Abstract
Education and training in disaster medicine for undergraduate medical students have been advocated for years in several countries. Despite the inclusion of disaster medicine into the medical curriculum being a reality in certain countries, such as the United States and Germany, it is still under scrutiny and yet to be embraced globally.
The objective of the study was to examine and map the range of literature and evidence available to support the inclusion of disaster education in the undergraduate medical curriculum and the identification of the related research gaps.
A scoping review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews methodology proposed by the Joanna Briggs Institute. A study protocol was designed and distributed to all the authors. English articles published in peer-reviewed journals were searched across various databases for the period between 2004 and 2021. Abstracts and available full texts referring to the incorporation of disaster health educational programs into the undergraduate medical curriculum in different forms and formats were included.
Sixty-four articles were collected from 2004 to 2021. The bulk of the articles published was from the USA (n = 24), Germany (n = 6), Italy (n = 5), Saudi Arabia (n = 4), the UK (n = 3), India (n = 3), and Canada (n = 3). The types of articles included were mainly survey studies (n = 26) and pilot studies (n = 12). Forty-six (71.9%) articles included were based on courses taught on disaster medicine. The modes of teaching used were mainly face-to-face, simulation, and e-learning. The curriculum covered in the taught courses included general principles of disaster medicine (n = 34), chemical, biological, radiological, and nuclear/bioterrorism (n = 10), and pandemics (n = 2). Thirty-three articles were based on a single course while 13 articles studied more than one course. Further research in disaster health education, establishing a concise undergraduate medical curriculum globally, using technology and simulation, training the faculty, and developing interdisciplinary disaster education programs were the significant gaps identified in this study.
Available literature supports the inclusion of disaster medicine into the undergraduate medical curriculum globally. However, the boundaries and the inclusion criteria of the basic disaster health educational program into the existing undergraduate medical curriculum must be defined and agreed upon.
Keywords: curriculum, disaster medicine, disaster medicine education, disaster planning, disasters, medical schools, medical students, undergraduate medical education
Introduction and background
Disasters are adverse events that seriously disrupt the routine life of communities and exhaust local, regional, and national resources. Natural, man-made, and technological hazards can be the cause, and multiple injuries and casualties can happen. The available resources are insufficient to cope with the immediate need for medical care and other health consequences for the affected community at large. Current climate alterations, outbreak events, and complex emergencies, such as in war-affected regions, which are often multifaceted, constitute some of the other serious threats occurring [1,2].
Educating and training, community members in general, and health workers in particular, in disaster medicine is fundamental to disaster preparedness and planning [3-5].
The Sendai Framework for Disaster Risk Reduction (SFDRR) 2015-2030 considers the increase of disaster preparedness of the health systems and the training capacities in the field of disaster medicine as one of the priorities of the disaster risk reduction strategies [6].
Health professionals’ postgraduate programs in emergency and disaster health are still limited worldwide [5,7], but even more when considering this kind of program for medical students.
Education and training in disaster medicine for medical students have been advocated for years as an essential step of the educational program in several countries, especially after certain significant events or disasters occur, such as the February 27, 2010, earthquake in Chile and the March 11, 2011, Fukushima nuclear disaster in Japan [8-11]. Disaster medicine has already become a part of the formal curriculum at several international medical schools in Sweden, the United States, Germany, Italy, and Saudi Arabia [3,12-15].
However, the development of disaster health education for medical students is still under scrutiny, is heterogeneous, dispersed in topics, and with limitations such as defining measurable learning objectives, practical contents, learning strategies, shortfalls in the evaluation process, and other learning outcomes. Disaster education encompasses a broader body of knowledge not always considered enough when planning or organizing disaster health learning programs for the different levels of education and training [16-25].
As far as we know, Cummings et al. published the first systematic review on the subject in 2006 [26]. It included an analysis of the education of medical students in this area and the courses provided to physicians in the public and military sectors [26]. Two years earlier (2004), the same two first authors had already published a proposal for a disaster medicine curriculum for Canadian medical schools [27]. Disaster education, including both medical care and public health modules, provided to undergraduate medical students might give them more confidence, essential knowledge, and adequate basic skills, which could contribute to surging the local capacity when a disaster occurs [26,27].
A scoping review can provide an enlarged and comprehensive review and analysis of relevant studies on this theme published during the last 17 years [28].
Objectives
The objectives of the study are to examine and map the range of literature and evidence available to include disaster education in the curriculum of medical schools as well as to identify research gaps regarding the potential impacts of incorporating disaster education into undergraduate medical programs.
Review
Methodology
Study Design
Frameworks for scoping reviews have been regularly developed and improved for almost 15 years by several authors to increase the clarity and quality of the review process [29,30]. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Extension for Scoping Reviews proposed by the Joanna Briggs Institute was used to develop this study [30,31].
Searching for previous existence and eventual registration of a scoping review on this topic was made in the Open Science Framework. Registration for the final study will be made prospectively [32].
To ensure consistency, an a priori protocol was designed, discussed, and distributed to the student (main author) and co-authors before the data collection. Peer-reviewed search literature was independently compiled and a review of the data and extracted results was made. The third individual, serving as both a co-author and supervisor, was tasked with resolving significant inconsistencies or disparities and ensuring that all collected data adhered rigorously to the established research methodology. Guidance on search terms and the screening strategy was also sought from an expert librarian.
Eligibility/Inclusion Criteria
The articles included in the study were published in English in peer-reviewed journals, between January 2004 and December 2021, with abstracts and full text available, and with a focus on any stage/phase of the pre-graduated physician education level (basic or advanced years of learning), and regional, local, or international context. Relevant reference lists and hand-searched articles were also included for the same period.
Population, Concept, and Context (PCC ) Approach
A PCC approach was used as proposed by the Joanna Briggs Institute [30]: population (undergraduate medical students, any stage/phase of medical education), concept (medical curriculum or learning programs in disaster health education, disaster medicine, and/or disaster planning or disaster preparedness, mentions to evaluation or effectiveness of programs or curricula tested or applied in the study), and context (any setting where undergraduate medical students were part of the target population, regional, local, or international context) were considered in the inclusion criteria.
Exclusion Criteria
Commentaries, editorials, book chapters, dissertation thesis, and conference abstracts or proceedings were also excluded from the study. Similarly, other grey literature was not included. Other health area students, such as nursing, pharmaceutical, paramedic, or other than physicians, were excluded.
Data Sources
Only peer-reviewed articles published from January 2004 to December 2021 were included. The reason for this specific period was that the first main systematic review on the topic was conducted in 2006 (medical students were a part of the studied population), and the first specific paper on the issue from the same authors was published in 2004 [26,27]. The data were collected from the electronic literature databases, including PubMed/MEDLINE (National Center for Biotechnology Information, National Institutes of Health, Bethesda, Maryland, USA), Scopus (Elsevier, Amsterdam, Netherlands), Web of Science Core Collection (Clarivate Analytics, Philadelphia, Pennsylvania, USA), and from the search engine Google Scholar (Google Inc., Mountain View, California, USA). Other sources included relevant reference lists from other papers and hand-searched articles from the journal “International Journal of Disaster Medicine” (Taylor & Francis).
Search Words and Phrases
The keywords searched during screening and article search contemplated terms such as “medical student(s)”, “undergraduate medical students”, “medical school(s)”, “curriculum”, disaster(s)”, “disaster medicine”, “disaster planning”, “disaster preparedness”, “disaster health education”, and “disaster medicine education” (Appendix 1).
Search and Screening Strategy
The search was conducted according to the current international research recommendations for each selected database (Appendix 2). The terms searched included the most relevant MeSH terms, relevant keywords, and free terms related to the type of study design. The Boolean operators were used to combine or exclude the search terms. The articles included in the study were screened in two phases. In the first phase, the articles were screened based on the relevance of the title and abstract, and then in the second one, full-text screening was performed.
Data Extraction
Mendeley (Elsevier B.V., Amsterdam, Netherlands) was used to compile the references, and Microsoft Excel 2007, version 12.0.4518.1014 (Microsoft Corporation, Redmond, Washington, USA) spreadsheet was used for data extraction.
Ethical Approval
Ethical approval is not a requisite for this kind of study. This study was conducted as a research thesis, a part of the Advanced Masters of Science in Disaster Medicine (European Masters in Disaster Medicine), and was approved by the Strategic Management Board of the Program.
Results
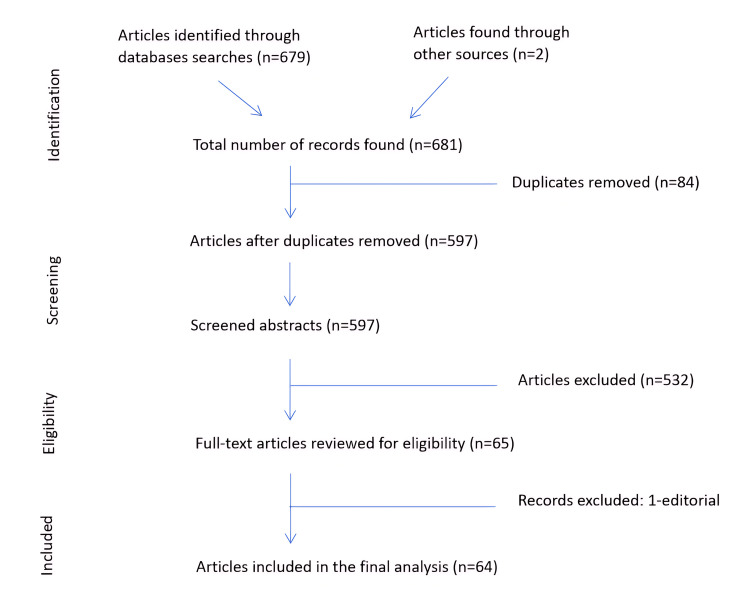
Based on the inclusion criteria, a total of 681 articles were identified during the search process in the first phase (Figure 1). Two articles were manually screened from the International Journal of Disaster Medicine. Sixty-four published study articles were finally selected based on the selection criteria. Studies' authors, year of publication, country of origin (where the study was published or conducted), type of studies, study population, adopted study method, and study analysis method used are presented in Table 1. The selected articles were reviewed on whether they supported the inclusion of disaster medicine in the undergraduate medical curriculum and for any study gaps identified by those studies.
Table 1. Summary of the selected study articles (n = 64).
AAMC: Association of American Medical Colleges; MCQ: multiple-choice questions; OSCE: Objective Structured Clinical Examination.
| Study reference | Year | Country | Type of study | Study population | Study method used | Study analysis method |
| Cummings G et al. [27] | 2004 | Canada | Survey | Medical students (undergraduate, fellowship, postgraduate) | Survey questionnaire | Survey analysis |
| Parrish AR et al. [33] | 2005 | USA | Interventional study | Medical students (72 2nd year - 2003-2004; 2004-2005) and course faculty (6 military experts) | Descriptive review /post-test and post-attitudinal questionnaire | Descriptive analysis/self-evaluation, attitudes & knowledge of the preparedness |
| Cummings GE et al. [34] | 2005 | Canada | Survey | 10 undergraduate and 14 fellowship program representatives (48 representatives and 15 Canadian medical schools) | Survey questionnaire (internet-based) | Survey analysis |
| Markenson D et al. [35] | 2005 | USA | Review study | 4 medical schools (physicians, public health, dental, nursing) | Author review of existing practices to deal with bioterrorism and development of core competencies for future | Expert analysis |
| Cummings G et al. [26] | 2006 | Canada | Systematic review | Medical students, physicians, medical military | Research studies critical review | Descriptive analysis |
| Subbarao I et al. [25] | 2008 | USA | Systematic review and Delphi study | All health professionals including medical students | Research studies expert working group review (18 persons)/3 round Delphi study | Review process + 3-stage Delphi process |
| Altintas KH et al. [18] | 2009 | Turkey | Survey | Medical students (191 1st-year and 232 6th-year students) | Survey questionnaire | Chi-square test |
| Kaiser HE et al. [36] | 2009 | USA | Survey | 523 medical students | Web-based survey questionnaire | Descriptive data analysis |
| Merlin MA et al. [37] | 2010 | USA | Survey | 49 (4th year) medical students | Pre- and post-rotation questionnaires | Simple paired t-test |
| Kaji AH et al. [38] | 2010 | USA | Pilot study | 6 medical students (4th year) | Summative feedback questionnaire-structure & utility of the course, 73-item oral exam, final lecture present | Survey analysis |
| Pfenninger EG et al. [39] | 2010 | Germany | Pilot study | Medical students, course faculty, and representatives of professional, societal, and government bodies | Curriculum development 6-step approach. Pilot testing (faculty & student feedback pilot versions of curriculum) during 2 years (pilot courses). Survey of all physicians (n = 477), German county disaster management agencies & district health authorities for additional input into disaster medicine needs competencies. Pre- and post-course questionnaire (oral &/or written final examination, comparing test results pre & post program, student & faculty summative and formative course evaluation | Survey analysis |
| Franc-Law J et al. [40] | 2010 | Italy | Prospective observational cohort | 22 medical students by year of education (random 50% interventional group; 50% control group) | Performance indicator scoring system, student evaluation questionnaire | R statistical analysis, χ2 test |
| Kaji AH et al. [41] | 2010 | USA | Descriptive and qualitative analysis | Medical students | Scored evaluation of the seminar, focus group discussion | Descriptive and qualitative analysis |
| Scott LA et al. [42] | 2010 | USA | Pilot study-Delphi study | Medical students (4th year) | Pre- and post-course questionnaire | Modified Delphi technique |
| Saiboon IM et al. [43] | 2011 | Malaysia | Survey | 45 medical students (5th year) | Pre- and post-lecture questionnaire (14 points) | Paired t-test |
| Carney JK et al. [44] | 2011 | USA | Survey | 3 classes of 115 medical students each/different institutions/different years: 1st, 2nd, and 4th year | Survey of workshops | Survey analysis |
| Datta R et al. [45] | 2012 | India | Review article | Undergraduate and postgraduate medical students and doctors | Author review, pre and post-lecture questionnaire | Author opinion, survey analysis |
| Smith J et al. [46] | 2012 | USA | Pilot survey | Educational liaison of 29 medical schools accredited by AAMC | Electronic on-line survey | Survey analysis |
| Scott LA et al. [47] | 2012 | USA | Delphi Study | 10 medical students and 17 emergency physicians, nurses, and emergency managers | Task force-Delphi process (development of competencies for the course) + small group exercises | Task force-Delphi process (development of competencies for the course) + small group exercises |
| Markenson D et al. [48] | 2013 | USA | Survey | Undergraduate medical, dental, and nursing students | Web-administered survey questionnaire | Survey analysis/comparative study |
| Su T et al. [49] | 2013 | China | Survey | 547 health professionals, 456 medical students, 1526 local residents | Self-reporting questionnaire survey | Descriptive analysis, chi-square, linear regression analysis |
| Ragazzoni L et al. [50] | 2013 | Italy | Survey | Medical students registered as members of the International Federation of Medical Students' Associations (undergraduate 1st to 6th year) and supplementary year (13) and post-graduate (4) | Web-based survey questionnaire (14 questions/4 groups) | Survey analysis |
| Jasper E et al. [51] | 2013 | USA | Survey | 130 new incoming interns at an academic teaching hospital | Questionnaires | Survey analysis |
| Grossi F et al. [52] | 2014 | Italy | Case-control study | Medical students = 125 (3rd to 6th year)/2 groups - 125 experimental group and 105 control (grade 44 students) | Case/control study (2 groups), pre and post-knowledge and attitude tests post a peer-reviewed course | Descriptive analysis, t-test, Wilcoxon–Mann–Whitney, and Wilcoxon signed rank test |
| Ingrassia PL et al. [14] | 2014 | Italy | Pilot study | 524 - 4th, 5th, and 6th-year medical students (21 medical schools corresponding to 52.5% of all Italian med schools) | Development course (six-step approach) and satisfaction and knowledge questionnaires + pre-test + post-test after completing the course (25 MCQ) | Survey analysis |
| Afzali M et al. [53] | 2015 | Denmark | Descriptive analysis | 66 medical students (3 groups of 16 and 1 group of 18) | Post-course student evaluation of the course and self-assessment | Descriptive analysis |
| Harmer A et al. [54] | 2015 | UK | Descriptive, case study | All director’s global health programs directors, 15 universities, UK undergraduate (6 programs) and postgraduate global health students (25 programs, both medical and non-medical) | Survey questionnaire | Survey analysis |
| Pollard KA et al. [55] | 2015 | USA | Pilot study | 52 medical students + pre-medical students, resident doctors (total = 45) | Student performance evaluation, pre and post-test questionnaire | Paired t-test |
| Mortelmans LJ et al. [56] | 2015 | Netherlands | Survey | 4408 (university total) - 5th and 6th senior medical students (from 6 to 8 faculties) | Descriptive cross-sectional survey (10 theoretical and practical case questions (validated)) | Survey analysis |
| Bajow N et al. [57] | 2015 | Saudi Arabia | Pilot study | Health expert stakeholders and international expert communities on disaster medicine, medical undergraduates | Questionnaire and interviews | Survey analysis |
| Bajow N et al. [58] | 2015 | Saudi Arabia | Survey | 30 medical schools - academic medical affairs directors | Online survey questionnaire (25 items) | Descriptive analysis, t-test, chi-square |
| Mohamed-Ahmed R et al. [59] | 2015 | UK | Interventional study | 27 students | Pre and post-test sessions evaluation forms (self-rate confidence in 8 learning domains)/qualitative + quantitative | Descriptive quantitative analysis, Wilcoxon signed-rank test |
| Bajow N et al. [15] | 2016 | Saudi Arabia | Pilot study | 29 medical students (15 male; 14 female) of 4th, 5th, and 6th year at Jazan University, Saudi Arabia | Develop a 5-stage approach (video lecture, workshops, group discussion; role-playing, mock & experimental learning, computer games, training for community education). Pre and post-course questionnaire, self-assessment, 3rd level of Kirkpatrick's evaluation | Wilcoxon test for paired samples |
| Barrimah I et al. [60] | 2016 | Saudi Arabia | Survey | 250 medical students (clinical phase) and teachers of the college, emergency physicians, and health administrators (interviews) | Quantitative and qualitative analysis of questionnaire + interviews | Survey analysis and SPSS for qualitative analysis |
| Mortelmans LJ et al. [61] | 2016 | Belgium | Survey and comparative study | All military students in medical sciences (not only medicine/27% senior level) & 999 civilian medical students | 10 theoretical and practical questions + comparison with previous similar data from med students | Survey comparative analysis + statistical analysis |
| Cole LA et al. [62] | 2016 | USA | Survey | 14 medical students (4th year) | Post-course student evaluation of the course | Descriptive analysis |
| Wunderlich R et al. [13] | 2017 | Germany | Prospective, cross-sectional, observational survey | All medical students of 37 German medical schools | Web-based, purpose-designed questionnaire | Survey analysis statistical analysis (descriptive + quantitative) |
| Jasper EH et al. [63] | 2017 | USA | Survey | 503 medical students (1st year) | Questionnaire (23 questions) | Survey analysis |
| Prihatiningsih TS et al. [64] | 2017 | Indonesia | Randomized controlled trial | 72 (3rd year) students of medicine, nursing, and health and nutrition programs at 1 university in Indonesia, 36 randomized interventional studies, and 36 randomized for control group | Randomized controlled trial | Descriptive mixed-method analysis |
| Yasui K et al. [11] | 2017 | Japan | Review article | Undergraduate and postgraduate medical students | Narrative review of published articles in several databases and focus on 3 new representatives of the curriculum of Japanese medical education that started after the Great East Japan Earthquake | Author analysis |
| Kim TE et al. [65] | 2017 | USA | Interventional study | 402 undergraduate medical, nursing, and pharmacy students | Pre-course and post-course assessments online (performance, leadership, teamwork, course satisfaction) | Qualitative analysis |
| Patel R et al. [66] | 2017 | USA | Survey | 631 medical, nursing, and pharmacy students | Survey questionnaire | Two-way ANOVA, post hoc analysis |
| Verson J et al. [67] | 2018 | USA | Pilot study | 28 medical students (1st year) | Exercise via email city-wide drill simulating a large-scale aerosolized release of Bacillus anthracis/arriving ED hospital post-call | Author opinion, descriptive analysis of drill |
| Drees S et al. [68] | 2018 | Germany | Descriptive study | 89 Medical students | Author review of 7 workshops and the game "AFTERSHOCK" + survey "student self-evaluation" + written evaluation | Survey analysis |
| Wiesner L et al. [21] | 2018 | USA | Interventional study | 2 cohort of studies - 30 medical students, 1st cohort and 51 medical students, 2nd cohort (from all class years) (2nd-year medical students) | 10 questions of multiple-choice (prior to and after each training session) + statistical analysis | Paired t-test |
| Patel VM et al. [69] | 2018 | USA | Interventional study/survey | 55 medical students | Pre-elective, post-lesson, and post-elective questionnaire | Survey analysis |
| Scott LA et al. [70] | 2018 | USA | Interventional study/survey | 708 participants (31.9% medical students, 49.9% physicians, 7.2% nurses, and 11% allied health professionals) enrolled in a university between 2011 and 2014 | Facilitator observation, pre and post-testing, and a course evaluation | Descriptive analysis, unpaired t-tests |
| Kommor MB et al. [12] | 2019 | USA | Pilot study | 68 medical students (2nd year - 47; third year - 21) | Retrospective questionnaire (survey for evaluation of the program) | Survey analysis |
| Back DA et al. [71] | 2019 | German | Pilot study | 51 medical students (3rd year) | Pre and post-course multiple-choice tests and questionnaire | Survey analysis |
| Rezaee R et al. [72] | 2019 | Iran | Delphi survey | 15 medical and disaster experts | Delphi questionnaire (2 rounds) | Survey analysis |
| Gouda P et al. [73] | 2020 | Ireland | Survey | About 830 medical students of an Ireland university | Online survey questionnaire | Pearson’s chi-square correlation, independent t-tests, and multinomial regression |
| Ragazzoni L et al. [74] | 2020 | Italy | Interventional study | 2316 medical students from 2014 to 2018/41 medical students become trainers (2013-2018) and students’ teacher | Demographic questionnaires, pre-test and post-tests, and satisfaction questionnaires | Survey analysis |
| Tsai YD et al. [75] | 2020 | Taiwan | Pilot study | 230 medical students | Questionnaire (knowledge at the beginning and end of training) - 10 MCQs | Survey analysis |
| Gillani AH et al. [76] | 2020 | Pakistan | Survey | 310 students, medical and pharmacy undergraduate students | Pretested and validated self-administered questionnaire | Independent t-test, one-way ANOVA, Pearson correlation, and regression analyses |
| Panda M et al. [77] | 2020 | India | Survey | Medical students | Predesigned semi-structured questionnaire | Survey analysis |
| Rajesh G et al. [78] | 2020 | India | Survey | 437 final-year students pursuing medicine (114), dentistry (86), nursing (42), physiotherapy (53), pharmacy (58), Ayurveda (23), and homeopathy (61) of 7 institutions in Mangalore and health professions | Questionnaire - 42 items (26 = knowledge; 8 = attitude; 8 = behavior) | Descriptive analysis, linear regression analysis |
| Ponampalam R et al. [79] | 2021 | Singapore | Survey | 250 medical students/10 in rotation every 3 months | MCQs, quizzes, and OSCE | Survey analysis |
| Ashcroft J et al. [80] | 2021 | UK | Systematic review | 23 studies met the inclusion criteria | Research studies critical review | Descriptive analysis |
| Al-Ziftawi NH et al. [81] | 2021 | Qatar | Survey | Medical, pharmacy, and health sciences students | Pretested and pre-validated survey questionnaire | Student's t-test, analysis of variance, correlation, and linear regression |
| Hermann S et al. [82] | 2021 | Germany | Prospective and cross-sectional survey | 102 medical students (5 courses from 2018-2020)/(3rd, 4th, and 5th year) | 3 survey tools | Paired sample t-test |
| Park H et al. [83] | 2021 | S. Korea | Scoping review | 57 papers met inclusion criteria | Arksey and O’Malley’s protocol methodology | Quantitative and thematic content analysis |
| Kasselmann N et al. [84] | 2021 | Germany | Survey | Deans of 36 German medical schools | Online questionnaire | Survey analysis, descriptive statistics |
| Saiboon IM et al. [85] | 2021 | Malaysia | Prospective cross-sectional survey | 168 pre-clinical year medical students | Validated online questionnaire | Survey analysis |
| Gable BD et al. [86] | 2021 | USA | Survey | Medical students | Pre and post-test questionnaire | Paired analysis, Wilcoxon signed-rank sum test |
Figure 1. PRISMA flow chart for the selected studies.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
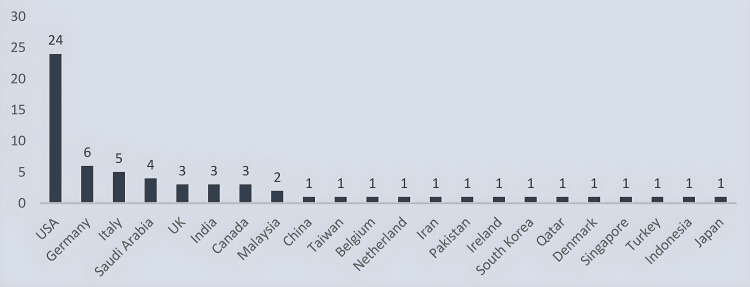
After passing through all the screening phases, 64 articles were selected to be included in this scoping review. Most of the articles were published in the USA (n = 24/38%). Six articles were from Germany while four articles each were of Italian and Saudi Arabian origin. There were three articles each from the UK, India, and Canada. Malaysia contributed two articles while one article each from China, Taiwan, Belgium, Netherlands, Iran, Pakistan, Ireland, South Korea, Qatar, Singapore, Denmark, Turkey, Indonesia, and Japan was made part of the study (Figure 2).
Figure 2. Country of origin of the selected studies (n = 64).
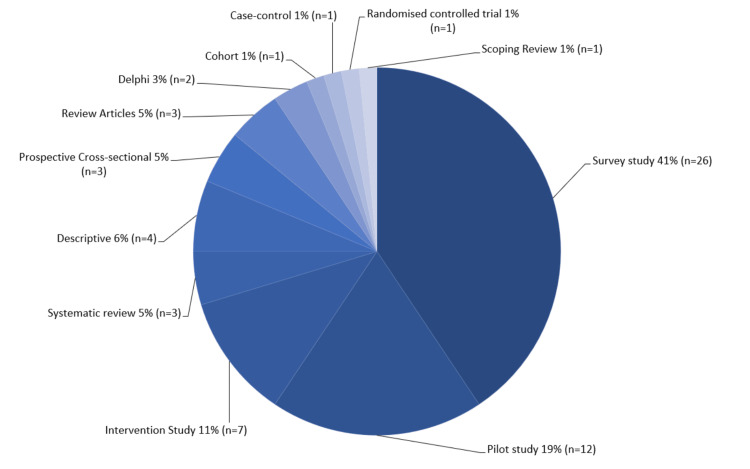
Twenty-six (41%) of the studies included were survey studies while 12 (19%) were pilot studies. Seven interventional studies, four descriptive studies, and three systematic reviews were included in this scoping review. In addition, three were cross-sectional studies and review articles. Two Delphi studies, one scoping review, one case-control study, one cohort study, and one randomized control study were also made part of this scoping review (Figure 3).
Figure 3. Types of selected studies (n = 64).
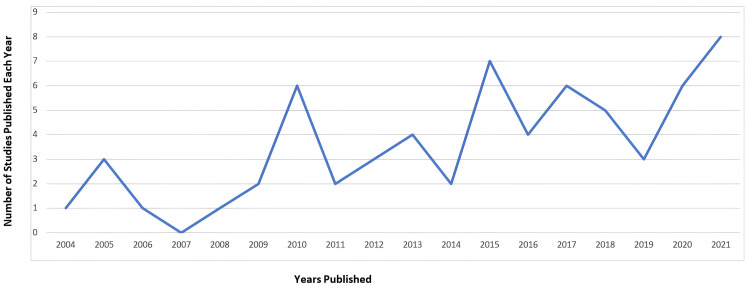
A directly proportional relation was noted between the number of articles published on disaster medical education for undergraduate medical students and every passing year. The highest number of articles included in the study were published in the year 2021 (n = 8) (Figure 4).
Figure 4. Year of publication of the selected studies (n = 64).
Overall, two main groups of articles were identified: one focusing on the organization, implementation, and follow-up of courses in disaster medicine for medical students (n = 46/71.9%), and the other primarily addressing self-perception or self-knowledge of students/other health professionals student respondents.
Mode of Education for the Courses in the Selected Studies
There were 46 articles in this scoping review involving educational courses on disaster medicine using different teaching modalities. Most of the study courses were a combination of face-to-face lectures and simulation (n = 31) whereas other taught courses used e-learning in addition to face-to-face and simulation methods (n = 8). The courses in two studies were based only on e-learning while in one study, the course was taught using simulation methods only. Three studies used a face-to-face and e-learning blended approach to teach their students while in one study, the course was taught via an e-learning and simulation method.
Curriculum of the Taught Courses in the Studies Selected
The curriculum taught in these courses was mainly general principles of disaster medicine (n = 34) [87] while chemical, biological, radiological, and nuclear disasters or bioterrorism was also a favorite topic taught in these courses (n = 10). Two articles included in this review were focused on COVID-19 and pandemics, i.e., health disasters.
Mandatory or Optional and Single or Multiple Taught Courses in the Selected Studies
Out of 46 articles based on taught courses, 36 articles studied optional or non-compulsory courses, i.e., not part of the mandatory curriculum, eight articles included courses based on mandatory curriculum while two articles had a combination of both mandatory and optional courses. Thirty-three articles were based on a single course while 13 articles made more than one course part of their study.
All the study articles suggested the inclusion of disaster medicine into the undergraduate medical curriculum.
Discussion
Education of disaster medicine for undergraduate medical students has been well advocated [13-15]. Education in disaster medicine has grown in popularity over recent times.
Disaster medicine education for undergraduate medical students is a relatively new and evolving field. Many studies included in this article recommend further research in disaster medicine education at the undergraduate level. Cummings et al. (2006) proposed that the available disaster medicine courses were well-documented and needed to be further studied, peer-reviewed, and indexed [26]. Jasper et al. (2017) recommended that the focus of future education research should be on developing interdisciplinary curricula to ensure that disaster medicine is taught across all undergraduate years [63]. Further research with a large sample size was suggested by Grossi et al. (2014) to differentiate between the traditional vertical teaching method and peer-led training in disaster medicine education [52]. Kim et al. (2017) suggested continuous research to demonstrate sustained improvement in the course and its clinical benefits [65]. Merlin et al. (2010) and Scott et al. (2018) emphasized the importance and need to find the areas of further research on disaster medicine education [37,70], while Gouda et al. (2020) pointed out the need for research and further experiences to establish disaster training programs and to find out appropriate roles of medical students during a disaster [73]. Scott et al. (2010) advocated the necessity of research to validate core competencies and to set out performance-based education goals in disaster medicine [42].
A blended approach, combining traditional lecture and simulation techniques, has been suggested by Ingrassia et al., Drees et al., and Panda et al. for better learning outcomes [14,68,77]. Similarly, Herman et al. (2021) studied a broader scope of virtual reality training in disaster medicine [82]. Park et al. (2021) highlighted the use of telemedicine, which helped a great deal during the COVID-19 pandemic [83]. Saiboon et al. (2011), Datta et al. (2012), Su et al. (2013), Patel et al. (2018), and Kasselmann et al. (2021) supported the use of e-learning and simulation for disaster medical training for ease of use and efficacy [43,45,49,69,84]. Saiboon et al. (2021) suggested that e-learning was beneficial in cognitive learning, but the complex decision-making knowledge was better taught as practical face-to-face learning [85].
Ragazzoni et al. (2013), Jasper et al. (2013), Mortelmans et al. (2015), Barrimah et al. (2016), Gouda et al. (2019), Gillani et al. (2020), and Al-Ziftawi et al. (2021) found that the medical undergraduates expressed keen interest in learning disaster medicine and willingness to be a part of the disaster response team in case of an adverse event [50,51,56,60,73,76,81]. Moreover, Gillani et al. (2020) showed a positive correlation between knowledge and attitude toward disaster medicine learning among healthcare professionals [76].
Bajow et al. (2015) suggested that most of the participating medical schools were willing to make disaster education a part of the undergraduate curriculum but were unable to do so due to the lack of trained staff [57]. Prihatiningsih et al. (2017) cited that already saturated undergraduate curricula, lack of financial resources, and assistance from the faculty and administration were the hurdles to implementing inter-professional disaster education [64].
Two articles studied military and civilian disaster training. Mortelmans et al. (2016) compared military with civilian medical undergraduates and found that military undergraduates had an overall better grasp and were more competent in dealing with a disaster as compared to civilian undergraduates [56] while Back et al. (2019) suggested that merging civilian and military disaster training programs would bring forth collaborated and multifaceted approach and might open up new avenues in disaster education [71].
Many educational and training courses, workshops, and seminars have been run in different countries, specially designed for undergraduate medical students [11,12,21]. Despite the literature evidence supporting the inclusion of disaster medical education in the undergraduate medical curriculum, disaster medicine has not yet been accepted worldwide by numerous medical schools, with some exceptions in the USA, Germany, Italy, and Saudi Arabia [13,14,21,39,50,58,84]. The Association of American Medical Colleges has strongly recommended including disaster medicine in the undergraduate medical curriculum to prepare health professionals for mass casualty incidence response [12,84]. The main reasons for disaster medical education not being part of the undergraduate medical curriculum were lack of resources and absence of organizational structure [84], scarcity of trained staff to train the medical students [57,58], lack of awareness about disaster medicine [50,60], and no formulated curriculum framework for the undergraduate medical students [14,51].
We still noticed that most of the studies do not have a strong evidence-based hierarchy. No study aimed at evaluating the validity of the course except one Italian study in 2014 by Ingrassia et al. (2014) that was conducted to evaluate the validity of disaster medicine training for undergraduate medical students in Italy [14]. It highlights the absence of a valid and uniformly accredited disaster medicine curriculum for medical undergraduates globally. The articles based on taught courses included in this scoping review had their own limitations. The barriers or limitations described in these articles were mainly selection bias, participant bias, time constraints, and a small study population affecting the validation of the study.
Limitations
This study did not include articles in languages other than English. Another important limitation is that grey literature was not included in the literature search. Both could have eventually limited the number of additional information important to the study. We believe that most cited and referenced papers were mentioned, and one cannot neglect that used search strategies could influence the number of results.
Conclusions
Disaster medicine education has not yet been embraced as a part of the undergraduate curriculum. If this subject is introduced gradually at different stages of medical training and on a global scale, it could have a huge impact.
This scoping review identified the need for (a) more research in the field of disaster medicine education, (b) better-designed quality studies with bigger samples, (c) planning interdisciplinary and competency-based curricula for disaster medicine training, and (d) use of the modern technology and simulations for training.
Acknowledgments
This article is a 'Research Thesis' as a part of the Advanced Masters of Science in Disaster Medicine, a program offered in combination by the University of Piemonte Orientale, Novara, Italy and Vrije Universiteit, Brussel Belgium. Dr. Pereira and Dr. Alexakis were the supervisor and co-supervisor, respectively, and contributed to the conceptualizing, acquisition, analysis, and interpretation of the data, critical review of the data, and supervised the whole thesis. We collaborated via Zoom, emails, and the Università degli Studi del Piemonte Orientale student and supervisor portal for the Advanced MSc (EMDM) Program. Unfortunately, Dr. Pereira died in December 2023. Her contributions to this article were enormous.
Appendices
Appendix 1
Table 2. Population, concept, and context (PCC) approach construction.
| Population | Concept | Context |
| MESH terms | MESH terms | MESH terms |
| Student*/medical | Disaster* | School*/medical |
| Undergraduate medical student* | Disaster medicine | Education/medical |
| Disaster planning | ||
| Keywords | Keywords | Keywords |
| Undergraduate | Disaster preparedness | Medical schools |
| Medical students | Curricul* | |
| Phrases | Phrases | Phrases |
| Disaster medicine education | ||
| Disaster health education | ||
| Disaster curricula |
Appendix 2
Table 3. Search strategy.
| PubMed/MEDLINE | Scopus | Web of Science Core Collection | Google Scholar |
| A first basic search with disaster medicine curriculum and medical students. Filters: Abstract, Full text, English, from 2004/1/1 - 2021/12/31. Second search (((disaster medicine OR “disaster planning” OR “disaster preparedness” OR (disaster medicine OR disaster* OR disaster planning [MeSH Terms])) AND “disaster medicine education” OR “disaster curricula”)) AND “(“medical students” OR undergraduate). Filters: Abstract, Free Full Text, from 2004/1/1 - 2021/12/31 | (TITLE-ABS-KEY {disaster*) OR TITLE-ABS-KEY ({disaster medicine} OR {disaster planning} OR {disaster preparedness}) OR TITLE-ABS-KEY ({disaster health education} OR {disaster medical education} OR {disaster curricul*}) AND TITLE-ABS-KEY ("undergraduate*" OR {undergraduate medical students} OR "medical student*") AND TITLE-ABS-KEY ("medical school" OR "medical university")) AND PUBYEAR > 2003 AND PUBYEAR <2022 AND (LIMIT-TO (SUBJAREA, "MEDI")) AND ( LIMIT-TO ( PUBSTAGE, "final")) AND (LIMIT-TO (LANGUAGE, "English)) | TS= disaster* OR “disaster medicine” OR “disaster planning” OR “disaster preparedness” AND TS = ”disaster health education” OR disaster medicine education” OR “curricul*” AND TS = ”medical student” OR “undergraduate” AND TS = ”medical school” OR “medical faculty”. From 2004-01-01 to 2021-12-31 English | Advanced search: Find articles: - with all the words: "disaster medical education" OR "disaster health education" OR "disaster preparedness" AND "medical students" AND " "medical schools" - with the exact phrase: "disaster health education" - with at least one of the words: education “disaster medicine” - not: Nurses. Anywhere in the text with citations 2004-2021, English language |
Disclosures
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Haroon Rashid
Acquisition, analysis, or interpretation of data: Haroon Rashid, Lykourgos Christos Alexakis, Irene Pereira
Drafting of the manuscript: Haroon Rashid
Critical review of the manuscript for important intellectual content: Haroon Rashid, Lykourgos Christos Alexakis, Irene Pereira
Supervision: Lykourgos Christos Alexakis, Irene Pereira
References
- 1.The International Federation of Red Cross and Red Crescent Societies (IFRC). What is a disaster? 2022. https://www.ifrc.org/our-work/disasters-climate-and-crises/what-disaster. https://www.ifrc.org/our-work/disasters-climate-and-crises/what-disaster [DOI] [PubMed]
- 2.Call for papers in the International Journal of Disaster Medicine. Lennquist S. https://resolver.scholarsportal.info/resolve/15031438/v02i0003/67_cfpitijodm.xml Int J Disaster Med. 2004;2:67–69. [Google Scholar]
- 3.Education and training in disaster medicine. Lennquist S. Scand J Surg. 2005;94:300–310. doi: 10.1177/145749690509400409. [DOI] [PubMed] [Google Scholar]
- 4.International standards and guidelines on education and training for the multi-disciplinary health response to major events that threaten the health status of a community. Seynaeve G, Archer F, Fisher J, et al. https://pubmed.ncbi.nlm.nih.gov/15506258/ Prehosp Disaster Med. 2004;19:0–30. [PubMed] [Google Scholar]
- 5.Education and research in disaster medicine and management: inextricably bound up with each other. Hubloue I, Debacker M. Eur J Emerg Med. 2010;17:129–130. doi: 10.1097/MEJ.0b013e32833981c7. [DOI] [PubMed] [Google Scholar]
- 6.United Nations Office for Disaster Risk Reduction. (2015. United Nations Office for Disaster Risk Reduction. Sendai framework for disaster risk reduction 2015-2030. 2015. https://www.undrr.org/publication/sendai-framework-disaster-risk-reduction-2015-2030 https://www.undrr.org/publication/sendai-framework-disaster-risk-reduction-2015-2030
- 7.Postgraduate education in disaster health and medicine. Algaali KY, Djalali A, Della Corte F, Ismail MA, Ingrassia PL. Front Public Health. 2015;3:185. doi: 10.3389/fpubh.2015.00185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Students' response to disaster: a lesson for health care professional schools. Reyes H. Ann Intern Med. 2010;153:658–660. doi: 10.7326/0003-4819-153-10-201011160-00009. [DOI] [PubMed] [Google Scholar]
- 9.Medical students and COVID-19: the need for pandemic preparedness. O'Byrne L, Gavin B, McNicholas F. J Med Ethics. 2020;46:623–626. doi: 10.1136/medethics-2020-106353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Terror medicine as part of the medical school curriculum. Cole LA, Wagner K, Scott S, et al. Front Public Health. 2014;2:138. doi: 10.3389/fpubh.2014.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Academic responses to Fukushima Disaster. Yasui K, Kimura Y, Kamiya K. https://www.jstor.org/stable/26686359. Asia Pac J Public Health. 2017;29:99–109. doi: 10.1177/1010539516685400. [DOI] [PubMed] [Google Scholar]
- 12.Development and implementation of a Disaster Medicine Certificate Series (DMCS) for medical students. Kommor MB, Hodge B, Ciottone G. Prehosp Disaster Med. 2019;34:197–202. doi: 10.1017/S1049023X19000165. [DOI] [PubMed] [Google Scholar]
- 13.Self-perception of medical students’ knowledge and interest in disaster medicine: nine years after the approval of the curriculum in German universities. Wunderlich R, Ragazzoni L, Ingrassia PL, Corte FD, Grundgeiger J, Bickelmayer JW, Domres B. Prehosp Disaster Med. 2017;32:374–381. doi: 10.1017/S1049023X17000280. [DOI] [PubMed] [Google Scholar]
- 14.Nationwide program of education for undergraduates in the field of disaster medicine: development of a core curriculum centered on blended learning and simulation tools. Ingrassia PL, Ragazzoni L, Tengattini M, Carenzo L, Della Corte F. Prehosp Disaster Med. 2014;29:508–515. doi: 10.1017/S1049023X14000831. [DOI] [PubMed] [Google Scholar]
- 15.Evaluation of a new community-based curriculum in disaster medicine for undergraduates. Bajow N, Djalali A, Ingrassia PL, Ragazzoni L, Ageely H, Bani I, Corte FD. BMC Med Educ. 2016;16:225. doi: 10.1186/s12909-016-0746-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Disaster health education and training: a pilot questionnaire to understand current status. Murray V, Clifford J, Seynaeve G, Fisher JM. Prehosp Disaster Med. 2006;21:156–167. doi: 10.1017/s1049023x00003629. [DOI] [PubMed] [Google Scholar]
- 17.Developing a health system approach to disaster management: a qualitative analysis of the core literature to complement the WHO Toolkit for assessing health-system capacity for crisis management. Bayntun C, Rockenschaub G, Murray V. https://pubmed.ncbi.nlm.nih.gov/23066520/ PLoS Curr. 2012;4:0. doi: 10.1371/5028b6037259a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Differences in opinions on disaster myths between first-year and sixth-year medical students. Altintas KH, Boztas G, Duyuler S, Duzlu M, Energin H, Ergun A. Eur J Emerg Med. 2009;16:80–83. doi: 10.1097/MEJ.0b013e32830a996c. [DOI] [PubMed] [Google Scholar]
- 19.The effectiveness of disaster training for health care workers: a systematic review. Williams J, Nocera M, Casteel C. Ann Emerg Med. 2008;52:211–222. doi: 10.1016/j.annemergmed.2007.09.030. [DOI] [PubMed] [Google Scholar]
- 20.Disaster medicine and pandemic response: a novel curriculum to improve understanding of complex care delivery during the COVID-19 pandemic. Peterson T, Wallace D, Evans J, et al. AEM Educ Train. 2021;5:0. doi: 10.1002/aet2.10647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Disaster training in 24 hours: evaluation of a novel medical student curriculum in disaster medicine. Wiesner L, Kappler S, Shuster A, DeLuca M, Ott J, Glasser E. J Emerg Med. 2018;54:348–353. doi: 10.1016/j.jemermed.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 22.What is the value of health emergency preparedness exercises? A scoping review study. Skryabina E, Reedy G, Amlôt R, Jaye P, Riley P. https://doi.org/10.1016/j.ijdrr.2016.12.010. Int J Disaster Risk Reduct. 2017;21:274–283. doi: 10.1016/j.ijdrr.2020.101503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The need of collaboration in medical education for worldwide disaster. Komasawa N, Terasaki F, Tomioka M, Saura R, Kawata R. Disaster Med Public Health Prep. 2021;15:539. doi: 10.1017/dmp.2020.126. [DOI] [PubMed] [Google Scholar]
- 24.Health workforce development in health emergency and disaster risk management: the need for evidence-based recommendations. Hung KK, Mashino S, Chan EY, et al. https://doi.org/10.3390/ijerph18073382. Int J Environ Res Public Health. 2021;18:3382. doi: 10.3390/ijerph18073382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.A consensus-based educational framework and competency set for the discipline of disaster medicine and public health preparedness. Subbarao I, Lyznicki JM, Hsu EB, et al. Disaster Med Public Health Prep. 2008;2:57–68. doi: 10.1097/DMP.0b013e31816564af. [DOI] [PubMed] [Google Scholar]
- 26.Disaster medicine education for physicians: a systematic review. Cummings G, Della Corte F, Cummings G. Int J Disaster Med. 2006;4:125–136. [Google Scholar]
- 27.Designing a curriculum in disaster medicine for Canadian medical schools. Cummings GE, Della Corte F. Int J Disaster Med. 2004;2:135–147. [Google Scholar]
- 28.Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. Munn Z, Peters MD, Stern C, Tufanaru C, McArthur A, Aromataris E. BMC Med Res Methodol. 2018;18:143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.A scoping review on the conduct and reporting of scoping reviews. Tricco AC, Lillie E, Zarin W, et al. https://doi.org/10.1186/s12874-016-0116-4. BMC Med Res Methodol. 2016;16:15. doi: 10.1186/s12874-016-0116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.The Joanna Briggs Institute. Methodology for JBI scoping reviews. The Joanna Briggs Institute. Adelaide, Australia: The Joanna Briggs Institute; 2015. The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI Scoping Reviews. [Google Scholar]
- 31.PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Tricco AC, Lillie E, Zarin W, et al. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 32.Open Science Framework (OSF. Open Science Framework. OSF Registries. 2024. https://osf.io/registries https://osf.io/registries
- 33.A short medical school course on responding to bioterrorism and other disasters. Parrish AR, Oliver S, Jenkins D, Ruscio B, Green JB, Colenda C. Acad Med. 2005;80:820–823. doi: 10.1097/00001888-200509000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Disaster medicine education in Canadian medical schools before and after September 11, 2001. Cummings GE, Della Corte F, Cummings GG. https://pubmed.ncbi.nlm.nih.gov/17355706/ CJEM. 2005;7:399–405. [PubMed] [Google Scholar]
- 35.Preparing health professions students for terrorism, disaster, and public health emergencies: core competencies. Markenson D, DiMaggio C, Redlener I. Acad Med. 2005;80:517–526. doi: 10.1097/00001888-200506000-00002. [DOI] [PubMed] [Google Scholar]
- 36.Perspectives of future physicians on disaster medicine and public health preparedness: challenges of building a capable and sustainable auxiliary medical workforce. Kaiser HE, Barnett DJ, Hsu EB, Kirsch TD, James JJ, Subbarao I. Disaster Med Public Health Prep. 2009;3:210–216. doi: 10.1097/DMP.0b013e3181aa242a. [DOI] [PubMed] [Google Scholar]
- 37.Improving medical students' understanding of prehospital care through a fourth year emergency medicine clerkship. Merlin MA, Moon J, Krimmel J, Liu J, Marques-Baptista A. Emerg Med J. 2010;27:147–150. doi: 10.1136/emj.2008.066654. [DOI] [PubMed] [Google Scholar]
- 38.A disaster medicine curriculum for medical students. Kaji AH, Coates W, Fung CC. Teach Learn Med. 2010;22:116–122. doi: 10.1080/10401331003656561. [DOI] [PubMed] [Google Scholar]
- 39.Medical student disaster medicine education: the development of an educational resource. Pfenninger EG, Domres BD, Stahl W, Bauer A, Houser CM, Himmelseher S. Int J Emerg Med. 2010;3:9–20. doi: 10.1007/s12245-009-0140-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.The effectiveness of training with an emergency department simulator on medical student performance in a simulated disaster. Franc-Law JM, Ingrassia PL, Ragazzoni L, Della Corte F. CJEM. 2010;12:27–32. doi: 10.1017/s1481803500011982. [DOI] [PubMed] [Google Scholar]
- 41.Medical student participation in a disaster seminar and drill: brief description of activity and report of student experiences. Kaji AH, Coates WC, Fung CC. Teach Learn Med. 2010;22:28–32. doi: 10.1080/10401330903446040. [DOI] [PubMed] [Google Scholar]
- 42.Disaster 101: a novel approach to disaster medicine training for health professionals. Scott LA, Carson DS, Greenwell IB. J Emerg Med. 2010;39:220–226. doi: 10.1016/j.jemermed.2009.08.064. [DOI] [PubMed] [Google Scholar]
- 43.The effectiveness of simulation based medical education in teaching concepts of major incident response. Saiboon IM, Jaafar MJ, Harunarashid H, Jamal SM. Procedia Soc Behav Sci. 2011;18:372–378. [Google Scholar]
- 44.Planning and incorporating public health preparedness into the medical curriculum. Carney JK, Schilling LM, Frank SH, Biddinger PD, Bertsch TF, Grace CJ, Finkelstein JA. Am J Prev Med. 2011;41:0–9. doi: 10.1016/j.amepre.2011.05.026. [DOI] [PubMed] [Google Scholar]
- 45.Simulation and its role in medical education. Datta R, Upadhyay K, Jaideep C. Med J Armed Forces India. 2012;68:167–172. doi: 10.1016/S0377-1237(12)60040-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Disaster curricula in medical education: pilot survey. Smith J, Levy MJ, Hsu EB, Lee Levy J. Prehosp Disaster Med. 2012;27:492–494. doi: 10.1017/S1049023X12001215. [DOI] [PubMed] [Google Scholar]
- 47.High-fidelity multiactor emergency preparedness training for patient care providers. Scott LA, Maddux PT, Schnellmann J, Hayes L, Tolley J, Wahlquist AE. Am J Disaster Med. 2012;7:175–188. doi: 10.5055/ajdm.2012.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Disaster medicine and public health preparedness of health professions students: a multidisciplinary assessment of knowledge, confidence, and attitudes. Markenson D, Woolf S, Redlener I, Reilly M. Disaster Med Public Health Prep. 2013;7:499–506. doi: 10.1017/dmp.2013.96. [DOI] [PubMed] [Google Scholar]
- 49.Knowledge levels and training needs of disaster medicine among health professionals, medical students, and local residents in Shanghai, China. Su T, Han X, Chen F, et al. PLoS One. 2013;8:0. doi: 10.1371/journal.pone.0067041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Italian medical students and disaster medicine: awareness and formative needs. Ragazzoni L, Ingrassia PL, Gugliotta G, Tengattini M, Franc JM, Corte FD. Am J Disaster Med. 2013;8:127–136. doi: 10.5055/ajdm.2013.0119. [DOI] [PubMed] [Google Scholar]
- 51.Disaster preparedness: what training do our interns receive during medical school? Jasper E, Berg K, Reid M, et al. Am J Med Qual. 2013;28:407–413. doi: 10.1177/1062860612471843. [DOI] [PubMed] [Google Scholar]
- 52.A peer-education based disaster medicine course to turn medical students into a useful resource. Grossi F, Mangini M, Giuli M, et al. https://doi.org/10.1016/j.ijdrr.2014.02.003 Int J Disaster Risk Reduct. 2014;8:153–157. [Google Scholar]
- 53.Full-scale simulation may be used to train medical students in disaster medicine. Afzali M, Viggers S. Trends Anaesth Crit Care. 2015;5:17–22. [Google Scholar]
- 54.Global health education in the United Kingdom: a review of university undergraduate and postgraduate programmes and courses. Harmer A, Lee K, Petty N. Public Health. 2015;129:797–809. doi: 10.1016/j.puhe.2014.12.015. [DOI] [PubMed] [Google Scholar]
- 55.Development of a disaster preparedness curriculum for medical students: a pilot study of incorporating local events into training opportunities. Pollard KA, Bachmann DJ, Greer M, Way DP, Kman NE. Am J Disaster Med. 2015;10:51–59. doi: 10.5055/ajdm.2015.0188. [DOI] [PubMed] [Google Scholar]
- 56.Dutch senior medical students and disaster medicine: a national survey. Mortelmans LJ, Bouman SJ, Gaakeer MI, Dieltiens G, Anseeuw K, Sabbe MB. Int J Emerg Med. 2015;8:34. doi: 10.1186/s12245-015-0077-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Proposal for a community-based disaster management curriculum for medical school undergraduates in Saudi Arabia. Bajow N, Djalali A, Ingrassia PL, Ageely H, Bani I, Della Corte F. Am J Disaster Med. 2015;10:145–152. doi: 10.5055/ajdm.2015.0197. [DOI] [PubMed] [Google Scholar]
- 58.Disaster medicine curricula in Saudi Arabian medical schools. Bajow N, Djalali A, Ingrassia PL, Ageely H, Bani I, Della Corte F. J Emerg Med Trauma Acute Care. 2015;2015:8. doi: 10.5055/ajdm.2015.0197. [DOI] [PubMed] [Google Scholar]
- 59.'Disaster day': global health simulation teaching. Mohamed-Ahmed R, Daniels A, Goodall J, O'Kelly E, Fisher J. Clin Teach. 2016;13:18–22. doi: 10.1111/tct.12349. [DOI] [PubMed] [Google Scholar]
- 60.Disaster medicine education for medical students: is it a real need? Barrimah I, Adam I, Al-Mohaimeed A. Med Teach. 2016;38:0–5. doi: 10.3109/0142159X.2016.1142515. [DOI] [PubMed] [Google Scholar]
- 61.Are Belgian military students in medical sciences better educated in disaster medicine than their civilian colleagues? Mortelmans LJ, Lievers J, Dieltiens G, Sabbe MB. J R Army Med Corps. 2016;162:383–386. doi: 10.1136/jramc-2015-000563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.A course on terror medicine: content and evaluations. Cole LA, Natal B, Fox A, et al. Prehosp Disaster Med. 2016;31:98–101. doi: 10.1017/S1049023X15005579. [DOI] [PubMed] [Google Scholar]
- 63.Implementing a disaster preparedness curriculum for medical students. Jasper EH, Wanner GK, Berg D, Berg K. South Med J. 2017;110:523–527. doi: 10.14423/SMJ.0000000000000681. [DOI] [PubMed] [Google Scholar]
- 64.A lesson learnt: implementation of interprofessional education in disaster management at Faculty of Medicine Universitas Gadjah Mada, Indonesia. Prihatiningsih TS, Widyandana Widyandana, Hapsari ED, Helmiyati S, Ananda AJ. J Interprof Educ Pract. 2017;9:121–125. [Google Scholar]
- 65.Healthcare students interprofessional critical event/disaster response course. Kim TE, Shankel T, Reibling ET, et al. Am J Disaster Med. 2017;12:11–26. doi: 10.5055/ajdm.2017.0254. [DOI] [PubMed] [Google Scholar]
- 66.Health care student knowledge and willingness to work in infectious disease outbreaks. Patel R, Wattamwar K, Kanduri J, et al. Disaster Med Public Health Prep. 2017;11:694–700. doi: 10.1017/dmp.2017.18. [DOI] [PubMed] [Google Scholar]
- 67.Design and implementation of a medical student hazardous materials response team: the Medical Student HazMat Team. Verson J, Dyga N, Agbayani N, Serafin F, Hondros L. Int J Emerg Med. 2018;11:38. doi: 10.1186/s12245-018-0195-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Crisis on the game board - a novel approach to teach medical students about disaster medicine. Drees S, Geffert K, Brynen R. GMS J Med Educ. 2018;35:0. doi: 10.3205/zma001192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Disaster preparedness medical school elective: bridging the gap between volunteer eagerness and readiness. Patel VM, Dahl-Grove D. Pediatr Emerg Care. 2018;34:492–496. doi: 10.1097/PEC.0000000000000806. [DOI] [PubMed] [Google Scholar]
- 70.Preparing for the surge: a half-day emergency preparedness training course for the “second front”. Scott LA, Madden LA, Wahlquist AE, Fisher DW. Disaster Med Public Health Prep. 2018;12:121–126. doi: 10.1017/dmp.2017.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Deployment and disaster medicine in an undergraduate teaching module. Back DA, Lembke V, Fellmer F, Kaiser D, Kasselmann N, Bickelmayer J, Willy C. Mil Med. 2019;184:0–9. doi: 10.1093/milmed/usy250. [DOI] [PubMed] [Google Scholar]
- 72.Needs assessment for standardized educational program for Iranian medical students in crisis and disaster management. Rezaee R, Peyravi M, Ahmadi Marzaleh M, Khorram-Manesh A. J Adv Med Educ Prof. 2019;7:95–102. doi: 10.30476/JAMP.2019.44713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Attitudes of medical students toward volunteering in emergency situations. Gouda P, Kirk A, Sweeney AM, O'Donovan D. Disaster Med Public Health Prep. 2020;14:308–311. doi: 10.1017/dmp.2019.81. [DOI] [PubMed] [Google Scholar]
- 74.A nationwide peer-assisted learning program in disaster medicine for medical students. Ragazzoni L, Conti A, Dell'Aringa M, Caviglia M, Maccapani F, Della Corte F. Eur J Emerg Med. 2020;27:290–297. doi: 10.1097/MEJ.0000000000000668. [DOI] [PubMed] [Google Scholar]
- 75.Pilot study of a longitudinal integrated disaster and military medicine education program for undergraduate medical students. Tsai YD, Tsai SH, Chen SJ, et al. Medicine (Baltimore) 2020;99:0. doi: 10.1097/MD.0000000000020230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Evaluation of disaster medicine preparedness among healthcare profession students: a cross-sectional study in Pakistan. Gillani AH, Mohamed Ibrahim MI, Akbar J, Fang Y. Int J Environ Res Public Health. 2020;17:2027. doi: 10.3390/ijerph17062027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.A sneak peek into the curriculum on disaster management medicine in India for health professionals: a mixed-methods approach. Panda M, Pathak R, Agarwalla R, Rasheed N. J Educ Health Promot. 2020;9:13. doi: 10.4103/jehp.jehp_360_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Insights into disaster management scenario among various health-care students in India: a multi-institutional, multi-professional study. Rajesh G, Binnal A, H Pai MB, Nayak SV, Shenoy R, Rao A. Indian J Community Med. 2020;45:220–224. doi: 10.4103/ijcm.IJCM_104_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Medical students as disaster volunteers: a strategy for improving emergency department surge response in times of crisis. Ponampalam R, Pong JZ, Wong XY. World J Crit Care Med. 2021;10:163–169. doi: 10.5492/wjccm.v10.i5.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Preparing medical students for a pandemic: a systematic review of student disaster training programmes. Ashcroft J, Byrne MH, Brennan PA, Davies RJ. Postgrad Med J. 2021;97:368–379. doi: 10.1136/postgradmedj-2020-137906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Assessment of knowledge, attitudes, and readiness to practice regarding disaster medicine and preparedness among university health students. Al-Ziftawi NH, Elamin FM, Mohamed Ibrahim MI. Disaster Med Public Health Prep. 2021;15:316–324. doi: 10.1017/dmp.2019.157. [DOI] [PubMed] [Google Scholar]
- 82.Presentation and evaluation of a modern course in disaster medicine and humanitarian assistance for medical students. Hermann S, Gerstner J, Weiss F, et al. BMC Med Educ. 2021;21:610. doi: 10.1186/s12909-021-03043-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.A scoping review on adaptations of clinical education for medical students during COVID-19. Park H, Shim S, Lee YM. Prim Care Diabetes. 2021;15:958–976. doi: 10.1016/j.pcd.2021.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Implementation of disaster medicine education in German medical schools - a nationwide survey. Kasselmann N, Willy C, Domres BD, Wunderlich R, Back DA. GMS J Med Educ. 2021;38:0. doi: 10.3205/zma001475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.E-learning in teaching emergency disaster response among undergraduate medical students in Malaysia. Saiboon IM, Zahari F, Isa HM, Sabardin DM, Robertson CE. Front Public Health. 2021;9:628178. doi: 10.3389/fpubh.2021.628178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Disaster day: a simulation-based disaster medicine curriculum for novice learners. Gable BD, Misra A, Doos DM, Hughes PG, Clayton LM, Ahmed RA. J Med Educ Curric Dev. 2021;8 doi: 10.1177/23821205211020751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Koenig KL, Schultz CH. Edition 2. Cambridge, UK: Cambridge University Press; 2016. Koenig and Schultz's Disaster Medicine: Comprehensive Principles and Practices; p. 782. [Google Scholar]