Abstract
Introduction
Compare the anatomical and functional outcomes, operation duration, and complication rates between standard scleral buckling (SSB) and chandelier-assisted scleral buckling (CSB) for phakic eyes with rhegmatogenous retinal detachment (RRD).
Methods
PubMed, Embase, and Cochrane Library databases were searched from inception to June 2024. The primary endpoint will be set as a final success. The secondary endpoint will be primary success, operation time, and final BCVA.
Results
Our meta-analysis showed that there is no statistical difference between CSB and SSB for the final success rate (RR = 1.00, 95% CI = 0.97–1.03). For the primary success rate, there is no statistical difference between CSB and SSB (RR = 1.00, 95% CI = 0.94–1.06). For operation time, our meta-analysis showed that the CSB group is less than the SSB group (pooled MD = −15.8, 95% CI = −22.60 to −9.00). For postoperative complications, our study shows that the CSB group presented with lower pooled risk than the SSB group (RR = 0.59, 95% CI = 0.41–0.89). There is a trend that the ERM formation risk is higher in the CSB group if there is no routine suture for the sclerotomy (p = 0.08).
Conclusion
CSB showcases a significantly reduced operation duration and less postoperative complication in contrast to the SSB group, maintaining comparable primary and ultimate anatomical success rates as well as final BCVA.
Keywords: Rhegmatogenous retinal detachment, Chandelier-assisted scleral buckling surgery, Standard scleral buckling, Epiretinal membranes
Introduction
Rhegmatogenous retinal detachment (RRD) is a sight-threatening condition. Recognized as a medical emergency, RRD demands timely intervention to optimize the prognosis [1]. Several treatment options are available, including vigilant observation, laser demarcation, pneumatic retinopexy, scleral buckling (SB), and pars plana vitrectomy (PPV), all demonstrating varying degrees of efficacy [2].
For a significant period, SB stood as the primary surgical approach, boasting an anatomical success rate of over 90% in achieving reattachment [2–4]. However, advancements in microincisional instruments and the introduction of wide-angle microscopic viewing systems have broadened the role of vitrectomy. A survey in Taiwan found that by 2002, PPV had become more common than SB for primary RRD cases [5]. This trend is global; US Medicare data show a 70% decline in scleral buckles without vitrectomy for RRD repair [6].
Despite a significant global decline in SB procedures for RRD, it continues to hold its place as an essential treatment option, offering distinct advantages such as cost-effectiveness, preservation of the vitreous, improved final visual acuity in phakic eyes, and less cataract progression. Nevertheless, the challenges associated with SB surgery, including extended operation duration, a longer learning curve, and a higher incidence of neck and back discomfort for the surgeon, have led some to label SB as a somewhat neglected or less preferred technique, particularly among younger surgeons.
In an effort to reverse the declining preference for SB surgery, chandelier-assisted scleral buckling (CSB) surgery was introduced in 2012 by Aras et al. [7]. This innovative approach involves the insertion of a transscleral light source, facilitating wide-field visualization through the operating microscope, similar to the field achieved during PPV. CSB is believed to offer several advantages over standard SB (SSB) which was defined as using an indirect ophthalmoscopy to localize the retinal breaks, including improved surgical visibility, reduced risk of musculoskeletal injuries for surgeons, shorter operation duration, and simplified cryopexy procedures [8–14]. However, a recent randomized controlled trial (RCT) has presented conflicting evidence, reporting a higher incidence of complications with CSB, particularly in the development of epiretinal membranes (ERMs) [15].
To explore this issue further, we conducted a systematic review and meta-analysis aimed at assessing the treatment outcomes of SSB and CSB for the management of RRD. This study aimed to expand our current knowledge regarding the safety and effectiveness of CSB versus SSB.
Methods
The Protocol Registration
We conducted this study according to the PRISMA guideline [16]. We registered this study in PROSPERO(CRD42023433092).
Study Search
Databases including PubMed, Embase, and Cochrane Library were searched from inception to June 2024. The search keyword was set as SCLERAL BUCKLING and Wide-angled endoillumination or CHANDELIER-ASSISTED or traditional scleral buckling or conventional scleral buckling. The inclusion and exclusion criteria are listed below.
Inclusion:
-
1.
The study compared CSB and SSB in patients with RRD
-
2.
Adult population
-
3.
Human study
-
4.
RCT or cohort study or case-control study
Exclusion:
-
1.
Patient with previous vitrectomy
-
2.
Patient with posterior or giant breaks
-
3.
Patient with macular holes
-
4.
Patient with media opacity
-
5.
Patient with any other ocular pathologies
-
6.
Case report or case series
Data Extraction
Two authors extracted data including publication year, the surname of the first author, patient number, characteristics of the patient groups, main outcomes, additional outcomes, and publication country. Conflicts will be solved by consensus.
The primary endpoint will be set as a final success. The secondary endpoint will be set as primary success, operation time, and final BCVA.
Statistical Analysis
Random effect models will be used in this study. We aim to calculate the pooled mean difference, pooled odds ratio, p value, and 95% confidence interval using the inverse variance method. The heterogeneity of studies will be evaluated by the Cochrane’s Q test and I2 score. A p value <0.05 is set as statistical significance. Subgroup analysis was performed based on the following criteria: patients receiving suture sclerotomy or not.
Quality Assessment
For retrospective studies, the quality was assessed by the NOS scale. For randomized control trials, the quality was assessed by the ROB-2 scale. The publication bias was evaluated by the funnel plot. If the included studies are more than ten, then Egger’s test was performed.
Results
The Characteristics of Literature
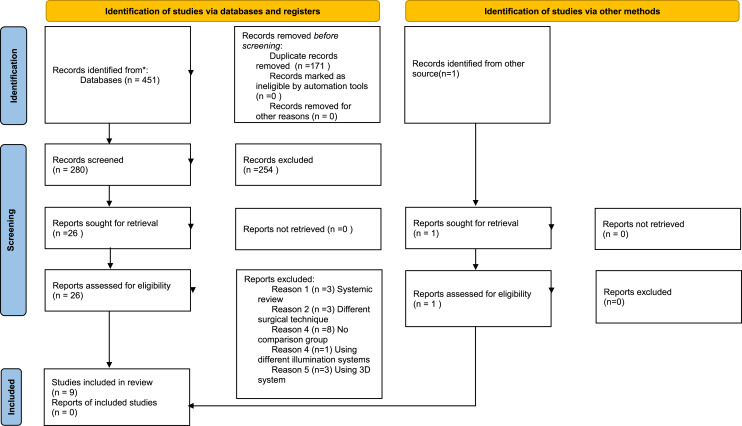
A total of 451 articles were initially included. After article selection, nine articles were included in the final analysis. All the included studies are using a 25-gauge system. The PRISMA flowchart is shown in Figure 1. The characteristics of the included studies are provided in Table 1. The exclusion list was provided in online supplementary material 1 (for all online suppl. material, see https://doi.org/10.1159/000540820).
Fig. 1.
PRISMA 2020 flow diagram.
Table 1.
Characteristics of the included studies
| Author, year | Nation | Accrual year | Group (n analyzed) | Macula off, n (%) | RD quadrant >2, n (%) | Refractive error, D, M±SD | Multiple breaks, n (%) | Routine suture (for sclerotomy) | |
|---|---|---|---|---|---|---|---|---|---|
| Patients’ baseline characteristics | |||||||||
| Albalkini et al. [15] (2022) | Egypt | 2018–2020 | CSB (23) | 19 (83) | 13 (51) | −6.26±6.57 | 13 (57) | No | |
| SSB (27) | 20 (74) | 15 (55) | −5.74±6.21 | 17 (63) | |||||
| Cohen et al. [8] (2019) | Israel | 2011–2015 | CSB (22) | 6 (27.3) | NR | −5.32±2.69 | 12 (54.5) | No | |
| SSB (27) | 11 (40.7) | NR | −5.75±3.26 | 8 (29.6) | |||||
| Li et al. [10] (2016) | China | 2010–2013 | CSB (47) | 10 (21.3) | NR | −4.72±1.85 | NR | No | |
| SSB (47) | 9 (19.2) | NR | −4.46±2.21 | NR | |||||
| Narayanan et al. [16] (2016) | India | 2013–2014 | CSB (14) | x | NR | NR | 6 (42.9) | No | |
| SSB (14) | x | NR | NR | 5 (35.7) | |||||
| Tomita et al. [9] (2015) | Japan | 2012–2014 | CSB (16) | 2 (12.5) | 8 (50) | −5.81±3.24 | NR | No | |
| SSB (23) | 4 (17.4) | 15 (65.2) | −3.61±3.14 | NR | |||||
| Ali et al. [17] (2022) | Peshawar | 2020 | CSB (20) | 14 (70) | NR | NR | 11 (55) | Yes | |
| SSB (20) | 13 (65) | NR | NR | 9 (45) | |||||
| Ilhan et al. [18] (2022) | Turkey | NR | CSB (20) | 8 (40) | 5 (25) | NR | 8 (40) | Yes | |
| SSB (25) | 5 (20) | 6 (24) | NR | 6 (24) | |||||
| Talcott et al. [19] 2017 | USA | NR | CSB (17) | 13 (76) | NR | NR | NR | NR | |
| SSB (17) | 8 (47) | NR | NR | NR | |||||
| Fujikawa et al. [20] (2016) | Japan | 2008–2015 | CSB (38) | NR | NR | NR | NR | NR | |
| SSB (34) | NR | NR | NR | NR | |||||
| Author, year | Nation | Accrual year | Group (n analyzed) | OP time, min, M±SD | Primary success, n (%) | Final BCVA, logMAR, M±SD | Final success, n (%) | ERM, n (%) | Intra-op comp., n | Post-op comp., n |
|---|---|---|---|---|---|---|---|---|---|---|
| Intra-op and post-op data | ||||||||||
| Albalkini et al. [15] (2022) | Egypt | 2018–2020 | CSB (23) | 102.48±43.76 | 18 (78.3) | 0.67±0.45 | 21 (91.3) | 8 (44) | 14 | 8 |
| SSB (27) | 120.3±39.05 | 21 (80.8) | 0.50±0.36 | 26 (100) | 4 (19) | 3 | 1 | |||
| Cohen et al. [8] (2019) | Israel | 2011–2015 | CSB (22) | NR | 18 (81.8) | 0.245±0.30 | 22 (100) | NR | 1 | 2 |
| SSB (27) | NR | 23 (85.2) | 0.368±0.34 | 27 (100) | NR | 0 | 2 | |||
| Li et al. [10] (2016) | China | 2010–2013 | CSB (47) | 62.53±8.43 | 44 (94.3) | 0.12±0.08 | 47 (100) | 0 (0) | NR | 12 |
| SSB (47) | 83.15±9.34 | 43 (92.4) | 0.13±0.08 | 47 (100) | 1 (2.13) | NR | 22 | |||
| Narayanan et al. [16] (2016) | India | 2013–2014 | CSB (14) | 77.85±16.37 | 13 (92.9) | 0.6 | 14 (100) | NR | 0 | 1 |
| SSB (14) | 95.71±26.59 | 12 (85.7) | 0.9 | 14 (100) | NR | 0 | 1 | |||
| Tomita et al. [9] (2015) | Japan | 2012–2014 | CSB (16) | 107±41 | 15 (93.8) | −0.04±0.08 | 16 (100) | 1 (6.3) | 0 | 2 |
| SSB (23) | 130±46 | 22 (95.7) | −0.01±0.11 | 23 (100) | 0 (0) | 6 | 10 | |||
| Ali et al. [17] (2022) | Peshawar | 2020 | CSB (20) | NR | 19 (95) | 0.34±0.23 | 20 (100) | NR | 0 | 1 |
| SSB (20) | NR | 19 (95) | 0.29±0.16 | 20 (100) | NR | 0 | 0 | |||
| Ilhan et al. [18] (2022) | Turkey | NR | CSB (20) | NR | 17 (85.00) | 0.48±0.30 | NR | 2 (10) | 0 | 9 |
| SSB (25) | NR | 20 (80.00) | 0.41±0.37 | NR | 6 (24) | 0 | 22 | |||
| Talcott et al. [19] (2017) | USA | NR | CSB (17) | 69±10 | 14 (82.4) | 0.65±0.70 | NR | NR | NR | NR |
| SSB (17) | 75±15 | 15 (88.2) | 0.43±0.54 | NR | NR | NR | NR | |||
| Fujikawa et al. [20] (2016) | Japan | 2008–2015 | CSB (38) | 92.1±26.8 | 34 (89.5) | NR | NR | NR | NR | NR |
| SSB (34) | 107.1±34.6 | 31 (91.2) | NR | NR | NR | NR | NR | |||
CSB, chandelier-assisted scleral buckling; SSB, standard scleral buckling; n, number; RD, retinal detachment; D, diopters; NR, not reported; OP, operation; logMAR, logarithm of the minimum angle of resolution; M±SD, mean±standard deviation; min, minutes; ERM, epiretinal membrane; intra-op comp., intra-operative complications; post-op comp., post-operative complications; the number of complications was calculated by summing all mentions in the articles.
Statistical Analysis
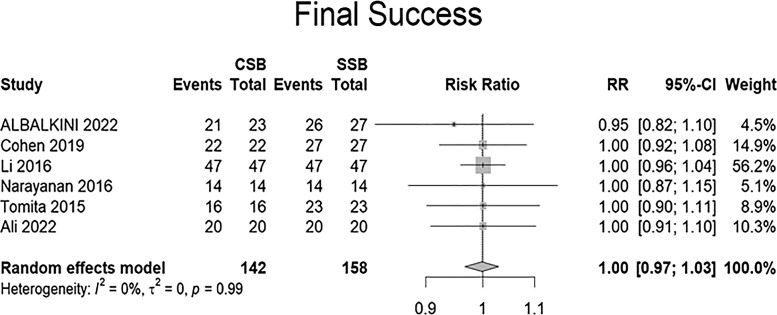
Our meta-analysis showed that there is no statistical difference between CSB and SSB for final success rate (RR = 1.00, 95% CI = 0.97–1.03). The I2 score is 0, which means that there is low heterogeneity among studies for the endpoint of final success. The forest is shown in Figure 2.
Fig. 2.
Forest plot for final success rate.
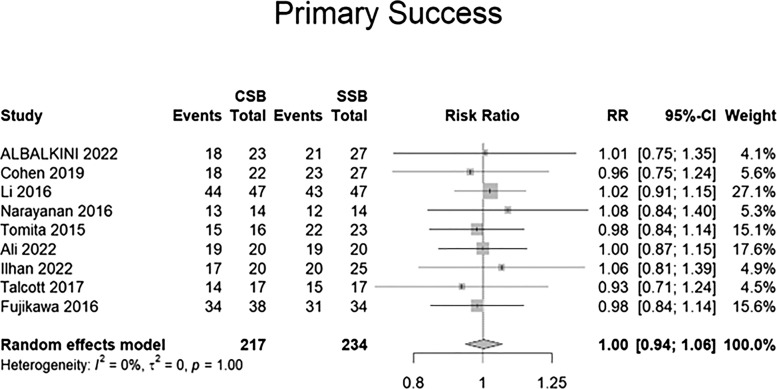
For the primary success rate, there is no statistical difference between CSB and SSB (RR = 1.00, 95% CI = 0.94–1.06). The I2 score is 0, which means that there is low heterogeneity among studies for the endpoint of primary success. The forest is shown in Figure 3.
Fig. 3.
Forest plot for primary success rate.
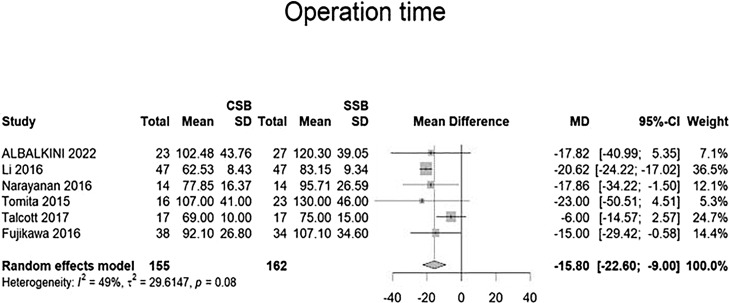
For operation time, our meta-analysis showed that the CSB group is less than the SSB group (pooled MD = −15.8, 95% CI = −22.60 to −9.00). The I2 score is 49%, which means that there is low heterogeneity among studies for the endpoint of primary success. The forest is shown in Figure 4.
Fig. 4.
Forest plot for operation time.
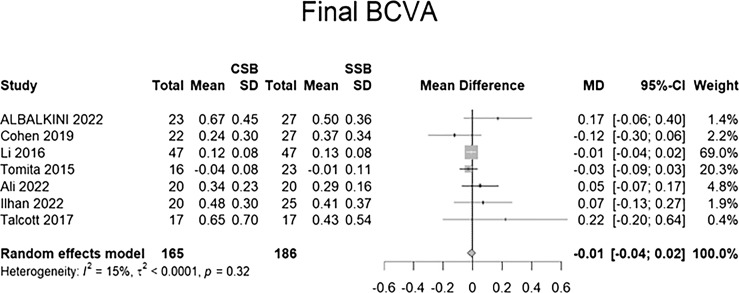
For final BCVA, there is no statistical difference between CSB and SSB (MD = −0.01, 95% CI = −0.04–0.02). The I2 score is 15%, which means that there is low heterogeneity among studies for the endpoint of primary success. The forest is shown in Figure 5.
Fig. 5.
Forest plot for BCVA.
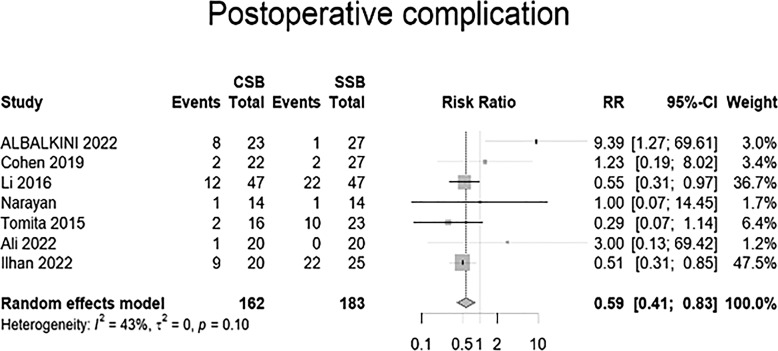
For postoperative complications, there is a statistical difference between CSB and SSB (RR = 0.59, 95% CI = 0.41–0.89). The I2 score is 43%, which means that there is low heterogeneity among studies for the endpoint of postoperative complications. The forest is shown in Figure 6.
Fig. 6.
Forest plot for postoperative complication.
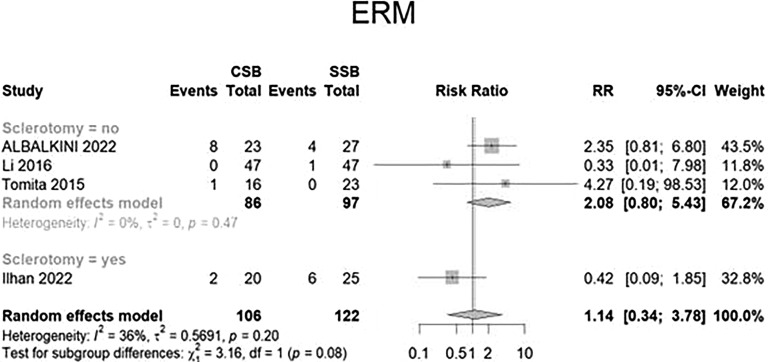
Subgroup Analysis
We further conduct subgroup analysis according to whether the patient receives suture sclerotomy routinely or not for the endpoint of ERM. Although there is no statistical significance, we can find that there is a trend that ERM formation risk is higher in the CSB group if no routine suture for the sclerotomy (p = 0.08). The forest is shown in Figure 7.
Fig. 7.
Analysis of ERM regarding the status of sclerotomy.
Quality Assessment
The quality of included literature is high; for non-RCT studies, 7 out of 9 articles scored more than 6. For the only RCT, four domains are low risk; only “bias due to deviations from intended interventions” has some concerns/low risk. The reason is that operators already know the type of surgery before operation. ROB-2 is shown in online supplementary material 2, and the NOS scale is presented in online supplementary material 3.
Publication Bias Assessment
Publication bias was evaluated for final success, primary success, operation time, and final BCVA. Because we included less than ten articles, Egger’s test was not performed. The funnel plot for final success, primary success, operation time, final BCVA, and postoperative complication is shown in online supplementary material 4–8, respectively.
Discussion
To the best of our knowledge, this marks the first meta-analysis conducted to assess the effectiveness and safety of CSB in comparison with SSB for primary RRD surgery. The pooled results indicate that the operation time for CSB is significantly shorter than that of the SSB group, with low heterogeneity observed among the studies. Also, a lower rate of postoperative complications was also shown in the CSB group. The subgroup analysis revealed trends, albeit statistically nonsignificant, indicating a higher risk of ERM formation in CSB groups when sclerotomy sites were not routinely sutured. However, parameters such as primary and final anatomical success, as well as final BCVA, did not exhibit significant differences between these two groups.
Several studies have emphasized a significant decrease in surgical time with CSB, attributed to the broad, unobscured, and well-illuminated surgical field facilitated by the wide-angle viewing system [8, 9, 17, 18, 21, 22]. Nonetheless, there is conflicting evidence regarding the surgical durations between the two groups [15]. A possible explanation for this inconsistency is that a substantial number of vitreoretinal surgeons, particularly younger practitioners, are more familiar with wide-field viewing systems than with indirect ophthalmoscopes. This disparity in familiarity may lead to challenges in accurately locating peripheral retinal breaks and effectively performing cryopexy when employing the indirect ophthalmoscope. It can be argued that when proficiency in peripheral retinal examination is achieved, the duration required for the SSB procedure becomes comparable to that of utilizing a wide-field viewing system.
Regarding the identification of new breaks during the operation, only three studies provided relevant data. Cohen et al. [8] documented a noteworthy 71.9% discrepancy in the intraoperative discovery rate of retinal breaks, favoring CSB (18.5% in the SSB group compared to 31.8% in the CSB group). Meanwhile, Albalkini et al. [15] and Ali et al. [17] reported comparable findings between the two groups. Due to the limited number of studies available on this topic, we refrained from conducting a subgroup analysis.
Regarding the prevalence of postoperative complications, the variability in definitions across studies diminishes the robustness of the assessment. However, among the seven studies that reported cumulative complications, only Albalkini et al. [15] observed higher postoperative complication rates in the CSB groups (34.8% vs. 3.8%, p < 0.05). Other studies reported either lower or similar complication rates. And no studies have reported the presence of endophthalmitis. However, it is crucial to be vigilant about publication bias in retrospective cohort studies. There is a tendency for studies showcasing positive, statistically significant, or favorable results aligned with the study hypotheses to be published, particularly in the context of new surgical techniques. Additionally, since not all retrospective studies reported the same surgeon being responsible for both procedures, there might be a higher likelihood of more experienced surgeons performing the new surgical method than the original procedure. Therefore, further RCTs are necessary to address this concern and supplement the results of this meta-analysis.
There are several concerns associated with CSB, particularly the shift from an extraocular to an intraocular procedure. Issues were raised regarding the long-term safety of the procedure in terms of cataract formation, endophthalmitis, proliferative vitreoretinopathy, trocar insertion site-related retinal detachment, as well as ERM or macular hole incidence. Literature reports various illumination systems for CSB, including non-valved cannula-based, valved cannula-based, or non-cannula-based chandelier light probes. Regardless of the system used, all studies stated suturing of sclerotomies either as a routine or when vitreous prolapse occurred after cannula removal. Additionally, minimal vitrectomy with a cutter probe was conducted externally at the sclerotomy site if any vitreous prolapse was observed at the end of the procedure. Vitreous incarceration within sclerotomy sites can lead to numerous complications, most notably ERM formation [23, 24]. Loss of formed vitreous and its entrapment can increase vitreous traction, contributing to the postoperative development of ERM [25]. Our subgroup analysis indicates a trend, though not statistically significant, suggesting a higher risk of ERM formation in groups where sclerotomy was not routinely sutured, showing a relative risk of 2.08 with a 95% CI of 0.80 to 5.43 (subgroup difference p = 0.08). However, due to the lack of precise information regarding which patients underwent sclerotomy suturing, further analysis cannot be conducted.
Currently, there is no consensus on whether routinely suturing the sclerotomy site. Some surgeons address prolapsed vitreous solely through vitrectomy at the sclerotomy site without suturing [26–29], while others choose to suture the sclerotomy site regardless of the presence of vitreous leakage [30, 31]. According to our findings, we recommend routinely suturing all sclerotomies in CSB, even in the absence of apparent vitreous prolapse. Albalkini et al. [15] reached a similar conclusion, demonstrating in a small subgroup analysis that eight out of 15 eyes developed ERM when the sclerotomy was left unsutured, whereas none of the four eyes with sutured sclerotomies developed ERM. The difference between the two groups was statistically significant (p = 0.023).
The limitation of this study is that the number of included studies is less than 10. As a result, we did not perform Egger’s test. We intend to update our findings as additional studies become accessible. Furthermore, different studies have varied designs, and the majority of those reviewed were retrospective, with only one being prospective. Additionally, the follow-up periods were not long enough to provide long-term conclusions. A primary bias observed in surgical interventions is performance bias, where extra attention and caution are often applied when executing a new surgical procedure. Additionally, publication bias tends to favor the reporting of false-positive results, leading to an overrepresentation of positive outcomes. However, despite these biases, the current meta-analysis demonstrated low heterogeneity among the variables, thereby significantly reducing potential biases.
In conclusion, CSB demonstrates a notably shorter operation time compared to the SSB group while exhibiting similar primary and final anatomical success rates alongside final BCVA. Furthermore, the subgroup analysis, despite lacking statistical significance, suggests a potential increased risk of ERM formation in CSB groups when sclerotomy sites are not routinely sutured. CSB presents a promising solution to revitalize the fading popularity of the SB technique and provides enhanced ergonomics for retinal surgeons.
Statement of Ethics
An ethics statement is not applicable because this study is based exclusively on published literature.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This study was not supported by any sponsor or funder.
Author Contributions
Yung-Shuo Kao, Chia-Yun Chen, Yu-Te Huang, and San-Ni Chen have satisfied the four criteria of authorship detailed by International Committee of Medical Journal Editors (ICMJE) recommendations. All authors contributed substantially to one or more of the following aspects of the manuscript: conception of the study, data acquisition, statistical analysis, drafting, revision for intellectual content, and final approval.
Funding Statement
This study was not supported by any sponsor or funder.
Data Availability Statement
All generated data are included in this paper. Further inquiries are to be directed to the corresponding author.
Supplementary Material.
Supplementary Material.
Supplementary Material.
Supplementary Material.
Supplementary Material.
Supplementary Material.
Supplementary Material.
Supplementary Material.
References
- 1. Chen SN, Lian IB, Wei YJ. Epidemiology and clinical characteristics of rhegmatogenous retinal detachment in Taiwan. Br J Ophthalmol. 2016;100(9):1216–20. [DOI] [PubMed] [Google Scholar]
- 2. Kunikata H, Abe T, Nakazawa T. Historical, current and future approaches to surgery for rhegmatogenous retinal detachment. Tohoku J Exp Med. 2019;248(3):159–68. [DOI] [PubMed] [Google Scholar]
- 3. Sultan ZN, Agorogiannis EI, Iannetta D, Steel D, Sandinha T. Rhegmatogenous retinal detachment: a review of current practice in diagnosis and management. BMJ Open Ophthalmol. 2020;5(1):e000474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen SN, Jiunn-Feng H, Te-Cheng Y. Pediatric rhegmatogenous retinal detachment in taiwan. Retina. 2006;26(4):410–4. [DOI] [PubMed] [Google Scholar]
- 5. Ho JD, Liou SW, Tsai CY, Tsai RJ, Lin HC. Trends and outcomes of treatment for primary rhegmatogenous retinal detachment: a 9-year nationwide population-based study. Eye. 2009;23(3):669–75. [DOI] [PubMed] [Google Scholar]
- 6. Ramulu PY, Do DV, Corcoran KJ, Corcoran SL, Robin AL. Use of retinal procedures in medicare beneficiaries from 1997 to 2007. Arch Ophthalmol. 2010;128(10):1335–40. [DOI] [PubMed] [Google Scholar]
- 7. Aras C, Ucar D, Koytak A, Yetik H. Scleral buckling with a non-contact wide-angle viewing system. Ophthalmologica. 2012;227(2):107–10. [DOI] [PubMed] [Google Scholar]
- 8. Cohen E, Rosenblatt A, Bornstein S, Loewenstein A, Barak A, Schwartz S. Wide-angled endoillumination vs traditional scleral buckling surgery for retinal detachment - a comparative study. Clin Ophthalmol. 2019;13:287–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tomita Y, Kurihara T, Uchida A, Nagai N, Shinoda H, Tsubota K, et al. Wide-angle viewing system versus conventional indirect ophthalmoscopy for scleral buckling. Sci Rep. 2015;5:13256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Li XJ, Yang XP, Lyu XB. Comparison of scleral buckling using wide-angle viewing systems and indirect ophthalmoscope for rhegmatogenous retinal detachment. Int J Ophthalmol. 2016;9(9):1310–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nagpal M, Bhardwaj S, Mehrotra N. Scleral buckling for rhegmatogenous retinal detachment using vitrectomy-based visualization systems and chandelier illumination. Asia Pac J Ophthalmol. 2013;2(3):165–8. [DOI] [PubMed] [Google Scholar]
- 12. Kita M, Fujii Y, Kawagoe N, Hama S. Scleral buckling with a noncontact wide-angle viewing system in the management of retinal detachment with undetected retinal break: a case report. Clin Ophthalmol. 2013;7:587–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nam KY, Kim WJ, Jo YJ, Kim JY. Scleral buckling technique using a 25-gauge chandelier endoilluminator. Retina. 2013;33(4):880–2. [DOI] [PubMed] [Google Scholar]
- 14. Yokoyama T, Kanbayashi K, Yamaguchi T. Scleral buckling procedure with chandelier illumination for pediatric rhegmatogenous retinal detachment. Clin Ophthalmol. 2015;9:169–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Albalkini AS, Abdullatif AM, Albalkini MS, Macky TA, Khattab A, Attya M. Chandelier-assisted versus standard scleral buckling for primary rhegmatogenous retinal detachment: a randomized clinical study. Retina. 2022;42(9):1745–55. [DOI] [PubMed] [Google Scholar]
- 16. Narayanan R, Tyagi M, Hussein A, Chhablani J, Apte RS. Scleral buckling with wide-angled endoillumination as a surgical educational tool. Retina. 2016;36(4):830–3. [DOI] [PubMed] [Google Scholar]
- 17. Ali A, Ahmad N, Nawaz F, Munim A, Rafe A, Saleem H, et al. Efficacy of novel endoillumination assisted modified scleral buckling versus conventional scleral buckling. Pakistan J Med Health Sci. 2022;16(11):475–8. [Google Scholar]
- 18. Ilhan C, Citirik M, Dulger SC, Ozdemir M. Long-term complications of conventional and chandelier-assisted scleral buckle for primary repair of rhegmatogenous retinal detachment. J Curr Ophthalmol. 2022;34(3):323–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Talcott K, Obeid A, Chiang A, Garg S, Ho A, Regillo CD, et al. Comparison of chandelier-assisted scleral buckling versus traditional scleral buckling for rhegmatogenous retinal detachment repair at an academic teaching center. Invest Ophthalmol Vis Sci. 2017;58(8):4154. [Google Scholar]
- 20. Fujikawa A, Kumagami T, Tsuiki E, Kitaoka T. Evaluation of scleral buckling with chandelier illumination for rhegmatogenous retinal detachment. Invest Ophthalmol Vis Sci. 2016;57(12):1042. [Google Scholar]
- 21. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jo J, Moon BG, Lee JY. Scleral buckling using a non-contact wide-angle viewing system with a 25-gauge chandelier endoilluminator. Korean J Ophthalmol. 2017;31(6):533–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tosi GM, Malandrini A, Cevenini G, Neri G, Marigliani D, Cerruto A, et al. Vitreous incarceration in sclerotomies after valved 23-25-or 27-gauge and nonvalved 23- or 25-gauge macular surgery. Retina. 2017;37(10):1948–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sabti K, Kapusta M, Mansour M, Overbury O, Chow D. Ultrasound biomicroscopy of sclerotomy sites: the effect of vitreous shaving around sclerotomy sites during pars plana vitrectomy. Retina. 2001;21(5):464–8. [DOI] [PubMed] [Google Scholar]
- 25. Tanenbaum HL, Schepens CL, Elzeneiny I, Freeman HM. Macular pucker following retinal detachment surgery. Arch Ophthalmol. 1970;83(3):286–93. [DOI] [PubMed] [Google Scholar]
- 26. Yan H. Scleral buckling with a noncontact wide-angle viewing system in the management of rhegmatogenous retinal detachment. Eur J Ophthalmol. 2017;27(1):98–103. [DOI] [PubMed] [Google Scholar]
- 27. Caporossi T, Finocchio L, Barca F, Franco F, Tartaro R, Rizzo S. Scleral buckling for primary rhegmatogenous retinal detachment using a noncontact wide-angle viewing system with a cannula-based 27-G chandelier endoilluminator. Retina. 2019;39(Suppl 1):S144–50. [DOI] [PubMed] [Google Scholar]
- 28. Jeon GS, Han JR. Effectiveness of scleral buckling with a wide-field surgical microscope and chandelier illumination in retinal detachment repair. Ophthalmologica. 2019;242(1):31–7. [DOI] [PubMed] [Google Scholar]
- 29. Hu Y, Si S, Xu K, Chen H, Han L, Wang X, et al. Outcomes of scleral buckling using chandelier endoillumination. Acta Ophthalmol. 2017;95(6):591–4. [DOI] [PubMed] [Google Scholar]
- 30. Jahangir T, Tayyab H, Naeem M, Lateef Q, Khan AA. Modified scleral buckling with a non-contact wide angle viewing system and a 25g chandelier endoillumintor. Ann King Edw Med Univ. 2016;21(4):219. [Google Scholar]
- 31. Assi A, Abdelmassih Y, El-Khoury S. Endoillumination-assisted modified scleral buckling. Retina. 2018;38(2):320–4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All generated data are included in this paper. Further inquiries are to be directed to the corresponding author.