Abstract
Purpose
(1) To determine the clinical outcomes following revision arthroscopy for patients with hip synovial chondromatosis (SC), and (2) to compare the clinical outcomes between patients undergoing revision hip arthroscopy and primary hip arthroscopy.
Methods
Patients undergoing hip arthroscopy between December 2014 and January 2021 was reviewed. Patients treated for SC and confirmed by postoperative pathology were included. Exclusion criteria were age less than 18 years old, hip osteoarthritis (Tönnis grade > 1), history of autoimmune disease, avascular necrosis, and Legg–Calve–Perthes disease. Patients undergoing revision surgery were included in the revision group, while those undergoing primary surgery were matched in a 1:4 ratio and included in the primary group. Preoperative and postoperative patient-reported outcome (PRO) scores including Visual Analog pain Scale (VAS), modified Harris Hip Score (mHHS), Nonarthritic Hip Score (NAHS), and international Hip Outcome Tool, 12-component form (iHOT-12) were collected and compared. The PROs and percentage of achieving minimal clinically important difference (MCID) and patient acceptable symptom state (PASS) of mHHS, iHOT-12, and NAHS were compared between the two groups.
Results
A total of 12 patients were included in the revision group, while 48 patients were included in the primary group. No significant difference was found in baseline characteristics (all with P > .05). No significant difference was found in the arthroscopic findings and procedures (all with P > .05). Both groups presented significant improvement of postoperative PROs compared to the preoperative PROs (all with P < .001). No significant difference was found in preoperative PROs between the two groups (all with P > .05). Postoperatively, the revision group presented inferior VAS (P = .007), mHHS (P = .007), iHOT-12 (P = .004), and NAHS (P = .028), as well as lower rate of achieving MCID of NAHS (P = .038), and PASS of mHHS (P = .003) compared to the primary group.
Conclusion
Patients undergoing revision arthroscopy for hip SC presented favorable clinical outcomes at minimum of 2-year follow-up, although the postoperative PROs, rate of achieving MCID, and PASS were lower compared to patients undergoing primary arthroscopy.
Level of Evidence: III.
Keywords: Synovial chondromatosis, Hip arthroscopy, Revision hip arthroscopy
Introduction
Synovial Chondromatosis (SC) is a benign synovium disease that commonly affects the hip joint [1]. The condition of SC is characterized by metaplasia of the synovial membrane and the formation of multiple calcified nodules [2]. Although the cause of hip SC remains unknown, the condition can lead to erosive changes and secondary osteoarthritis (OA) of the joint [3]. Patients with hip SC typically manifests as hip pain, decreased range of motion, mechanical locking, and stiffness that result in impaired hip function and poor quality of life [4].
Primary arthroscopic treatment including removal of loose bodies and synovectomy can yield favorable clinical outcomes [4–8]. The percentage of recurrence identified by a combination of clinical symptoms and imaging findings, was reported to be 7.1% in a systematic review. Among these patients, 12 out of 14 (85.7%) underwent subsequent surgery, with 9 (64.3%) underwent revision arthroscopy [3]. Recurrence of SC not only exacerbate morbidity but also have the potential to induce malignant transformation [4]. Therefore, receiving a timely revision surgery, holds the potential to enhance the prognosis for these patients. However, this topic was rarely addressed, and little is known on the clinical outcomes following revision arthroscopy [4, 6, 8, 9].
Therefore, the purposes of the present study are: (1) to determine the clinical outcomes following revision arthroscopy for patients with hip SC, and (2) to compare the clinical outcomes between patients undergoing revision hip arthroscopy and primary hip arthroscopy. It was hypothesized that patients undergoing revision arthroscopy could present favorable clinical outcomes, whereas these patients were expected to demonstrate inferior overall outcomes compared to patients undergoing primary arthroscopy.
Methods
Patient selection
After institutional review board approval, data were retrospectively reviewed for all patients who underwent hip arthroscopy between December 2014 and January 2021 at our institution. The inclusion criteria were as follow: underwent hip arthroscopic treatment for SC (diagnosed preoperatively on radiologic examinations, or discovered during arthroscopic treatment for femoroacetabular impingement syndrome [FAIS]: alpha angle [AA] > 55 degrees for cam-type impingement, lateral center edge angle [LCEA] > 40 degrees for pincer-type impingement, and presentation of labral tear or bone marrow effusion on MRI) [10, 11]. Among the included patients, recurrence of SC were considered to some of them with persistent hip pain and recurrence of loose bodies on postoperative CT or MRI after primary arthroscopy, and revision arthroscopy was performed for them [3]. Patients were excluded if they had: (1) age less than 18 years old; (2) hip osteoarthritis (Tönnis grade > 1); (3) history of autoimmune disease; (4) avascular necrosis, and (5) Legg–Calve–Perthes disease. Patients underwent revision arthroscopy were included in the revision group, while other only underwent primary arthroscopy were matched and included in the primary group.
Matching protocol
All of the included patients who underwent revision surgery were included in the revision group. Patients who underwent primary arthroscopy were matched in a 1:4 ratio using coarsened exact matching (CEM) with bins defined based on age categories (< 34, 34–50, or > 50 years), sex (male or female), and body mass index (BMI) categories (< 24, 24–30, or > 30), in order to effectively reduce imbalance within observational data when controlling for a few strong confounders [12–14].
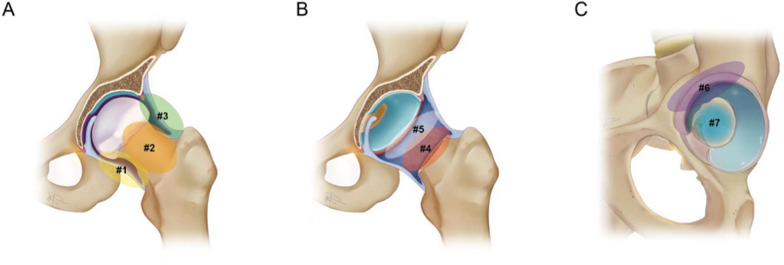
Surgical technique
Two senior surgeons (Y.X. and J.W.) with over 10-year experience in hip arthroscopy performed all operations using a standard supine approach [15] on a traction table (Smith & Nephew, Andover, MA).The arthroscopic inspection, removal of loose bodies, and synovectomy were orderly performed from the peripheral compartment to the central compartment (Fig. 1). The proximal mid-anterior portal (PMAP) and the mid-anterior portal (MAP) was firstly established. With PMAP being the viewing portal and MAP being the working portal, the arthroscopic inspection was started at the medial and anterior capsular recess without traction. The hip was gradually flexed and internal rotated for synovectomy and loose bodies removal. Switch the viewing portal to MAP, use PMAP and anterolateral portal (AL) to be the working portal, keep the hip in flexion and neutral position, synovectomy and loose bodies removal was performed at lateral capsular recess. After traction, extended capsulotomy for the iliofemoral ligament or the iliofemoral ligament plus the anterior part of ischiofemoral ligament (less than half) was made through AL along the posterior-inferior rim of the zona orbicularis. With MAP being the viewing portal and AL being the working portal, synovectomy and loose bodies removal was performed at the posterior site. After managing the peripheral compartment, arthroscopy was moved into the central compartment, using AL as the viewing portal and MAP as the working portal. In addition to removing loose bodies and synovectomy, labral debridement or repair was then performed according to the condition of labrum. Acetabular and femoral head cartilage was evaluated according to Outerbridge classification [16] and chondroplasty was performed for cartilage lesions and chondral flaps. If a cam lesion in the head-neck junction or acetabular over-coverage was identified, femoral or acetabular osteoplasty was performed. Finally, with the hip flexed by about 60 degrees, the joint capsule was sutured through PMAP and MAP at the 12, 1, 2, and 3 o’clock positions under AL inspection. During revision arthroscopy, there were requirements for addressing the adhesions and bleeding in the scar tissues to enhance accessibility. The steps and order of synovectomy, loose bodies removal, and managements for concomitant lesions were identical to primary arthroscopy. Loose bodies (Fig. 2) and synovium were evaluated using Milgram [17] classification and sent for pathological examination.
Fig. 1.
Revision arthroscopy for a 51-year-old man’s right hip. A The anterior capsular recess. B The medial capsular recess. C The lateral capsular recess. D The medial endpoint of extended capsulotomy at the iliofemoral ligament. E The lateral endpoint of extended capsulotomy at the iliofemoral ligament. F The posterior capsular recess. G The peri-labrum region. H The acetabular fossa. FN: femoral neck; FH: femoral head; L: labrum; *: loose bodies; arrow head: endpoint of capsulotomy
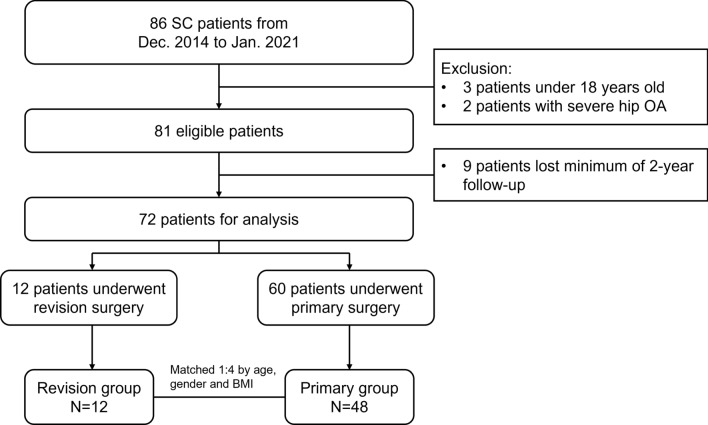
Fig. 2.
Loose bodies extracted from the hip joint
Rehabilitation protocol
A standardized rehabilitation protocol was implemented for all patients. Isometric contractions and passive range of motion exercises were initiated on day 1 to 2 after surgery. Partial weight-bearing exercises for restoring range of motion and promoting regular gait were introduced from day 3 to week 3, followed by full weight-bearing walking at week 4. Full weight-bearing muscle strength exercises and dynamic balance training began at week 6. Patients gradually resumed activities and returned to sports based on their tolerance.
Data collection
Patients’ demographic characteristics including age at surgery, sex, height, weight, body mass index (BMI), and duration from the onset of symptoms to the primary surgery were collected. For patients undergoing revision surgery, the interval between primary and revision surgery was collected.
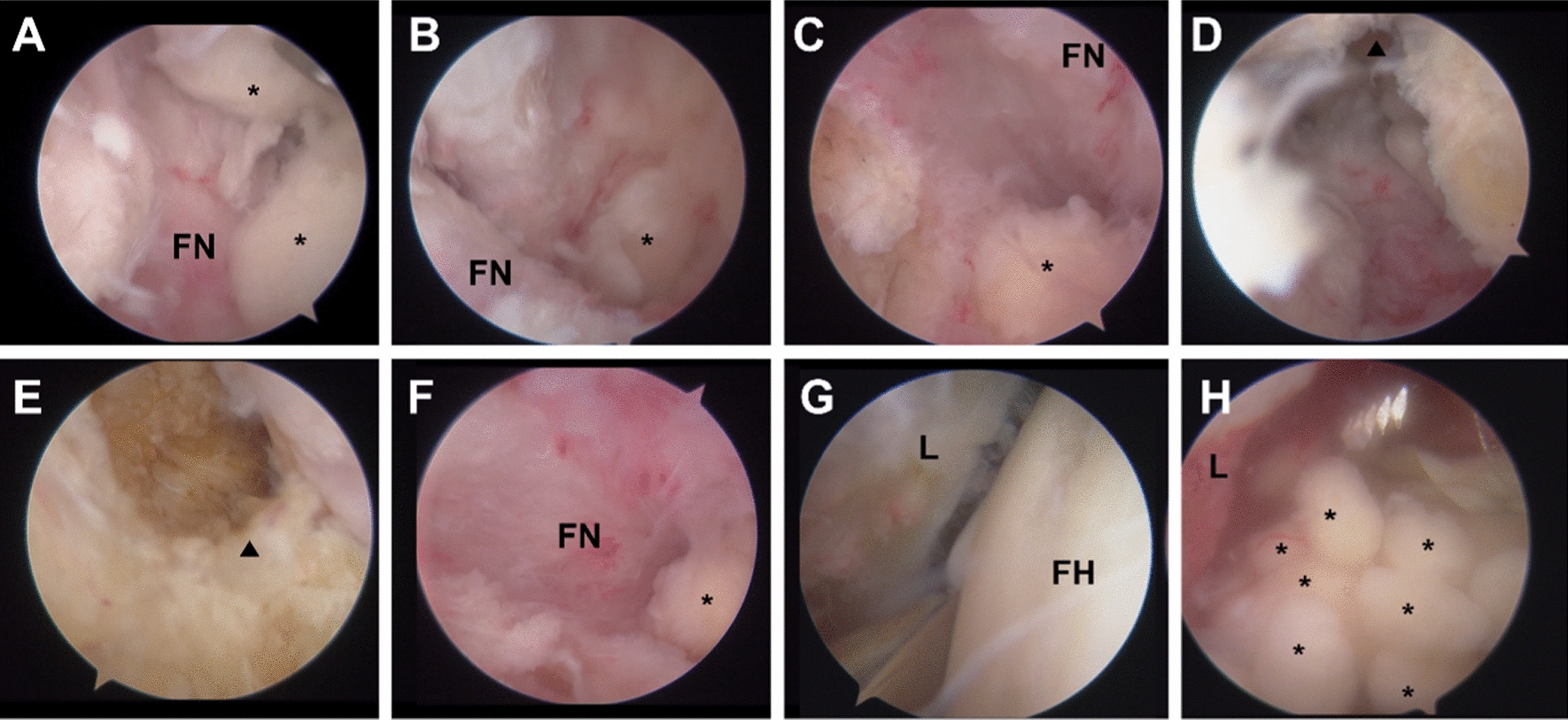
Hip radiography and CT were performed preoperatively to preliminarily locate loose bodies. The AA, LCEA, Tönnis grade and joint space were collected using methods described by previous studies [18–21]. Hip MRI examinations were performed preoperatively using a 3.0-T magnetic resonance scanner (Magnetom Trio with TIM system; Siemens Healthcare) to confirm the presentation of loose bodies and evaluate the condition of labrum, cartilage and ligaments. Immediate postoperative CT were performed on the day after surgery to confirm the removal of loose bodies. As shown in Fig. 3, we divided the hip synovium of both the peripheral and central compartments into7 regions as described by Zhu et al. [22]. The presence of residual loose bodies and their locations following primary arthroscopy were recorded based on immediate postoperative CT. For patients undergoing primary arthroscopy at other institutes, the residual loose bodies were determined on their early follow-up CT or MRI.
Fig. 3.
Regions of the hip synovium. A Region #1: the medial capsular recess; Region #3: the lateral capsular recess; Region #2: the anterior capsular recess, which is located between regions #1 and #3. B The posterior recess is divided into two portions by taking the rim of the zona orbicularis as the boundary. Region #4: posteroinferior recess; Region #5: posterosuperior recess. C Region #6: peri-labrum, which is defined as the synovial tissue attached to the labrum; Region #7: the acetabular fossa
Patient-reported outcomes (PROs) including Visual Analog pain Scale (VAS), modified Harris Hip Score (mHHS), Nonarthritic Hip Score (NAHS), international Hip Outcome Tool, 12-component form (iHOT-12) were used to assess hip function for all patients [23–25]. The PROs were assessed both preoperatively and at a minimum of 2-year follow-up for all patients. Cutoff values for the minimum clinically important difference (MCID) of the mHHS and iHOT-12 were calculated using a distribution-based method originally proposed by Norman et al. [26], in which the MCID cutoff was set to half the standard deviation of the preoperative outcome scores of the cohort. Patient acceptable symptom state (PASS) of mHHS, NAHS, and iHOT-12 defined by published studies were used: 74 for mHHS, 81.9 for NAHS, and 69.1 for iHOT-12 [27–29].
All preoperative data for the revision group were collected before the revision arthroscopy. The surgical procedures for the revision group were also collected at the revision arthroscopy.
Statistical analysis
All the data were analyzed by IBM SPSS Statistics 27.0 (SPSS Inc., Chicago, IL, USA). The Kolmogorov–Smirnov test was firstly performed to check for normal distributions. The Wilcoxon signed-rank test was applied for the skewed variables and paired t test was applied for the normally distributed variables to compare the preoperative and postoperative PROs. Pearson’s chi-square test was applied to compare the categorical variables between the two groups. Mann–Whitney U test and independent t test was applied to compare the skewed variables and normally distributed variables between the two groups. Statistical significance was considered when P < 0.05.
Results
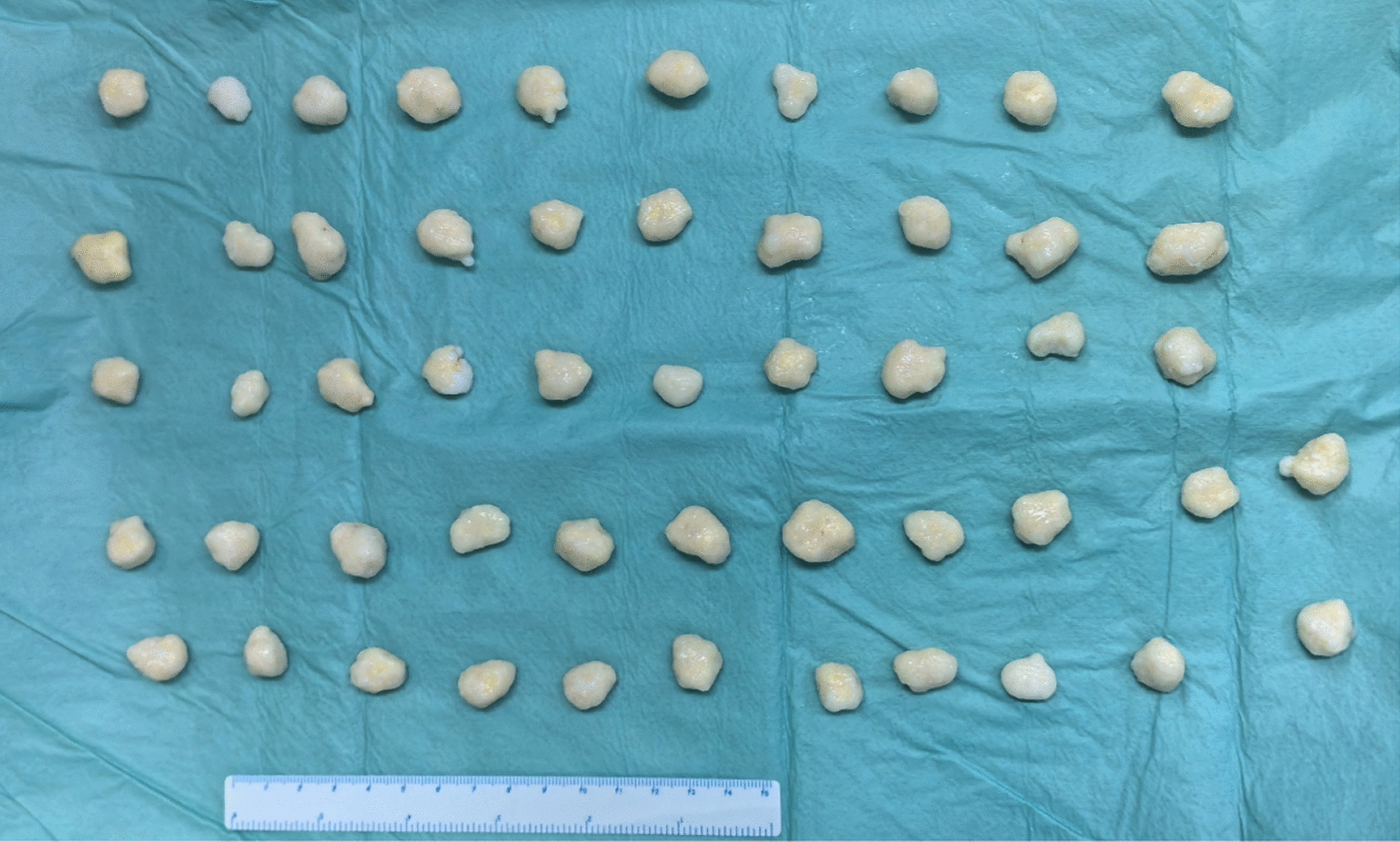
As shown in Fig. 4, a total of 60 patients were included in the study. Among them, 12 patients were included in the revision group, and 48 patients were matched and included in the primary group. The mean interval between primary and revision arthroscopy was 32.64 months (range 12–96 months). The detailed comparison of patients’ characteristics between the revision group and the primary group was listed in Table 1. No significant difference was found in age at surgery, sex, height, weight, BMI, AA, LCEA, Tönnis grade, joint space, symptom duration, and follow-up period between the two groups (all with P > 0.05).
Fig. 4.
Flow chart of patient selection
Table 1.
Comparison of patients’ characteristics between the two groups*
| Revision, N = 12 | Primary, N = 48 | P Value | |
|---|---|---|---|
| Age, years | 41.9 ± 11.9 (23–62) | 40.23 ± 12.1 (19–64) | 0.677 |
| Sex | 1 | ||
| Male | 7 (58.3) | 28 (58.3) | |
| Female | 5 (41.7) | 20 (41.7) | |
| Height, cm | 172.6 ± 7.3 (163–183) | 170.1 ± 6.5 (157–185) | 0.326 |
| Weight, kg | 71.0 ± 12.4 (50–92) | 71.6 ± 12.3 (47–110) | 0.882 |
| BMI, kg/m2 | 23.8 ± 3.7 (17.9–31.1) | 24.6 ± 3.1 (17.9–32.9) | 0.471 |
| AA, deg | 55.8 ± 11.7 (41.8–77.1) | 56.4 ± 12.4 (35.0–80.5) | 0.922 |
| LCEA, deg | 35.5 ± 7.2 (22.7–49.5) | 35.5 ± 9.5 (21.4–58.6) | 0.876 |
| Cam-type FAIS | 8 (66.7) | 28 (58.3) | 0.598 |
| Pincer-type FAIS | 3 (25.0) | 12 (25.0) | 1 |
| Tönnis grade | 0.690 | ||
| 0 | 4 (33.3) | 19 (39.6) | |
| 1 | 8 (66.7) | 29 (60.4) | |
| Joint space, mm | 4.6 ± 1.1 (2.7–6.7) | 4.3 ± 1.1 (2.3–7.3) | 0.442 |
| Symptom duration, months | 42.0 ± 35.3 (12–120) | 37.3 ± 37.8 (6–180) | 0.626 |
| Follow-up period, months | 40.5 ± 21.7 (24–97) | 40.6 ± 17.6 (24–100) | 0.643 |
*Values are presented as mean ± standard deviation (range). BMI body mass index, AA alpha angle, LCEA lateral center–edge angle
As shown in Table 2, the detailed comparison of arthroscopic findings and procedures were listed. No significant difference was found in the location of loose bodies and Milgram stage between the two groups (all with P > 0.05). Synovial hypertrophy was observed in all the patients. No significant difference of the procedure of labral repair, femoroplasty, and acetabuloplasty was found between the two groups (all with P > 0.05). The Outerbridge grade of the acetabular and femoral head cartilage did not present significant differences between the two groups (all with P > 0.05). Labral repair was performed in 9 patients and 23 patients in the revision group and the primary group, respectively (P > 0.05).
Table 2.
Comparison of arthroscopic findings and procedures between the two groups*
| Revision, N = 12 | Primary, N = 48 | P Value | |
|---|---|---|---|
| Location of loose bodies | |||
| Peripheral compartment | 12 (100) | 44 (91.7) | .301 |
| Central compartment | 9 (75.0) | 44 (91.7) | .108 |
| Milgram stage | .513 | ||
| Stage 2 | 6 (50.0) | 29 (39.6) | |
| Stage 3 | 6 (50.0) | 19 (60.4) | |
| Synovial hypertrophy | 12 (100) | 44 (100) | 1 |
| Labral repair | 9 (75.0) | 23 (47.9) | .093 |
| Femoroplasty | 8 (66.7) | 28 (58.3) | .598 |
| Acetabuloplasty | 3 (25.0) | 12 (25.0) | 1 |
| Acetabular cartilage | .162 | ||
| Outerbridge grade 0 | 2 (16.7) | 25 (52.1) | |
| Outerbridge grade 1 | 3 (25.0) | 7 (14.6) | |
| Outerbridge grade 2 | 2 (16.7) | 8 (16.7) | |
| Outerbridge grade 3 | 3 (25.0) | 6 (12.5) | |
| Outerbridge grade 4 | 2 (16.7) | 2 (4.2) | |
| Femoral head cartilage | .735 | ||
| Outerbridge grade 0 | 9 (75.0) | 39 (81.3) | |
| Outerbridge grade 1 | 2 (16.7) | 4 (8.3) | |
| Outerbridge grade 2 | 1 (8.3) | 3 (6.3) | |
| Outerbridge grade 3 | 0 | 2 (4.2) | |
| Outerbridge grade 4 | 0 | 0 | |
| Capsular repair | 12 (100) | 48 (100) | 1 |
*Values are presented as No. of hips (%)
As shown in Table 3, residual loose bodies were observed in 8 (66.7%) patients and 26 (54.2%) patients following primary surgery in the revision and the primary group, respectively. There was no significant difference in the rate and locations of residual loose bodies between the two groups (all with P > 0.05). The locations of residual loose bodies and recurrence of SC for each case in the revision group were demonstrated in Table 4.
Table 3.
Comparison of rate and locations of residual loose bodies following primary surgery between the two groups*
| Revision, N = 12 | Primary, N = 48 | P Value | |
|---|---|---|---|
| Residual loose bodies | 8 (66.7) | 26 (54.2) | 0.434 |
| Locations | |||
| Region #1 | 1 (8.3) | 4 (8.3) | 1 |
| Region #2 | 2 (16.7) | 6 (12.5) | 0.704 |
| Region #3 | 2 (16.7) | 6 (12.5) | 0.704 |
| Region #4 | 4 (33.3) | 14 (29.2) | 0.778 |
| Region #5 | 3 (25.0) | 15 (31.3) | 0.637 |
| Region #6 | 2 (16.7) | 11 (22.9) | 0.638 |
| Region #7 | 4 (33.3) | 11 (22.9) | 0.456 |
| Extra-articular | 3 (25.0) | 7 (18.4) | 0.386 |
*Values are presented as No. of hips (%)
Table 4.
Locations of recurrence in the revision group
| Locations of residual loose bodies | Locations of recurrence | |
|---|---|---|
| Case 1 | Region #1, #2, #3, #4, #5, #6, #7, extra-articular | Region #1, #2, #3, #4, #5, #6, #7, extra-articular |
| Case 2 | Region #7 | Region #3, #7 |
| Case 3 | N/A | Region #2 |
| Case 4 | Region #4, #6 | Region #4, #5, #6, extra-articular |
| Case 5 | Region #5 | Region #5, #7 |
| Case 6 | N/A | Region #1, #2, #3, #4, #5 |
| Case 7 | N/A | Region #5 |
| Case 8 | Region #4, #5, extra-articular | Region #2, #3, #4, #5, extra-articular |
| Case 9 | N/A | Region #6 |
| Case 10 | Region #7 | Region #7 |
| Case 11 | Region #7 | Region #1, #2, #3, #4, #5, #6, #7, extra-articular |
| Case 12 | Region #2, #3, #4, extra-articular | Region #1, #2, #3, #4, #5, extra-articular |
N/A, not applicable
Both groups showed improvement in all of the postoperative PROs compared to the preoperative PROs (all with P < 0.001). The comparison of preoperative and postoperative PROs between the two groups was presented in Table 5. No significant difference was found in all of the preoperative PROs between the two groups (all with P > 0.05). Postoperatively, the revision group presented inferior VAS (P = 0.007), mHHS (P = 0.007), iHOT-12 (P = 0.004), and NAHS (P = 0.028) compared to the primary group. No patients complained about the complications including wound infection and neuropraxia.
Table 5.
Comparison of patients' reported outcomes between the two groups*
| Revision, N = 12 | Primary, N = 48 | P Value | |
|---|---|---|---|
| Preoperative VAS | 4.8 ± 1.9 (2–8) | 3.8 ± 1.5 (1–7) | 0.165 |
| Postoperative VAS | 2.4 ± 2.3 (0–6) | 0.8 ± 1.2 (0–4) | 0.007 |
| Preoperative mHHS | 58.8 ± 11.9 (41–84) | 65.8 ± 12.7 (32–87) | 0.058 |
| Postoperative mHHS | 81.2 ± 16.9 (52–100) | 93.5 ± 6.7 (72–100) | 0.007 |
| Preoperative iHOT-12 | 44.7 ± 7.8 (33–56) | 49.6 ± 10.5 (23–74) | 0.111 |
| Postoperative iHOT-12 | 57.6 ± 17.4 (31–76) | 72.3 ± 9.0 (49–83) | 0.004 |
| Preoperative NAHS | 44.4 ± 6.8 (31–54) | 46.9 ± 7.2 (19–64) | 0.255 |
| Postoperative NAHS | 68.4 ± 19.3 (52–100) | 81.7 ± 8.6 (58–100) | 0.028 |
*Values are presented as mean ± standard deviation (range). VAS visual analog pain scale, mHHS modified Harris Hip Score, iHOT-12 international Hip Outcome Tool, 12-component form, NAHS Nonarthritic Hip Score. Boldface indicates statistically significant difference between groups (P < 0.05)
As shown in Table 6, the rate of achieving clinical thresholds were compared between the two groups. The MCID of mHHS, iHOT-12, and NAHS was calculated to be 6.8, 5.1, and 3.6 respectively. More patients in the primary group achieved MCID of NAHS (P = 0.038) than the revision group, while no significant difference was found in achieving MCID of mHHS (P = 0.053) and iHOT-12 (P = 0.108). A higher proportion of patients in the primary group achieved PASS of mHHS (P = 0.003), while no significant difference was observed in achieving PASS of iHOT-12 (P = 0.147) and NAHS (P = 0.364). One patient (8.3%) in the revision group underwent subsequent open surgery 6 months after revision arthroscopy, and conversion to total hip arthroplasty (THA) 12 months after the second revision surgery. The CT and MRI of this patient before and after revision surgery was presented in Fig. 5.
Table 6.
Comparison of percentage of patients achieving MCID and PASS between the two groups*
| Revision, N = 12 | Primary, N = 48 | P Value | |
|---|---|---|---|
| mHHS | |||
| MCID | 9 (75.0) | 45 (93.8) | 0.053 |
| PASS | 8 (66.7) | 46 (95.8) | 0.003 |
| iHOT-12 | |||
| MCID | 9 (75.0) | 44 (91.7) | 0.108 |
| PASS | 5 (41.7) | 31 (64.6) | 0.147 |
| NAHS | |||
| MCID | 10 (83.3) | 47 (97.9) | 0.038 |
| PASS | 4 (33.3) | 23 (47.9) | 0.364 |
*Values are presented as No. of hips (%). mHHS modified Harris Hip Score; iHOT-12 international Hip Outcome Tool, 12-component form; NAHS Nonarthritic Hip Score; MCID minimum clinically important difference; PASS Patient Acceptable Symptom State. Boldface indicates statistically significant difference between groups (P < 0.05)
Fig. 5.
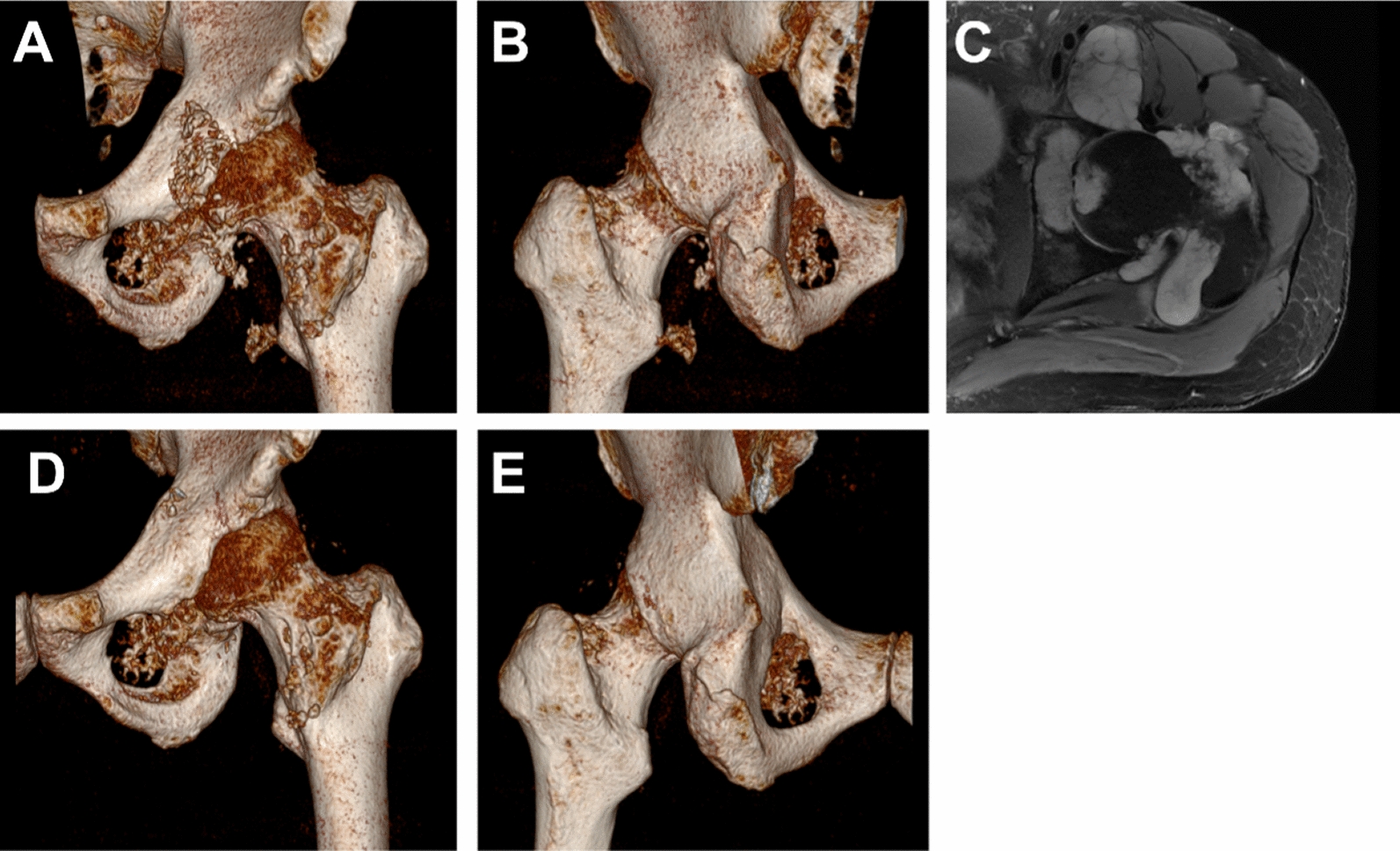
Preoperative and postoperative CT and MRI of a 48-year-old male undergoing revision arthroscopy. A, B Reconstruction of preoperative CT showed extensive loose bodies and bone erosion. C Preoperative MRI showed diffuse high signal intensity with T2-weighting, indicating synovial process diffusely involving the joint with bursal extensions. D, E Reconstruction of postoperative CT showed decreased number of loose bodies. The majority of residual loose bodies were observed in the region of the obturator externus
Discussion
The primary findings of the study were that patients undergoing revision arthroscopy for hip SC presented favorable clinical outcomes at minimum of 2-year follow-up, although the postoperative PROs, rate of achieving MCID, and PASS were lower compared to patients undergoing primary arthroscopy.
In the present study, primary arthroscopic treatment for hip SC demonstrated significant improvement of the PROs, which was consistent to previous studies [4–8]. Although some of the studies reported cases of recurrence, the clinical outcomes of this specific population were not reported and compared. To our expectation, the significant improvement of all of the PROs were also observed in the revision group, which suggested that revision arthroscopy could achieve favorable therapeutical effect. However, we found that patients in the revision group presented inferior postoperative PROs compared to the primary group. Similarly, these patients demonstrated lower rates of achieving MCID and PASS. The challenges associated with performing complete synovectomy and removing loose bodies during revision arthroscopy may exert a certain impact on the outcomes. Although arthroscopy has advantages of less invasion, reduced complications, better perioperative care, and fast rehabilitation compared to open surgery, it cannot provide easy access to the acetabular fossa and the posterior proximal aspect of the femur that are commonly affected by SC [5]. In our clinical practice, the management of revision arthroscopy treatment is challenged by the severe adhesion, elevated tension, and insertion of residual loose bodies into the erosive bone in these patients. It was reported that inadequate removal of synovium and loose bodies is one of the most common reasons for recurrence [3]. Therefore, we have developed and applied a standardized protocol in order to maximize the removal of loose bodies and synovium [15]. An extensive capsulotomy was performed for all patients to enhance accessibility. However, the accessibility is still limited and presents challenges, particularly in managing the posterior capsular and the region of obturator externus. Therefore, for the case presented persistent hip pain and residual loose bodies following revision arthroscopy in the present study, a subsequent open surgery was performed. The extensive capsulotomy also held the potential risk of residual loose bodies leaking [30]. Therefore, capsular repair was performed for all patients.
Among the 12 patients in the revision group, only 1 patient underwent second revision surgery and finally conversion to THA. Similarly, de SA et al. [3] conducted a systematical review and found a relatively satisfactory survivorship, with 1 out of 9 patients undergoing second revision surgery. However, caution should be exercised when interpreting the results of survivability due to the limited sample size and follow-up period.
In the present study, all of the demographic characteristics and radiographic parameters were comparable between the two groups. Relevant factors of recurrence have been preliminarily investigated in previous studies. Boyer et al. [9] and Zini et al. [4] suggested that increasing age may be a predictor to recurrence, while the similar results were not observed in other studies [6, 8]. The different exclusion criteria of OA may contribute to the difference, as Boyer et al. did not mention this aspect, and Zini et al. excluded patients with Kellgren-Lawrence grade > 2.
In addition to baseline factors, it is important to consider that various activities of SC may also exert an influence. Milgram et al. [17] classified SC into 3 stages. In Stage 1, metaplasia occurs in the synovial membrane without the presence of loose bodies. In Stage 2, progressive metaplasia results in the detachment of partially surrounded loose bodies by a synovial membrane. In Stage 3, metaplastic activity of the synovial membrane is restrained and multiple loose bodies can be observed within the joint. Boyer et al. [9] categorized patients into an active group (stage 1 and 2) and a quiescent group (stage 3), and compared the clinical outcomes. However, the recurrence rate was comparable between the two groups. Similar results were also found in the present study, as there was no significant difference in the proportions of Milgram stage 2 and 3 between patients who underwent revision and primary arthroscopy. In our clinical practice, loose bodies and pathological synovium containing gelatinous material were frequently observed under arthroscopy in a majority of patients from the revision group. Furthermore, we observed that revision surgery was performed in 8 out of 12 patients (66.7%) who presented radiographic recurrence within a 2-year period following primary arthroscopy. Although the correlation between various pathological features and recurrence remains unclear, we recommend surgeons to perform regular follow-up, particularly during the initial 2 years following primary surgery for these patients.
Interestingly, we observed a high prevalence of cam-type impingement concomitant to SC. FAIS is an abnormal contact between the proximal aspect of the femur and the acetabulum, which causes similar symptoms to SC such as hip pain and joint stiffness [2, 5]. Although idiopathic anatomic abnormalities of the femoral neck and the acetabulum are the most common causes of the cam- and the pincer-type impingement respectively, various etiologies have been proposed as causes of secondary FAIS. Concurrent presentation of SC and FAIS was observed in a subset of patients, as evidenced by radiography and arthroscopy [4, 5, 31]. Abolghasemian et al. [5] suggested that synovial inflammation at an early stage of SC and subsequent interposition of loose bodies was supposed to be the potential mechanisms underlying FAIS. Generally, residual cam-impingement was an important factor related to persistent hip pain and the result of revision surgery [32]. In the present study, a relative high rate of patients underwent femoroplasty during the revision process. However, no significant difference was found in Alpha angle and LCEA between the two groups, which suggested that impingement may not be the primary factor contributing to revision surgery rather than SC. We proposed that the cam-type impingement may be a subsequent condition of SC, while this topic still requires further study with dynamic radiographic examinations. Nevertheless, patients should be informed the potential risk of concomitant FAIS, and the necessity of more extensive surgery for treating both SC and FAIS.
Overall, the present study provided compelling evidence through the utilization of multiple validated PROs, facilitating comprehensive assessment of hip function across various dimensions. The results revealed that patients could expect significant improvements in their clinical outcomes following revision arthroscopy for treating hip SC. However, it is crucial for surgeons to provide critical context to these patients, as they may not experience the same level of satisfaction with their postoperative results comparing to primary arthroscopy.
Limitations
Several limitations in the present study must be acknowledged. Due to the retrospective nature of the study, selection and recall bias were inevitable. The sample size was relatively small and under power due to the rarity of SC. A prior power analysis was performed given the matching ratio to be 1:4, MCID of mHHS to be 8, and the standard deviation to be 10. A total of 80 patients were required to achieve a power of 0.8 when alpha was set as 0.05. Caution should be exercised when interpreter the results of comparison of clinical outcomes and achievement of clinical thresholds between the two groups, as there was a risk of beta error. Further study with a larger sample size and longer follow-up period was required in the future. The surgical technique applied in the present study necessitates extensive experience. Caution should be exercised when generalizing the outcomes to the entire population who underwent revision arthroscopy for hip SC. In the revision group, only 5 patients underwent primary arthroscopy at our institute. Therefore, we only collected preoperative and intraoperative data before and during the revision arthroscopy for this group. Although we considered SC as the most prominent factor for persistent pain and requirement of surgery in this cohort, over half of patients presented concomitant FAIS. Therefore, further study should include patients with isolated SC to eliminate the effect of FAIS.
Conclusion
Patients undergoing revision arthroscopy for hip SC presented favorable clinical outcomes at minimum of 2-year follow-up, although the postoperative PROs, rate of achieving MCID, and PASS were lower compared to patients undergoing primary arthroscopy.
Abbreviations
- SC
Synovial chondromatosis
- PRO
Patient-reported outcome
- VAS
Visual Analog pain Scale
- mHHS
Modified Harris Hip Score
- NAHS
Nonarthritic Hip Score
- iHOT-12
International Hip Outcome Tool 12-component form
- MCID
Minimal clinically important difference
- PASS
Patient acceptable symptom state
- OA
Osteoarthritis
- CEM
Coarsened exact matching
- BMI
Body mass index
- PMAP
Proximal mid-anterior portal
- MAP
Mid-anterior portal
- AL
Anterolateral portal
- AA
Alpha angle
- LCEA
Lateral center edge angle
- THA
Total hip arthroplasty
- FAIS
Femoroacetabular impingement syndrome
Author contribution
1. Conception and design of the study: Yichuan Zhu, Guanying Gao and Yan Xu. 2. Acquisition of data: Yichuan Zhu. 3. Analyses of data: Yichuan Zhu. 4. Drafting the work: Yichuan Zhu. Revising it critically for important intellectual content: Guanying Gao, Xin Zhang, Jianquan Wang and Yan Xu. 5. Final approval of the version to be published: Yichuan Zhu, Xin Zhang, Jianquan Wang, Guanying Gao, and Yan Xu.
Funding
The Capital Health Research and Development of Special (No. 2022-2Z-40915).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Guanying Gao, Email: gao-guan@126.com.
Yan Xu, Email: Yanxu@139.com.
References
- 1.Adelani MA, Wupperman RM, Holt GE. Benign synovial disorders. J Am Acad Orthop Surg. 2008;16(5):268–75. 10.5435/00124635-200805000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Maurice H, Crone M, Watt I. Synovial chondromatosis. J Bone Joint Surg Br. 1988;70(5):807–11. 10.1302/0301-620x.70b5.3192585. [DOI] [PubMed] [Google Scholar]
- 3.de Sa D, Horner NS, MacDonald A, Simunovic N, Ghert MA, Philippon MJ, et al. Arthroscopic surgery for synovial chondromatosis of the hip: a systematic review of rates and predisposing factors for recurrence. Arthroscopy. 2014;30(11):1499–504. 10.1016/j.arthro.2014.05.033. [DOI] [PubMed] [Google Scholar]
- 4.Zini R, Longo UG, de Benedetto M, Loppini M, Carraro A, Maffulli N, et al. Arthroscopic management of primary synovial chondromatosis of the hip. Arthroscopy. 2013;29(3):420–6. 10.1016/j.arthro.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 5.Abolghasemian M, Gharanizadeh K, Kuzyk P, Masdari Z, Fakharian M, Safir O. Hips with synovial chondromatosis may display the features of femoroacetabular impingement. J Bone Joint Surg Am. 2014;96(2): e11. 10.2106/JBJS.L.01550. [DOI] [PubMed] [Google Scholar]
- 6.Lee JB, Kang C, Lee CH, Kim PS, Hwang DS. Arthroscopic treatment of synovial chondromatosis of the hip. Am J Sports Med. 2012;40(6):1412–8. 10.1177/0363546512445150. [DOI] [PubMed] [Google Scholar]
- 7.Liu Y, Li J, Ma N, An M, Gao F, Hu B, et al. Arthroscopic treatment of synovial chondromatosis of hip joint. J Orthop Surg Res. 2020;15(1):405. 10.1186/s13018-020-01928-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marchie A, Panuncialman I, McCarthy JC. Efficacy of hip arthroscopy in the management of synovial chondromatosis. Am J Sports Med. 2011;39(Suppl):126S-S131. 10.1177/0363546511414014. [DOI] [PubMed] [Google Scholar]
- 9.Boyer T, Dorfmann H. Arthroscopy in primary synovial chondromatosis of the hip: description and outcome of treatment. J Bone Joint Surg Br. 2008;90(3):314–8. 10.1302/0301-620x.90b3.19664. [DOI] [PubMed] [Google Scholar]
- 10.Startzman A, Collins D, Carreira D. A systematic literature review of synovial chondromatosis and pigmented villonodular synovitis of the hip. Phys Sportsmed. 2016;44(4):425–31. 10.1080/00913847.2016.1216238. [DOI] [PubMed] [Google Scholar]
- 11.Griffin DR, Dickenson EJ, O’Donnell J, Agricola R, Awan T, Beck M, et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50(19):1169–76. 10.1136/bjsports-2016-096743. [DOI] [PubMed] [Google Scholar]
- 12.Ripollone JE, Huybrechts KF, Rothman KJ, Ferguson RE, Franklin JM. Evaluating the utility of coarsened exact matching for pharmacoepidemiology using real and simulated claims data. Am J Epidemiol. 2020;189(6):613–22. 10.1093/aje/kwz268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Torabian KA, Cherian NJ, Dean MC, Eberlin CT, Kucharik MP, Dowley KS, et al. Outcomes of hip arthroscopy in the setting of concomitant symptomatic lumbosacral spine pathology: a matched control study with minimum 24-month follow-up. Am J Sports Med. 2023;51(12):3268–79. 10.1177/03635465231197374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guy D, Karp I, Wilk P, Chin J, Rodrigues G. Propensity score matching versus coarsened exact matching in observational comparative effectiveness research. J Comp Eff Res. 2021;10(11):939–51. 10.2217/cer-2021-0069. [DOI] [PubMed] [Google Scholar]
- 15.Tian K, Gao G, Dong H, Zhang W, Wang J, Xu Y. Arthroscopic synovectomy of the hip joint: the regional surgical technique. Arthrosc Tech. 2022;11(7):e1181–7. 10.1016/j.eats.2022.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43:752–7. 10.1302/0301-620x.43b4.752. [DOI] [PubMed] [Google Scholar]
- 17.Milgram JW. The classification of loose bodies in human joints. Clin Orthop Relat Res. 1977;124:282–91. [PubMed] [Google Scholar]
- 18.Mansor Y, Perets I, Close MR, Mu BH, Domb BG. In search of the spherical femoroplasty: cam overresection leads to inferior functional scores before and after revision hip arthroscopic surgery. Am J Sports Med. 2018;46(9):2061–71. 10.1177/0363546518779064. [DOI] [PubMed] [Google Scholar]
- 19.Megerian MF, Strony JT, Mengers SR, Joseph NM, Salata MJ, Wetzel RJ. Use of anatomic radiographic horizons for the lateral center-edge angle in the classification of hip dysplasia. Am J Sports Med. 2022;50(13):3610–6. 10.1177/03635465221125784. [DOI] [PubMed] [Google Scholar]
- 20.Hiza E, Dierckman BD, Guanche C, Applegate G, Shah D, Ryu JH. Reliability of the tonnis classification and its correlation with magnetic resonance imaging and intraoperative chondral damage. Arthroscopy. 2019;35(2):403–8. 10.1016/j.arthro.2018.08.036. [DOI] [PubMed] [Google Scholar]
- 21.Reis P, Nahal-Said R, Ravaud P, Dougados M, Amor B. Are radiological joint space widths of normal hips asymmetrical? Ann Rheum Dis. 1999;58(4):246–9. 10.1136/ard.58.4.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhu Y, Gao G, Luan S, Wu K, Wang H, Zhang Y, et al. Longitudinal assessment of clinical outcomes after arthroscopic treatment for hip synovial chondromatosis and the effect of residual loose bodies: minimum 4-year and 8-year follow-up. Am J Sports Med. 2024;52(9):2306–13. 10.1177/03635465241260354. [DOI] [PubMed] [Google Scholar]
- 23.Byrd JW. Hip arthroscopy: patient assessment and indications. Instr Course Lect. 2003;52:711–9. [PubMed] [Google Scholar]
- 24.Griffin DR, Parsons N, Mohtadi NG, Safran MR, Multicenter Arthroscopy of the Hip Outcomes Research N. A short version of the International Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthroscopy. 2012;28(5):611–6. 10.1016/j.arthro.2012.02.027. [DOI] [PubMed] [Google Scholar]
- 25.Christensen CP, Althausen PL, Mittleman MA, Lee JA, McCarthy JC. The nonarthritic hip score: reliable and validated. Clin Orthop Relat Res. 2003;406:75–83. 10.1097/01.blo.0000043047.84315.4b. [DOI] [PubMed] [Google Scholar]
- 26.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–92. 10.1097/01.Mlr.0000062554.74615.4c. [DOI] [PubMed] [Google Scholar]
- 27.Nwachukwu BU, Beck EC, Kunze KN, Chahla J, Rasio J, Nho SJ. Defining the clinically meaningful outcomes for arthroscopic treatment of femoroacetabular impingement syndrome at minimum 5-year follow-up. Am J Sports Med. 2020;48(4):901–7. 10.1177/0363546520902736. [DOI] [PubMed] [Google Scholar]
- 28.Kemp JL, Collins NJ, Roos EM, Crossley KM. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am J Sports Med. 2013;41(9):2065–73. 10.1177/0363546513494173. [DOI] [PubMed] [Google Scholar]
- 29.Rosinsky PJ, Kyin C, Maldonado DR, Shapira J, Meghpara MB, Ankem HK, et al. Determining clinically meaningful thresholds for the nonarthritic hip score in patients undergoing arthroscopy for femoroacetabular impingement syndrome. Arthroscopy. 2021;37(10):3113–21. 10.1016/j.arthro.2021.03.059. [DOI] [PubMed] [Google Scholar]
- 30.Lee YK, Moon KH, Kim JW, Hwang JS, Ha YC, Koo KH. Remaining loose bodies after arthroscopic surgery including extensive capsulectomy for synovial chondromatosis of the hip. Clin Orthop Surg. 2018;10(4):393–7. 10.4055/cios.2018.10.4.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang X, Gao G, Wang J, Xu Y. Clinical outcomes after arthroscopic treatment of synovial chondromatosis in the hip. Cartilage. 2021;13(1_suppl):1324S-30S. 10.1177/1947603520912316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chapman R, Horner N, Ziauddin L, Hevesi M, Nho SJ. Patients undergoing revision hip arthroscopy demonstrate comparable survivability and improvement but worse postoperative outcomes compared to patients undergoing primary hip arthroscopy: a propensity matched study at five-year follow-up. Arthroscopy. 2024;40(3):802–9. 10.1016/j.arthro.2023.07.047. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.