Abstract
Objective:
This meta-analysis aimed to investigate daily versus intermittent iron supplementation among children.
Methods:
The author searched the Cochrane Library, PubMed, Medline, and Google Scholar for randomized controlled trials and compared daily versus intermittent iron supplementation. The keywords iron deficiency anemia, iron therapy, daily, twice per week, and once weekly were used. The search was limited to the period January 2012 up to November 2023. The age of participant range from two months to 18 years.
Result:
Out of the 735 studies, 540 were eligible after removal of duplication, of them, 28 full texts were screened and only 10 studies were included. Daily iron supplementation was better in improving hemoglobin odd ratio, 0.41, 95 CI, 0.38-0.44, Z=26.53, and p-Value <0.001 than intermittent prescription odd ratio, 0.69, 95 CI, 0.67-0.72, Z=49.98, and P-value < 0.001.
Conclusion:
Daily supplementation increased hemoglobin more compared to weekly or twice/week among children with iron deficiency anemia. Further larger studies assessing tolerance and compliance are needed.
KEYWORDS: Iron supplementation, Daily, Intermittent, Children, Iron deficiency anemia
INTRODUCTION
Iron deficiency anemia is the most common cause of anemia in the world. One-third of people worldwide suffer from anemia, with iron deficiency accounting for half of the instances.1,2 An estimated 273 million children under the age of five were anemic worldwide in 2011, with iron deficiency being the cause of roughly half of those instances.3 There have been reports of IDA prevalence in Saudi Arabia ranging from 10% to 60% overall.4
The symptoms of iron deficiency anemia in children are feeling exhausted, and weak, experiencing lightheadedness and dizziness, having trouble focusing and remembering things, and performing poorly at school. In addition, to negative immune system effects. In more extreme situations, the requirement to raise cardiac output results in palpitations and dyspnea.5 Moreover, iron deficiency anemia stunted children’s psychomotor development.6
Diagnosis of iron deficiency anemia depends on a complete blood count to determine the hemoglobin and the mean corpuscular volume; microcytic anemia is highly suspicious with ferritin levels below the normal range confirming the diagnosis.7 Management of IDA is by iron supplement either oral or intravenous, the dose of oral iron therapy varies from 3 to 6 mg/kg/day, and the frequency is either daily, twice per week, or weekly to avoid side effects and for a better complaint.8
The first three years of life are critical for organ development including the brain, iron stores are important for biochemical reactions and organ development.9 Evidence from human and animal studies confirmed that brain iron deficiency occurs before red blood cells.10 Importantly, brain iron deficiency in childhood negatively impacts brain function in adult life, poor academic achievement, lower job opportunities, and psychiatric diseases.11
Daily iron supplementation is recommended after six months of age depending on the geographical location and the prevalence of iron deficiency.12 However, adherence issues and the fact that gastrointestinal cells are renewed every five to six days with poor absorption of irons. Therefore, intermittent iron supplementation was suggested to overcome non-compliance and enhance iron absorption.13
Intermittent versus daily iron supplementation was assessed in pregnant women.14,15 Literature regarding the effects of intermittent versus daily iron supplementation in children is scarce. Therefore, the current review aimed to compare Hemoglobin levels after three months of daily, twice-per-week, and once-weekly oral iron therapy.
METHODS
Eligibility Criteria according to Population, Intervention, Comparison, Outcomes and Study PICOS:
This meta-analysis was conducted during November and December 2023, the PRISMA guidelines were strictly followed.
Inclusion criteria:
We considered whether the investigations were prospective or retrospective cohorts, case-control, cross-sectional, or randomized controlled trials (RCTs). Studies that reported oral iron therapy once a day, twice a week, or weekly were eligible. Randomized controlled trials assessing iron supplementation (supervised and unsupervised) among children were included. Simple random technique was considered for the included studies.
Exclusion criteria:
Prospective or retrospective cohorts, case-control, cross-sectional, animal research, case reports, case series, protocols without data, and systematic reviews and meta-analyses were not pursued. Patients belonging to specific sub-groups and those with any chronic disease were not included. The study duration of less than four weeks, and studies conducted among adults were not eligible.
Outcome measures:
Hemoglobin increment after oral iron therapy where is it once daily, twice per week, or once weekly?
Information sources and search:
We searched the Cochrane Library, PubMed, Medline, and Google Scholar. The search was conducted during November and December 2023 and was limited to the period January 2012 up to November 2023. The search was limited to articles published in the English language. The keywords iron deficiency anemia, iron therapy, daily, twice per week, and once weekly were used. Out of the 735 studies, 540 were eligible after removal of duplication, of them, 28 full texts were screened and only 10 studies were included in the final analysis.
Data extraction:
An Excel sheet detailing the author’s name, year of publication, number of patients, and the increment of hemoglobin level in various frequencies used daily, twice per week, or once weekly was used. A modified Cochrane Risk of Bias (ROB-2) assessed the quality of the included study.16 Fig.1 and Tables-I and II.
Fig.1.
Daily versus weekly iron supplementation (the PRISMA Chart).
Table-I.
Randomized trials investigating daily versus intermittent iron supplementation among children with iron deficiency anemia.
| Author name | Age year | Duration of study | Does daily vs intermittent | Gender girl % daily vs intermittent | Country | Daily g/dL | Twice/week | Weekly |
|---|---|---|---|---|---|---|---|---|
| Berger et al. 199717 | 3.3-8.3 | 16 weeks | 3-4 mg /kg of elemental iron | 53.4 vs 48.3 | Bolivia | 1.86±0.59/58 | - | 1.52±0.17/58 |
| Faqih et al. 200618 | 2-6 | 12 weeks | 5 mg/kg ferrous sulfated | 38 vs 42.8 | Jordon | 2.47 ± 0.17/21 | 2.12 ± 0.18/21 | 2.18 ± 0.18/21 |
| Hyder et al. 200719 | 1-2 | 8 weeks | 12.5 mg vs 30 mg elemental iron | 47.1 vs 47 | Bangladesh | 1.61±1.32/70 | - | 1.23±1.33/66 |
| Kapil et al. 201320 | 3-5 | 14 weeks | 20-40 vs 40mg iron | - | India | 1.5±0.3/226 | - | 0.6±0.1/110 |
| Khademloo et al. 200921 | 0.5-2 | 12 weeks | 15 vs 30 drops of iron | 50 | Iran | 0.6±0.17/50 | - | 0.4±0.33/50 |
| Siddiqui et al. 200422 | 5-10 | 8 weeks | 200 mg ferrous sulfate | 50 | Pakistan | 2.5±0.3/30 | - | 2.02±0/30 |
| Sungthong et al. 200223 | 6 -13 | 16 weeks | 60 mg of elemental iron | 50 vs 52. | Thailand | 6.5±6.0/39 | - | 5.7± 6.3/40 |
| Desai et al. 200424 Unsupervised | 2-59 m | 12 weeks | 3-6 mg/kg vs 6-12 mg/kg ferrous sulfate | 51 vs 49 | USA | 0.82±0.2/251 | 0.47±0.21/271 | - |
| Desai et al. 200424 supervised | 2-59 m | 12 weeks | 3-6 mg/kg vs 6-12 mg/kg ferrous sulfate | 46 vs 51 | USA | 1.15±0.2/261 | 0.59±0.21/266 | - |
| Gunadi et al. 200925 | 9-12 | 4 weeks | 5 mg/kg/day elemental iron | 54.7 vs 47.2 | Indonesia | 4.81±0.59/50 | 2.26±0.02/47 | - |
| Zavaleta et al. 200026 | 12-18 | 17 weeks | 60 mg ferrous sulfate | 100 | Peru | 1.11±0.9/20 | 0.68±0.8/18 | - |
Table-II.
Risk of bias assessment of the included studies according to Cochrane risk of bias of randomized controlled trials.
| Author | Selection bias1 | Selection bias2 | detection | Attrition bias | Reporting bias | Other bias |
|---|---|---|---|---|---|---|
| Berger et al.199717 | Unknown | Low | Low | Low | Unknown | Low |
| Faqih et al.200618 | Low | Unknown | High | High | High | High |
| Hyder et al.200719 | Low | Low | Unknown | Unknown | Low | Low |
| Kapil et al.201320 | Low | Low | Unknown | Unknown | Low | Unknown |
| Khademloo et al.200921 | Unknown | Unknown | High | Unknown | Unknown | Low |
| Siddiqui et al.200422 | Unknown | Unknown | High | Low | Unknown | Unknown |
| Sungthong et al.200223 | Low | Low | Low | Low | Unknown | Unknown |
| Desai et al.200424 Unsupervised | Low | Low | High | Low | Unknown | Unknown |
| Desai et al.200424 supervised | Low | Low | High | Low | Unknown | Unknown |
| Gunadi et al.200925 | Low | Low | High | Unknown | Unknown | Unknown |
| Zavaleta et al.200026 | Low | Low | low | Low | Unknown | Low |
Data analysis:
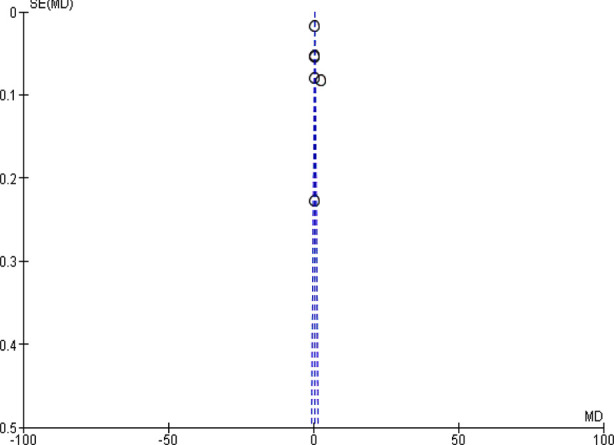
The data were all continuous and were processed using the RevMan meta-analysis tool (version, 5.4,1, United Kingdom). For the continuous data, a 95% CI of 5% was used. Depending on the degree of heterogeneity, either the fixed effect or the random effect was applied. Sensitivity analysis was done by removing studies with a high risk of bias. The assessment of lateralization was done using Funnel plots. The p-Values <less 0.05 were regarded as significant.
RESULTS
Characteristics of the included studies:
We included 10 clinical trials; two were from South America, seven from Asia, and one from USA.
Findings:
In this meta-analysis, seven unsupervised studies including 1073 children were pooled.17-23 Daily iron supplementation was better than intermittent in improving hemoglobin, odd ratio, 0.41, 95 CI, 0.38-0.44, Z=26.53, and p-value <0.001. The Chi-square=686.14. A significant heterogeneity was found, I2=99%, p-value for heterogeneity <0.001, and the standard difference = 5. Fig.2.
Fig.2.
Daily versus weekly iron supplementation in children with iron deficiency anemia (unsupervised).
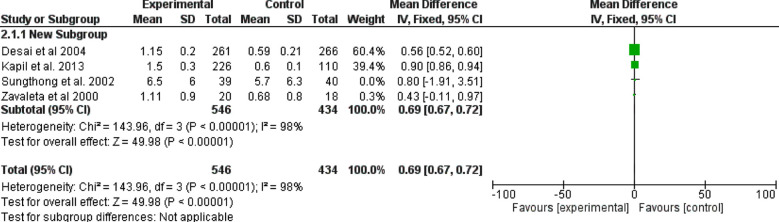
Four studies (980 children included) assessed the difference between daily and intermittent supervised iron supplementation.18,24-26 They showed that daily iron supplementation was better, with odd ratio, 0.69, 95 CI, 0.67-0.72, Z=49.98 and p-value ≤ 0.001. The Chi-square=143.96. A significant heterogeneity was found, I2=98%, p-value for heterogeneity <0.001. Fig.3.
Fig.3.
Daily versus intermittent iron supplementations (supervised).

DISCUSSION
The current findings showed that daily iron supplementation was superior to twice/week, and weekly iron supplementation, odd ratio, 0.41, 95 CI, 0.38-0.44, Z=2.15 and p-value < 0.001, A sub-analysis including only supervised iron supplementation confirmed the same, odd ratio, 0.69, 95 CI, 0.67-0.72, Z=49.98 and p-value < 0.001. Previous meta-analyses conducted in children showed the benefit of daily iron supplementation on hemoglobin levels with limited evidence on adherence, side effects, and clinical outcomes.27-29
The available studies assessed the effects of daily iron supplementation, however, meta-analyses comparing daily, and intermittent iron supplementation are scarce. De-Regil et al30 compared daily iron supplementation versus placebo and intermittent supplementations. The study included children with and without anemia. Importantly, the authors included only six studies comparing daily versus intermittent intake. In addition, the study was published in the year 2011 and new trials were published.20,31 therefore, an update is justifiable.
A recent meta-analysis included 129 trials and showed similar effects of frequent and intermittent iron supplementation in contradiction to the current findings.32 However, the authors searched the literature up to 2020 and the significant heterogeneity limited their conclusions. In addition, the author included folate supplementation, indicators of infection, and child development. The contradicting findings might have been explained by the fact that Andersen compared 1-2/week versus 3-7/week a frequency that is not so different.
The World Health Organization recommended supplementation of iron in regions with a high prevalence of iron deficiency anemia.33 However, gastrointestinal side effects of iron are a major challenge.33 Our findings supported the previous finding that daily iron supplementation was better than infrequent iron therapy. However, intermittent iron supplementation is an effective alternative. There is existing evidence that gastrointestinal cells renewed every six days.
Therefore, daily, or twice weekly supplementation bears the advantage of more tolerance and lower side effects.34 New iron formulations with few gastrointestinal side effects might solve the problem of intolerance.35 An interesting finding of reduced iron transportation from the gastrointestinal tract to the blood following larger doses of iron, pointed to the importance of doses of iron prescription.36 This meta-analysis included an up-to-date and larger number of randomized trials and showed the superiority of daily iron supplementation compared to intermittent schedules. In addition, the current findings were different from the previous studies that showed similar efficacy of daily and intermittent prescriptions.31,32
International organizations stated that supervised iron supplementation could be a better strategy than unsupervised recommendations in reducing anemia among children. In addition, more research is suggested to compare biweekly supervised iron supplementation with the loose strategy of recommending 100 days/year of continuous dosing.37 In the current meta-analysis, we assessed both supervised and unsupervised iron supplementation and both were shown to be effective.
Although iron supplementation was effective in the reduction of anemia. However, neurodevelopmental issues, interaction with other trace elements, increased incidence of infection, and gut microbiota disturbance are major concerns38 excess iron competes with trace elements absorption and masks zinc and copper deficiency.39 Importantly, iron supplementation for prevention and in areas of low iron deficiency might lead to cell death, organ damage, and mortality. Iron overload leads to high oxygen free radicals and oxidative stress inducing oxidation of lipids, proteins, and DNA leading to cell death (ferroptosis).40 In addition, iron deposits in the gastrointestinal tract lead to gut dysbiosis with the abundance of Escherichia/Shigella, and Clostridium, and reduction of Bifidobacterium infantis. The above results in microbiota shift and infections.41,42
Limitation
It includes the short duration of the trials included and the high heterogeneity observed.
CONCLUSION
Daily iron supplementation is better than the weekly and twice/week approach among children with iron deficiency anemia. The results remain robot after assessing only supervised iron therapy.
Footnotes
Recommendations: Pediatricians should prescribe daily iron supplementation rather than intermittent for children with iron deficiency anemia. Further larger randomized controlled trials investigating the effects of iron supplementation on iron-deficient children and reporting the effects on the gut Microbiota are suggested.
Source of Funding: None.
Conflicts of Interest: None.
REFERENCES
- 1.Lopez A, Cacoub P, Macdougall IC, Biroulet PL. Iron deficiency anaemia. Lancet. 2016;387:907–916. doi: 10.1016/S0140-6736(15)60865-0. doi:10.1016/S0140-6736(15)60865-0. [DOI] [PubMed] [Google Scholar]
- 2.Sundararajan S, Rabe H. Prevention of iron deficiency anemia in infants and toddlers. Pediatr Res. 2021;89:63–73. doi: 10.1038/s41390-020-0907-5. doi:10.1038/s41390-020-0907-5. [DOI] [PubMed] [Google Scholar]
- 3.Owaidah T, Numair AN, Suliman A, Zolaly M, Hasanato R, Zahrani AF, et al. Iron Deficiency and Iron Deficiency Anemia Are Common Epidemiological Conditions in Saudi Arabia:Report of the National Epidemiological Survey. Anemia. 2020;2020:6642568. doi: 10.1155/2020/6642568. doi:10.1155/2020/6642568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Falkingham M, Abdelhamid A, Curtis P, Tait FS, Dye L, Hooper L, et al. The effects of oral iron supplementation on cognition in older children and adults:a systematic review and meta-analysis. Nutr J. 2010;9:4. doi: 10.1186/1475-2891-9-4. doi:10.1186/1475-2891-9-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walter T. Effect of iron-deficiency anemia on cognitive skills and neuromaturation in infancy and childhood. Food Nutr Bull. 2003;24(4 Suppl):S104–S110. doi: 10.1177/15648265030244S207. doi:10.1177/15648265030244S207. [DOI] [PubMed] [Google Scholar]
- 6.Short M, Domagalski JE. Iron deficiency anemia:evaluation and management. Am Fam Physician. 2013;87:98–104. [PubMed] [Google Scholar]
- 7.Ozdemir N. Iron deficiency anemia from diagnosis to treatment in children. Turk Pediatri Ars. 2015;50:11–19. doi: 10.5152/tpa.2015.2337. doi:10.5152/tpa.2015.2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mattiello V, Schmugge M, Hengartner H, Von der Weid N, Renella R. SPOG Pediatric Hematology Working Group. Diagnosis and management of iron deficiency in children with or without anemia:consensus recommendations of the SPOG Pediatric Hematology Working Group. Eur J Pediatr. 2020;179(4):527–545. doi: 10.1007/s00431-020-03597-5. doi:10.1007/s00431-020-03597-5. [DOI] [PubMed] [Google Scholar]
- 9.Cann MS, Perapoch Amadó M, Moore SE. The Role of Iron in Brain Development:A Systematic Review. Nutrients. 2020;12(7):2001. doi: 10.3390/nu12072001. doi:10.3390/nu12072001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gisslen T, Rao R, Georgieff MK. Anemia, Iron Supplementation, and the Brain. Clin Perinatol. 2023;50:853–868. doi: 10.1016/j.clp.2023.07.009. doi:10.1016/j.clp.2023.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Georgieff MK, Krebs NF, Cusick SE. The Benefits and Risks of Iron Supplementation in Pregnancy and Childhood. Annu Rev Nutr. 2019;39:121–146. doi: 10.1146/annurev-nutr-082018-124213. doi:10.1146/annurev-nutr-082018-124213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Varea A, Disalvo L, Fasano MV, Sala M, Avico AJ, Azrack MA, et al. Effectiveness of weekly and daily iron administration for the prevention of iron deficiency anemia in infants. Arch Argent Pediatr. 2023;121:e202202815. doi: 10.5546/aap.2022-02815.eng. doi:10.5546/aap.2022-02815.eng. [DOI] [PubMed] [Google Scholar]
- 13.Christensen L, Sguassero Y, Cuesta CB. Anemia y adherencia a la suplementación oral con hierro en una muestra de niños usuarios de la red de salud pública de Rosario, Santa Fe. Arch Argent Pediatr. 2013;111:288–294. doi: 10.5546/aap.2013.eng.288. doi:10.5546/aap.2013.xx. [DOI] [PubMed] [Google Scholar]
- 14.Rosas JP, Regil DLM, Malave GH, Urrutia FMC, Dowswell T. Intermittent oral iron supplementation during pregnancy. Cochrane Database Syst Rev. 2015;2015:CD009997. doi: 10.1002/14651858.CD009997.pub2. doi:10.4038/cmj.v46i4.6440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Haider BA, Bhutta ZA. Multiple-micronutrient supplementation for women during pregnancy. Cochrane Database Syst Rev. 2017;4(4):CD004905. doi: 10.1002/14651858.CD004905.pub5. doi:10.1002/14651858. CD004905.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins JP, Altman DG, Gøtzsche PC, Juni P, Moher D, Oxman AD, et al. Cochrane Bias Methods Group;Cochrane Statistical Methods Group. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. doi:10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berger J, Aguayo VM, Téllez W, Luján C, Traissac P, Miguel SJL, et al. Weekly iron supplementation is as effective as 5 day per week iron supplementation in Bolivian school children living at high altitude. Eur J Clin Nutr. 1997;51:381–386. doi: 10.1038/sj.ejcn.1600418. doi:10.1038/sj.ejcn.1600418. [DOI] [PubMed] [Google Scholar]
- 18.Faqih AM, Kakish SB, Izzat M. Effectiveness of intermittent iron treatment of two- to six-year-old Jordanian children with iron-deficiency anemia. Food Nutr Bull. 2006;27:220–227. doi: 10.1177/156482650602700304. doi:10.1177/156482650602700304. [DOI] [PubMed] [Google Scholar]
- 19.Hyder SM, Haseen F, Rahman M, Tondeur MC, Zlotkin SH. Effect of daily versus once-weekly home fortification with micronutrient Sprinkles on hemoglobin and iron status among young children in rural Bangladesh. Food Nutr Bull. 2007;28:156–164. doi: 10.1177/156482650702800204. doi:10.1177/156482650702800204. [DOI] [PubMed] [Google Scholar]
- 20.Kapil U, Sachdev HP, Dwivedi SN, Pandey RM, Upadhyay AD, Sareen N, et al. Relative efficacy of weekly and two differing doses of daily iron-folate supplementation in improving hemoglobin in mild and moderately anemic children between 3 and 5 years of age:a cluster randomized trial. Eur J Clin Nutr. 2013;67:343–347. doi: 10.1038/ejcn.2013.13. doi:10.1038/ejcn.2013.13. [DOI] [PubMed] [Google Scholar]
- 21.Khademloo M, Karami H, Ajami A, Yasari M. Comparison of the effectiveness of weekly and daily iron supplementation in 6- to 24-months-old babies in urban health centers of Sari, Iran. Pak J Biol Sci. 2009;12(2):195–197. doi: 10.3923/pjbs.2009.195.197. doi:10.3923/pjbs.2009.195.197. [DOI] [PubMed] [Google Scholar]
- 22.Siddiqui IA, Rahman MA, Jaleel A. Efficacy of daily vs. weekly supplementation of iron in schoolchildren with low iron status. J Trop Pediatr. 2004;50:276–278. doi: 10.1093/tropej/50.5.276. doi:10.1093/tropej/50.5.276. [DOI] [PubMed] [Google Scholar]
- 23.Sungthong R, Suwan ML, Chongsuvivatwong V, Geater AF. Once weekly is superior to daily iron supplementation on height gain but not on hematological improvement among schoolchildren in Thailand. J Nutr. 2002;132:418–422. doi: 10.1093/jn/132.3.418. doi:10.1093/jn/132.3.418. [DOI] [PubMed] [Google Scholar]
- 24.Desai MR, Dhar R, Rosen DH, Kariuki SK, Shi YP, Kager PA, et al. Daily iron supplementation is more efficacious than twice weekly iron supplementation for the treatment of childhood anemia in western Kenya. J Nutr. 2004;134:1167–1174. doi: 10.1093/jn/134.5.1167. doi:10.1093/jn/134.5.1167. [DOI] [PubMed] [Google Scholar]
- 25.Gunadi D, Rosdiana N, Lubis B. Comparison of once a day and three times a day iron treatment in 9–12-year-old elementary school children with iron deficiency anemia. Paediatrica Indonesiana. 2009;49:104–107. doi:10.14238/pi49.2.2009.104-7. [Google Scholar]
- 26.Zavaleta N, Respicio G, Garcia T. Efficacy and acceptability of two iron supplementation schedules in adolescent schoolgirls in Lima, Peru. J Nutr. 2000;130:462S–464S. doi: 10.1093/jn/130.2.462S. doi:10.1093/jn/130.2.462S. [DOI] [PubMed] [Google Scholar]
- 27.Low M, Farrell A, Biggs BA, Pasricha SR. Effects of daily iron supplementation in primary-school-aged children:systematic review and meta-analysis of randomized controlled trials. Can Med Assoc J. 2013;185:E791–802. doi: 10.1503/cmaj.130628. doi:10.1503/cmaj.130628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thompson J, Biggs BA, Pasricha SR. Effects of daily iron supplementation in 2- to 5-year-old children:systematic review and meta-analysis. Pediatrics. 2013;131:739–753. doi: 10.1542/peds.2012-2256. doi:10.1542/peds.2012-2256. [DOI] [PubMed] [Google Scholar]
- 29.Cembranel F, Dallazen C, Chica GDA. Effectiveness of ferrous sulfate supplementation in the prevention of anemia in children:a systematic literature review and meta-analysis. Cad Saude Publica. 2013;29:1731–1751. doi: 10.1590/0102-311x00152312. doi:10.1590/0102-311x00152312. [DOI] [PubMed] [Google Scholar]
- 30.Regil DLM, Jefferds ME, Sylvetsky AC, Dowswell T. Intermittent iron supplementation for improving nutrition and development in children under 12 years of age. Cochrane Database Syst Rev. 2011;2011:CD009085. doi: 10.1002/14651858.CD009085.pub2. doi:10.1002/14651858. CD009085.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Matos TA, Arcanjo FP, Santos PR, Arcanjo CC. Prevention and Treatment of Anemia in Infants through Supplementation, Assessing the Effectiveness of Using Iron Once or Twice Weekly. J Trop Pediatr. 2016;62:123–130. doi: 10.1093/tropej/fmv085. doi:10.1093/tropej/fmv085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Andersen CT, Marsden DM, Duggan CP, Liu E, Mozaffarian D, Fawzi WW, et al. Oral iron supplementation and anaemia in children according to schedule, duration, dose and cosupplementation:a systematic review and meta-analysis of 129 randomised trials. BMJ Glob Health. 2023;8:e010745. doi: 10.1136/bmjgh-2022-010745. doi:10.1136/bmjgh-2022-010745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guideline:Daily Iron Supplementation in Infants and Children. Geneva: World Health Organization; 2016. [(Last Accessed October 2,2024)]. Available at: https://www.who.int/publications/i/item/9789241549523 . [PubMed] [Google Scholar]
- 34.Fischer JAJ, Cherian AM, Bone JN, Karakochuk CD. The effects of oral ferrous bisglycinate supplementation on hemoglobin and ferritin concentrations in adults and children:a systematic review and meta-analysis of randomized controlled trials. Nutr Rev. 2023;81:904–920. doi: 10.1093/nutrit/nuac106. doi:10.1093/nutrit/nuac106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tolkien Z, Stecher L, Mander AP, Pereira DI, Powell JJ. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults:a systematic review and meta-analysis. PLoS One. 2015;10:e0117383. doi: 10.1371/journal.pone.0117383. doi:10.1371/journal.pone.0117383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shinoda S, Arita A. Regulatory mechanisms of intestinal iron absorption:iron-deficient mucosal cells respond immediately to dietary iron concentration. J Phys Fitness Sports Med. 2014;3:399–407. doi:10.7600/jpfsm.3.399. [Google Scholar]
- 37.Sachdev HP, Gera T. Preventing childhood anemia in India:iron supplementation and beyond. Eur J Clin Nutr. 2013;67:475–480. doi: 10.1038/ejcn.2012.212. doi:10.1038/ejcn.2012.212. [DOI] [PubMed] [Google Scholar]
- 38.Millen MSA, Dean R, Dihardja E, Ji P, Lonnerdal B. Benefits and Risks of Early Life Iron Supplementation. Nutrients. 2022;14(20):4380. doi: 10.3390/nu14204380. doi:10.3390/nu14204380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kondaiah P, Yaduvanshi PS, Sharp PA, Pullakhandam R. Iron and Zinc Homeostasis and Interactions:Does Enteric Zinc Excretion Cross-Talk with Intestinal Iron Absorption? Nutr. 2019;11(8):1885. doi: 10.3390/nu11081885. doi:10.3390/nu11081885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li J, Cao F, Yin HL, Huang ZJ, Lin ZT, Mao N, et al. Ferroptosis:past, present and future. Cell Death Dis. 2020;11(2):88. doi: 10.1038/s41419-020-2298-2. doi:10.1038/s41419-020-2298-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jaeggi T, Kortman GA, Moretti D, Chassard C, Holding P, Dostal A, et al. Iron fortification adversely affects the gut microbiome, increases pathogen abundance and induces intestinal inflammation in Kenyan infants. Gut. 2015;64:731–742. doi: 10.1136/gutjnl-2014-307720. doi:10.1136/gutjnl-2014-307720. [DOI] [PubMed] [Google Scholar]
- 42.Paganini D, Uyoga MA, Kortman GAM, Cercamond CI, Winkler HC, Boekhorst J, et al. Iron-containing micronutrient powders modify the effect of oral antibiotics on the infant gut microbiome and increase post-antibiotic diarrhoea risk:a controlled study in Kenya. Gut. 2019;68:645–653. doi: 10.1136/gutjnl-2018-317399. doi:10.1136/gutjnl-2018-317399. [DOI] [PubMed] [Google Scholar]