Abstract
The aim of this study was to investigate the effect of using different core build-up materials on biaxial flexural strength (BFS) of multilayered strength-gradient zirconia ceramic in comparison to lithium disilicate ceramic. Thirty zirconia discs were fabricated from IPS e.max ZirCAD Prime (Zir), 30 discs from IPS e.max CAD (LS2), 30 composite discs were prepared from Tetric N-Ceram (TNC) and 30 from MultiCore Flow (MCF). The ceramic discs were adhesively cemented to composite discs forming 4 groups (n = 15) (Zir-MCF, Zir-TNC, LS2-MCF and LS2-TNC). BFS was determined using a piston-on-3-ball test. The data were statistically analyzed with independent t-tests for significant differences (p = 0.05). In zirconia groups, significantly higher stress values were recorded in the composite and the ceramic for Zir-TNC, compared to Zir-MCF (p < 0.001), while for LS2 groups, no significant differences were found between the 2 composites (p = 0.157) but stresses in LS2 were significantly higher for LS2-TNC than LS2-MCF (p < 0.001). Comparing the values between the ceramic groups, stresses were significantly higher for zirconia than LS2 (p < 0.001). It was concluded that the tested composite materials significantly differ in their strength, which also influenced the strength of the overlying ceramics, and that strength-gradient zirconia had higher strength than LS2. Monolithic strength-gradient zirconia restorations supported by composite core build-up materials with superior mechanical properties can be durable restorative options for high stress-bearing areas.
Keywords: Biaxial flexural strength, Strength-gradient zirconia, Lithium disilicate, Bulk-fill composite
Subject terms: Biophysics, Materials science
Introduction
Endodontically treated teeth face challenges in long-term survival, influenced by factors such as the chosen restorative approach1. Core build-up materials play a pivotal role in the restoration process, as they should provide sufficient strength to withstand stresses2. Traditionally, composite resins have been used for core build-up, offering satisfactory mechanical properties. More recently, resin-based materials tailored specifically for core build-up were introduced, providing enhanced mechanical properties and a variety of curing options such as dual-cured resin composites2,3. Bulk-fill composites can be applied in thick layers and polymerized in a single step, saving time while ensuring more compact void-free fillings2,4,5. Bulk-fill composites showed improved mechanical properties and enhanced clinical performance comparable to conventional composites6.
Full coverage indirect restorations are recommended for endodontically treated teeth with large structural loss7. For such restorations, all-ceramic restorative materials have gained popularity during the last few decades and can be categorized into glass ceramics, polycrystalline ceramics, and resin-matrix ceramics8,9. Lithium disilicate (LS2), classified as a glass-ceramic, was first introduced in 1998 as IPS Empress 2 that was used to produce ceramic cores via heat-pressing technique10–13. In 2005, IPS e.max Press was introduced exhibiting improved mechanical properties and optical features which allowed its use for monolithic restorations and later on became very popular with the advent of CAD-CAM technology9–14. When fully-crystallized, IPS e.max CAD contains 70% vol LS2 crystals, 1–3 μm in length and 0.1–0.4 μm in width, increasing the flexural strength and fracture toughness of the material10,15,16. IPS e.max CAD is suitable for both laboratory and chairside restorations and can be utilized for both tooth- and implant-supported restorations, from anterior veneers to posterior resin-bonded single restorations, like inlays, onlays, overlays, non-retentive partial crowns and full coverage table-tops9,10,14. Although LS2 monolithic crowns have been shown to have superior mechanical properties12,16, their limited strength raises concerns about their use in the posterior area, especially in patients with bruxism10,17. Furthermore, utilization of LS2 for fixed partial dentures (FPD) is a controversial topic as their survival rate was low, especially in the posterior locations10,13.
On the other hand, zirconia dental restorations have recently become a popular restorative alternative18,19. Pure zirconia displays 3 crystalline phases at different temperatures; monoclinic, tetragonal and cubic. Zirconia can be stabilized with different oxides thus retaining the zirconia crystals in their cubic or tetragonal phase at room temperature20–22. The change from the tetragonal phase to the monoclinic phase is accompanied by volume expansion hindering crack propagation in a mechanism called phase transformation toughening18–20,23.
The first generation of dental zirconia (3 Y-TZP) was the high-strength tetragonal crystalline phase, stabilized with 3 mol% yttria and enhanced with 0.25% alumina24. Although it has excellent fracture toughness and flexural strength, due to its opacity, it must be veneered with a compatible material and chipping of the veneering ceramic is a common clinical problem20,21,25. In the second generation of 3Y-TZP, the alumina content was decreased to 0.05wt%, providing a more translucent and yet a more susceptible material to low-temperature degradation23,26. Later on, the use of full-contour monolithic zirconia was emphasized25,27. When zirconia is doped with 5 mol% yttria (5Y-TZP), a partially stabilized zirconia with increased translucency is formed. However, this results in inferior mechanical properties19,23,24,28,29. Compared to LS2, 5Y-TZP has comparable or slightly superior flexural strength and fracture toughness20,21,26. More recently, another newer generation was produced (4Y-TZP) with 4 mol% yttria, offering a material with intermediate strength and improved translucency22,26,29.
Later on, the multilayered technology was introduced in 2015 which simulates the gradient color of natural teeth by using various color pigments obtaining restorations where the highest translucency is in the incisal region while the cervical area has increased opacity18–20,28–30. However, these ceramics did not solve the trade-off between strength and translucency of conventional zirconia as shade-gradient 3Y-TZP has high strength but low translucency, while shade-gradient 4Y-PSZ or 5Y-PSZ have high translucency but limited flexural strength31.
Therefore, an innovative generation of strength-gradient multilayered zirconia was introduced, with the yttria content increasing from cervical to incisal region mimicking the shade and strength gradient of natural teeth24–26,28,29,32,33. One such material is IPS e.max ZirCAD MT Multi which has 4Y- and 5Y-TZP in one blank29,32. More recently, IPS e. max ZirCAD Prime was introduced combining (5Y- and 3Y-TZP) and can be used for 14-unit restorations, with maximum 2 adjacent pontics18,32. Different strength-gradient zirconia blanks are currently available and more recently, a new gradient technology that combines 3 zirconia formulations in a single blank has been marketed19. Several studies evaluated the mechanical properties of strength gradient zirconia. Compared to color- gradient 4Y-TZP zirconia, porcelain-veneered bilayers and LS2, strength-gradient zirconia revealed superior mechanical properties, but when compared to 3Y-TZP, gradient strength zirconia had significantly lower fracture load values and relatively inhomogeneous optical and mechanical properties18,21,25,33. Furthermore, different composition and sintering shrinkage of the layers in both strength-gradient and color-gradient blanks might lead to internal stresses and thus impair the long-term reliability. Therefore, the indications for such materials should be carefully considered26.
Flexural strength is a reliable method to assess the durability of ceramic material34. While uniaxial tests are sensitive to flaws along the sample edges, in biaxial tests, maximum stress state is created near the center of the specimen and edge failures are usually eliminated, resulting in a more accurate estimate of strength35–37. Therefore, the biaxial flexural strength (BFS) test was recommended by the American Society for Testing and Materials as an international standard for evaluating dental ceramics35,38,39. Piston-on-three-ball test was selected as the test of choice for dental ceramic materials as it is not affected by the presence of frictional contact between the three supporting balls and the disc-shaped specimen and also it is less sensitive to undetectable surface flaws, hence it can accommodate for slightly warped specimens35,38.
A comprehensive understanding of the mechanics and failure behavior of these multilayered zirconia materials is still very limited28. Moreover, very few studies compared the strength gradient zirconia to LS2 or investigated the effect of core build-up materials on the overlying indirect restorations1,7,8,21. Therefore, the aim of the present study was to investigate the effect of using different composite core build-up materials on the stresses in the overlying strength-gradient zirconia and LS2 materials. The null hypotheses tested were:
Composite core material has no effect on the stresses in the overlying ceramic restorations.
Within the same ceramic groups, there is no statistically significant difference in the stresses between the 2 composite core build-up materials tested.
Regardless of the type of composite material underlying the ceramic, there is no statistically significant difference in the stresses between monolithic strength-gradient zirconia and LS2.
Materials and methods
Based on a power analysis which showed that for α = 0.05, power = 0.8, 60 disc-shaped ceramic specimens (10 mm diameter, 2 mm thickness) and 60-disc-shaped composite core specimens (10 mm diameter, 4 mm thickness) were fabricated. Thirty disc-shaped specimens were fabricated using strength-gradient zirconia material (IPS e.max ZirCAD Prime, Ivoclar Vivadent, Schaan, Liechtenstein), shade A2, and 30 specimens were fabricated using monolithic LS2 (IPS e.max CAD, Ivoclar Vivadent, Schaan, Liechtenstein). The materials used in this study are shown in Table 1. The zirconia specimens were designed using CAD software (3Shape Dental Software) and manufactured from partially sintered zirconia using a five-axis milling machine (Wieland Zenotec Select Hybrid, Ivoclar Vivadent AG, Schaan, Liechtenstein). The location of the cut was made through the middle layer of zirconia blocks. After milling, the samples were finished (Zolid Green-State Finishing Kit; Amann Girrbach AG) and sintered using a special furnace (Programat S1 1600, Ivoclar Vivadent AG, Schaan, Liechtenstein) at 1,500 °C for 4.5 h. The specimens were then finished (Zolid Sinter-State Finishing Kit; Amann Girrbach AG), sandblasted using 50 μm Al₂O₃-powder at 0.1 MPa pressure at constant distance of 10 mm for 15 s (Dentify sandblaster, Engen, Germany), followed by ultrasonic cleaning using isopropanol bath for 5 min and air-drying for 15 s7,21.
Table 1.
Materials used in this study.
| Brand | Material | Chemical composition | Manufacturer | ||
|---|---|---|---|---|---|
| IPS e.max ZirCAD Prime | Medium and high translucent zirconia (3Y-TZP and 5Y-TZP) | 88.0–95.5% Zirconium oxide (ZrO2), > 4.5% – ≤ 7.0% Yttrium oxide (Y2O3), ≤ 5.0% Hafnium oxide (HfO2), ≤ 1.0% Aluminium oxide (Al2O3), ≤ 1.5% Other oxides | Ivoclar Vivadent AG (Schaan, Liechtenstein) | ||
| IPS e.max CAD |
SiO2 57–80% Li2O 11–19% K2O 0–13% Other oxides 0–8% |
Ivoclar Vivadent AG (Schaan, Liechtenstein) | |||
| Tetric N-Ceram |
Nano-hybrid resin composite |
Urethane dimethacrylate, ethoxylated Bis-EMA, Bis-GMA (18.8 wt%), barium glass filler, ytterbium trifluoride, mixed oxide (63.5 wt%), polymer (17 wt%), additives, catalysts, stabilizers, and pigments (0.7 wt%) | (Ivoclar Vivadent, Schaan, Liechtenstein) | ||
| MultiCore Flow | Self-cured core build-up composite with light-cured option |
(Wt%) -Bis-GMA, urethane dimethacrylate, triethyleneglycol dimethacrylate highly dispersed silicon dioxide. -Barium glass fillers, Ba-Al-fluorosilicate glass, highly dispersed silicone dioxide -Ytterbium trifluoride -Catalysts, stabilizers, pigments |
Base 28.1 54.9 16.4 0.6 |
Catalyst 28.4 54.4 16.2 1.0 |
(Ivoclar Vivadent, Schaan, Liechtenstein) |
| Multilink Automix resin cement | two paste, self- curing adhesive resin cement | DMA and HEMA, adhesive monomer, barium glass filler, SiO2 filler, Ytterbium triflorite, accelarator and stabilisator and pigments | (Ivoclar Vivadent, Schaan, Liechtenstein) | ||
| Monobond N | Universal Primer | Contains 3 different functional methacrylates: Silane methacrylate, phosphoric methacrylate and sulfide methacrylate. | (Ivoclar Vivadent, Schaan, Liechtenstein) |
LS2 specimens were designed and fabricated from IPS e.max CAD blocks using the same equipment used for zirconia specimens. After milling the samples in the blue stage, they were crystallized and glazed at 840◦C for 20 min following manufacturers’ instructions. The specimens were then finished, cleaned in isopropanol ultrasonic bath for 5 min and air-dried for 15 s21. The discs were then Etched using 5% hydrofluoric acid for 20s, thoroughly rinsed with water spray and dried with oil-free air.
For the composite cores, 30 disc-shaped specimens were prepared of each composite material using a customized resin mold (Asiga DentaGUM, Sydney, Australia) that was designed with specific dimensions using CAD software (3shape Dental Software) and printed using 3D printer (Asiga 3D Printer, Sydney, Australia). For the first group, Tetric N-Ceram (TNC) (Ivoclar Vivadent, Schaan, Liechtenstein), shade IVA, was applied into the resin mold in 2 increments (2 mm each) to a total thickness of 4 mm. Each increment was carefully condensed with ST instrument with a plastic working end (OptraSculpt, Ivoclar Vivadent, Schaan, Liechtenstein). For the second group, MultiCore Flow (MCF) (Ivoclar Vivadent, Schaan, Liechtenstein), shade Medium, was injected into the resin mold in a single bulk until completely filled using the automatic mixing tips7. A mylar strip and glass slide were placed on top of the mold to remove any excess material and achieve a uniform surface finish. The materials were photo-polymerized for 40 s using a light cure unit (Bluephase, Ivoclar Vivadent AG, Schaan, Liechtenstein) placed perpendicular on top of the glass plate with an intensity of 1100 mW/cm2 and a constant distance of 2 mm. The specimens were then removed from the mold, and excess composite was removed using fine polishing discs (Sof-Lex, 3 M ESPE, St Paul, MN, USA)40,41.
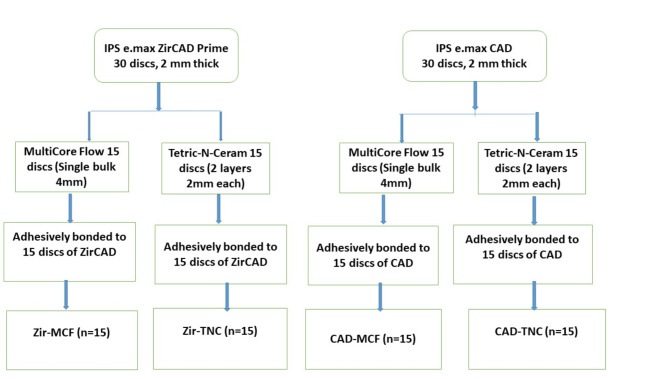
Consequently, a thin coat of Monobond N ( Ivoclar Vivadent, Schaan, Liechtenstein ) was applied with a minibrush (Ivoclar Vivadent) to the pre-treated surfaces of both materials. The material was allowed react for 60 s, the remaining excess was dispersed with a strong stream of air. Finally, self-etching, dual-cure Multilink Automix resin-cement (Ivoclar Vivadent, Schaan, Liechtenstein) was applied using automatic mixing tips to the intaglio surfaces of the ceramic specimens to which composite samples were bonded in a special device under a constant load of 750 g7. Excess cement was then removed using a disposable minibrush. The luting material was then cured at a distance of 5 mm for 20 s from each side and oxygen protection gel (Air-Block Liquid Strip, Ivoclar Vivadent) was applied to the margins for 5 min to ensure total self-curing of the cement. Specimens were stored in distilled water at 37 °C for 24 h. The ceramic discs were hence subdivided into 2 groups each (n = 15), according to the type of composite they were cemented to. Therefore, 4 groups were compared in this study; IPS e.max ZirCAD Prime/ Tetric N-Ceram (Zir-TNC), IPS e.max ZirCAD Prime/ MultiCore Flow(Zir-MCF), IPS e.max CAD/ Tetric N-Ceram (LS2-TNC) and IPS e.max CAD/MultiCore Flow (LS2-MCF). Figure 1 is a flow chart clarifying the fabrication of the 4 different groups.
Fig. 1.
Flow chart for the fabrication of the 4 groups tested.
Specimens were subjected to the BFS test using the universal testing machine (WDW-20; Jinan Testing Equipment IE Corporation, Jinan, China) according to ISO 6872:2008 for dental ceramics42,43. The specimens were placed so that load was applied at the ceramic surface while the core surface of the specimen was at the bottom, mimicking the clinical situation. For the piston-on-three-ball test, the sample holder was made of 3 hardened steel balls with a diameter of 3.2 mm each. The steel balls were positioned at 120° apart forming an equilateral triangle on a support circle with a diameter of 10 mm. The center of the specimens was placed upon the steel balls and the center of the equilateral triangle was aligned coaxially. The load was applied centrally through a flat piston, with a diameter of 1.4 mm, at a crosshead speed of 1 mm/min until failure42,43. The load at fracture (P) was recorded, in Newton (N), when a dramatic drop in the applied load occurred, which was associated with acoustic sound.
Stress values in the ceramic and composite layers were calculated using the following formulas39:
 |
 |
where  is the maximum tensile stress in the composite core layer;
is the maximum tensile stress in the composite core layer;  is the maximum tensile stress in the zirconia layer; P is the load at fracture; a is the radius of the supporting cycle; c is the radius of the piston; R is the radius of the disc; z is the interface between the layers in vertical cylindrical coordinate; t1 is the thickness of the composite core layer; t2 is the thickness of the ceramic layer; v1 is the Poisson ratio of composite core material; v2 is the Poisson ratio of ceramic material; z* is the neutral surface position; D* is the flexural rigidity; and v is the average Poisson ratio of the bilayer.
is the maximum tensile stress in the zirconia layer; P is the load at fracture; a is the radius of the supporting cycle; c is the radius of the piston; R is the radius of the disc; z is the interface between the layers in vertical cylindrical coordinate; t1 is the thickness of the composite core layer; t2 is the thickness of the ceramic layer; v1 is the Poisson ratio of composite core material; v2 is the Poisson ratio of ceramic material; z* is the neutral surface position; D* is the flexural rigidity; and v is the average Poisson ratio of the bilayer.
 |
 |
where E1 is the elastic modulus of the composite core layer and E2 is the elastic modulus of the ceramic layer. Elastic moduli and Poisson ratios of the tested materials, provided by the manufacturers, were (210,0.3) for Zir, (95,0.25) for LS2, (10.8,0.24) for TNC, and (7.5,0.28) for MCF. For this study, a = 5 mm, c = 0.7 mm, R = 5 mm, t1 = 4 mm, t2 = 2 mm, z1 = 0, z2 = 2 mm
 |
Additionally, stresses at composite and zirconia interfaces,  and
and  , respectively, were calculated according to the following equations:
, respectively, were calculated according to the following equations:
 |
 |
Analytical data calculations were carried out using the SPSS version 26.0 (SPSS, Chicago, IL, USA) statistical program. The results were statistically analyzed using the independent t-tests. All data were subjected to Levene’s test of homogeneity of variance (α < 0.05) following the assumption of equal variance. p-value of less than 0.05 (2-tailed) was considered statistically significant. σ1, σ2, σ1stress and σ2stress for the 4 groups were calculated, analyzed, and compared for any statistically significant differences. In order to simplify the analyses of the data, all stress values were treated as strength values.
Results
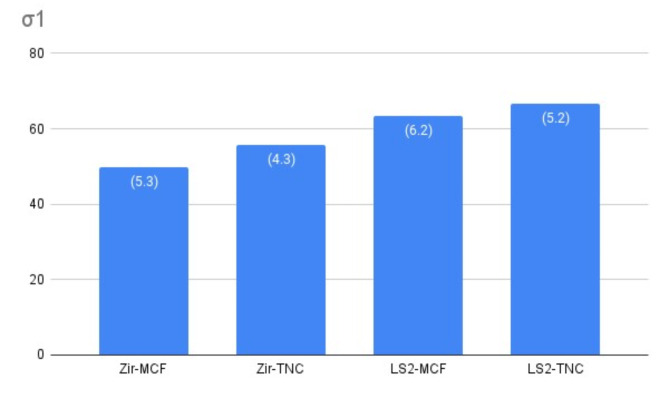
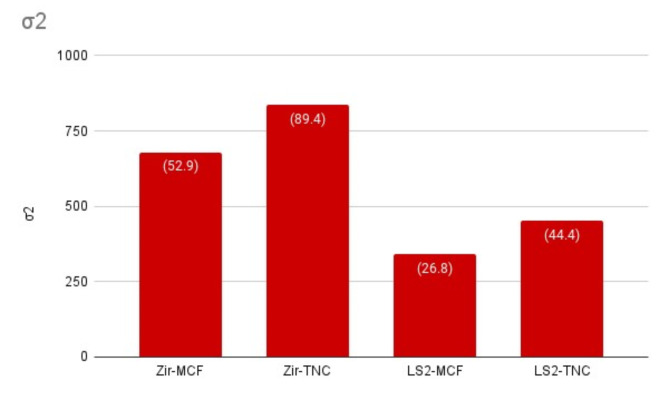
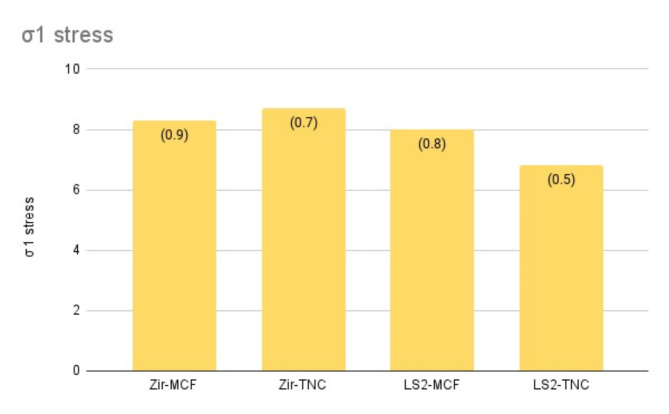
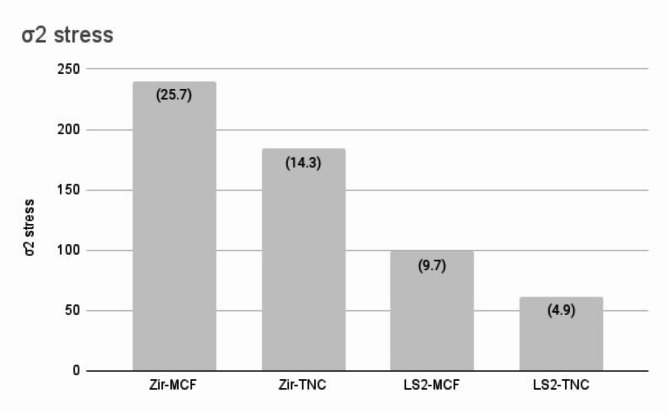
The Kolmogorov-Smirnov test revealed no deviation from the normal distribution and data were analyzed parametrically. Table 2 shows the results of independent t-test, comparing the stresses at different layers between MCF and TNC in Zirconia groups and LS2 groups, separately. In Zirconia groups, significantly higher values were recorded for both the composite core (σ1) and the overlying ceramic (σ2) for Zir-TNC, compared to Zir-MCF, while σ2stress was significantly higher for Zir-MCF and σ1stress was similar in both groups. For LS2 groups, no significant differences were found in σ1 between the 2 composites, while σ2 was significantly higher for LS2-TNC and σ1stress and σ2stress were lower for LS2-TNC.
Table 2.
The means, in MPa, and standard deviations (SD) of BFS and the p values of the independent t-tests comparing Zir-MCF with Zir-TNC, and LS2-MCF with LS2-TNC.
| Zir-MCF | Zir- TNC | p value | LS2-MCF | LS2-TNC | p value | |
|---|---|---|---|---|---|---|
| σ1 | 49.7 (5.3) | 55.8 (4.3) | 0.002 | 63.4 (6.2) | 66.6 (5.2) | 0.157 |
| σ2 | 679.5 (52.9) | 835.8 (89.4) | 0.000 | 340.5 (26.8) | 453.2 (44.4) | 0.000 |
| σ1 stress | 8.3 (0.9) | 8.7 (0.7) | 0.18 | 8.0 (0.8) | 6.8 (0.5) | 0.000 |
| σ2 stress | 240.1(25.7) | 184.5 (14.3) | 0.000 | 99.0 (9.7) | 61.8 (4.9) | 0.000 |
σ1 is stress in composite core materials, σ2 is the stress in the ceramic materials, σ1stress is the interfacial stress values at the composite layers and σ2stress is the interfacial stress at the ceramic layers.
Comparing the values between the ceramic groups in Table 3, σ2 was significantly higher for zirconia than LS2, regardless of the type of core material used, as well as σ2 stress, and σ1stress which was higher for zirconia, but only significant in TNC groups. σ1 was significantly higher for LS2 groups than Zirconia groups regardless of the type of core used. Values of σ2stress were significantly higher for Zirconia than LS2 with both core materials.
Table 3.
The means, in MPa, and standard deviations (SD) of BFS and the p values of the independent t-tests comparing Zir-MCF with LS2-MCF, and Zir-TNC with LS2-TNC.
| Zir-MCF | LS2-MCF | p value | Zir-TNC | LS2-TNC | p value | |
|---|---|---|---|---|---|---|
| σ1 | 49.7 (5.3) | 63.4 (6.2) | 0.000 | 55.8 (4.3) | 66.6 (5.2) | 0.000 |
| σ2 | 679.5 (52.9) | 340.5 (26.8) | 0.000 | 835.8 (89.4) | 453.2 (44.4) | 0.000 |
| σ1 stress | 8.3 (0.9) | 8.0 (0.8) | 0.344 | 8.7 (0.7) | 6.8 (0.5) | 0.000 |
| σ2 stress | 240.1(25.7) | 99.0 (9.7) | 0.000 | 184.5 (14.3) | 61.8(4.9) | 0.000 |
These results are summarized in Figs. 2, 3, 4 and 5.
Fig. 2.
Histogram showing the differences in σ1 between the 4 tested groups.
Fig. 3.
Histogram showing the differences in σ2 between the 4 tested groups.
Fig. 4.
Histogram showing the differences in σ1stress between the 4 tested groups.
Fig. 5.
Histogram showing the differences in σ2stress between the 4 tested groups.
Discussion
This study investigated the stresses of 2 composite core materials (TNC and MCF) and their influence on the stresses of strength-gradient Zirconia and LS2 ceramics. The results showed significant effect of the composite core materials on the stresses in both ceramics, hence the first null hypothesis stating that composite core material has no effect on the stresses in the overlying ceramic restorations, was rejected. TNC had significantly higher stresses than MCF in Zirconia groups but the difference was insignificant in LS2 groups, and therefore the second null hypothesis, that stated that there is no statistically significant difference in the stresses between the 2 composite core build-up materials tested within the same ceramic groups, was partially accepted. Moreover, the results showed significant differences between the 2 ceramics, therefore the third null hypothesis, that indicated that there is no statistically significant difference in the stresses between monolithic strength-gradient zirconia and LS2, was rejected.
The comparison of σ2 in Table 2; Fig. 3 showed that ceramics cemented to TNC had higher σ2 than those cemented to MCF, in both ceramics, indicating that variation in the modulus of elasticity and curing method of the core materials might affect the strength of the overlying ceramic restorations. This disagrees with the findings previously reported by Azer et al. in 2001, while it agrees with results found by Abdelaziz et al.1,8. The results of our study are also in disagreement with Musa and Ereifej 2023, who found that the composite core materials, which were similar to the ones used in our study, had no effect on the overlying ceramic restorations, however, LS2 was not used in their study7. The use of rigid ceramic restoration makes the ceramic restoration more prone to flexural damage. Hence, a stronger core restoration, as TNC, might be a preferable choice for clinicians to use, to provide better support for the ceramic restoration16.
The core build‑up materials investigated in our study were selected as they are commonly used for direct restorations in practice, with variable polymerization processes, resin formulas and filler characteristics1. Figure 2; Table 2 show that σ1 of TNC was always higher than MCF, although the difference was insignificant in LS2 groups. This difference can be explained by variations in the chemical composition, type of resin, type of inorganic filler, and size and content of filler particles7,44. As the volume and weight of the filler increase, the strength of the composite materials was reported to increase, which might explain the results of our study, as TNC has a higher filler volume (63.5% vol) compared to MCF (54.4% vol)2,45. Furthermore, higher filler content enhances the modulus of elasticity resulting ultimately in higher strength which can be confirmed in our study, as the elastic modulus of TNC is 10.8, while it is 7 for MCF41. Additionally, other factors might contribute to the overall strength of composite material including the resin matrices, different types of fillers, or filler size and distribution40,46. Therefore, the presence of nano-sized filler particles along with high molecular weight monomers in the composition of the TNC might contribute to its higher σ1values2,44.
IPS e.max ZirCAD Prime blanks consist of a 9-mm-thick high strength (> 1200 MPa) 3Y-TZP dentin layer at the bottom side of the blank, a 4-mm-thick 4Y-TZP transition layer, and a 3-mm-thick reduced strength (< 650 MPa) 5Y-TZP incisal layer at the top of the blank for improved translucency20,31–33. Zirconia samples in our study were milled from the middle layer of zirconia blanks, as done in a previous study, since inclusion of all layers in the block was not possible in this test set up, and as the middle layer of IPS e.max ZirCAD Prime was reported to have higher fracture load than those taken from the uppermost layer7,32,33. This might indicate that the composition of the ceramic sample used here was mainly 4Y-TZP, which has strength that is intermediate between 3Y-TZP and 5Y-TZP. The values obtained in our study confirm this and were similar to values obtained previously for this material7. σ2 values, as shown in Fig. 3; Table 3, were always significantly lower for LS2 than Zirconia, which is in agreement with Michailova et al. 2020 who reported that LS2 showed lower fracture load than strength gradient-zirconia and 4Y-TZP21. In partially stabilized zirconia, the tetragonal phase provides a strengthening effect due to the transformation toughening. In strength-gradient zirconia, as yttria content decreases in transitional and body layers compared to enamel layers, tetragonal phase of zirconia increases, increasing the effect of transformation toughening, decreasing grain size of zirconia crystals, and enhancing the strength of the material31. In 4Y-TZP, there is still predominantly more tetragonal (68–82%) than cubic phase which explains the high σ2 values for 4Y-TZP zirconia in our study21,31. On the other hand, LS2 was reported to have an effective crack deflection and crack bridging mechanism, due to the relative large and elongated LS2 crystals, improving its mechanical properties. When comparing LS2 to zirconia, 4Y-TZP and 3Y-TZP showed better mechanical properties, and 5Y-TZP revealed only a marginally higher fracture toughness and flexural strength15–17,24. According to ISO6872:2015, our results showed that zirconia had sufficiently high σ2 values allowing its use for the construction of anterior and posterior three-unit FPDs including molar restorations, while LS2 cannot be used for 3-unit FPDs and it is mostly suited for single crown restorations, whether tooth supported or implant supported14,23,26,47.
Nevertheless, the load bearing property of the ceramic restoration is governed by the elastic modulus mismatch between the ceramic restoration and cement/dentin foundation. As the elastic modulus of zirconia (210GPa) is almost double that of LS2 (95GPa), this makes LS2 much more compatible with the dentin-like substrate which has an elastic modulus of 18.6 GPa16. Furthermore, when bonded to and supported by dentin, the load-bearing capacity of LS2 was reported comparable to that of 4Y-PSZ and much higher than 5Y-PSZ suggesting that LS2 might have great potential for durable restorations16. Therefore, although LS2 had inferior σ2 values in our study, after adhesive cementation to teeth, the load bearing capacity and hence survival of the 2 materials might be comparable26. This can be further evaluated by future clinical studies.
When the bilayered specimen is composed of 2 distinct layers with different moduli of elasticity, large stresses usually emerge including the compressive force zone at the top layer and the tensile force zone at the bottom layer, in addition to interfacial stresses that arise due to the modulus mismatch between the 2 cemented layers3,42,48. Therefore, the present study assessed the interfacial stresses as illustrated in Tables 2 and 3 as well as Figs. 4 and 5. For all groups, the stresses that occurred at the interfaces of the ceramic layers were higher than those that occurred in the composite layers and at the interfaces of the composite layer. This can be explained by the higher elastic modulus mismatch at the ceramic interfaces than composite interfaces. Figure 5 shows that σ2stress was significantly higher in zirconia groups than LS2 groups which can also be explained by the higher elastic modulus mismatch between zirconia and cement layer, compared to LS2. In addition to that, due to the different chemical composition and the lower modulus of elasticity of MCF compared to the TNC, this might have resulted in differences in σ1stress between the 2 tested composites, as shown in Fig. 4, as well as differences in σ2stress among the groups with different composite core materials, as shown in Fig. 57,42,48.
One of limitations of our study was the absence of tooth substrate. However, previous studies reported the reliability of piston-on-three-ball test for studying the BFS of dental ceramics36. Furthermore, the complexity of the forces exerted during the masticatory function and the particularities of the intra-oral environment were not represented in this in vitro study12. Therefore, our results must be evaluated with caution and future studies evaluating the clinical performance and survival of these materials are recommended. Moreover, composition and mechanical properties of these materials are different among different manufacturers. Consequently, the results for one manufacturer’s material cannot be directly applied to other materials20,24. Future studies should focus on comparison between the materials produced by different manufacturers.
Conclusions
Within the limitations of this study, the following conclusions can be withdrawn:
The type of core build-up material affects the stresses in the overlying ceramic restorations.
Tetric N-Ceram composite has superior strength compared to MultiCore Flow material.
IPS e.max ZirCAD Prime has superior strength compared to IPS e.max CAD.
Author contributions
N. E and D.M designed the experiment. N.E, D.M, Y.O performed the study. M.A and A.T collected the data. M.A and A.T analyzed the data. N.E, Y.O and M.A wrote and reviewed the manuscript. All authors revised the manuscript.
Data availability
The numerical data generated in this work are available from the corresponding author upon reasonable request at the e.mail address nadia_ereifej116@hotmail.com.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Abdelaziz, K. M., Keshk, C. K., Alshadidi, A., Mafraq, S. & Murchison, D. F. Fracture resistance of ceramic crowns supported with indirect chair-side composite cores. J. Int. Soc. Prev. Community Dent.8, 34–40 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warangkulkasemkit, S. & Pumpaluk, P. Comparison of physical properties of three commercial composite core buildup materials. Dent. Mater.38, 177–181 (2019). [DOI] [PubMed] [Google Scholar]
- 3.Rüttermann, S., Alberts, I., Raab, W. H. M. & Janda, R. R. Physical properties of self-, dual-, and light-cured direct core materials. Clin. Oral Investig. 15, 597–603 (2011). [DOI] [PubMed] [Google Scholar]
- 4.Benalca´zar Jalkh, E. B. et al. Effect of thermocycling on biaxial flexural strength of CAD / CAM, bulk fill, and conventional resin composite materials. Oper. Dent.44, 254–262 (2019). [DOI] [PubMed] [Google Scholar]
- 5.Chesterman, J., Jowett, A., Gallacher, A. & Nixon, P. Bulk-fill resin-based composite restorative materials: A review. Br. Dent. J.222, 337–344 (2017). [DOI] [PubMed] [Google Scholar]
- 6.de Almeida Durão, M., de Andrade, A. K. M., da Silva Santos, M. C. M., Montes, M. A. J. R. & de Melo Monteiro, G. Q. Clinical performance of bulk-fill resin composite restorations using the United States Public Health Service and Federation Dentaire Internationale Criteria: A 12-month randomized clinical trial. Eur. J. Dent.15, 179–192 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Musa, D. B. & Ereifej, N. S. The influence of core – build up materials on biaxial flexural strength of monolithic strength – gradient zirconia; an in – vitro study. BMC Oral Health. 23, 873 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Azer, S. S., Drummond, J. L., Campbell, S. D. & El Moneim Zaki, A. Influence of core buildup material on the fatigue strength of an all-ceramic crown. J. Prosthet. Dent.86, 624–631 (2001). [DOI] [PubMed] [Google Scholar]
- 9.Chen, Y., Yeung, A. W. K., Pow, E. H. N. & Tsoi, J. K. H. Current status and research trends of lithium disilicate in dentistry: A bibliometric analysis. J. Prosthet. Dent.126, 512–522 (2021). [DOI] [PubMed] [Google Scholar]
- 10.Zarone, F., Di Mauro, M. I., Ausiello, P., Ruggiero, G. & Sorrentino, R. Current status on lithium disilicate and zirconia: A narrative review. BMC Oral Health. 19, 134 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schestatsky, R. et al. CAD-CAM milled versus pressed lithium-disilicate monolithic crowns adhesively cemented after distinct surface treatments: Fatigue performance and ceramic surface characteristics. J. Mech. Behav. Biomed. Mater.94, 144–154 (2019). [DOI] [PubMed] [Google Scholar]
- 12.Schestatsky, R. et al. Microstructure, topography, surface roughness, fractal dimension, internal and marginal adaptation of pressed and milled lithium-disilicate monolithic restorations. J. Prosthodont. Res. (2020). 64,12 – 9. [DOI] [PubMed] [Google Scholar]
- 13.Abdulrahman, S., Mahm, C. V. S., Talabani, R. & Abdulateef, D. Evaluation of the clinical success of four different types of lithium disilicate ceramic restorations: A retrospective study. BMC Oral Health. 21, 625 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Angelis, P. et al. Monolithic CAD-CAM lithium disilicate versus monolithic CAD-CAM zirconia for single implant-supported posterior crowns using a digital work flow: A 3-year cross-sectional retrospective study. J. Prosthet. Dent.123, 252–256 (2020). [DOI] [PubMed] [Google Scholar]
- 15.Zhang, F., Reveron, H., Spies, B. C., Van Meerbeek, B. & Chevalier, J. Trade-off between fracture resistance and translucency of zirconia and lithium-disilicate glass ceramics for monolithic restorations. Acta Biomater.91, 24–34 (2019). [DOI] [PubMed] [Google Scholar]
- 16.Yan, J., Kaizer, M. R. & Zhang, Y. Load-bearing capacity of lithium disilicate and ultra-translucent zirconias. J. Mech. Behav. Biomed. Mater.88, 170–175 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hamza, T. A. & Sherif, R. M. Fracture resistance of monolithic Glass-ceramics versus Bilayered Zirconia-based restorations. J. Prosthodont.28, e259–264 (2019). [DOI] [PubMed] [Google Scholar]
- 18.Attia, M. A. & Shokry, T. E. Effect of dynamic loading on fracture resistance of gradient zirconia fi xed partial denture frameworks. J. Prosthet. Dent.130, 242–249 (2023). [DOI] [PubMed] [Google Scholar]
- 19.Attia, M. A. et al. Effect of different sintering protocols on the fracture strength of 3-unit monolithic gradient zirconia fixed partial dentures: An in vitro study. J. Prosthet. Dent.130, 908 (2023). [DOI] [PubMed] [Google Scholar]
- 20.Winter, A., Schurig, A., Odenthal, A. L. & Schmitter, M. Impact of different layers within a blank on mechanical properties of multi-layered zirconia ceramics before and after thermal aging. Dent. Mater.38, e147–154 (2022). [DOI] [PubMed] [Google Scholar]
- 21.Michailova, M. et al. Comparison between novel strength-gradient and color-gradient multilayered zirconia using conventional and high-speed sintering. J. Mech. Behav. Biomed. Mater.111, 103977 (2020). [DOI] [PubMed] [Google Scholar]
- 22.Dimitriadis, K., Constantinou, M., Moschovas, D., Constantinides, G. & Agathopoulos, S. Microstructural features, physic ο -mechanical properties, and wear behavior of dental translucent polychromic multilayer zirconia of hybrid composition prepared by milling technology. J. Esthet Restor. Dent.35, 1121–1130 (2023). [DOI] [PubMed] [Google Scholar]
- 23.Kwon, S. J., Lawson, N. C., Mclaren, E. E., Nejat, A. H. & Burgess, J. O. Comparison of the mechanical properties of translucent zirconia and lithium disilicate. J. Prosthet. Dent.120, 132–137 (2018). [DOI] [PubMed] [Google Scholar]
- 24.Strasser, T., Wertz, M., Koenig, A., Koetzsch, T. & Rosentritt, M. Microstructure, composition, and flexural strength of different layers within zirconia materials with strength gradient. Dent. Mater.39, 463–468 (2023). [DOI] [PubMed] [Google Scholar]
- 25.Marini, G. et al. Fatigue performance analysis of strength-graded zirconia polycrystals for monolithic three-unit implant-supported prostheses. J. Mech. Behav. Biomed. Mater.140, 105736 (2023). [DOI] [PubMed] [Google Scholar]
- 26.Pöppel, M. L. et al. Fracture load and fracture patterns of monolithic three-unit anterior fixed dental prostheses after in vitro artificial aging — a comparison between color-gradient and strength-gradient multilayer zirconia materials with varying yttria content. J. Clin. Med.11, 4982 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miura, S. et al. Effect of low-temperature degradation and sintering protocols on the color of monolithic zirconia crowns with different yttria contents. Dent. Mater. J.43, 164–171 (2024). [DOI] [PubMed] [Google Scholar]
- 28.Li, Q. et al. Effect of low-temperature degradation on the fatigue performance of dental strength-gradient multilayered zirconia restorations. J. Dent.142, 104866 (2024). [DOI] [PubMed] [Google Scholar]
- 29.Machry, R. V. et al. Mechanical characterization of a multi-layered zirconia: Flexural strength, hardness, and fracture toughness of the different layers. J. Mech. Behav. Biomed. Mater.135,105455 (2022). [DOI] [PubMed] [Google Scholar]
- 30.Hoffmann, M., Mayinger, F. & Stawarczyk, B. Influence of different surface finishing procedures of strength-gradient multilayered zirconia crowns on two-body wear and fracture load: Lithium silicate or leucite glazing versus polishing ? J. Mech. Behav. Biomed. Mater.150, 106307 (2024). [DOI] [PubMed] [Google Scholar]
- 31.Inokoshi, M. et al. Layer characteristics in strength-gradient multilayered yttria-stabilized zirconia. Dent. Mater.39, 430–441 (2023). [DOI] [PubMed] [Google Scholar]
- 32.Schönhoff, L. M., Lümkemann, N., Buser, R., Hampe, R. & Stawarczyk, B. Fatigue resistance of monolithic strength-gradient zirconia materials. J. Mech. Behav. Biomed. Mater.119, 104504 (2021). [DOI] [PubMed] [Google Scholar]
- 33.Rosentritt, M., Preis, V., Schmid, A. & Strasser, T. Multilayer zirconia: influence of positioning within blank and sintering conditions on the in vitro performance of 3-unit fixed partial dentures. J. Prosthet. Dent.127, 141–145 (2022). [DOI] [PubMed] [Google Scholar]
- 34.Juntavee, N. & Attashu, S. Effect of different sintering process on flexural strength of translucency monolithic zirconia. J. Clin. Exp. Dent..10, e821–e830 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang, C. W. & Hsueh, C. H. Piston-on-three-ball versus piston-on-ring in evaluating the biaxial strength of dental ceramics. Dent. Mater.27, e117–e123 (2011). [DOI] [PubMed] [Google Scholar]
- 36.Dikicier, S., Ayyildiz, S., Ozen, J. & Sipahi, C. Influence of core thickness and artificial aging on the biaxial flexural strength of different all-ceramic materials: an in-vitro study. Dent. Mater. J.36, 296–302 (2017). [DOI] [PubMed] [Google Scholar]
- 37.Fabris, D. et al. The bending stress distribution in bilayered and graded zirconia-based dental ceramics. Ceram. Int.42, 11025–11031 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hsueh, C. H. & Kelly, J. R. Simple solutions of multilayered discs subjected to biaxial moment loading. Dent. Mater.25, 506–513 (2009). [DOI] [PubMed] [Google Scholar]
- 39.Hsueh, C. H., Luttrell, C. R. & Becher, P. F. Analyses of multilayered dental ceramics subjected to biaxial flexure tests. Dent. Mater.22, 460–469 (2006). [DOI] [PubMed] [Google Scholar]
- 40.Hiriotappa, W. et al. Comparison of flexural strength between five commercial bulk-fill resin composites. TMJ20, 156–164 (2020). [Google Scholar]
- 41.Eweis, A. H., Yap, A. U. & Yahya, N. A. Comparison of flexural properties of bulk-fill restorative/flowable composites and their conventional counterparts. Oper. Dent.45, 41–51 (2020). [DOI] [PubMed] [Google Scholar]
- 42.Sawada, T. et al. Biaxial flexural strength of the bilayered disk composed of ceria-stabilized zirconia/alumina nanocomposite (Ce-TZP/A) and veneering porcelain. Dent. Mater.34, 1199–11210 (2018). [DOI] [PubMed] [Google Scholar]
- 43.International Organization for Standardization ISO 6872:2008. Dentistry Ceramic Materials (International Organization for Standardiization, Geneva, 2008).
- 44.Alrahlah, A. Diametral tensile strength, flexural strength, and surface microhardness of bioactive bulk fill restorative. J. Contemp. Dent. Pract..19, 13–19 (2018). [DOI] [PubMed] [Google Scholar]
- 45.Didem, A., Gözde, Y. & Nurhan, Ö. Comparative mechanical properties of bulk-fill resins. Open. J. Compos. Mater..4, 117–121 (2014). [Google Scholar]
- 46.Atalay, C. et al. Fracture resistance of endodontically treated teeth restored with bulk fill, bulk fill flowable, fiber-reinforced, and conventional resin composite. Oper. Dent.41, e131–e140 (2016). [DOI] [PubMed] [Google Scholar]
- 47.Carrabba, M. et al. Translucent zirconia in the ceramic scenario for monolithic restorations: A flexural strength and translucency comparison test. J. Dent.60, 70–76 (2017). [DOI] [PubMed] [Google Scholar]
- 48.Güngör, M. B., Yilmaz, H., Nemli, S. K., Bal, B. T. & Aydin, C. Effect of surface treatments on the biaxial flexural strength, phase transformation, and surface roughness of bilayered porcelain/zirconia dental ceramics. J. Prosthet. Dent.113, 585–595 (2015). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The numerical data generated in this work are available from the corresponding author upon reasonable request at the e.mail address nadia_ereifej116@hotmail.com.