Cancer: Randomized Controlled Trial. JMIR Mhealth Uhealth. 2021. May 18; 9(5): e19262. doi: 10.2196/19262. PMID: 34003138; PMCID: PMC8170553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33]. Li M, Xie X, Xu H, Li H. A Psychological Nursing Intervention for Patients with Breast Cancer on Inflammatory Factors, Negative Emotions and Quality of Life. Iran J Public Health. 2022. Sep; 51(9): 2041-2047. doi: 10.18502/ijph.v51i9.10559. PMID: 36743364; PMCID: PMC9884377. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Statement: No datasets were generated or analyzed during the current study.


