Abstract
Background/purpose
Traditional restorative composites require time-consuming incremental layering techniques which poses challenges in pediatric dentistry. SonicFill bulk resin allows for thicker layers to be placed efficiently, reducing treatment time and enhancing filling quality. This prospective, parallel, randomized, controlled clinical study aimed to compare the operative time and outcomes between SonicFill bulk resin and conventional restorative composite for deep proximal restorations in primary molars.
Materials and methods
A total of 129 primary molars in patients with proximal deep caries were randomly assigned to two groups. The experimental group (n = 66) received SonicFill bulk resin treatment, while the control group (n = 63) underwent restoration using traditional composite. The operative time was documented, and all teeth were evaluated at 6, 12, 18, and 24 -months post-treatment based on the modified criteria from the United States Public Health Service and radiographic examination score.
Results
The operative time for SonicFill resin (137.5 ± 5.2 s) revealed a significant reduction compared to traditional composite (193.5 ± 14.4 s), (t = 29.64, P < 0.05). No significant differences were observed between the two groups in terms of colour match, marginal adaptation and so on. Success rates were 95.2% for the control group and 89.4% for the experimental group (χ2 = 1.44, P>0.05).
Conclusion
The SonicFill resin technique has proven to be a viable and time-efficient option for the restoration of primary molars with deep proximal caries.
Trial registration
This study was registered in the Chinese Clinical Trial Registry (ChiCTR2200055570) on the date of 13/01/2022.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12903-024-05242-1.
Keywords: Proximal deep caries, SonicFill bulk resin, Traditional composite, Primary molar
Introduction
According to the World Health Organization (WHO), the estimated global average prevalence of caries in deciduous teeth is 43%, affecting 514 million children worldwide [1]. Caries occurring in proximal surfaces are more commonly observed. Traditional restorative composite with a light-curing depth of less than 2 mm often requires an incremental layering technique to ensure optimal filling quality and reduce microleakage [2]. For children with poor coordination, shallow oral cavities, and increased salivary flow, this procedure is time-consuming and has suboptimal outcomes.
SonicFill bulk resin (Kerr, Brea, CA, USA) represents a ground-breaking filling material that utilizes a sonic wave-driven handpiece to deliver sonic energy to the composite resin. This innovation extended the depth of cure, enabling layer-by-layer insertion into prepared cavities up to 4- or 5-mm thick, thereby streamlining the restorative process and saving valuable time [3].
The composition of SonicFill bulk resin includes a matrix and an inorganic filler, boasting a higher resin filler and nanofiller content than that of traditional resin. This formulation significantly reduces the polymerization shrinkage rate and gap formation [4]. Additionally, it shows a certain degree of fluidity under ultrasound observation, facilitating ease of placement and reducing marginal microleakage [5, 6]. Furthermore, SonicFill bulk resin exhibits excellent mechanical properties and abrasion resistance [7, 8], with its hardness closely resembling that of traditional restorative composite commonly used in primary teeth.
Clinical trials have demonstrated the efficacy of SonicFill bulk resin in permanent teeth, resulting in significant reductions in filling time and positive outcomes over a period of 1–2 years [9–11]. However, there is limited literature available on its application in deciduous teeth.
In this study, we aimed to compare the operative time and effectiveness of SonicFill bulk resin with traditional composite in the restoration of proximal deep caries in primary molars and to seek a superior treatment material for paediatric patients.
Materials and methods
This prospective, parallel, randomized, controlled clinical study aimed to compare the filling time and clinical effects of the SonicFill bulk resin (Kerr, A2) versus the traditional restorative composite Beautifil II (Shofu, A2) in the restoration of proximal deep caries in primary molars (Table 1).
Table 1.
Restorative Materials and Adhesive System Used in the Study
| Material | Composition | Filler loading | Manufacturer |
|---|---|---|---|
| SonicFill |
Bis-GMA, Bis-EMA, EBPADMA, TEGDMA Silicon dioxide modified dimethacrylate aminoformate"。 |
81.3 wt% (65.5 vol%) |
Kerr, Brea, CA USA |
| Beautifil II |
Bis-GMA, TEGDMA Multifunctional glass filler, Surface prereacted glass-ionomer filler based on aluminofluoro-borosilicate glass |
83.3 wt% (68.6 vol%) |
Shofu, Tokyo, Japan |
| Clearfil SE-Bond |
Primer: MDP, HEMA, dimethacrylate monomer, water, catalyst Bond: MDP, HEMA, dimethacrylate monomer, microfiller, catalyst |
Kuraray, Tokyo, Japan | |
Abbreviations: Bis-GMA bisphenol-a-glycidyl dimethacrylate, Bis-EMA ethoxylated bisphenol-a-glycol dimethacrylate, EBPADMA ethoxylated bisphenol A dimethacrylate, TEGDMA triethylene glycol dimethacrylate,MDPMedronic Acid, HEMA 2-Hydroxyethyl methacrylate
This study was conducted at the Third Clinical Division of the Peking University School and Hospital of Stomatology, Beijing, China, approved by the Ethics Committee of the Peking University School and Hospital of Stomatology (ref. PKUSSIRB-202167125) and registered in the Chinese Clinical Trial Registry (ChiCTR2200055570). The authors registered the study with the Consolidated Standards of Reporting Trials.
SonicFill bulk resin was hypothetically not inferior to the traditional composite. The sample size calculation was based on two independent sample rates and was performed using the PASS software (NCSS, LLC, Kaysville, UT, USA). We assumed that the success rates of both traditional composite and SonicFill bulk resin were 90%, according to similar materials reported in the literature [12]. To account for a desired accuracy of 20%, a significance level of 5%, and a safety margin of 10% to compensate for patient dropouts and changes in treatment interventions, a minimum sample size of 63 teeth in each group was required. Consequently, 129 teeth were selected from 28 patients, aged between 4 and 8 years, who presented with proximal deep caries between August and November 2021.
A comprehensive pain history of each included molar was obtained from the children and confirmed by their parents/guardians. The tooth with the chief complaint was examined and analyzed using clinical examinations including palpation, percussion, mobility testing, gingival assessments, and radiation examinations (apical radiographs).
The inclusion criteria were as follows:
Primary molars exhibiting proximal caries with ICDAS (International Caries Detection and Assessment System) scores of 3, 4, or 5 [13], but without any indications of spontaneous pain or nocturnal discomfort;
Caries located supragingivally;
Mobility within normal limits;\
Caries imaging revealed no involvement of the pulp, and there was no apical radiolucency observed on the radiographs.
Good patient compliance.
All teeth were then randomized into the control or the experimental group using the coin toss method. The filling method may vary among different teeth in a patient. The evaluators and the patients did not know the allocation process.
A skilled paediatric dentist with at least 10 years of clinical experience performed the treatment. The affected tooth was anaesthetized with 4% articaine and epinephrine (1:100 000) and isolated using a dental dam. The cavity was then opened and expanded using a water-cooled, high-speed handpiece equipped with a diamond. The peripheral carious enamel and soft dentin were then removed using a large round carbide bur until hard dentin layer was reached. The cavity was bonded with a two-step, self-etch adhesive (Clearfil SE-Bond, Kuraray, Tokyo, Japan). The experimental group used SonicFill bulk resin, whereas the control group used Beautifil composite for restoration. The operative time, from the application of the adhesive coating to the completion of the blending polish, was recorded using a timer (VWR, Radnor, PA, USA).
All teeth were clinically and radiographically evaluated 6, 12, 18, and 24 months after treatment. Evaluators who had more than 10 years of clinical experience were kept unaware of the materials used in this double-blind study. The inter-examiner Kappa index was 0.85, and the intra-examiner Kappa index was 0.88. Any disagreements were discussed in order to reach a consensus. They evaluated the retention, color matching, edge integrity, surface quality, etc. of the restoration according to the modified criteria of the United States Public Health Service (USPHS) (Table 2) [9]. A radiographic examination was also performed. The absence of periapical radiolucency was scored as ‘a’, while the presence of periapical radiolucency was scored as ‘c’.
Table 2.
Modified united states public health service evaluation criteria
| Category | Scores | Criteria |
|---|---|---|
| Retention | a | Complete retention of the restoration |
| c | Loss of the restoration | |
| Secondary caries | a | No evidence of caries |
| c | Caries is evident | |
| Colour match | a | Restoration matches adjacent tooth structure in color and translucency |
| b | Mismatch is within an acceptable range of tooth color and translucency | |
| c | Mismatch is outside the acceptable range | |
| Marginal adaptation |
a b |
Closely adapted, no visible crevice Visible crevice, explorer will penetrate |
| c | Crevice in which dentin is exposed | |
| Marginal discoloration |
a b |
Absence of marginal discoloration Presence of marginal discoloration, limited and not extended |
| c | Evident marginal discoloration, penetrated toward the pulp chamber | |
| Anatomic form | a | Continuous |
| b | Slight discontinuity, clinically acceptable | |
| c | Discontinuous, failure |
A case was deemed a failure if it scored ‘c’ in either the clinical or radiographic evaluation. Conversely, if a case did not score ‘c’ in either evaluation, it was considered a success.
The data were final analyzed according to the modified intention-to-treat (MITT) principle and using the Statistical Package for Social Sciences software, version 19.0. The results were analyzed using t test, Chi-square test and Fisher’s exact test. Survival curves were generated and assessed using Kaplan-Meier analysis with log-rank tests. The confidence level was set to 95% (P<0.05).
Results
The baseline clinical characteristics of the two groups are shown in Table 3. No significant differences were observed at the baseline.
Table 3.
Clinical characteristics
| Factor | control group | experimental group | χ2 | P | |
|---|---|---|---|---|---|
| n | 63 | 66 | |||
| Age | 5.8±1.2 | 5.5±1.1 | |||
| Gender, n (%) | Male | 40(63) | 42(64) | 0 | 0.986 |
| Female | 23(37) | 24(36) | |||
| Location | Maxillary | 30(48) | 23(35) | 2.17 | 0.141 |
| Mandibular | 33(52) | 43(65) | |||
A comparison of the operative times is shown in Table 4. The operative time of the control group was 193.5±14.4s, while that of the experimental group was 137.5±5.2s. Operative time in the experimental group was significantly lower than that in the control group (t=29.64, P<0.05).
Table 4.
Comparison of operative time between two groups
| Group | Teeth number | Time(s) |
|---|---|---|
| Control group | 63 | 193.5±14.4 |
| Experimental group | 66 | 137.5±5.2 |
| t | 29.64 | |
| P | <0.001 |
An Evaluation of the restoration at 6, 12, 18, and 24 months is shown in Tables 5, 6, and 7. Three teeth in the control group and five in the experimental group experienced retention loss after the 6 months follow-up. Additionally, two teeth in the experimental group exhibited retention loss after the 12-month follow-up. None of the restorations showed secondary caries or X-ray abnormality. The results all scored ‘a’, suggesting no differences between the two groups with regard to colour matching and anatomic form. The majority of teeth in both groups scored ‘a’ in marginal adaptation, with a slightly higher percentage in the control group (100% vs. 98%). For marginal discoloration, the difference was not significant after the 2-year follow-up. Specifically, eight teeth in the experimental group scored ‘b’ (86%), while two in the control group scored ‘b’ (96%).
Table 5.
Results of the clinical evaluation of retention criterion
| 6 m | 12m | 18 m | 24 m | |||||
|---|---|---|---|---|---|---|---|---|
| The control group | a | 55(94.8%) | 54(100%) | 54(100%) | 54(100%) | |||
| c | 3(5.2%) | 0 | 0 | 0 | ||||
| The experimental group | a | 61(92.4%) | 58(96.7%) | 56(100%) | 56(100%) | |||
| c | 5(7.6%) | 2(3.3%) | 0 | 0 | ||||
| Fisher’s exact P-value | 0.722 | 0.497 | ||||||
Table 6.
Results of the clinical evaluation of marginal adaptation criterion
| 6 m | 12m | 18 m | 24 m | |||
|---|---|---|---|---|---|---|
| The control group | a | 55(100%) | 54(100%) | 54(100%) | 54(100%) | |
| b | 0 | 0 | 0 | 0 | ||
| The experimental group | a | 60(98%) | 55(98%) | 55(98%) | 55(98%) | |
| b | 1(2%) | 1(2%) | 1(2%) | 1(2%) | ||
| Fisher’s exact p-value | 1 | 1 | 1 | 1 | ||
Table 7.
Results of the clinical evaluation of marginal discoloration criterion
| 6 m | 12m | 18 m | 24 m | |||
|---|---|---|---|---|---|---|
| The control group | a | 53(96%) | 52(96%) | 52(96%) | 52(96%) | |
| b | 2(4%) | 2(4%) | 2(4%) | 2(4%) | ||
| The experimental group | a | 56(92%) | 51(93%) | 48(86%) | 48(86%) | |
| b | 5(8%) | 5(7%) | 8(14%) | 8(14%) | ||
| Fisher’s exact P-value | 0.719 | 0.438 | 0.094 | 0.094 | ||
Kaplan–Meier survival curves for the teeth are shown in Fig. 1. In the control group, five teeth were lost to follow-up after 6 months, and one tooth was lost to follow-up after 12 months. In the experimental group, one tooth was lost to follow-up after 12 months. The survival rate represents the success rate. The success rate at 6 months was 95.2% and 92.4% for the control and experimental groups, respectively, and 95.2% and 89.4% for the control and experimental groups, at 12 months and beyond, respectively. However, statistical analysis revealed no significant difference between the two groups. (χ2=1.44, P>0.05).
Fig. 1.
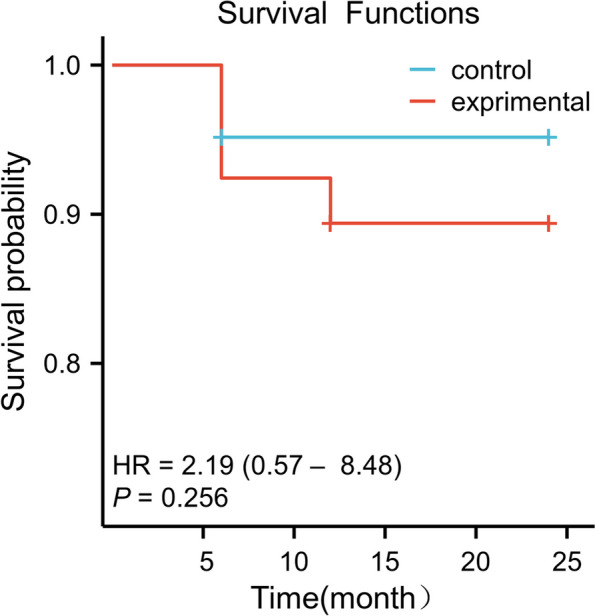
Kaplan–Meier survival curves for restoration
Discussion
Since the caries involved both enamel and dentin in our study, the self-etching system was chosen because it offered enhanced adhesive performance. Moreover, the self-etching technique saved time by eliminating the need for separate etching and rinsing steps for enamel. It also minimized the risk of over-etching and reduced potential irritation to the dental pulp.
Light-cured composite is frequently used in paediatric dentistry for treating dental caries due to its aesthetic appeal, durability, and effective restoration properties. Beautifil II, a specific type of material, is designed to release and recharge fluoride along with five other ions, thereby effectively reducing plaque adhesion and preventing bacterial colonisation [14]. As such, in the control group, the Beautifil II composite was used for restoration via incremental layering techniques, whereas in the experimental group, we utilised Sonicfill bulk resin integration. The operative time and effectiveness were compared in this study.
The operative time of the experimental group was significantly reduced, by approximately 29.5%, compared to the control group. This finding aligns with results from both in vitro trials and other in vivo trials, where operative time reductions ranged from 18 to 57% [15–18].
The filling effect in this study was evaluated using both the modified USPHS criteria and a radiographic examination score. The modified criteria of the USPHS, which reflect the clinical success of dental restorations, are widely used in clinical trials to assess key characteristics of these restorations [12, 19, 20]. Additionally, periodic radiographs were taken to better diagnose secondary caries and apical lesions. This approach complemented the clinical examinations and enhanced the reliability of the results.
Failure that occurred within the first 6–12 months can be attributed to several factors, including the size and location of the filling, biting forces, and oral habits [21]. Secondary caries and restoration fractures were the major causes of failure. All cases with filling loss had secondary caries, and in 6 out of 12 cases, there were missing proximal fillings while the occlusal fillings remained intact. The proximal areas may be more susceptible to food debris and bacterial invasion, leading to secondary caries and subsequent filling failure. Additionally, improper bite alignment can cause excessive pressure in certain areas, increasing the risk of filling loss. No apical lesions were detected on the radiographs of any of the teeth. We did not test for sensitivity due to the difficulty of children effectively expressing their sensations. The process of resin filling can affect dental pulp vitality since the temperature changes with the use of a high-speed handpiece. The curing process of resin fillings can lead to polymerization shrinkage, generating stress on the tooth structure and potentially affecting pulp vitality. Improper bonding or sealing of resin might result in microleakage, allowing fluids and bacteria to penetrate the tooth, leading to potential irritation of the dental pulp [22, 23]. Although these factors may have an impact, modern techniques and materials aim to minimize such effects and prioritized the preservation of dental pulp health. The restorative complex must endure all the physicochemical challenges [24, 25]. It is important to note that no restoration can be expected to last indefinitely. However, the rate of restoration failure can be reduced by improving dentists’ technique skills in cavity preparation, bonding and restoration placement; improving the oral hygiene through patient education, and improving the quality of the materials used.
Marginal adaptation of the resin is crucial in dental restorations since it is directly related to the long-term stability and success of tooth restoration. In this study, every tooth in the control group achieved a score of ‘a’, whereas in the experimental group, one tooth scored ‘b’, and the remaining teeth scored ‘a’. No significant difference was observed between the two groups. The findings suggest that the incremental layering technique produces better internal adaptation than the bulk-fill technique [26]. However, techniques such as preheating and sonic insertion can enhance the internal adaptation of the resin materials [27]. Therefore, the marginal adaptation of the SonicFill bulk resin is comparable to that of the traditional incremental filling with Beautifil resin.
A marginal discoloration score of ‘b’ could be attributed to factors such as plaque accumulation and superficial staining. It is important to note that this is not necessarily indicative of marginal microleakage, which is characterised by the presence of penetrating discoloration [28]. Rather than being replaced, the restoration could be refurbished and polished. In this study, although the experimental group exhibited a higher rate of ‘b’ scores compared to the control group, the results did not show a significant difference, which is consistent with findings from previous studies [29, 30]. Despite this, marginal discoloration might result from defects that exist between the composite restoration and the cavity margins, and regular follow-ups remain crucial for monitoring.
SonicFill bulk resin not only reduced operative time but also exhibited clinical outcomes comparable to traditional resin. However, it is crucial to acknowledge the limitations of this study. To address the potential bias resulting from patient loss-to-follow-up, we used a modified intention-to-treat analysis. Patients who dropped out were excluded from the final analyses due to missing outcome data. This modification aimed to mitigate the impact of the potential bias associated with patients lost to follow-up. Furthermore, it is important to emphasize that findings of our study warrant further validation through additional research with larger sample sizes and extended follow-up durations.
Conlusion
In conclusion, SonicFill bulk resin was effective in reducing operative time without compromising clinical performance for the restoration of proximal deep caries in primary molars. This study is significant as it highlights the efficiency of SonicFill bulk resin in pediatric dentistry, potentially setting a new standard for quicker and equally effective dental restorations, thus improving patient comfort and clinical outcomes.
Supplementary Information
Acknowledgements
The authors thank Professor Jun Li for the Language refinement of the article. The authors thank Professor Xueying Li for her valuable input into the analysis of the outcome. The authors thank the faculty of the Third Clinical Division, Peking University School and Hospital of Stomatology &National Center of Stomatology, for helping with subject recruitment.
Abbreviations
- MITT
Modified intention-to-treat
- USPHS
United States Public Health Service
- Bis-GMA
Bisphenol-a-glycidyl dimethacrylate
- Bis-EMA
Ethoxylated bisphenol-a-glycol dimethacrylate
- EBPADMA
Ethoxylated bisphenol A dimethacrylate
- TEGDMA
triethylene glycol dimethacrylate
- MDP
Medronic Acid
- HEMA
2-Hydroxyethyl methacrylate
Authors’ contributions
Dr Yingting Yang and Prof. Bin Xia contributed to study design, project administration, data analysis, study conduct, data collection and analysis, and manuscript preparation. Haihua Lei, Yang Liu contributed to study design, study conduct, and data collection. Dr Yingting Yang wrote the main manuscript text.
Funding
This research was conducted without any external funding support.
Data availability
The data of this research are available upon reasonable request from the corresponding author.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of the Peking University School and Hospital of Stomatology, reference number PKUSSIRB-202167125. The written informed consent was obtained from the patients’ parents.
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization: Global Oral Health Status Report: Towards universal health coverage for oral health by 2030. World Health Organization. 2022. https://www.who.int/publications-detail-redirect/9789240061484. Accessed 18 Nov 2022.
- 2.Park J, Chang J, Ferracane J, et al. How should composite be layered to reduce shrinkage stress: incremental or bulk filling? Dent Mater. 2008;24(11):1501–5. [DOI] [PubMed] [Google Scholar]
- 3.Benetti AR, Havndrup-Pedersen C, Honoré D, et al. Bulk-fill resin composites: polymerization contraction, depth of cure, and gap formation. Oper Dent. 2015;40(2):190–200. [DOI] [PubMed] [Google Scholar]
- 4.Tauböck TT, Jäger F, Attin T. Polymerization shrinkage and shrinkage force kinetics of high- and low-viscosity dimethacrylate- and ormocer-based bulk-fill resin composites. Odontology. 2019;107(1):103–10. [DOI] [PubMed] [Google Scholar]
- 5.Kalakijuybari FZ, Pasdar N, Ahmadi G, et al. Investigating the impact of flowable composite liner on the fracture strength and microleakage of large composite resin restorations of primary anterior teeth. Eur Arch Paediatr Dent. 2023;24(4):473–9. [DOI] [PubMed] [Google Scholar]
- 6.Gamarra VSS, Borges GA, Júnior LHB, et al. Marginal adaptation and microleakage of a bulk-fill composite resin photopolymerized with different techniques. Odontology. 2018;106(1):56–63. [DOI] [PubMed] [Google Scholar]
- 7.Alshali RZ, Salim NA, Satterthwaite JD, et al. Post-irradiation hardness development, chemical softening, and thermal stability of bulk-fill and conventional resin-composites. J Dent. 2015;43(2):209–18. [DOI] [PubMed] [Google Scholar]
- 8.Alkhudhairy FI. The effect of curing intensity on mechanical properties of different bulk-fill composite resins. Clin Cosmet Investig Dent. 2017;9:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bayraktar Y, Ercan E, Hamidi MM, et al. One-year clinical evaluation of different types of bulk-fill composites. J Investig Clin Dent. 2017;8(2):10. [DOI] [PubMed] [Google Scholar]
- 10.Atabek D, Aktaş N, Sakaryali D, et al. Two-year clinical performance of sonic-resin placement system in posterior restorations. Quintessence Int. 2017;48(9):743–51. [DOI] [PubMed] [Google Scholar]
- 11.Colak H, Tokay U, Uzgur R, et al. A prospective, randomized, double-blind clinical trial of one nano-hybrid and one high-viscosity bulk-fill composite restorative systems in class II cavities: 12 months results. Niger J Clin Pract. 2017;20(7):822–31. [DOI] [PubMed] [Google Scholar]
- 12.Akalιn TT, Bozkurt FO, Kusdemir M, et al. Clinical evaluation of Sonic-activated high viscosity bulk-fill Nanohybrid Resin Composite restorations in Class II cavities: a prospective clinical study up to 2 years. Eur J Prosthodont Restor Dent. 2018;30(3):152–60. [DOI] [PubMed] [Google Scholar]
- 13.Shivakumar K, Prasad S, Chandu G. International Caries Detection and Assessment System: a new paradigm in detection of dental caries. J Conserv Dent. 2009;12(1):10–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Naoum S, Ellakwa A, Martin F, et al. Fluoride release, recharge and mechanical property stability of various fluoride-containing resin composites. Oper Dent. 2011;36(4):422–32. [DOI] [PubMed] [Google Scholar]
- 15.Leinonen KM, Leinonen J, Bolstad NL, et al. Procedure time and filling quality for bulk-fill base and conventional incremental composite techniques-A randomised controlled in vitro trial. J Dent. 2023;138:104725. [DOI] [PubMed] [Google Scholar]
- 16.Vianna-de-Pinho MG, Rego GF, Vidal ML, et al. Clinical time required and internal adaptation in cavities restored with bulk-fill composites. J Contemp Dent Pract. 2017;18(12):1107–11. [DOI] [PubMed] [Google Scholar]
- 17.Medina-Sotomayor P, Ortega G, Aguilar J, et al. Dental restoration operative time and analysis of the internal gap of conventional resins (incremental technique) vs. bulk fill (single-Increment technique): in vitro study. J Clin Exp Dent. 2023;15(8):e621–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tardem C, Albuquerque EG, Lopes LS, et al. Clinical time and postoperative sensitivity after use of bulk-fill (syringe and capsule) vs. incremental filling composites: a randomized clinical trial. Braz Oral Res. 2019;33(0):e089. [DOI] [PubMed] [Google Scholar]
- 19.Durão MA, Andrade AKM, Santos MDCMDS, et al. Clinical performance of Bulk-Fill Resin Composite Restorations Using the United States Public Health Service and Federation Dentaire Internationale Criteria: a 12-Month Randomized Clinical Trial. Eur J Dent. 2021;15(2):179–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Akman H, Tosun G. Clinical evaluation of bulk-fill resins and glass ionomer restorative materials: a 1-year follow-up randomized clinical trial in children. Niger J Clin Pract. 2020;23(4):489–97. [DOI] [PubMed] [Google Scholar]
- 21.Ástvaldsdóttir Á, Dagerhamn J, van Dijken JW, et al. Longevity of posterior resin composite restorations in adults – A systematic review. J Dent. 2015;43(8):934–54. [DOI] [PubMed] [Google Scholar]
- 22.Ribeiro APD, Sacono NT, Soares DG, et al. Human pulp response to conventional and resin-modified glass ionomer cements applied in very deep cavities. Clin Oral Investig. 2020;24(5):1739–48. [DOI] [PubMed] [Google Scholar]
- 23.Bin-Shuwaish MS. Effects and Effectiveness of Cavity disinfectants in Operative Dentistry: A literature review. J Contemp Dent Pract. 2016;17(10):867–79. [DOI] [PubMed] [Google Scholar]
- 24.Demarco FF, Collares K, Correa MB, et al. Should my composite restorations last forever? Why are they failing? Braz Oral Res. 2017;31(suppl 1):e56. [DOI] [PubMed] [Google Scholar]
- 25.Demarco FF, Cenci MS, Montagner AF, et al. Longevity of composite restorations is definitely not only about materials. Dent Mater. 2023;39(1):1–12. [DOI] [PubMed] [Google Scholar]
- 26.Alqudaihi FS, Cook NB, Diefenderfer KE, et al. Comparison of internal adaptation of bulk-fill and increment-fill Resin Composite materials. Oper Dent. 2019;44(1):E32–44. [DOI] [PubMed] [Google Scholar]
- 27.Demirel G, Orhan AI, Irmak O, et al. Effects of Preheating and Sonic Delivery techniques on the internal adaptation of bulk-fill Resin composites. Oper Dent. 2021;46(2):226–33. [DOI] [PubMed] [Google Scholar]
- 28.Kim JH, Cho J, Lee Y, et al. The survival of Class V Composite restorations and analysis of marginal discoloration. Oper Dent. 2017;42(3):E93–101. [DOI] [PubMed] [Google Scholar]
- 29.Balkaya H, Arslan S, Pala K. A randomized, prospective clinical study evaluating effectiveness of a bulk-fill composite resin, a conventional composite resin and a reinforced glass ionomer in Class II cavities: one-year results. J Appl Oral Sci. 2019;27:e20180678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Balkaya H, Arslan SA, Two-year. Clinical comparison of three different restorative materials in class II cavities. Oper Dent. 2020;45(1):E32–42. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data of this research are available upon reasonable request from the corresponding author.


