Key summary points
Aim
This the study describes the clinical presentation of COVID-19 and the risk factors for complications and death in octogenarian hospitalized patients across the different waves of the disease.
Findings
The most frequently reported symptoms in hospitalized octogenarian patients were fever, cough, dyspnea, and asthenia with acute respiratory distress syndrome, renal failure, and delirium being the most frequent complications. Regarding complications, diabetes mellitus, heart failure, dyspnea, and higher baseline levels of creatinine were identified as risk factors, while a higher Barthel index and presence of cough were found to be protective. Age, dyspnea, abnormal bilateral chest x-ray, CRP, and sodium were identified as risk factors for death.
Message
These findings could be valuable for managing future pandemics by contributing to tailored interventions and strategies to reduce COVID-19 mortality and complications in this patient group.
Supplementary Information
The online version contains supplementary material available at 10.1007/s41999-024-01063-1.
Keywords: COVID-19, Octogenarians, Clinical complications, Mortality, Risk factors, Pandemic waves, Aged 80 and over
Abstract
Objective
This study aimed to describe the clinical presentation of COVID-19 in hospitalized patients aged 80 or above and to identify predictors for death and complications throughout the epidemic waves of the disease.
Methods
This was an observational, multicenter, ambispective study conducted between March 2020 and August 2021 using data collected in five centers from southern metropolitan area of Barcelona (COVID-MetroSud cohort). Patients were grouped based on the pandemic waves of inclusion in the registry. We conducted a descriptive analysis, followed by bivariate and multivariate analyses (binary logistic regression) to identify predictors of risk for death or complications.
Results
A total of 1192 patients (mean [SD] age 85.7 [4.22] years and 46.8% female) were included. The most frequently reported symptoms in all waves were fever (63.1%), cough (56.5%), dyspnea (48.2%), and asthenia (27.5%). Laboratory and radiological findings consistently showed abnormal bilateral chest X-ray results (72.5% of patients) and elevated inflammatory markers such as lactate dehydrogenase (mean [SD] 335 [188] U/L), C-reactive protein (CRP) (mean [SD] 110 [88.4] U/L), and ferritin (mean [SD] 842 [1561] U/L). Acute respiratory distress syndrome (43.7%), renal failure (19.2%), and delirium (17.5%) were the most frequent complications. The overall mortality rate was 41.4% and declined across the epidemic waves. Age, diabetes mellitus, heart failure, dyspnea, and higher baseline levels of creatinine were identified as risk factors for complications, while a higher Barthel index and presence of cough were found to be protective. Age, dyspnea, abnormal bilateral chest X-ray, CRP, and sodium were identified as risk factors for death.
Conclusions
This study demonstrates the clinical presentation of COVID-19 (fever, cough, dyspnea, and asthenia) and the different risk factors for mortality and complications in octogenarian hospitalized patients throughout the pandemic. These findings could be highly valuable for managing future virus pandemics.
Supplementary Information
The online version contains supplementary material available at 10.1007/s41999-024-01063-1.
Introduction
The SARS-CoV-2 pandemic (COVID-19) had a significant impact on healthcare systems worldwide. Since its spread in March 2020 to the present day 765 million cases and 6.9 million deaths have been recorded worldwide [1]. In Spain, since the start of the pandemic, 13.8 million cases and 120,964 deaths have been reported, of which 931,616 cases and 77,136 deaths were among patients over 80 years of age [2, 3].
Older individuals experience physiological changes associated with aging, multiple age-related comorbidities, and polypharmacy [4]. The immune system of older adults undergoes various age-related changes, collectively known as immune senescence, which affect both the innate and adaptive immune systems. As a result, this population becomes more susceptible to infectious diseases [5]. These factors contribute to the occurrence of nonspecific and atypical clinical manifestations of COVID-19 [6].
Additionally, age is one of the most important factors associated with mortality in patients with COVID-19 admitted to the hospital [7, 8]. Early statistical data from China reported a mortality rate in people over 80 years of up to 14.8% [9, 10]. Similarly, a meta-analysis reported the highest mortality rates in this age segment, which were six times higher than in younger patients [11]. The increased mortality rates and complications in older patients may be attributed to a high multimorbidity, including dementia [12] and geriatric syndromes, increased frailty, and lower physiological and functional reserve [13].
Various epidemiological studies have described COVID-19 and identified risk factors for mortality in the general population. These factors include underlying pathologies, such as hypertension, cardiovascular disease, diabetes, chronic obstructive pulmonary disease, and cancer, presenting symptoms, such as dyspnea and expectoration, and radiological or analytical data, such as lactate dehydrogenase, D-dimer, and troponin [14–17]. However, limited epidemiological studies have investigated the clinical characteristics of COVID-19 in the very older population, only a few have identified risk factors for mortality, and none have focused on risk factors for complications in this population across multiple epidemics waves of the disease.
Considering Spain’s significant proportion of older individuals, with 6.2% of the population aged 80 or older, and the limited information available regarding patient profiles and clinical outcomes for this age group across different waves of the pandemic, there is a crucial need to gain a comprehensive understanding of COVID-19 in this specific population. This ambispective study aimed to describe the clinical presentation of COVID-19 in hospitalized patients aged 80 or above using data collected in five centers from the region south of Barcelona, Spain, throughout the epidemic waves of the disease. In addition, we aimed to identify predictors for death and complications in this population.
Methods
Study design and population
This was an observational, multicenter, ambispective study conducted between March 2020 and August 2021 in the southern metropolitan area of Barcelona, Spain. The data were collected from electronic medical records obtained from the COVID-MetroSud cohort, which comprises five large healthcare centers in the region: Hospital Universitario de Bellvitge (a tertiary-level hospital), Complejo Hospitalario Moisés Broggi, Consorci Sanitari Alt Penedès i Garraf, Hospital Viladecans, and Parc Sanitari Sant Joan de Déu (secondary-level hospitals). These healthcare centers collectively serve a reference population of 1,200,000 inhabitants and have a total of 2000 beds, including over 150 intensive care beds (expanded to 200 during the peak of the COVID-19 epidemic) and 200 intermediate care beds.
Patients were grouped based on the pandemic waves of inclusion in the registry. The first wave spanned from March 1 to March 15, 2020, the second wave from October 1 to November 30, 2020, the third wave from January 1 to February 28, 2021, the fourth wave from April 2021 1 to May 31, 2021 and the fifth wave from July 1 to August 31, 2021. No data were recorded for the fourth epidemic wave, which was of lower intensity and shorter duration than the others.
This study included hospitalized patients aged ≥ 80 years who were diagnosed with COVID-19 using real-time reverse transcription polymerase chain reaction (rRT-PCR) tests on nasal or pharyngeal samples. Patients with respiratory symptoms compatible with COVID-19 who were treated upon admission but had negative rRT-PCR tests were excluded. Additionally, patients who were not admitted, either because they were transferred to other hospitals or died in the emergency department, were also excluded.
Patient data were collected in real-time from the hospital information service in the REDCap (Research Electronic Data Capture) platform version 10.7.0, from admission with a prospective follow-up until death, discharge, transfer to another center (August 2021) [18, 19]. Data from deceased and discharged patients at the time of inclusion were retrospectively recorded.
Structured information (i.e., demographic data and laboratory results) was extracted from hospital electronic medical records for analysis. Unstructured information contained in the clinical course of patients was extracted by investigators from different participating centers using an electronic case report form implemented in the REDCap platform version 10.7.0 [18, 19].
For pseudonymization, all study data were identified by a case code and stored without any accompanying personal identification data. Considering that routinely collected data were anonymized, informed consent was not required. The sponsor and investigators of the study ensured that patient data procedures followed the General Data Protection Regulation (EU) 2016/679 (GDPR) and the Organic Law 3/2018 of December 5 on the Protection of Personal Data and guarantee of digital rights in Spain. This study was approved by the Research Ethics Committee of the Hospital Universitario de Bellvitge. Additionally, it was developed in accordance with ethical principles originating from the latest version of the Helsinki Declaration accepted by local authorities and in line with Good Clinical Practice (GCP) and the requirements of current Spanish regulations.
Endpoints and variables
The main objective of this study was to describe the clinical presentation of COVID-19 in hospitalized octogenarian patients throughout the epidemic waves of the disease. As secondary objectives, we evaluated the complications presented by older patients hospitalized due to COVID-19 and identified predictors for complications and mortality.
At the time of admission, variables related to the form of presentation of the disease were recorded, including presentation symptoms (e.g., presence or absence of cough, fever, dyspnea), vital signs (heart rate, blood pressure, and oxygen saturation), pulmonary auscultation data (presence of pathological sounds and type). At the time of disease presentation, the degree of radiological involvement (none, unilateral, or bilateral), all available laboratory data, and the appearance of clinical complications (ARDS, delirium, cardiac and renal complications) were also recorded. (Table S3).
In addition, we collected for each patient sociodemographic (date of birth, sex, age, institutionalization), and clinical data including Barthel index score (a scoring system that measures a patient’s performance in activities of daily living ranging from 0: dependent to 100: independent), toxic habits (smoker/alcoholic), body mass index (BMI), previous pathologies, degree of comorbidity according to the Charlson Index, and previous pharmacological treatment, including antiplatelet and anticoagulant drugs (active ingredient and dosage), anti-inflammatory drugs, antidiabetic drugs, and cardiovascular, respiratory, and immune system medications).
Statistical analysis
A descriptive analysis of all study variables was performed. Categorical variables were expressed as frequencies and percentages (%) and continuous variables were described using mean and standard deviation (SD), or median and interquartile range [IQR].
To identify predictors of risk for death or developing complications, we constructed several multivariate models (binary logistic regression), including variables significantly associated with the outcome in a previous bivariate analysis (p < 0.05) and those with clinical relevance according to the researchers' criteria. The independent variables were analyzed in blocks: (1) sociodemographic variables and pathological antecedents, (2) variables related to clinical presentation, and (3) laboratory findings. All models were adjusted for age and sex. Similarly, multivariate models were constructed to identify predictors of additional outcomes: cardiac complications, renal complications, and delirium. All estimates were reported with their odds ratio (OR) and 95% confidence interval (CI).
The database was reviewed to remove erroneous data and outliers as evaluated by the investigator. Patients with missing data for any of the following variables were excluded: age, sex, comorbidities evaluated in Charlson Index Score or outcome (discharge, exitus). Statistical analysis was performed using R version 4. 1.0 (R Core Team 2021).
Results
Study population and characteristics
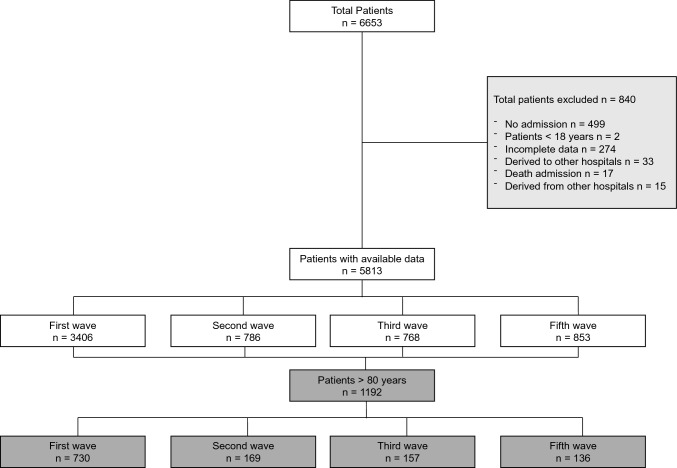
A total of 6653 patients diagnosed with COVID-19 were included in the MetroSud registry, of which 1192 were 80 or older and were included in this study. Of these, 61.2% (n = 730) were admitted in the first epidemic wave of COVID-19 and 38.8% (n = 462) in successive waves (Fig. 1).
Fig. 1.
Patient selection flowchart
Patients included had a mean age of 85.7 years (SD 4.22) and 46.8% were female. Most patients were non-smokers, did not reside in nursing homes, were overweight or obese, and had hypertension and dyslipidemia. The mean Barthel index was 78.2 (SD 28.9) and the Charlson comorbidity index was 6.23 (SD 1.84) (Table 1). Regarding previous treatments (described in Table S1), the most frequently prescribed medications were statins, ACE inhibitors, acetylsalicylic acid, and antidiabetic drugs. There were two vaccinated patients in the third wave (1.3%) and 121 (89.0%) in the fifth wave (Tables 1, 2).
Table 1.
Sociodemographic and clinical characteristics
| 1st wave n = 730 |
2nd wave n = 169 |
3rd wave n = 157 |
5th wave n = 136 |
Total n = 1192 |
|
|---|---|---|---|---|---|
| Sociodemographic characteristics | |||||
| Sex, n (%) | |||||
| Male | 394 (54.0) | 88 (52.1) | 80 (51.0) | 72 (52.9) | 634 (53.2) |
| Female | 336 (46.0) | 81 (47.9) | 77 (49.0) | 64 (47.1) | 558 (46.8) |
| Age (years), mean (SD) | 85.4 (4.04) | 86.0 (4.47) | 85.9 (4.36) | 86.9 (4.51) | 85.7 (4.22) |
| Smoker, n (%) | |||||
| No | 555 (76.0) | 125 (74.0) | 120 (76.4) | 90 (66.2) | 890 (74.7) |
| Yes | 13 (1.78) | 5 (2.96) | 5 (3.18) | 5 (3.68) | 28 (2.35) |
| Ex-smoker | 162 (22.2) | 39 (23.1) | 32 (20.4) | 41 (30.1) | 274 (23.0) |
| Alcohol consumption, n (%) | 10 (1.37) | 9 (5.33) | 9 (5.73) | 2 (1.47) | 30 (2.52) |
| Long-term facility, n (%) | 193 (26.4) | 19 (11.2) | 18 (11.5) | 10 (7.35) | 240 (20.1) |
| Complete COVID-19 vaccine | 0 (0%) | 0 (0%) | 2 (1.29%) | 121 (89,0%) | 123 (10.3%) |
| Categorical BMI (kg/m2), n (%) | |||||
| Low weight | 2 (0.41) | 1 (0.68) | 0 (0.00) | 0 (0.00) | 3 (0.33) |
| Normal | 96 (19.7) | 29 (19.6) | 25 (17.9) | 31 (25.4) | 181 (20.2) |
| Overweight | 248 (50.8) | 68 (45.9) | 57 (40.7) | 47 (38.5) | 420 (46.8) |
| Obese | 142 (29.1) | 50 (33.8) | 58 (41.4) | 44 (36.1) | 294 (32.7) |
Table 2.
Comorbidities
| 1st wave n = 730 |
2nd wave n = 169 |
3rd wave n = 157 |
5th wave n = 136 |
Total n = 1192 |
|
|---|---|---|---|---|---|
| Diabetes mellitus, n (%) | 245 (33.6) | 55 (32.5) | 52 (33.1) | 45 (33.1) | |
| With target organ involvement | 73 (29.8) | 12 (21.8) | 0 (0.00) | 0 (0.00) | 85 (21.4) |
| Without complications | 172 (70.2) | 43 (78.2) | 52 (100) | 45 (100) | 312 (78.6) |
| Chronic pulmonary pathology, n (%) | 192 (26.3) | 51 (30.2) | 36 (22.9) | 43 (31.6) | 322 (27.0) |
| COPD | 110 (57.3) | 22 (43.1) | 15 (41.7) | 28 (65.1) | 175 (54.3) |
| OSA | 50 (16.9) | 18 (35.3) | 7 (19.4) | 6 (14.0) | 81 (19.0) |
| Asthma | 39 (13.2) | 13 (25.5) | 8 (22.2) | 7 (16.3) | 67 (15.7) |
| Interstitial pneumopathy | 7 (3.65) | 3 (5.88) | 6 (16.7) | 5 (11.6) | 21 (6.52) |
| Hypertension, n (%) | 571 (78.2) | 136 (80.5) | 125 (79.6) | 121 (89.0) | 953 (79.9) |
| Dyslipidemia, n (%) | 327 (44.8) | 93 (55.0) | 93 (59.2) | 72 (52.9) | 585 (49.1) |
| Moderate-severe kidney disease, n (%) | 103 (14.1) | 19 (11.2) | 10 (6.37) | 4 (2.94) | 136 (11.4) |
| Hemodialysis, n (%) | 9 (1.23) | 2 (1.18) | 1 (0.64) | 2 (1.47) | 14 (1.17) |
| Heart failure, n (%) | 150 (20.5) | 28 (16.6) | 29 (18.5) | 32 (23.5) | 239 (20.1) |
| Coronary heart disease, n (%) | 81 (11.1) | 29 (17.2) | 25 (15.9) | 16 (11.8) | 151 (12.7) |
| Acute myocardial infarction, n (%) | 81 (11.1) | 16 (9.47) | 14 (8.92) | 14 (10.3) | 125 (10.5) |
| Atrial fibrillation, n (%) | 137 (18.8) | 44 (26.0) | 38 (24.2) | 43 (31.6) | 262 (22.0) |
| Hematologic malignancy, n (%) | 10 (1.37) | 8 (4.73) | 4 (2.55) | 14 (10.3) | 36 (3.02) |
| Non-metastatic malignancy, n (%) | 71 (9.73) | 22 (13.0) | 19 (12.1) | 26 (19.1) | 138 (11.6) |
| Ictus, n (%) | 112 (15.3) | 23 (13.6) | 24 (15.3) | 22 (16.2) | 181 (15.2) |
| Ischemic or hemorrhagic stroke with sequelae | 29 (38.7) | 9 (39.1) | 7 (29.2) | 5 (22.7) | 50 (34.7) |
| TIA or ischemic stroke without sequelae | 46 (61.3) | 14 (60.9) | 17 (70.8) | 17 (77.3) | 94 (65.3) |
| Peripheral vasculopathy, n (%) | 50 (6.85) | 23 (13.6) | 19 (12.1) | 11 (8.09) | 103 (8.64) |
| Dementia, n (%) | 173 (23.7) | 44 (26.0) | 31 (19.7) | 33 (24.3) | 281 (23.6) |
| Anxiety, n (%) | 31 (4.25) | 14 (8.28) | 13 (8.28) | 6 (4.41) | 64 (5.37) |
| Depression, n (%) | 67 (9.18) | 25 (14.8) | 23 (14.6) | 12 (8.82) | 127 (10.7) |
| Connective tissue disease, n (%) | 37 (5.07) | 13 (7.69) | 14 (8.92) | 11 (8.09) | 75 (6.29) |
| Rheumatoid arthritis | 7 (22.6) | 5 (38.5) | 0 (0.00) | 6 (54.5) | 18 (26.1) |
| SLE | 1 (3.23) | 0 (0.00) | 0 (0.00) | 1 (9.09) | 2 (2.90) |
| Other | 23 (74.2) | 8 (61.5) | 14 (100) | 4 (36.4) | 49 (71.0) |
| Neurodegenerative disease, n (%) | 35 (4.79) | 14 (8.28) | 8 (5.10) | 3 (2.21) | 60 (5.03) |
| Barthel Index, mean (SD) | 75.7 (31.8) | 79.0 (26.6) | 83.4 (23.8) | 79.6 (25.7) | 78.2 (28.9) |
| Charlson Index, mean (SD) | 6.22 (1.85) | 6.43 (2.10) | 5.99 (1.63) | 6.27 (1.58) | 6.23 (1.84) |
SD standard deviation, BMI body mass index, DM diabetes mellitus, COPD chronic obstructive pulmonary disease, OSA obstructive sleep disease, TIA transient ischemic attack, SLE systemic lupus erythematosus
Clinical presentation of COVID-19
The most common recorded symptoms were fever (63.1%), cough (56.5%), dyspnea (48.2%), and asthenia (27.5%) (Table 3). The overall incidence of delirium was 11.0% and was higher during the initial two waves of the epidemic than the subsequent two waves. Rhinorrhea and headache incidence were higher in third and fifth waves. In the physical examination findings (Table 4), as the epidemic waves progressed, patients presented hypoxemia less frequently and better respiratory rate and SAFI (oxygen saturation [SpO2]/fraction of inspired oxygen [FiO2] ratio).
Table 3.
Most frequent patient’s symptoms at admission (> 5% of patients), n (%)
| 1st wave n = 730 |
2nd wave n = 169 |
3rd wave n = 157 |
5th wave n = 136 |
Total n = 1192 |
|
|---|---|---|---|---|---|
| Rhinorrhea | 23 (3.15) | 5 (2.96) | 7 (4.46) | 16 (11.8) | 51 (4.28) |
| Anosmia | 14 (1.92) | 11 (6.51) | 11 (7.01) | 5 (3.68) | 41 (3.44) |
| Ageusia | 25 (3.42) | 11 (6.51) | 14 (8.92) | 6 (4.41) | 56 (4.70) |
| Arthromyalgia | 133 (18.2) | 32 (18.9) | 12 (7.64) | 15 (11.0) | 192 (16.1) |
| Fever | 495 (67.8) | 101 (59.8) | 80 (51.0) | 76 (55.9) | 752 (63.1) |
| Chills | 48 (13.3) | 9 (8.91) | 4 (5.00) | 3 (3.95) | 64 (10.3) |
| Cough | 415 (56.8) | 91 (53.8) | 86 (54.8) | 82 (60.3) | 674 (56.5) |
| Dyspnea | 359 (49.2) | 81 (47.9) | 73 (46.5) | 62 (45.6) | 575 (48.2) |
| Expectoration | 116 (15.9) | 26 (15.4) | 21 (13.4) | 27 (19.9) | 190 (15.9) |
| Diarrhea | 135 (18.5) | 34 (20.1) | 38 (24.2) | 29 (21.3) | 236 (19.8) |
| Vomiting | 42 (5.75) | 8 (4.73) | 7 (4.46) | 8 (5.88) | 65 (5.45) |
| Nausea | 49 (6.71) | 9 (5.33) | 5 (3.18) | 7 (5.15) | 70 (5.87) |
| Asthenia | 168 (23.0) | 59 (34.9) | 62 (39.5) | 39 (28.7) | 328 (27.5) |
| Anorexia | 79 (10.8) | 26 (15.4) | 33 (21.0) | 21 (15.4) | 159 (13.3) |
| Headache | 25 (3.42) | 9 (5.33) | 17 (10.8) | 15 (11.0) | 66 (5.54) |
| Chest pain | 24 (3.29) | 9 (5.33) | 6 (3.82) | 3 (2.21) | 42 (3.52) |
| Abdominal pain | 24 (3.29) | 10 (5.92) | 9 (5.73) | 6 (4.41) | 49 (4.11) |
| Delirium* | 85 (11.6) | 28 (16.6) | 9 (5.73) | 9 (6.62) | 131 (11.0) |
| Bacterial infection | 17 (2.33) | 3 (1.78) | 0 (0.00) | 1 (0.74) | 21 (1.76) |
| Previous visit to the emergency room | 71 (9.73) | 21 (12.4) | 14 (8.92) | 12 (8.82) | 118 (9.90) |
*Delirium was defined as any acute alteration in cognition or inattention in the emergency report or at the time of admission
Table 4.
Physical examination findings
| 1st wave n = 730 |
2nd wave n = 169 |
3rd wave n = 157 |
5th wave n = 136 |
Total n = 1192 |
|
|---|---|---|---|---|---|
| Temperature ºC, mean (SD) | 36.9 (1.02) | 36.7 (0.88) | 36.6 (0.81) | 36.7 (0.84) | 36.8 (0.96) |
| Provided FiO2%, mean (SD) | 28.4 (18.6) | 28.7 (16.5) | 30.2 (18.5) | 28.9 (14.3) | 28.7 (17.8) |
| SBP mmHg, mean (SD) | 131 (23.6) | 136 (26.1) | 137 (24.5) | 135 (23.6) | 133 (24.2) |
| DBP mmHg, mean (SD) | 70.2 (14.9) | 70.9 (12.8) | 74.5 (13.1) | 69.5 (13.2) | 70.8 (14.3) |
| Oxygen saturation %, mean (SD) | 92.1 (6.89) | 93.6 (4.83) | 94.5 (4.91) | 95.0 (3.40) | 93.0 (6.16) |
| Heart rate BPM, mean (SD) | 87.3 (18.2) | 83.3 (18.1) | 84.1 (18.6) | 81.5 (16.4) | 85.6 (18.1) |
| Respiratory rate, BPM, mean (SD) | 22.9 (6.91) | 22.8 (6.24) | 22.3 (5.99) | 20.4 (4.82) | 22.5 (6.47) |
| SAFI, mean (SD) | 386 (104) | 380 (103) | 371 (107) | 369 (94.4) | 381 (103) |
| Normal respiratory exploration, n (%) | 100 (18.6) | 26 (16.6) | 23 (14.7) | 15 (11.0) | 164 (16.6) |
| Abnormal respiratory exploration, n (%) | 373 (86.3) | 114 (87.0) | 118 (88.7) | 107 (88.4) | 712 (87.1) |
| Sibilants | 50 (12.3) | 20 (15.3) | 11 (8.27) | 20 (16.5) | 101 (12.8) |
| Roncus | 74 (17.8) | 27 (20.6) | 14 (10.5) | 16 (13.2) | 131 (16.4) |
SD standard deviation, SBP systolic blood pressure, DBP diastolic blood pressure, BPM beats/breaths per minute, SAFI oxygen saturation (SpO2)/fraction of inspired oxygen (FiO2) ratio
Radiological and laboratory findings on admission are described in Table S2. Older patients admitted for COVID-19 frequently presented leukocytosis with neutrophilia and lymphopenia. In addition, they had elevated lactate dehydrogenase (LDH) and acute phase reactants (C-reactive protein [CRP] and serum ferritin levels), and altered coagulation parameters (fibrinogen, and D-dimer) and liver and renal functions.
Mean levels of inflammatory parameters (D-dimer, CRP, LDH, and ferritin levels) decreased after the first wave. In addition, bilateral infiltrates were detected at lower frequencies after the first wave.
Complications
Mortality and complications are described in Table S3. Of the patients included, 41.4% (n = 493) died. Mortality decreased progressively with each new wave, from 46.2% in the first wave to 24.3% in the fifth wave. Overall, 47.9% (n = 569) of patients experienced some complications. A higher prevalence of complications was observed in the first and second epidemic waves and decreased in the third and fifth waves. The most common complications were acute respiratory distress syndrome (ARDS) (43.7%), followed by renal failure (19.2%), and delirium (17.5%). Table S4 shows the results of a stratified analysis of mortality and complications separately from the first wave to the combined subsequent waves.
Variables associated with the risk of complications and death
The multivariate analysis of risk factors associated with death and complications, including sociodemographic variables and comorbidities, showed that age was significantly associated with the risk of death, and age, male sex, and diabetes mellitus were associated with the risk of complications (Table 5). Diabetes mellitus (DM) and heart failure were associated with a 58% and 61% increase in the risk of complications, whereas, with each 5-year increment in age, the risk of complications and death increased by 22% (p = 0.039) and 25%, respectively (p = 0.024). Furthermore, 10-units increment in the Barthel index score was associated with a 7% lower risk of both complications and death (p = 0.012 and p = 0.028, respectively).
Table 5.
Multivariate analysis assessing the association between sociodemographic, clinical and laboratory predictors with the risk of complications and death
| Predictors | Risk of any complication | Risk of death | ||||||
|---|---|---|---|---|---|---|---|---|
| Odds ratio | Std. Error | 95% CI | p- value | Odds Ratio | Std. Error | 95% CI | p-value | |
| Sociodemographic | ||||||||
| Age | 1.22 | 0.12 | 1.01–1.48 | 0.039 | 1.25 | 0.12 | 1.03–1.51 | 0.024 |
| Sex (Female) | 0.65 | 0.11 | 0.47–0.90 | 0.010 | 0.79 | 0.13 | 0.56–1.08 | 0.130 |
| Barthel index | 0.93 | 0.03 | 0.87–0.99 | 0.035 | 0.93 | 0.03 | 0.87–0.98 | 0.028 |
| Diabetes mellitus | 1.58 | 0.26 | 1.14–2.20 | 0.006 | ||||
| Hypertension | 0.92 | 0.19 | 0.61–1.39 | 0.682 | 0.67 | 0.14 | 0.45–1.02 | 0.058 |
| Dyslipidemia | 1.13 | 0.18 | 0.82–1.55 | 0.455 | 1.32 | 0.21 | 0.96–1.81 | 0.093 |
| COPD | 0.69 | 0.13 | 0.48–1.00 | 0.053 | 0.98 | 0.19 | 0.67–1.43 | 0.931 |
| Dementia | 1.01 | 0.22 | 0.66–1.55 | 0.961 | 1.13 | 0.25 | 0.74–1.73 | 0.565 |
| Corticosteroids | 1.22 | 0.25 | 0.81–1.83 | 0.345 | 1.20 | 0.25 | 0.79–1.80 | 0.3841 |
| Heart failure | 1.61 | 0.30 | 1.12–2.33 | 0.010 | 1.11 | 0.21 | 0.76–1.60 | 0.598 |
| Clinical | ||||||||
| Cough | 0.83 | 0.12 | 0.62–1.11 | 0.217 | 0.58 | 0.09 | 0.43–0.78 | < 0.001 |
| Dyspnea | 1.39 | 0.20 | 1.04–1.85 | 0.025 | 1.84 | 0.28 | 1.37–2.49 | < 0.001 |
| Abnormal unilateral chest x-ray | 0.84 | 0.25 | 0.47–1.49 | 0.548 | 1.17 | 0.39 | 0.61–2.26 | 0.638 |
| Abnormal bilateral chest x-ray | 0.86 | 0.20 | 0.55–1.35 | 0.504 | 2.16 | 0.56 | .31–3.65 | 0.003 |
| Delirium | 2.77 | 0.67 | 1.73–4.49 | < 0.001 | ||||
| Laboratory | ||||||||
| Total leukocytes | 1.07 | 0.23 | 0.70–1.62 | 0.751 | 1.16 | 0.25 | 0.75–1.78 | 0.496 |
| D- Dimer | 1.00 | 0.00 | 1.00–1.00 | 0.015 | 1.00 | 0.00 | 1.00–1.00 | 0.077 |
| CRP | 1.02 | 0.01 | 1.00–1.04 | 0.060 | 1.07 | 0.01 | 1.05–1.09 | < 0.001 |
| Sodium | 1.15 | 0.15 | 0.89–1.50 | 0.285 | 1.80 | 0.25 | 1.37–2.40 | < 0.001 |
| Creatinine | 2.45 | 0.41 | 1.78–3.63 | < 0.001 | 1.34 | 0.21 | 0.99–1.84 | 0.061 |
Age (continuous variable) was evaluated as 5-year increment. Barthel Index was evaluated as 10 units increment. Total leukocytes, CRP, sodium, and creatinine were evaluated as 10 units increments. Ddimer was evaluated as 50 units increments. Bold values indicate significant findings
Std standard, 95% CI 95% confidence interval, COPD chronic obstructive pulmonary disease, CRP C-reactive protein
In multivariate models that considered clinical variables, dyspnea was associated with an 84% increased risk of death (p < 0.001), an abnormal bilateral chest X-ray increased the risk of death by 116% (p = 0.024), and the presence of delirium increased the risk of death by 177% (p < 0.001). Interestingly, cough emerged as a protective factor against death, reducing the risk by 42% (p < 0.001). Additionally, dyspnea also increased the risk of complications by 39% (p = 0.024) (Table 5).
In multivariate models incorporating laboratory findings, a 10-unit increment in creatinine levels was associated with a 145% increment in the risk of complications (p < 0.001). Additionally, a 10-unit increase in CRP and sodium levels was associated with a 7% (p < 0.001) and 80% (p < 0.001) increase in the risk of death, respectively (Table 5).
Variables associated with the risk of specific complications
In the multivariate analysis assessing risk factors for the development of delirium as a complication of COVID-19 (described in Table S5), female sex was identified as a protective factor, reducing the risk by 39% (p = 0.023). On the other hand, dementia and each 10-unit increase in sodium levels were associated with 86% (p < 0.019) and 45% (p < 0.016) increase in the risk of developing the syndrome, respectively. In terms of cardiac complications, heart failure, and dyspnea were identified as the only predictive factors, with a 170% (p < 0.001) and 156% (p < 0.001) increase in the risk of occurrence, respectively (Table S6). Finally, DM, heart failure, and each 10-unit increment in sodium levels were associated with an increase of 86% (p = 0.008), 67% (p = 0.029), and 62% (p < 0.002) in the risk of renal complications, respectively. Notably, each 10-unit increase in baseline creatinine levels was found to be related to an eight-fold increase in the risk of renal complications (p < 0.001) (Table S7).
A summary of the variables associated with death and complications is included in Table S8.
Discussion
This study comprehensively describes the clinical presentation of COVID-19 and the risk factors for complications and death in octogenarian hospitalized patients across the different waves of the disease. Thus, the most frequently reported symptoms in all waves were fever, cough, dyspnea, and asthenia. Laboratory and radiological findings consistently showed abnormal bilateral chest X-ray results and elevated inflammatory markers such as LDH, CRP, and ferritin. Among the observed complications, ARDS, renal failure, and delirium were the most frequent. The overall mortality rate was 41.4% and declined across the epidemic waves.
In our study, age, DM, heart failure, dyspnea, and higher baseline levels of creatinine were identified as risk factors for complications, while a higher Barthel index and presence of cough were found to be protective. Similarly, age, dyspnea, delirium, abnormal bilateral chest x-ray, CRP, and sodium were risk factors for death. In terms of specific complications, dementia and sodium levels were identified as risk factors for delirium, while female sex was a protective factor. Additionally, dementia and elevated sodium levels were identified as risk factors for cardiac complications, and DM, heart failure, and elevated creatinine levels for renal complications.
The comorbidities most frequently found in our study (hypertension and dyslipidemia) are also considered common older patients without COVID-19, suggesting that these conditions may not be related to the disease [20]. However, hospitalized patients in this cohort had a higher prevalence of overweight or obesity in contrast to general older Spanish population without COVID-19 [21].
Regarding the clinical symptoms, the most frequently observed in our study (fever, cough, dyspnea, and asthenia) have also been reported as the most common symptoms in cohorts of older Spanish patients hospitalized for COVID-19 [22–24]. During the later epidemic waves, the clinical presentation changed significantly, with a higher proportion of patients presenting with rhinorrhea and headache. Respiratory parameters also improved on average in the later waves, suggesting less severe respiratory involvement. Consistent with the findings of other studies, the older individuals in our cohort predominantly presented elevated inflammatory markers, such as ferritin and CRP, and frequent elevation of D-dimer and LDH [22, 23]. This laboratory profile did not differ across the various epidemic waves.
One in ten patients in our sample presented with delirium at admission, with a higher incidence during the initial two waves of the epidemic compared to the subsequent two, similar to that described by Minnema [25]. The decrease in clinical severity among hospitalized older patients in each new wave could explain the decreasing incidence. Furthermore, the relaxation of hospital regulations in later waves allowed companions in patient rooms. Nevertheless, delirium is frequently underdiagnosed and underreported, suggesting its actual incidence during COVID-19 could be higher than detected in our study [26]. Moreover, the methods used for delirium detection vary across studies, lacking rigor, leading to highly heterogeneous reported frequencies. Gutiérrez-Rodríguez and Annweiler reported a similar frequency of delirium to our study in the subgroup of patients aged 80 or older, while other authors found higher frequencies [22, 23, 27–29].
A decrease in the prevalence of complications was observed in the third and fifth waves possibly due to the emergence of vaccines, more effective treatments, changes in virus variants and reduced assistance pressure in hospitals. The proportion of patients experiencing ARDS (40%) was similar to other studies [6, 22, 23]. Despite being high, the incidence of ARDS in hospitalized patients is likely underestimated in most studies, as physicians do not always document this diagnosis in the medical records [29]. After ARDS, the most common complications were delirium and renal failure, with one-fifth of the hospitalized older patients developing acute kidney injury. Other cohort studies assessing hospitalized older patients have reported acute kidney injury, which is likely related to tubular injury caused by local and systemic inflammation and immune systems, aggravated by hemodynamic instability [22, 23, 31]. Moreover, underlying chronic kidney disease is frequent among octogenarians, further contributing to an increased risk of developing acute kidney injury during hospitalization.
Older patients are particularly vulnerable to developing severe forms of the disease [31]. The current study further confirms the clinical presentation, severity, and high mortality rate associated with COVID-19 infection in very older patients during the SARS-CoV-2 pandemic. The mortality rate, exceeding 40% in our hospitalized octogenarian group, aligns with the findings reported by two other Spanish cohorts [29, 33]. Notably, mortality was higher in the first wave than in the others, and the mortality rate decreased with the progression of the epidemic waves, likely reflecting the successful use of vaccines (starting massively in March 2021) and more effective treatments as the pandemic advanced. Few studies on the older patients have analyzed clinical presentation, hospital mortality, and their associated factors across different epidemic waves [34, 35]. Only one previous study has specifically focused on octogenarian patients [23].This study, that focused only on the first two epidemic waves and did not analyze risk factors for complications, found a slightly higher overall fatality rate than ours (46.9%), possibly because the study did not include vaccinated patients, which is associated with lower mortality.
Regarding the risk of mortality during hospitalization, this study found that age and elevated levels of CRP and sodium were associated with a higher risk of death. These findings have been consistent with previous studies conducted on older patients [24, 36, 37]. During the hospitalization of COVID-19 patients, both hyponatremia and hypernatremia have been associated with worse prognoses and increased mortality rates [38, 39]. In our study, elevated sodium levels emerged as a risk factor for death and complications, possibly because patients in a more severe condition may experience tachypnea, fever, and dehydration. On the other hand, patients who presented with a cough at the time of hospitalization and those with higher Barthel index scores had a lower risk of death. While no studies specifically analyze cough as a risk factor for mortality in older patients, studies encompassing patients of all ages have yielded contradictory results [40, 41]. Regarding the Barthel index score, other studies have reported similar findings to ours, indicating a higher degree of dependence as a risk factor for mortality [24, 36].
This study was limited by the use of secondary data obtained from medical records, which could introduce information biases related to underreporting certain symptoms or pathologies, in addition to missing information. For the same reason, variables associated with geriatric syndromes (such as malnutrition, falls, or frailty) could not be studied. However, the pre-existing functional status (Barthel index) and delirium were adequately recorded in terms of frequency and quality, allowing their inclusion in our analysis and confirming their significant role in COVID-19 among the older people. Vaccination started late in this study, resulting in a relatively low number of vaccinated patients, limited to the most recent epidemic waves. This is why the effect of vaccines could not be well studied, although it may be related to the improved prognosis observed in the latest epidemic waves, as reflected in our data. Additionally, the heterogeneity in the collection of certain laboratory parameters across different hospitals (with varying units or reference levels) and throughout the different waves posed a challenge for analysis. Therefore, some laboratory parameters that could not be standardized across the databases were excluded from the analysis, precluding their inclusion in the multivariate analysis. It is important to note that our findings exclusively apply to older patients hospitalized with COVID-19 and may not be applicable to older individuals with milder forms of the disease who did not require hospitalization.
Despite these limitations, a substantial number of hospitalized octogenarian patients with COVID-19 were included across different waves of the disease in various hospital centers, yielding robust results. Thus, this study offers valuable insights into the disease among the older people, specifically regarding the characteristics of hospitalized patients, the clinical manifestations of the disease, abnormalities observed in laboratory and radiological assessments, the frequency and types of complications, as well as the in-hospitalmortality rate and prognostic factors, which may help identify older patients who are at risk of developing complications or death during their hospital stay.
Conclusions
This study describes the clinical characteristics, predictors of complications, and mortality in octogenarian patients hospitalized with COVID-19 across multiple epidemic waves. Our findings provide insight into the disease and its risk factors in older patients, contributing to the development of tailored therapeutic interventions and strategies aimed at reducing mortality and complications from COVID-19 in this patient group.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank CERCA Programme/Generalitat de Catalunya for institutional support. MetroSud Study group: Carlota Gudiol, Judit Aranda-Lobo, Montserrat Sanmartí, Encarna Moreno, Maria C Alvarez, Ana Faura, Martha González, Paula Cruz, Mireia Colom, Andrea Perez, Laura Serrano, Sebastià Videla. Divine Study group: Mireia Besalú, Erik Cobo, Jordi Cortés, Daniel Fernández, Leire Garmendia, Guadalupe Gómez, Pilar Hereu, Klaus Langohr, Núria Pérez-Álvarez, Xavier Piulachs. Natàlia Pallares, Cristian Tebé, Mireia Besalú, Erik Cobo, Jordi Cortés, Daniel Fernández, Klaus Langohr, Núria Pérez-Álvarez, Xavier Piulachs, Guadalupe Gómez were partially supported by Departament de Recerca i Universitats (Generalitat de Catalunya) [2021 SGR 01421]. The authors thank the i2e3 team (Barcelona, Spain) and especially Sara Gutierrez, Ph.D., and Sara Cervantes, Ph.D., for providing medical writing support.
Declarations
Conflict of interest
The authors declare that the have no conflict of interest.
Ethical approval
For pseudonymization, all study data were identified by a case code and stored without any accompanying personal identification data. The sponsor and investigators of the study ensured that patient data procedures followed the General Data Protection Regulation (EU) 2016/679 (GDPR) and the Organic Law 3/2018 of December 5 on the Protection of Personal Data and guarantee of digital rights in Spain. This study was approved by the Research Ethics Committee of the Hospital Universitario de Bellvitge. Additionally, it was developed in accordance with ethical principles originating from the latest version of the Helsinki Declaration accepted by local authorities and in line with Good Clinical Practice (GCP) and the requirements of current Spanish regulations.
Informed consent
Considering that routinely collected data were anonymized, informed consent was not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
6/4/2025
A Correction to this paper has been published: 10.1007/s41999-025-01249-1
Contributor Information
Marta Arroyo-Huidobro, Email: arroyo@clinic.cat.
On behalf of MetroSud and Divine Study Group:
Carlota Gudiol, Judit Aranda-Lobo, Montserrat Sanmartí, Encarna Moreno, Maria C. Alvarez, Ana Faura, Martha González, Paula Cruz, Mireia Colom, Andrea Perez, Laura Serrano, Sebastià Videla, Mireia Besalú, Erik Cobo, Jordi Cortés, Daniel Fernández, Leire Garmendia, Guadalupe Gómez, Pilar Hereu, Klaus Langohr, Núria Pérez-Álvarez, Xavier Piulachs, Natàlia Pallares, Cristian Tebé, Mireia Besalú, Erik Cobo, Jordi Cortés, Daniel Fernández, Klaus Langohr, Núria Pérez-Álvarez, Xavier Piulachs, and Guadalupe Gómez
References
- 1.World Healt Organization. Coronavirus (COVID-19) Dashboard. Accessed May 9, 2023. https://covid19.who.int/
- 2.Ministerio de Sanidad España. Situación actual enfermedad por nuevo coronavirus, COVID-19. Accessed May 9, 2023. https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/situacionActual.htm
- 3.Equipo COVID-19. RENAVE. Informe No 176. Situación de COVID-19 En España.; 2023. Accessed May 9, 2023. https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Paginas/InformesCOVID-19.aspx
- 4.Cope DG (2013) Polypharmacy in older adults: the role of the advanced practitioner in oncology. J Adv Pract Oncol 4(2):107–112 [PMC free article] [PubMed] [Google Scholar]
- 5.Nikolich-Zugich J, Knox KS, Rios CT, Natt B, Bhattacharya D, Fain MJ (2020) SARS-CoV-2 and COVID-19 in older adults: what we may expect regarding pathogenesis, immune responses, and outcomes. Geroscience 42(2):505–514. 10.1007/s11357-020-00186-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen T, Dai Z, Mo P et al (2020) Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China: a single-centered, retrospective study. J Gerontol 75(9):1788–1795. 10.1093/gerona/glaa089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez-Nava G, Yanez-Bello MA, Trelles-Garcia DP et al (2021) Clinical characteristics and risk factors for death of hospitalized patients with COVID-19 in a community hospital: a retrospective cohort study. Mayo Clin Proc Innov Qual Outcomes 5(1):1–10. 10.1016/j.mayocpiqo.2020.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Martín-Sánchez FJ, del Toro E, Cardassay E et al (2020) Clinical presentation and outcome across age categories among patients with COVID-19 admitted to a Spanish Emergency Department. Eur Geriatr Med 11(5):829–841. 10.1007/s41999-020-00359-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu K, Chen Y, Lin R, Han K (2020) Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J Infect 80(6):e14–e18. 10.1016/j.jinf.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhao H, Huang Y, Huang Y (2020) Mortality in older patients with COVID-19. J Am Geriatr Soc 68(8):1685–1687. 10.1111/jgs.16649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bonanad C, García-Blas S, Tarazona-Santabalbina F et al (2020) The effect of age on mortality in patients with COVID-19: a meta-analysis with 611,583 subjects. J Am Med Dir Assoc 21(7):915–918. 10.1016/j.jamda.2020.05.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Madruga Flores M, Corrales López M, Gómez-Pavón J (2023) El impacto de las primeras olas pandémicas de la COVID-19 en las personas mayores con demencia. Aten. Prim. (Barc., Ed. Impr.) 2023:102622–102622. 10.1016/j.aprim.2023.102622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bonanad C, García-Blas S, Tarazona-Santabalbina FJ et al (2020) Coronavirus: la emergencia geriátrica de 2020. Documento conjunto de la Sección de Cardiología Geriátrica de la Sociedad Española de Cardiología y la Sociedad Española de Geriatría y Gerontología. Rev Esp Cardiol 73(7):569–576. 10.1016/j.recesp.2020.03.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Parohan M, Yaghoubi S, Seraji A, Javanbakht MH, Sarraf P, Djalali M (2020) Risk factors for mortality in patients with Coronavirus disease 2019 (COVID-19) infection: a systematic review and meta-analysis of observational studies. Aging Male 23(5):1416–1424. 10.1080/13685538.2020.1774748 [DOI] [PubMed] [Google Scholar]
- 15.Lv Z, Lv S (2021) Clinical characteristics and analysis of risk factors for disease progression of COVID-19: a retrospective Cohort Study. Int J Biol Sci 17(1):1–7. 10.7150/ijbs.50654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Booth A, Reed AB, Ponzo S et al (2021) Population risk factors for severe disease and mortality in COVID-19: a global systematic review and meta-analysis. PLoS ONE 16(3):e0247461. 10.1371/journal.pone.0247461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Du RH, Liang LR, Yang CQ et al (2020) Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J 55(5):2000524. 10.1183/13993003.00524-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harris PA, Taylor R, Minor BL et al (2019) The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 95:103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jaul E, Barron J (2017) Age-related diseases and clinical and public health implications for the 85 years old and over population. Front Public Health. 10.3389/fpubh.2017.00335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laboratorio Envejecimiento en red. Un perfil de las personas mayores en España 2022 Indicadores estadísticos básicos. Published 2022. Accessed July 20, 2023. http://envejecimiento.csic.es/documentos/documentos/enred-indicadoresbasicos2022.pdf
- 22.Ramos-Rincon JM, Buonaiuto V, Ricci M et al (2021) Clinical characteristics and risk factors for mortality in very old patients hospitalized with COVID-19 in Spain. J Gerontol 76(3):e28–e37. 10.1093/gerona/glaa243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ramos-Rincon JM, Cobos-Palacios L, López-Sampalo A et al (2022) Differences in clinical features and mortality in very old unvaccinated patients (≥ 80 years) hospitalized with COVID-19 during the first and successive waves from the multicenter SEMI-COVID-19 Registry (Spain). BMC Geriatr 22(1):546. 10.1186/s12877-022-03191-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rodríguez-Sánchez I, Redondo-Martín M, Furones-Fernández L et al (2021) Functional, clinical, and sociodemographic variables associated with risk of in-hospital mortality by COVID-19 in people over 80 years old. J Nutr Health Aging 25(8):964–970. 10.1007/s12603-021-1664-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Minnema J, Tap L, van der Bol JM, van Deudekom FJ, Faes MC, Jansen SW et al (2023) Delirium in older patients with COVID-19: Prevalence, risk factors and clinical outcomes across the first three waves of the pandemic. Int J Geriatr Psychiatry 38(11):e6024. 10.1002/gps.6024 [DOI] [PubMed] [Google Scholar]
- 26.Kennedy M, Helfand BKI, Gou RY et al (2020) Delirium in older patients with COVID-19 presenting to the emergency department. JAMA Netw Open 3(11):e2029540. 10.1001/jamanetworkopen.2020.29540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gutiérrez Rodríguez J, Montero Muñoz J, Jiménez Muela F, Guirola García-Prendes C, Martínez Rivera M, Gómez AL (2020) Variables asociadas con mortalidad en una población de pacientes mayores de 80 años y con algún grado de dependencia funcional, hospitalizados por COVID-19 en un Servicio de Geriatría. Rev Esp Geriatr Gerontol 55(6):317–325. 10.1016/j.regg.2020.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Annweiler C, Sacco G, Salles N et al (2021) National French Survey of Coronavirus Disease (COVID-19) symptoms in people aged 70 and over. Clin Infect Dis 72(3):490–494. 10.1093/cid/ciaa792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lozano-Montoya I, Quezada-Feijoo M, Jaramillo-Hidalgo J, Garmendia-Prieto B, Lisette-Carrillo P, Gómez-Pavón FJ (2021) Mortality risk factors in a Spanish cohort of oldest-old patients hospitalized with COVID-19 in an acute geriatric unit: the OCTA-COVID study. Eur Geriatr Med 12(6):1169–1180. 10.1007/s41999-021-00541-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Song X, Weister TJ, Dong Y, Kashani KB, Kashyap R (2021) Derivation and validation of an automated search strategy to retrospectively identify acute respiratory distress patients per Berlin definition. Front Med (Lausanne). 10.3389/fmed.2021.614380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Legrand M, Bell S, Forni L et al (2021) Pathophysiology of COVID-19-associated acute kidney injury. Nat Rev Nephrol 17(11):751–764. 10.1038/s41581-021-00452-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.D’ascanio M, Innammorato M, Pasquariello L et al (2021) Age is not the only risk factor in COVID-19: the role of comorbidities and of long staying in residential care homes. BMC Geriatr 21(1):63. 10.1186/s12877-021-02013-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fernández Ibáñez JM, Morales Ballesteros MC, Galindo Andúgar MÁ, Fernández Anguita MJ, Arias Arias Á, Barberá-Farré JR (2022) Factores de riesgo de mortalidad en pacientes mayores de 65 años hospitalizados por COVID-19. Rev Esp Geriatr Gerontol 57(1):6–12. 10.1016/j.regg.2021.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Paepe A, Vlieghe E, Brusselaers N, Soentjens P, Theunissen C, Brosius I, van Ierssel SH (2024) COVID-19 in three waves in a tertiary referral hospital in Belgium: a comparison of patient characteristics, management, and outcome. Virol J 21(1):1–11. 10.1186/s12985-024-02360-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fericean RM, Rosca O, Citu C, Manolescu D, Bloanca V, Toma AO, Oancea C (2022) COVID-19 clinical features and outcomes in elderly patients during six pandemic waves. J Clin Med 11(22):6803. 10.3390/jcm11226803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Covino M, De Matteis G, Della PDA et al (2021) Predictors of in-hospital mortality and death risk stratification among covid-19 patients aged ≥ 80 years old. Arch Gerontol Geriatr 95:104383. 10.1016/j.archger.2021.104383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vrillon A, Hourregue C, Azuar J et al (2020) COVID-19 in older adults: a series of 76 patients aged 85 years and older with COVID-19. J Am Geriatr Soc 68(12):2735–2743. 10.1111/jgs.16894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tzoulis P, Waung JA, Bagkeris E et al (2021) Dysnatremia is a predictor for morbidity and mortality in hospitalized patients with COVID-19. J Clin Endocrinol Metab 106(6):1637–1648. 10.1210/clinem/dgab107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shrestha AB, Sapkota UH, Shrestha S et al (2022) Association of hypernatremia with outcomes of COVID-19 patients: a systematic review and meta-analysis. Medicine 101(51):e32535. 10.1097/MD.0000000000032535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bahl A, Van Baalen MN, Ortiz L et al (2020) Early predictors of in-hospital mortality in patients with COVID-19 in a large American cohort. Intern Emerg Med 15(8):1485–1499. 10.1007/s11739-020-02509-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sisay G, Mantefardo B, Beyene A (2022) Time from symptom onset to severe COVID-19 and risk factors among patients in Southern Ethiopia: a survival analysis. J Int Med Res 50(8):030006052211193. 10.1177/03000605221119366 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.