Background and epidemiology: Buruli ulcer, caused by Mycobacterium ulcerans, is the third most common mycobacterial disease in immunocompetent people, after tuberculosis and leprosy.1 It begins as a painless nodule or papule on the skin but, if left untreated, progresses to massive ulceration that may cover 15% of a patient's skin.2 Healing is protracted and often results in deformity and disability, particularly in children, in whom it can cause joint contracture, subluxation, disuse atrophy or distal lymphedema.3
The name is derived from the Buruli region in Uganda, where superficial ulcerative lesions in Ugandan children were investigated in 1962. In the past decade the incidence has increased dramatically in West Africa,1 in concert with environmental changes (e.g., regional flooding). In some communities up to 16% of the people have been affected.3 In 1998 the World Health Organization (WHO) established the Global Buruli Ulcer Initiative to draw attention to this disease and mobilize international efforts to understand and deal with it (www.who.int/gtb-buruli).
The natural reservoir for M. ulcerans is unknown.3 Skin contamination is thought to be the route of exposure. An environmental exposure, either by direct inoculation or an insect vector, is suspected. Many victims live near slow-moving or stagnant water. People of all ages, but particularly children less than 15, are affected. Most lesions occur on the limbs (right arms in children and left legs in adults). These observations support the hypothesis that M. ulcerans is usually harmless, living in symbiosis with the roots of certain plants in swampy areas, and that transmission to humans occurs through penetrating injuries when these organisms and their habitats are disturbed. The left leg is most often exposed to weeds and grasses when farmers use cutlasses, and children often grasp vegetation with their right hands. Incubation is thought to take anywhere from 2 months to several years.4
Clinical management: A painless, firm nodule teeming with bacteria marks the first stage of disease. Associated systemic signs are rare.4 Erythema and induration usually accompany the first stage but subside as ulceration occurs.2 Unlike most other mycobacteria, M. ulcerans produces a circumscribed area of necrosis that primarily contains extracellular acid-fast bacilli.2 The lesions are symmetrical, with associated coagulation necrosis in the deep dermis; they rarely penetrate beyond the fascia to underlying muscle. The observation that the necrosis often extends some distance from the site of bacterial colonization has led to the understanding that M. ulcerans secretes one or more toxins.2 The absence of host-derived inflammatory exudates has led some to suggest that factors secreted by M. ulcerans may possess immunosuppressive properties that indirectly contribute to the destruction of human tissue. Others attribute this to infarction, with no contribution from cytotoxic bacterial factors.3
The painless ulcer has undermined edges and necrotic slough. Early excision of small, preulcerative lesions is curative. Necrotic lesions should be excised beyond the margins of the necrosis to prevent persistent subcutaneous infection. Skin grafting is often necessary. Treatment with antimycobacterial agents has generally been disappointing, especially in advanced cases.4
Prevention: Bacillus Calmette–Guérin vaccine has an incomplete protective effect against Buruli ulcers.4 Early detection and rapid surgical treatment are the best interventions available until other means of prevention and treatment are identified. Unfortunately, because the ulcers are painless and the victims often live in remote communities, most patients do not receive medical attention until the damage is extensive. A review of 102 patients in Ghana indicated that the average length of hospital stay was more than 100 days; the infection led to 10 amputations, 12 joint contractures and 2 deaths from tetanus and sepsis.5
Strengthening general health services in endemic areas is key to controlling Buruli ulcers. This includes health education, training health workers and upgrading surgical facilities. The WHO is appealing for research in areas that could provide better understanding of the mode of transmission, including the link to environmental disturbances such as flooding, and of prevention and treatment.3
Erica Weir CMAJ
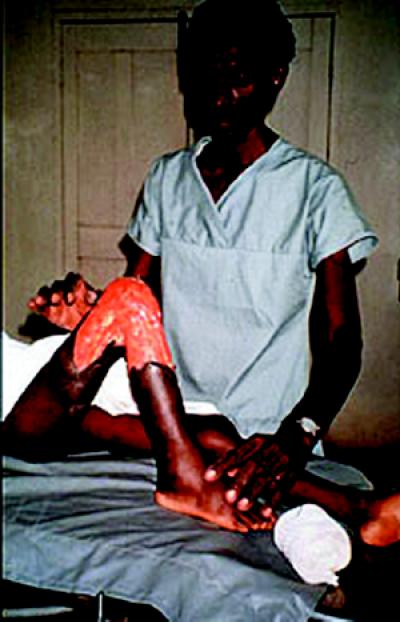
Figure. Early detection and rapid surgical treatment are the best interventions. Photo by: World Health Organization
References
- 1.Buruli ulcer. Wkly Epidemiol Rec 2000;75 (13): 106-8. [PubMed]
- 2.George K, Chatterjee D, Gunawardana G, Welty D, Hayman J, Lee R, et al. Mycolactone: a polyketide toxin from Mycobactrium ulcerans required for virulence. Science 1999;283:854-7. [DOI] [PubMed]
- 3.Dobos KM, Quinn FD, Ashford DA, Horsburgh CR, King CH. Emergence of a unique group of necrotizing mycobacterial diseases. Emerg Infect Dis 1999;5(3):367-78. [DOI] [PMC free article] [PubMed]
- 4.Van der Werf TS, van der Graaf WT, Tappero JW, Asiedu K. Mycobacterium ulcerans infection [review]. Lancet 1999;354:1013-8. [DOI] [PubMed]
- 5.Asiedu K, Etuaful S. Socioeconomic implications of Buruli ulcer in Ghana: a three-year review. Am J Trop Med Hyg 1998;59:1015-22. [DOI] [PubMed]


