Abstract
Introduction and importance
Low-grade appendicular mucinous neoplasms are rare. In contrast to other malignant tumors, they lack the ability for infiltrative growth or lymph node metastasis, but intraperitoneal mucin spread may lead to a life-threatening condition, known as a pseudomyxoma peritonei.
Case presentation
Patient, a 47-year-old female, with complaints of a palpable mass in her right inguinal area, presented to our clinic. After a clinical workup, which included computer tomography, magnetic resonance imaging, and colonoscopy, a preliminary diagnosis of LAMN was established. Laparoscopic cecal pole resection was performed. A pathological examination confirmed the diagnosis of LAMN. Patient was followed up for six months after the surgery, at which point a contrast-enhanced CT scan was obtained with no pathological findings.
Clinical discussion
Mucinous neoplasms of the appendix are a group of tumors in which mucin accumulates within the lumen of the appendix and while this type of neoplasia cannot spread hematologically, extramural mucin may lead to pseudomyxoma peritonei. Not long ago, a right hemicolectomy was accepted as a radical treatment method. Nowadays various studies have shown that laparoscopic appendectomy may be a safe option in patients with mucin, confined to the lumen of the appendix. This case holds educational value due to the detailed course of the disease presented and justified clinical decisions.
Conclusion
LAMN is a rare type of neoplasm. When confined to the lumen of the appendix, it lacks the ability for infiltrative growth and lymph node metastasis. Appropriate treatment in case of a contained disease is surgical removal.
Keywords: Laparoscopy, Case report, Appendicular neoplasm, LAMN, AMN, Pseudomyxoma peritonei
Highlights
-
•
This manuscript describes a case of LAMN confined to the lumen of the appendix.
-
•
Laparoscopic cecal pole resection was performed.
-
•
Data on LAMN pathological exams from our institution was reviewed.
1. Introduction
Mucinous neoplasms with low-grade epithelial dysplasia (LAMN) are rare appendiceal neoplasia with an incidence rate of 0.7–1.7 % [1]. Appendicular mucinous neoplasms are different from the rest of malignant tumors. While confined to the appendix they lack the ability of infiltrative growth or lymph node metastasis [2]. LAMN may be suspected during clinical investigation, and the pathological examination of the resected specimen is the only way to confirm the diagnosis [3]. The accepted extent and technique of resection for the surgery to be deemed radical in cases of Mucinous neoplasms of the appendix has seen changes in the last decades, from being a counterindication for a laparoscopic appendectomy [4] to laparoscopic single-incision resections being accepted as a standard of care in some institutions [5]. In our case, we present a female patient with a confined LAMN, managed by a laparoscopic cecal pole resection.
This case was presented following the updated consensus Surgical Case Report (SCARE) guidelines [6].
2. Case presentation
A female patient, 47 years of age was referred to our clinic by her family physician. She had complaints of discomfort and a palpable mass in her right inguinal area. Her medical history includes a cesarian section 15 years ago. She is a non-smoker, doesn't take any drugs, and has no chronic diseases. A contrast-enhanced CT scan of the thorax, abdomen, and pelvis was made: a homogenous mass with some calcifications extending from behind the cecum to a subhepatic space (Fig. 1). No other pathology or lymphadenopathy was observed.
Fig. 1.

CT: neoplasia in the projection of the appendix.
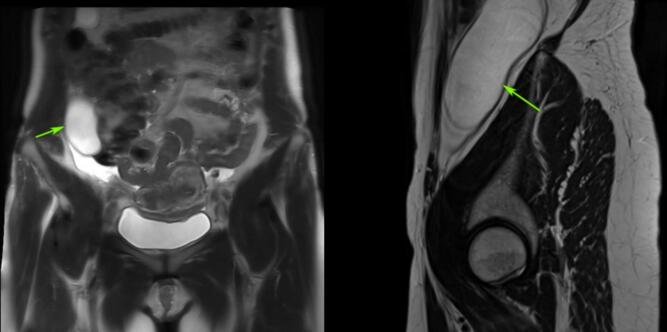
A diagnosis of appendicular mucinous neoplasm was suspected. The patient underwent additional clinical and instrumental examination: on MRI of the abdominal cavity – in the right iliac region, between the lower edge of the liver, behind the ascending colon, spreading inside the pelvis, a thin-walled cystic formation of an elongated shape with total conventional dimensions of ~4.6 × 4.5 × 11.0 cm. is visualized. A hyperintense MR signal on T2WI and a reduced signal on T1WI are noted. Invasion of adjacent structures by the indicated formation at the scanning level is not visualized (Fig. 2).
Fig. 2.
MRI: neoplasia situated between the liver, ascending colon, and the right kidney.
During colonoscopy, a deformation of the ileocecal valve due to an external compression is observed, swelling and infiltration of tissues at the mouth of the appendix is noted.
The patient's blood tests, including tumor markers, were within the reference range. All of the above-listed findings were presented to the tumor board of our institution, where the preliminary diagnosis of low-grade appendiceal mucinous neoplasm was established, and operative treatment in the extent of cecal resection was recommended, due to tissue abnormalities in the mouth of the appendix, which were observed on colonoscopy.
Preoperative preparation included antibiotic prophylaxis 60 min before skin incision and low-molecular heparin for the prophylaxis of thrombotic complications. Iodine–impregnated adhesive drapes were used after skin preparation with chlorhexidine solution. Ultrasound-guided TAP block was administered.
A laparoscopic approach was chosen. A 10 mm. video-trocar was placed above the umbilicus, and additional ports were placed along the midclavicular line on the left, below the umbilicus, suprapubic and along the anterior axillary line on the right, as shown on Fig. 3.
Fig. 3.
Trocar placement.
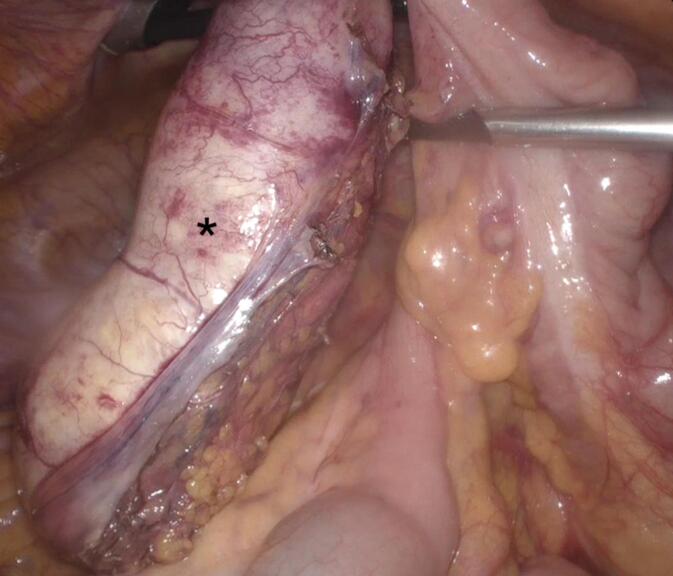
On laparoscopy, no free fluid or mucin in the abdomen and pelvis was detected. The Mucinous neoplasm was located at the right paracolic gutter. The cecum and ascending colon were mobilized with a lateral–to–medial approach (Fig. 4). After the mobilization was completed a linear–cutting stapler was placed on the cecum and fired. Then the appendix with the tumor was placed in the specimen–extraction bag and removed via the 5 cm-in-length Pfannenstiel incision, using the wound protector. Operative time was 83 min. Blood – loss was minimal.
Fig. 4.
View through the laparoscope - the mobilized LAMN is marked with the asterisk.
A pathology review of the specimen was performed: the appendix is 12.5 cm long and 4.5 cm in diameter. The resection margin is marked with a staple line. A serous layer is intact, and the wall of the appendix is 0.2 cm in width. Inside the lumen are jelly-like masses of a pale, yellowish color. Microscopically the wall of the appendix is unevenly thinned, with lymphatic infiltration and fibrous changes of the muscular and subserosal layers. The epithelial lining is mostly eroded. In the preserved areas of mucosa, there is mild epithelial dysplasia. In the place of eroded epithelium, there is mucin layering with its penetration inside the appendicular wall. Extramural spread of mucin and severe epithelial dysplasia were not detected. On the resection margin, the cecal wall is of a typical histological structure. The histological picture corresponds with a low-grade mucinous neoplasm of the appendix.
The postoperative period was without complications, the patient received standard postoperative care, which included early activation, and adequate pain relief laparoscopic approach allowed a quick recovery. The patient was discharged on postoperative day 4. Six months after the treatment, no evidence of recurrence on CT.
3. Discussion
From 2019 to 2024, in the Department of Pathomorphology and Oncogenetics of our institution, a histological examination of 224 appendixes was carried out. Of them, 86 (38.4 %) were studied in colonic resection specimens of various volumes, varying from resection of the ileocecal junction to total colectomy; 46 (20.5 %) – in specimens for simultaneous operations; 92 (41.1 %) – in specimens for appendectomies, open and laparoscopic. Out of 224 appendixes examined, 12 (5.4 %) specimens were with neoplasms of different nature.
Within this group, there was 1 (0.45 %) case of metastatic lesion of the appendix by high-grade ovarian serous carcinoma. 11 cases of primary neoplasms, of which 3 (1.4 %) were malignant and 8 (3.6 %) – benign. In the case of malignant neoplasms, there were 2 (0.9 %) cases of low-grade neuroendocrine tumors and 1 (0.45 %) case of mucinous adenocarcinoma. Benign neoplasms included 1 case (0.45 %) of sessile serrated lesion of the appendix. 3 (1.4 %) cases of appendiceal mucocele. 4 (1.8 %) cases of low-grade appendiceal mucinous neoplasms (LAMN). Our institutional experience in the treatment of appendicular neoplasia, as may be observed in the data provided by pathology department - is limited.
To confirm the diagnosis of LAMN, a thorough pathological examination of the appendiceal wall is performed. The main criterion for establishing the diagnosis is the presence of mild epithelial dysplasia. To assess the prognosis, the distribution of mucin must be evaluated, which is carried out during the preparation of the specimen for microscopic examination. Microscopically there are fibrous changes within the submucosal and muscular layers. Vanishing of proper and muscular plates within the mucosal layer is noted as well as suppression of lymphoid tissue (Fig. 5C). The epithelial lining is flat or villous with low–grade dysplasia (Fig. 5D). There is no invasive growth of dysplastic epithelium. Mucin may accumulate inside the appendicular wall, which subsequently causes its rupture [7]. Both exfoliated enterocytes and viable neoplastic cells can be observed in mucin.
Fig. 5.
Mucinous neoplasia of the appendix with epithelial low–grade dysplasia (LAMN). H&Ex40. A: Intraluminal mucin inside the appendix. B: The epithelial lining of the appendix with mild epithelial dysplasia, the lamina propria, and the muscular lamina of the mucous membrane is not defined, fibrotic changes in the submucosa and muscular layers are present. C: Extramural spread of cellular mucin with angiomatosis. D: Prolapse of acellular mucin in the subserous layer of the appendix.
Prognostic factors for mucinous neoplasia of the appendix are the degree of epithelial dysplasia, the presence of dysplastic changes at the resection margin, the extramural spread of mucin, and the presence of tumor cells in it [8,9].
Evaluation of the degree of epithelial dysplasia is a differential diagnostic criterion between mucinous neoplasia of the appendix with mild epithelial dysplasia (LAMN) and mucinous neoplasia of the appendix with severe epithelial dysplasia (HAMN). However, due to the rarity of this pathology, limited data, and heterogeneity of data from different studies, the reliable prognostic value of LAMN/HAMN confined to the appendix is unknown [10,11].
Dysplastic changes, present at the resection margin of the appendix increase the probability of recurrence or malignancy onset in the cecum. There is also a probability of mucin-producing tumor cells dissemination throughout the abdominal cavity, with the emergence of pseudomyxoma peritonei [12].
During the pathological investigation, the main indicator of preoperative rupture of mucinous tumor is the reaction of the serous membrane and visceral peritoneum of the mesentery, which is presented by inflammatory cell infiltration, and angiomatosis (Fig. 5C). These features are absent in case of postoperative rupture of the appendix or benign transfer of mucin on instruments [7]. The presence of mucin inside the muscular and subserous layers of the appendicular wall, without violation of its integrity (Fig. 5D) doesn't have a negative prognostic value [13].
Out of four investigated cases of LAMN in our center, only one was mucin extravasation, but in this case, no tumor cells inside mucin were detected. In the case presented, all of the above-mentioned prognostic factors are favorable.
The clinical picture of mucinous appendicular tumors, confined to the appendix - is mostly asymptomatic, most of the time diagnosis is established during a pathological examination of the specimen, and in the experience of our institution, after resections for non-related diseases. In the case described above, mucinous neoplasia has grown to a considerable size, which led to our patient presenting with complaints of discomfort and a palpable mass in the right lower quadrant. Sometimes mucinous tumors of the appendix may lead to an intestinal obstruction, as described in several case reports [14]. An encounter with a mucinous tumor in the setting of an acute abdominal emergency requires the surgeon to make a correct decision on the extent of resection, which wouldn't just relieve an acute condition but also be radical, so the patient doesn't develop pseudomyxoma peritonei.
As for the surgical treatment of AMN, confined to the lumen of the appendix, without intraabdominal mucin spread - a couple of decades ago, a right hemicolectomy was thought to be a radical procedure of choice regardless of the extent of the disease, because of an opinion that the disease could stay within occult lymph nodes, this concept was disproven in 2004 by González-Moreno S. and Sugarbaker P.H. [15]. Further research on this topic led the authors to describe the technique of radical appendectomy, for mucinous tumors of the appendix, which could be performed via an open technique or laparoscopically [16].
4. Conclusions
LAMN is a rare type of neoplasm, often diagnosed incidentally. When confined to the lumen of the appendix, it lacks the ability for infiltrative growth and lymph node metastasis. Appropriate treatment in case of a contained disease is surgical. While it is of utmost importance to prevent the spread of mucin inside the abdomen, technological advances and scientific data allowed the recommended extent of the surgery to be scaled down in the last couple of decades from a right hemicolectomy to a laparoscopic appendectomy. In our case, a cecal pole resection was necessary due to the size and width of neoplasia, to achieve negative resection margin.
Ethical approval
Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author contribution
Makarov Vladyslav, Romasko Ivan: Drafted the manuscript.
Yaroslav Voitiv, Borysenko Andrii, Makarov Vladyslav: Managed the patient.
Kropelnytskyi Vladyslav, Romasko Ivan: Performed pathological examination, and presented our institutional data.
Yaroslav Voitiv: Supervised the writing of the manuscript.
Oleksandr Usenko: Approved the final manuscript.
Guarantor
Olexandr Usenko ORCID iD 0000-0003-3866-4286 Director of National Institute of Surgery and Transplantology. Head of Department, Department of Thoracoabdominal Surgery, Professor, DSc, MD.
Consent
Written informed consent was obtained from the patient for publication of this report and accompanying images.
Declaration of competing interest
The authors declare no conflicts of interest related to this study.
References
- 1.Perivoliotis K., Christodoulidis G., Samara A.A., et al. Low-grade appendiceal mucinous neoplasm (LAMN) primarily diagnosed as an ovarian mucinous tumor. Case Rep Surg. 2021 doi: 10.1155/2021/5523736. Published 2021 Apr 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Smeenk R.M., van Velthuysen M.L., Verwaal V.J., Zoetmulder F.A. Appendiceal neoplasms and pseudomyxoma peritonei: a population based study. Eur. J. Surg. Oncol. 2008;34(2):196–201. doi: 10.1016/j.ejso.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 3.Umetsu S.E., Kakar S. Staging of appendiceal mucinous neoplasms: challenges and recent updates. Hum. Pathol. 2023;132:65–76. doi: 10.1016/j.humpath.2022.07.004. [DOI] [PubMed] [Google Scholar]
- 4.González Moreno S., Shmookler B.M., Sugarbaker P.H. Appendiceal mucocele. Contraindication to laparoscopic appendectomy. Surg. Endosc. 1998;12(9):1177–1179. doi: 10.1007/s004649900811. [DOI] [PubMed] [Google Scholar]
- 5.Kwak H.D. Outcomes of laparoscopic single-incision caecal pole resection for low-grade appendiceal mucinous neoplasm. J. Minim. Access Surg. 2023 doi: 10.4103/jmas.jmas_113_23. (Published online September 14) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sohrabi C., Mathew G., Maria N., et al. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2023;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. Published 2023 May 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Feely M, Gonzalez RS. LAMN and HAMN. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/appendixmucinousneoplasm.html.
- 8.Yantiss R.K., Shia J., Klimstra D.S., Hahn H.P., Odze R.D., Misdraji J. Prognostic significance of localized extra-appendiceal mucin deposition in appendiceal mucinous neoplasms. Am. J. Surg. Pathol. 2009;33(2):248–255. doi: 10.1097/PAS.0b013e31817ec31e. [DOI] [PubMed] [Google Scholar]
- 9.Pai R.K., Beck A.H., Norton J.A., Longacre T.A. Appendiceal mucinous neoplasms: clinicopathologic study of 116 cases with analysis of factors predicting recurrence. Am. J. Surg. Pathol. 2009;33(10):1425–1439. doi: 10.1097/PAS.0b013e3181af6067. [DOI] [PubMed] [Google Scholar]
- 10.Palavalli M., Koempel A., Kim A. Narrative review of appendiceal pseudomyxoma peritonei. Digest. Med. Res. 2023;6 doi: 10.21037/dmr-22-46. [DOI] [Google Scholar]
- 11.Murage N.W., Ahmed N.M., Underwood T.J., Walters Z.S., Breininger S.P. The genetic profile and molecular subtypes of human pseudomyxoma peritonei and appendiceal mucinous neoplasms: a systematic review. Cancer Metastasis Rev. 2023;42(1):335–359. doi: 10.1007/s10555-023-10088-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carr N.J., Cecil T.D., Mohamed F., et al. A consensus for classification and pathologic reporting of pseudomyxoma peritonei and associated appendiceal neoplasia: the results of the peritoneal surface oncology group international (PSOGI) modified Delphi process. Am. J. Surg. Pathol. 2016;40(1):14–26. doi: 10.1097/PAS.0000000000000535. [DOI] [PubMed] [Google Scholar]
- 13.Koç C., Akbulut S., Akatlı A.N., Türkmen Şamdancı E., Tuncer A., Yılmaz S. Nomenclature of appendiceal mucinous lesions according to the 2019 WHO Classification of Tumors of the Digestive System. Turk J Gastroenterol. 2020;31(9):649–657. doi: 10.5152/tjg.2020.20537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Komo T., Kohashi T., Hihara J., et al. Intestinal obstruction caused by low-grade appendiceal mucinous neoplasm: a case report and review of the literature. Int. J. Surg. Case Rep. 2018;51:37–40. doi: 10.1016/j.ijscr.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.González-Moreno S., Sugarbaker P.H. Right hemicolectomy does not confer a survival advantage in patients with mucinous carcinoma of the appendix and peritoneal seeding. Br. J. Surg. 2004;91(3):304–311. doi: 10.1002/bjs.4393. [DOI] [PubMed] [Google Scholar]
- 16.González-Moreno S., Sugarbaker P.H. Radical appendectomy as an alternative to right colon resection in patients with epithelial appendiceal neoplasms. Surg. Oncol. 2017;26(1):86–90. doi: 10.1016/j.suronc.2017.01.006. [DOI] [PubMed] [Google Scholar]