Abstract
Background
Unilateral biportal endoscopic transforaminal lumbar interbody fusion (UBE-TLIF) is a minimally invasive procedure for treating lumbar degenerative diseases. However, the use of endoscopic lumbar interbody fusion does not completely eliminate the risk of dural and nerve root injuries. This study has refined UBE-TLIF to incorporate en bloc resection of the ligamentum flavum for bilateral decompression and aim to detail the surgical procedure and evaluate the clinical outcomes of this modification.
Methods
This study analyzes the outcomes of 109 consecutive patients treated by a single surgeon for lumbar degenerative disease using UBE-TLIF. Patients were divided into two groups: Group A (51 patients) underwent en bloc resection of the ligamentum flavum, while Group B (58 patients) underwent routine piecemeal resection. Assessed outcomes included surgery-related complications, operation time, estimated blood loss, postoperative stay, visual analogue scale (VAS) score, and Oswestry Disability Index (ODI). The surgical technique is detailed within the study.
Results
In Group A, no nerve root or dura injuries were observed, whereas Group B reported one case of nerve root injury and three dura tears. The average operation time for Group A was shorter than that for Group B; however, the difference was not statistically significant (P > 0.05). No significant differences were found in the VAS score, ODI, estimated blood loss, or postoperative stay between the groups during follow-up.
Conclusions
En bloc resection of the ligamentum flavum for bilateral decompression in UBE-TLIF demonstrates satisfactory clinical outcomes and low perioperative complications rates, offering a safe and innovative alternative for the treatment of lumbar degenerative disease.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13018-024-05317-3.
Keywords: Lumbar degenerative disease, UBE, ULBD, Ligamentum flavum, Minimally invasive
Background
Degenerative lumbar disease represents a prevalent pathologic condition in spinal surgery, causing significant patient discomfort and imposing a substantial socioeconomic burden [1–4]. Lumbar fusion surgery, when performed on appropriately selected patients who meet surgical indications, has been demonstrated to effectively improve function, alleviate pain, and enhance quality of life [5–7]. However, traditional open fusion surgery often results in extensive dissection of paraspinal muscles, higher rates of perioperative complications, longer hospital stays, and extended recovery periods [8, 9].
There has been a shift in spinal surgery toward minimally invasive spine surgery (MISS) techniques, which offer substantial benefits by reducing surgical morbidities, such as less soft tissue dissection, reduced bleeding, and faster recovery [10, 11]. Recently, full endoscopic spinal surgery has been successfully applied to lumbar fusion procedures, noted for its safety and efficacy in yielding favorable clinical outcomes [10, 12]. However, the use of endoscopic lumbar interbody fusion does not completely eliminate the risk of dural and nerve root injuries [10, 11]. The Spine Patient Outcomes Research Trial study indicated that inadvertent durotomy occurred in up to 9% of cases, with other studies reporting rates between 7% and 10% [13–15]. Despite evidence from large studies suggesting that such incidents do not impair long-term outcomes, avoiding these complications remains a priority for surgeons [15, 16].
In response to these challenges, this study introduces a modification of the UBE-TLIF technique. The aim of this study is to describe the surgical approach in patients who underwent the modified technique (en bloc resection of the ligamentum flavum UBE-TLIF) and to comprehensively analyze the clinical outcomes during the follow-up period.
Methods
Patients
This study received approval from the ethics committee of a local hospital and was conducted in accordance with the Declaration of Helsinki. It involved a retrospective analysis of prospectively collected data on patients undergoing treatment. The inclusion criteria encompassed patients diagnosed with lumbar degenerative diseases who met the surgical indications for lumbar spondylolisthesis and lumbar spinal stenosis with instability. The exclusion criteria included the presence of spinal deformities such as scoliosis, lumbar disc herniation without bony spinal canal stenosis, spinal tumors, a history of lumbar surgery, and any other neurological lesions or conditions that could interfere with accurate preoperative and postoperative clinical assessments. According to a predefined protocol, 109 consecutive patients with lumbar degenerative diseases were included prospectively. All patients underwent single-level UBE-TLIF surgery. Patients were assigned to two groups: Group A underwent en bloc resection of the ligamentum flavum UBE-TLIF, and Group B underwent routine piecemeal resection of the ligamentum flavum UBE-TLIF. The assignment to these groups was based on alternating the two techniques monthly throughout the study duration. Each patient received one of the two techniques depending on the month of their surgery. All procedures were performed by the same surgical team, which had a minimum of five years of experience in endoscopic surgery.
Surgical technique
The surgical procedures, modified UBE-TLIF and routine UBE-TLIF, were performed on the left side at the L4-5 level. The techniques are summarized below with examples.
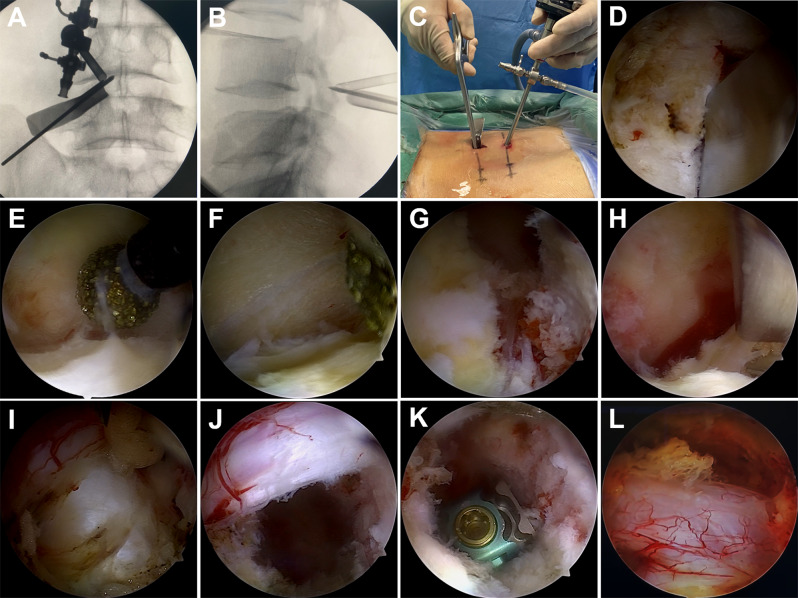
Modified UBE-TLIF
After successful anesthesia, the patient was positioned prone with abdominal suspension and slight knee flexion, and adjustments were made for optimal fluoroscopic visualization. Two 1-cm longitudinal incisions were created along the medial edge of the left L4 and L5 pedicle projections. The subcutaneous tissue was incised, and an expansion tube was subsequently inserted to dilate the soft tissue. Once the fluoroscopic positioning was confirmed to be satisfactory, an endoscope was introduced through the cephalic incision, and a radiofrequency electrode was inserted through the caudal incision. This setup facilitated the dissection of soft tissue surrounding the L4/5 articular processes, thereby exposing the lower edge of the L4 lamina, the upper edge of the L5 lamina, and the L4/5 articular process. A combination of a pendulum and osteotomy knife was employed to resect the lower edge of the L4 lamina and the left inferior articular process of L4. Subsequent steps involved the removal of the left lower edge of the L4 lamina (up to the origin of the ligamentum flavum), the inner edges of the L4 inferior and L5 superior articular processes, and the upper edge of the L5 lamina using a rongeur and a grinding drill. This procedure allowed the left ligamentum flavum to be mobilized. Further decompression was achieved using a grinding drill on the base of the L4/5 spinous process and lamina and the dorsal aspect of the contralateral dural sac. The grinding drill was also used to remove a portion of the contralateral lamina, increasing the space on the dorsal side of the ligamentum flavum to mitigate the risk of nerve injury. The contralateral thickened ligamentum flavum was freed using the same method. Subsequently, the bilateral ligamentum flavum was removed en bloc under endoscopic visualization, effectively alleviating the compression on the dural sac and L5 nerve root (Figs. 1 and 2). Following decompression, the intervertebral disc tissues were excised, and endoscopic preparation of the endplates was performed. Bone graft material was placed, followed by the implantation of an interbody cage for fusion. The polyetheretherketone interbody cages were sourced from the same manufacturer, with appropriate sizes selected based on the patient’s intervertebral disc space dimensions.
Fig. 1.
Procedures performed with the modified UBE-TLIF technique. A–C, Intraoperative C-arm perspective view and operation drawing. D, The lower edge of the L4 lamina and the L4 inferior articular process on the left side were resected using a pendulum saw and osteotomy knife. E–H, The attachment points of the ligamentum flavum were removed with grinding drills and rongeurs. I–K, The intervertebral disc was removed, and the interbody fusion cage was implanted. L, Dural sac after decompression
Fig. 2.

En bloc resection of the ligamentum flavum during the operation
Under fluoroscopic guidance, the percutaneous pedicle screws were inserted through the viewing portal and working portal. After the pedicle screws on the decompression side were implanted, the contralateral pedicle screws awere finally implanted. The screw-rod system was then securely locked in place. The procedure was concluded by placing a drainage tube and direct closure of the incisions. An illustrative operative video demonstrating the en bloc resection of the ligamentum flavum has been provided as supplementary material.
UBE-TLIF
Following successful anesthesia, the patient was positioned prone with abdominal suspension, slight knee flexion, and fluoroscopic positioning. The primary difference between UBE-TLIF and modified UBE-TLIF lies in the technique of ligamentum flavum removal. In the conventional UBE-TLIF, the ligamentum flavum is excised piecemeal, whereas in the modified UBE-TLIF, it is removed en bloc. Subsequent steps included the removal of intervertebral disc tissues, preparation of the endplates, and the placement of bone grafts and an interbody cage under endoscopic visualization to facilitate fusion.
Fluoroscopic guidance was then used to accurately place four K-wires into the bilateral pedicles of L4 and L5. Percutaneous pedicle screws were inserted along these wires, and the screw-rod system was securely locked. The procedure was concluded with the placement of a drainage tube and direct closure of the incisions.
Clinical outcome assessment
Postoperative assessments included surgery-related complications (e.g., nerve root injury, dura tear, infection) operation duration, estimated blood loss, and length of postoperative hospital stay. The visual analogue scale (VAS) scores for leg pain and back pain were evaluated preoperatively, three days postoperatively, and at 2-year follow-up. Additionally, Oswestry Disability Index (ODI) was collected both preoperatively and at 2-year follow-up. Fusion status was assessed by computed tomography (CT) scan at 2-year follow-up [17].
Statistical analysis
All continuous data were expressed as means and standard deviations. Differences between the two groups were evaluated using independent-sample t tests and paired-sample t tests. Categorical data were analyzed using the Chi-square test and Fisher exact test. A p value of less than 0.05 was considered statistically significant. All statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS version 25.0; IBM Corp., Armonk, NY, USA).
Results
Patient population
In total, the study comprised 109 patients, with 51 assigned to Group A and 58 to Group B. Table 1 presents the demographic and clinical characteristics of these patients. There were no significant differences between the two groups in terms of age, sex, body mass index, or spinal level. All patients were followed for 2-year postoperatively.
Table 1.
Demographic characteristics of the patients
| Variable | Modified UBE-TLIF (Group A) | UBE-TLIF (Group B) | P Value |
|---|---|---|---|
| Number of patients | 51 | 58 | |
| Sex (male/female) | 19/32 | 22/36 | 0.942 |
| Age (yr) | 57.5 ± 7.5 | 58.1 ± 8.9 | 0.683 |
| Body Mass Index (kg/m2) | 24.6 ± 3.1 | 25.4 ± 3.5 | 0.218 |
| Spinal level (n) | 0.997 | ||
| L4-L5 | 29 | 33 | |
| L5-S1 | 22 | 25 |
Data are given as (n) or mean ± SD; P < 0.05 was considered significant
Complications
Group A experienced fewer complications compared with Group B. Specifically, no instances of nerve root or dura injuries occurred postoperatively in Group A. In contrast, Group B reported four postoperative complications: one case of nerve root injury and three cases of dura tear. The patient with the nerve root injury presented with temporary numbness and pain in one lower limb, which gradually resolved after approximately three months of conservative treatment. The patients with dura tears underwent local compression at the incision site and received conservative treatment, with no residual symptoms observed during follow-up.
Clinical outcomes
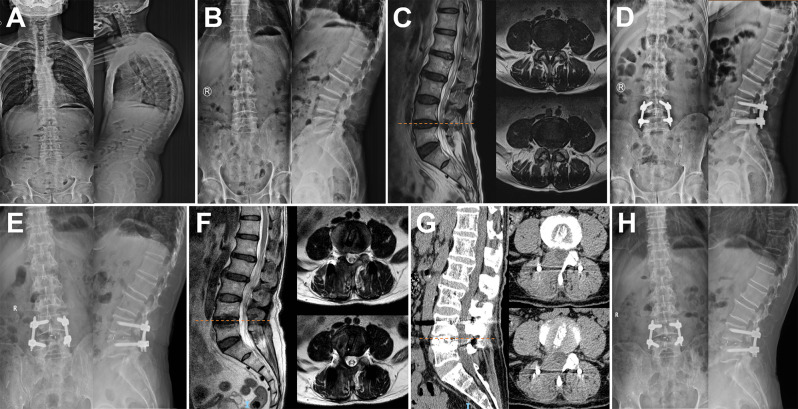
The average operation time for Group A was shorter than that for Group B, although this difference was not statistically significant (P > 0.05). Similarly, there were no significant differences between the two groups in terms of blood loss, length of postoperative stay, or the VAS score for leg pain measured preoperatively, three days postoperatively, and at 2-year follow-up (P > 0.05). Additionally, no significant differences were observed in the ODI preoperatively and at 2-year follow-up (P > 0.05). The lumbar fusion rate was 94% in Group A and 95% in Group B during the follow-up, with no statistically significant difference (P > 0.05). Detailed clinical outcomes are presented in Table 2. One case of lumbar degenerative disease treated with modified UBE-TLIF is depicted in Fig. 3.
Table 2.
Postoperative clinical outcomes
| Variable | Modified UBE-TLIF (Group A) | UBE-TLIF (Group B) | P Value |
|---|---|---|---|
| Complications, n (%) | 0.161 | ||
| Nerve root injury | 0 (0) | 1 (2) | |
| Dura tear | 0 (0) | 3 (5) | |
| Infection | 0 (0) | 0 (0) | |
| Operation time (min) | 207.5 ± 13.4 | 212.9 ± 17.7 | 0.074 |
| Estimated blood loss (mL) | 80.0 ± 23.7 | 84.0 ± 21.7 | 0.364 |
| Postoperative stay (days) | 3.6 ± 0.6 | 3.8 ± 0.8 | 0.136 |
| VAS score (leg) | |||
| Preoperative | 6.9 ± 0.9 | 6.9 ± 1.0 | 0.811 |
| Postoperative 3st day | 2.8 ± 0.8 | 2.7 ± 0.9 | 0.357 |
| 2-year follow-up | 0.9 ± 0.6 | 0.7 ± 0.6 | 0.102 |
| VAS score (back) | |||
| Preoperative | 6.6 ± 0.8 | 6.5 ± 0.7 | 0.817 |
| Postoperative 3st day | 2.6 ± 0.9 | 2.7 ± 0.9 | 0.502 |
| 2-year follow-up | 0.8 ± 0.7 | 0.9 ± 0.6 | 0.327 |
| ODI | |||
| Preoperative | 70.6 ± 6.9 | 70.4 ± 7.3 | 0.911 |
| 2-year follow-up | 15.1 ± 3.1 | 14.8 ± 3.2 | 0.534 |
| Fusion rate | 48 (94%) | 55 (95%) | 1.000 |
Data are given as (n) or mean ± SD; P < 0.05 was considered significant
Fig. 3.
A 71-year-old man diagnosed with degenerative lumbar disease underwent en bloc resection of ligamentum flavum UBE-TLIF. A–C, Preoperative X-ray and magnetic resonance imaging (MRI) of the lumbar spine. D, Postoperative Xray images of the lumbar spine 4 days after the operation. E–G, Postoperative X-ray, MRI, and CT images of the lumbar spine at 3-month follow-up. H, Postoperative X-ray images of the lumbar spine at 2-year follow-up
Discussion
Lumbar fusion surgery has been well established as an effective intervention for improving function, pain, and quality of life in individuals with severe degenerative lumbar spine disease [5–7]. Previous studies have reported that the primary complications associated with lumbar fusion surgery include but are not limited to infection, temporary or permanent neurological deficits, durotomy, cerebrospinal fluid leaks, nerve root injury, and misplaced hardware [18–20]. In recent years, percutaneous endoscopy has been integrated into lumbar fusion procedures, offering a minimally invasive approach that allows for direct decompression. UBE spinal surgery, employing one portal for the endoscope and another for surgical instruments, has shown encouraging outcomes in lumbar decompressive laminectomy and foraminotomy [21]. Despite the advantages of minimally invasive techniques, they do not entirely eliminate the risk of neurological deficits and injuries to the dural or nerve roots. Moreover, the ligamentum flavum serves as a critical natural barrier to the dural sac, playing a pivotal role in protecting the dura and nerve roots from direct injury during surgery [22]. A recent study reported that biportal decompression for spinal stenosis can be performed using the en bloc ligamentum flavum removal technique [23]. Therefore, this study aimed to describe the en bloc resection technique of the ligamentum flavum using UBE-TLIF and to analyze the clinical outcomes during follow-up.
Feasibility of en bloc resection of the ligamentum flavum using the UBE technique
The ligamentum flavum, a bifid ligament within the posterior ligamentous complex of the spine, is commonly encountered in lumbar surgery and serves as a crucial anatomical landmark. This ligament originates from the superior aspect of the inferior lamina and inserts onto the anteroinferior surface of the superior lamina [24, 25]. Biomechanically, the ligamentum flavum contributes to the resistance against kyphotic angulation in conjunction with other components of the posterior ligament complex. During posterior lumbar surgery, the proximity of the ligamentum flavum to vital neural structures necessitates careful surgical navigation to avoid damage. Furthermore, pathological changes such as proliferation of this ligament and the inner edge of the articular process can lead to compression of the dural sac and nerves, necessitating surgical intervention. The UBE technique, which employs two separate channels—an observation channel and an operation channel—provides a unique advantage. The substantial swing angle and range of these channels enhance the convenience of the operation and observation fields, facilitating the use of the “over-the-top technique” for contralateral decompression. Therefore, the UBE technique theoretically enables the en bloc resection of the ligamentum flavum, a capability supported by related studies [13].
Clinical outcomes of the en bloc resection of the ligamentum flavum in UBE-TLIF
It is unrealistic to expect that the en bloc technique will eliminate the risk of surgery-related complications, such as dural injuries and nerve root damage. Despite these inevitable complications, it is pertinent to question whether the overall incidence might be reduced by accurately identifying and navigating beyond the most constrained diameter of the canal [13]. Previous studies have noted that the incidence and consequences of incidental complications, such as dural tears, are often not anatomically localized where these events occur [13, 15]. The ligamentum flavum serves as a natural barrier, protecting the dura and nerve root from direct injury and can be strategically utilized throughout the procedure [22]. In this study, we observed fewer complications in Group A compared with Group B. Notably, there were no postoperative dural injuries or nerve root damage in Group A, whereas Group B experienced four postoperative complications, including one case of nerve root injury and three cases of dura tear. Therefore, we conclude that injuries to the nerve root or dura typically occur during spinal canal decompression, and the en bloc removal of the ligamentum flavum may offer protection to the transverse nerve root and dura.
Additionally, there are two noteworthy aspects of the en bloc resection of the ligamentum flavum. First, releasing the insertions of the ligamentum flavum decreases the number of Kerrison rongeur activations needed and maintains protective coverage over the dura throughout most of the surgery. Focusing on the insertion point also reduces the overall duration of the operation, aligning with the findings of this study to some extent. Furthermore, compared with piecemeal resection, en bloc resection of the ligamentum flavum prevents the inevitable expansion of the dural sac that occurs during decompression. This expansion increases the risk of dura tear during decompression, which can be mitigated by maintaining compression of the dural sac until all insertion points are released and the ligamentum flavum is completely removed.
Limitations
This study has several key limitations. First, it was conducted at a single center and involved a relatively small cohort, with the surgical techniques not being randomly assigned to each patient. Furthermore, the mean follow-up duration was only 2-year, which is insufficient for a thorough evaluation of clinical outcomes. Therefore, to more comprehensively analyze the clinical outcomes of modified UBE-TLIF, a randomized controlled clinical comparison study involving multiple centers, a larger sample size, and extended follow-up is needed.
Conclusions
En bloc resection of the ligamentum flavum for bilateral decompression in UBE-TLIF demonstrated satisfactory clinical outcomes and acceptably low rates of perioperative complications, establishing it as a safe and innovative alternative for the treatment of lumbar degenerative disease.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We thank Phoebe Chi, MD, from Liwen Bianji (Edanz) (www.liwenbianji.cn), for editing a draft of this manuscript.
Author contributions
Study conception and design: CL, BX, ZY. Material preparation, data collection and analysis: YZ, LQ, LY, RZ. The first draft of the manuscript was written by CL and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This study is supported by the National High Level Hospital Clinical Research Funding (Interdepartmental Research Project of Peking University First Hospital, 2023IR18), the National High Level Hospital Clinical Research Funding (Youth Clinical Research Project of Peking University First Hospital, 2024YC31), the National High Level Hospital Clinical Research Funding (Scientific Research Seed Fund of Peking University First Hospital, 2024SF50), the Capital Health Research and Development of Special Fund (2022-2Z-40713), and the National High Level Hospital Clinical Research Funding (Youth Clinical Research Project of Peking University First Hospital, 2023YC22).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This study was conducted in compliance with the Declaration of Helsinki of 1964 and was approved by the ethics committee of Peking University First Hospital (2023IR18). Informed consent was obtained from all individual participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Chao Li and Beiyu Xu contributed equally to this work.
References
- 1.Esposito CI, Miller TT, Kim HJ, Barlow BT, Wright TM, Padgett DE, et al. Does degenerative lumbar spine Disease Influence Femoroacetabular Flexion in patients undergoing total hip arthroplasty? Clin Orthop Relat Res. 2016;474(8):1788–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang S, Lassalle L, Mekki A, Appert G, Rannou F, Nguyen C, et al. Can T2-weighted Dixon fat-only images replace T1-weighted images in degenerative disc disease with Modic changes on lumbar spine MRI? Eur Radiol. 2021;31(12):9380–9. [DOI] [PubMed] [Google Scholar]
- 3.Heo DH, Son SK, Eum JH, Park CK. Fully endoscopic lumbar interbody fusion using a percutaneous unilateral biportal endoscopic technique: technical note and preliminary clinical results. Neurosurg Focus. 2017;43(2):E8. [DOI] [PubMed] [Google Scholar]
- 4.Reid PC, Morr S, Kaiser MG. State of the union: a review of lumbar fusion indications and techniques for degenerative spine disease. J Neurosurg Spine. 2019;31(1):1–14. [DOI] [PubMed] [Google Scholar]
- 5.Heemskerk JL, Oluwadara Akinduro O, Clifton W, Quinones-Hinojosa A, Abode-Iyamah KO. Long-term clinical outcome of minimally invasive versus open single-level transforaminal lumbar interbody fusion for degenerative lumbar diseases: a meta-analysis. Spine J. 2021;21(12):2049–65. [DOI] [PubMed] [Google Scholar]
- 6.Ao S, Zheng W, Wu J, Tang Y, Zhang C, Zhou Y, et al. Comparison of preliminary clinical outcomes between percutaneous endoscopic and minimally invasive transforaminal lumbar interbody fusion for lumbar degenerative diseases in a tertiary hospital: is percutaneous endoscopic procedure superior to MIS-TLIF? A prospective cohort study. Int J Surg. 2020;76:136–43. [DOI] [PubMed] [Google Scholar]
- 7.Fisher CG, Vaccaro AR, Patel AA, Whang PG, Thomas KC, Chi J, et al. Evidence-based recommendations for spine surgery. Spine (Phila Pa 1976). 2020;45(12):851–9. [DOI] [PubMed] [Google Scholar]
- 8.Jin M, Zhang J, Shao H, Liu J, Huang Y. Percutaneous transforaminal endoscopic lumbar Interbody Fusion for degenerative lumbar diseases: a consecutive Case Series with Mean 2-Year Follow-Up. Pain Physician. 2020;23(2):165–74. [PubMed] [Google Scholar]
- 9.Chan AK, Bisson EF, Bydon M, Foley KT, Glassman SD, Shaffrey CI, et al. A comparison of minimally invasive and open transforaminal lumbar Interbody Fusion for Grade 1 degenerative lumbar spondylolisthesis: an analysis of the prospective quality outcomes database. Neurosurgery. 2020;87(3):555–62. [DOI] [PubMed] [Google Scholar]
- 10.Pholprajug P, Kotheeranurak V, Liu Y, Kim J-S. The endoscopic lumbar Interbody Fusion: a narrative review, and future perspective. Neurospine. 2023;20(4):1224–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koreckij T, Park DK, Fischgrund J. Minimally invasive spine surgery in the treatment of thoracolumbar and lumbar spine trauma. Neurosurg Focus. 2014;37(1):E11. [DOI] [PubMed] [Google Scholar]
- 12.Kang M-S, You K-H, Choi J-Y, Heo D-H, Chung H-J, Park H-J. Minimally invasive transforaminal lumbar interbody fusion using the biportal endoscopic techniques versus microscopic tubular technique. Spine J. 2021;21(12):2066–77. [DOI] [PubMed] [Google Scholar]
- 13.Tumialán LM. En Bloc resection of ligamentum flavum with laminotomy of the caudal lamina in the minimally invasive laminectomy: surgical anatomy and technique. Neurosurg Focus. 2023;54(1):E8. [DOI] [PubMed] [Google Scholar]
- 14.Lurie JD, Tosteson TD, Tosteson A, Abdu WA, Zhao W, Morgan TS, et al. Long-term outcomes of lumbar spinal stenosis: eight-year results of the spine patient outcomes Research Trial (SPORT). Spine (Phila Pa 1976). 2015;40(2):63–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herren C, Sobottke R, Mannion AF, Zweig T, Munting E, Otten P, et al. Incidental durotomy in decompression for lumbar spinal stenosis: incidence, risk factors and effect on outcomes in the spine Tango registry. Eur Spine J. 2017;26(10):2483–95. [DOI] [PubMed] [Google Scholar]
- 16.Desai A, Ball PA, Bekelis K, Lurie J, Mirza SK, Tosteson TD et al. SPORT: Does incidental durotomy affect longterm outcomes in cases of spinal stenosis? Neurosurgery. 2015;76 Suppl 1(0 1). [DOI] [PMC free article] [PubMed]
- 17.Wang Y-Y, Chung Y-H, Huang C-H, Hu M-H. Comparison of minimally invasive transforaminal lumbar interbody fusion and midline lumbar interbody fusion in patients with spondylolisthesis. J Orthop Surg Res. 2024;19(1):286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wong AP, Smith ZA, Nixon AT, Lawton CD, Dahdaleh NS, Wong RH, et al. Intraoperative and perioperative complications in minimally invasive transforaminal lumbar interbody fusion: a review of 513 patients. J Neurosurg Spine. 2015;22(5):487–95. [DOI] [PubMed] [Google Scholar]
- 19.Weiss H, Garcia RM, Hopkins B, Shlobin N, Dahdaleh NS. A systematic review of complications following minimally invasive spine surgery including transforaminal lumbar Interbody Fusion. Curr Rev Musculoskelet Med. 2019;12(3):328–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sclafani JA, Kim CW. Complications associated with the initial learning curve of minimally invasive spine surgery: a systematic review. Clin Orthop Relat Res. 2014;472(6):1711–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaen A, Park MK, Son S-K. Clinical outcomes of uniportal compared with biportal endoscopic decompression for the treatment of lumbar spinal stenosis: a systematic review and meta-analysis. Eur Spine J. 2023;32(8):2717–25. [DOI] [PubMed] [Google Scholar]
- 22.Wang L, Li H, Zhao Y, Yuan S, Tian Y, Liu X. Ligamentum-preserved/Temporary Preserved minimally invasive transforaminal lumbar Interbody Fusion for lumbar spondylolisthesis: technical note and 2-year follow-up. Spine (Phila Pa 1976). 2022;47(8):E328–36. [DOI] [PubMed] [Google Scholar]
- 23.Park CW, Oh JY. Biportal endoscopic en bloc removal of the ligamentum flavum for spinal stenosis: nuances for the butterfly technique. Asian Spine J. 2024;18(4):587–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Olszewski AD, Yaszemski MJ, White AA. The anatomy of the human lumbar ligamentum flavum. New observations and their surgical importance. Spine (Phila Pa 1976). 1996;21(20):2307–12. [DOI] [PubMed] [Google Scholar]
- 25.Iwanaga J, Ishak B, Saga T, Singla A, Impastato D, Chapman JR, et al. The lumbar Ligamentum Flavum does not have two layers and is confluent with the interspinous ligament: anatomical study with application to Surgical and Interventional Pain procedures. Clin Anat. 2020;33(1):34–40. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.