Abstract
Background:
The largest identified kindred worldwide with a single mutation causing autosomal-dominant Alzheimer’s disease (ADAD) is a family from Antioquia, Colombia, carrying the Presenilin-1 (PSEN1) E280A (Paisa) mutation. The majority of mutation carriers develop dementia, typically commencing in their late 30 s, with a median onset age of 49 years. Cognitive decline is a hallmark feature.
Objective:
This review synthesizes the existing literature on neuropsychological assessments in PSEN1 E280A mutation carriers throughout their lifespan. We provide a comprehensive overview of cognitive outcomes in this unique population.
Methods:
We reviewed and integrated the published research, analyzing studies on neuropsychological assessments in PSEN1 E280A carriers. Our focus was on measures of verbal, semantic, episodic, and spatial memory, and encompassed other cognitive domains such as language, attention, visuospatial memory, and executive functioning.
Results:
Verbal, semantic, episodic, and spatial memory emerged as the most sensitive indicators of preclinical changes in PSEN1 E280A carriers. Inconsistencies were noted in findings from tests assessing language, attention, visuospatial memory, and executive functioning, suggesting potential limitations in detecting early cognitive changes in PSEN1 mutation carriers. Specific cognitive tasks developed for this population proved effective but underutilized.
Conclusions:
The review underscores the importance of continued test development tailored to detect early cognitive changes in PSEN1 E280A carriers, potentially enhancing ADAD screening. Furthermore, investigating ADAD mutations in children may identify early changes in AD and enhance our understanding of neuropsychological functioning across the lifespan. This synthesis provides valuable insights for researchers, clinicians, and policymakers engaged in the study and management of ADAD.
Keywords: Alzheimer’s disease, autosomal dominant Alzheimer’s disease, cognitive measures, cognitive outcomes, dementia, early detection, familial AD, preclinical AD
INTRODUCTION
Alzheimer’s disease (AD) is a neurodegenerative disorder that presents itself clinically by the progressive loss of cognitive functioning that eventually interferes with a person’s daily activities.1 Changes in cognition vary across disease stage/severity and by AD type. Differences in AD trajectory can also be impacted by environmental and genetic risk factors.2 Most individuals who develop AD demonstrate subtle changes in episodic memory and executive function first followed by changes in visuospatial processing and language.3,4 Cognitive tests that are sensitive to early changes in memory in particular are important for AD diagnosis and disease monitoring and can help determine the level of impairment and care individuals require.1,2
AD is the most common cause of late-onset dementia in older adults.3 The age at which individuals experience decline in cognitive function varies based on the etiology. Autosomal dominant AD (ADAD) is a form of AD caused by mutations in the genes coding for amyloid precursor protein (APP), presenilin 1 (PSEN-1), or presenilin 2 (PSEN-2). These mutations cause over-production of the amyloid-β peptide (Aβ).4 Aβ is often particularly abundant in the cerebral cortex, hippocampus, cerebellum, mid-brain, and basal ganglia and is associated with AD disease progression.4 Individuals with a mutation in one of these genes usually present symptoms before the age of 65 years, with most showing mild memory impairment in their late 30 s and dementia in their 40 s.
The largest identified ADAD kindred in the world with a single mutation is a family of individuals with the E280A mutation in PSEN1 (Paisa mutation) from Antioquia, Colombia. There are currently approximately 5,000 living members of this kindred spread among 25 families. Of the 5,000 members it is estimated 1,000 carry the mutation.5 There are about 400 confirmed carriers.5 By analyzing the cognitive outcomes of individuals with genetic AD, researchers can identify typical and atypical cognitive patterns, detect changes in the preclinical stages, and track the progression of the disease. This can help establish a nuanced understanding of how AD affects cognition, which can then be compared to sporadic AD cases to identify similarities and differences.
Early-onset AD also occurs in sporadic forms and is not limited to ADAD.6 However, different from sporadic forms, those with ADAD are genetically destined to develop dementia with near 100% certainty.7 While ADAD specifically refers to autosomal dominant cases typically presenting early in life, it shares pathological features with sporadic AD, including the accumulation of amyloid plaques and neurofibrillary (tau) tangles. These features are believed to damage brain structures, impair brain metabolism, and result in cognitive decline. The shared characteristics in disease progression and cognitive decline highlight the possibility of applying findings from ADAD research to other forms of the disease. If specific assessments demonstrate a strong ability to detect cognitive decline in ADAD, they could potentially be valuable for the early diagnosis and monitoring of sporadic AD patients as well. By understanding the cognitive outcomes of ADAD, researchers can explore treatment strategies in earlier stages of the disease that will be more effective in slowing cognitive decline. Because ADAD is deterministic, meaning that individuals develop cognitive decline with near certainty, a review of the literature that systematically characterizes the sensitivity of measures used to detect these declines will clarify which cognitive measures are most sensitive to earliest changes and where we can work to develop more sensitive measures in the future.
METHODS
A total of 38 research papers were identified for review. Our search focused on research on cognitive test data with the Colombian kindred. The articles evaluated described a comprehensive set of tests that measured cognitive functions including but not limited to attention, executive function, memory, language, praxis, abstract reasoning, subjective memory complaints, and global cognition. Articles dated from 1994, which was the year of the first published research that presented case studies on the neuropsychological outcomes of three individuals from the Colombian kindred,7 to the present. All studies were found using Google Scholar, PubMed, Scielo, and PsycInfo searches between September 2022 to January 2024. There was one researcher conducting the review (AG), and searches were done for relevant articles four separate times between September 2022 to January 2024, to ensure that any new published data were included. Search terms included Presenilin1 E280A, autosomal dominant Alzheimer’s disease, Colombian kindred, cognition, cognitive characteristics, and cognitive outcomes. Articles from this search included works in both English and Spanish. Only studies reporting cognitive data from this cohort were included. Studies focusing on biological, neuroimaging, or blood-based biomarkers without cognitive data were not included in this review. Those cognitive studies were then classified based on the age of the sample (children were classified as a mean age of <18 and adults as >18), and on the cognitive domains tested, as described previously.8,9 More details on study selection can be found in Fig. 1.
Fig. 1.
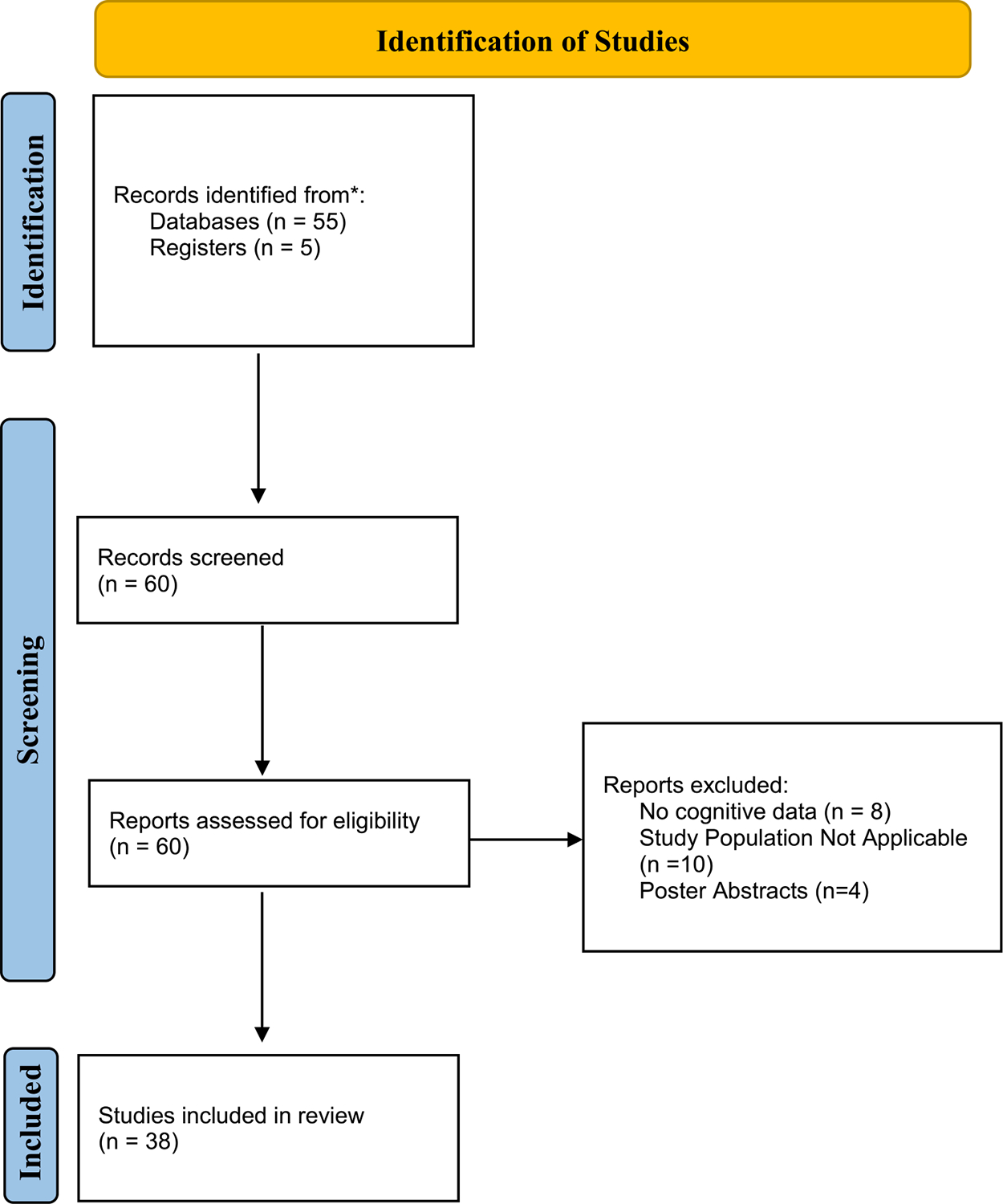
Identification of Studies for Review. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71
To examine cognitive changes across the lifespan, we included data from two cognition assessments in children from the same family (average age of approximately 11.6 at testing).8,10 Because there are currently only two published studies on children, and cognitive differences between carrier and non-carrier children are beginning to emerge, more research is needed to fully understand these cognitive differences.
We use the term “cognitively unimpaired carriers” to describe individuals carrying the PSEN1 E280A mutation who have not yet exhibited cognitive changes they are classified in the literature as having a Functional Assessment Staging Tool for Dementia (FAST) score of 2 or lower and a Mini-Mental State Examination Score (MMSE) of 25 or over.11,12 “Cognitively impaired carriers” refers to individuals displaying signs of memory loss. They are classified in the literature as having a FAST score higher than 3 (maximum 7), and MMSE lower than 24.11,12 These individuals are starting to experience memory and thinking issues but are still in the early stages of disease progression, and generally perform 1.5 SD away from normative values on objective cognitive tests. The definition of cognitively impaired carriers in various articles sometimes included individuals with mild cognitive impairment (MCI), and dementia. Readers should consult the original articles to understand the specific definitions used by the authors. Lastly, “non-carrier cognitively healthy controls” refers to age-matched family members of mutation carriers who have no cognitive impairments. It is important to note that because all the studies included in this review draw upon participants from the PSEN1 E280A cohort, it is difficult to quantify the exact number of unique participants, as participants may have participated in several studies. The median sample size of participants in studies that included adult carriers was 26 (interquartile range [IRQ]: 19–17) and the median sample size of non-carrier cognitively healthy controls was 31 (IRQ 21–75) across studies. The approximate age range of the adult samples was 22–66 years. Tables 1 and 2 provide a summary of the characteristics of the studies included in this review with adults (sample size, sample demographics).
Table 1.
Demographics of Studies that Included Cognitively Impaired and Cognitively Unimpaired Carriers versus Non-Carriers
| Cognitively unimpaired Carriers | Cognitively impaired/MCI Cognitively Impaired Carriers | Non-Carriers | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Sample Size | Age | Edu Level | Sample Size | Age | Edu Level | Sample Size | Age | Edu Level | |
| N | M (SD) | M(SD) | N | M (SD) | M (SD) | N | M (SD) | M (SD) | |
| Acosta-Baena, 20119 | 287 | NP | NP | 276 | NP | NP | 1335 | NP | NP |
| Arango Lasprilla, 200369 | 9 | 37.67 (5.61) | 3.67 (1.2) | 9 | 49.6 (4.9) | 3 (1.2) | 0 | NP | NP |
| Bobes, 201011 | 24 | 48.2 (NP) | NP | 25 | 42.8 (NP) | NP | 27 | 39.3 (NP) | NP |
| Fox-Fuller, 202253 | 35 | 30.4 (5.3) | 11.1 (3.4) | 5 | 30.5 (5.3) | 7.0 (2.8) | 26 | 36.6 (6.5) | 11.4 (4.3) |
| Guzmán-Vélez, 202078 | 24 | 35.8 (5.0) | 9.9 (4.5) | 5 | 44.5 (1.34) | 9.80 (5.17) | 19 | 36.8 (5.68) | 10.4 (4.2) |
| Guzmán-Vélez, 202112 | 13 | 38.8 (5.9) | 9.25 (4.7) | 6 | NP | NP | 19 | 36.4 (5.2) | 11.4 (3.9) |
| Lopera, 199745 | 0 | NP | NP | 15 | NP | NP | 34 | NP | NP |
| Norton, 202043 | 21 | 37.5 (6.5) | 11.4 (3.8) | 7 | 44.8 (1.4) | 9.3 (3.4) | 30 | 37.7 (6.5) | 9.9 (4.1) |
| Parra, 201087 | 30 | 45.2 (4.8) | 8.5 (4.2) | 22 | 45.2 (5.8) | 8.5 (4.2) | 30 | 40.9 (9.3) | 9.5 (3.2) |
| Parra, 201541 | 18 | 35.1 (5.5) | 10.2 (3.9) | 19 | 47.5 (6.4) | 7.3 (3.7) | 21 | 39.3 (8.3) | 10.3 (27) |
| Rosselli, 201027 | 0 | NA | NA | 12 | 49.61(4.9) | 2.6 (2.9) | 15 | 45.0(7.2) | 4.73 (3.7) |
| Tirado, 200488 | 39 | 50.1 (3.4) | 5.1 (3.4) | 21 | 50.1 (3.4) | 5.1 (3.4) | 30 | 38.5 (6.9) | 5.2 (3.9) |
| Tirado, 200828 | 39 | 49.8 (3.0) | 5.2 (3.8) | 22 | 49.8 (3.0) | 5.1 (3.4) | 30 | 40.9 (10.5) | 5.3 (3.5) |
| Vila-Castelar, 202049 | 35 | 32.14 (3.73) | 10.72 (3.68) | 19 | 40.3 (4.92) | 7.1 (3.8) | 48 | 34.4 (4.3) | 10.4 (4.2) |
| Vila-Castelar, 202089 | 19 | 32.1 (NP) | 12.3 (NP) | 11 | 32.9 (NP) | 8.4 (NP) | 23 | 47.6 (NP) | 11.3 (NP) |
NP, not provided; NA, not applicable.
Table 2.
Demographics of Studies that Include Cognitively Unimpaired Carriers Only
| Cognitively Unimpaired Carriers | Non-Carriers | |||||
|---|---|---|---|---|---|---|
| Sample Size | Age | Edu Level | Sample Size | Age | Edu Level | |
| n | Mean (SD) | M(SD) | n | Mean(SD) | M (SD) | |
| Aguirre-Acevedo, 201621 | 493 | 33.4 (11.7) | 7.2 (4.2) | 0 | NA | NA |
| Arango-Lasprilla, 200733 | 19 | 43.2 (3.0) | 5.0 (3.0) | 21 | 45.3 (3.7) | 5.6 (3.9) |
| Ardila, 200059 | 40 | 34.5 (7.2) | 5.5 (3.9) | 82 | 44.5 (12.0) | 5.5 (3.9) |
| Ayutyanont, 201480 | 56 | 43.9 (6.5) | 7.8 (4.6) | 78 | 44.9 (10.7) | 7.2 (3.9) |
| Baena, 202122 | 33 | 35.7 (5.6) | 10.0 (3.9) | 41 | 35.9 (5.3) | 10.4 (4.2) |
| Bocanegra, 202146 | 19 | 35 (NP) | 11.0 (NP) | 26 | 36.0 (NP) | 11 (NP) |
| Cuetos, 200766 | 19 | 43.2 (3.1) | 5.11 (3.0) | 21 | 45.3 (3.7) | 5.55 (3.9) |
| Gatchel, 202076 | 21 | 35.7 (5.4) | 9.7 (4.2) | 27 | 35.6 (5.2) | 10.5 (4.3) |
| Giudicessi, 202354 | 15 | 35.7 (5.5) | 10.6 (3.8) | 31 | 38.9 (6.1) | 11.4 (4.3) |
| Guzmán-Vélez, 201860 | 233 | 27.7 (9.5) | 7.8 (3.8) | 1162 | 32.0 (12.6) | 8.3 (4.4) |
| Lopera, 19947 | 3 | NP | NP | 0 | NP | NP |
| Martinez, 202226 | 310 | 27.5 (8.8) | 8.6 (4.2) | 1988 | 31.5 (10.4) | 9.4 (4.2) |
| Norton, 201775 | 26 | 35.6 (7.7) | 10.1 (3.0) | 26 | 37.2 (6.5) | 10.2 (3.5) |
| Quiroz, 201061 | 20 | 33.7 (6.0) | 10.7 (2.4) | 19 | 34.4 (6.4) | 10.8 (3.3) |
| Quiroz, 201179 | 10 | 34.2 (6.4) | 11.8 (2.4) | 11 | 33.2 (6.1) | 11.9 (0.9) |
| Quiroz, 201562 | 20 | 34.5 (6.3) | 10.7 (2.3) | 10 | 34.0 (5.9) | 10.8 (3.3) |
| Rios-Romenets, 202023 | 167 | 37 (5) | 8.8 (4.1) | 75 | 42 (6) | 8.5 (4.4) |
| Vannini, 202024 | 396 | 33.5 (12.5) | 7.8 (4.3) | 1983 | 30 (10.4) | 8.6 (4.5) |
| Vila-Castelar, 202025 | 0 | NA | NA | 59 | 50.3 (15.3) | 9 (4.1) |
| Vila-Castelar, 202132 | 167 | 37.7 (5.8) | 8.8 (4.2) | 75 | 41.5 (6.3) | 8.3 (4.8) |
| Yucebas, 202431 | 48 | 37.4 (7.2) | 9.8 (4.1) | 51 | 36.2 (6.0) | 9.7 (4.7) |
NP, not provided; NA, not applicable; SD, standard deviation.
RESULTS
Children
We included two studies that looked at the cognitive outcomes of children with PSEN1 E280A carriers and non-carrier healthy controls. The first study, published by Quiroz et al. (2015), collected neuropsychological and imaging data on a group of 37 children between the ages of 9–17 years (mean age 13 years), 18 of whom were PSEN1 E280A carriers and 19 non-carrier cognitively healthy controls.8 The second, by Fox-Fuller et al. (2021), collected neuropsychological data from of 1354 children, including 265 carriers ages 6–16 (mean age 11.6 years).10
Both studies used the Escala Wechsler de Inteligencia para Niños/Wechsler Intelligence Scale for Children (WISC), 3rd and 4th edition.8,10 The WISC is a neuropsychological battery commonly used to measure cognitive abilities in children ages 6–16 years.13 The WISC-IV has 15 subtests, with the first ten subtests being core subtests, and five complementary subtests. The five complementary subtests were not used in these two studies. The core 10 subtests provide a Full-Scale IQ score (FSIQ), and scores on the following four indices: Verbal Comprehension Index (VCI), Perceptual Reasoning Index (PRI), Working Memory Index (WMI), and Processing Speed Index (PSI). The VCI is used to test language-based abilities and consists of 3 subtests: Vocabulary, Similarities, and Comprehension subtests. WMI examines concentration and includes Digit Span and Letter-Number Sequencing subtests. PSI measures mental processing and includes Coding and Symbol Search subtests, both of which are timed. It is important to note that the normative data for this measure in Spanish were collected from children from Mexico, and this measure had not been normed for a Colombian population at the time of data collection for both of these studies.14
Outcomes
None of the studies reported scores for specific subtests. Only scores for the specific indices were provided in both studies, and in the case of Quiroz et al. (2015), FSIQ was also provided. In Quiroz et al. (2015), there were no differences between carriers and non-carrier cognitively healthy controls on any of the indices or FSIQ.8 This pattern also occurred in the study by Fox-Fuller et al. (2021), where carriers often performed slightly better than non-carrier healthy controls.10 Table 3 shows a side-by-side comparison of cognitive results of the two studies. It is worth noting that Fox-Fuller et al. (2021) found differences between sexes irrespective of genetic status, with boys performing lower on WMI, PRI and VCI.10 There was also an interaction between sex and genetic status in the full sample: Males who were carriers had lower WMI performance than carrier and non-carrier females. More research is needed to examine the potential biological underpinnings that could be contributing to differences between the sexes in cognition at this age such as puberty status.
Table 3.
Cognitive Outcomes for PSEN E280A Children
| Quiroz, 20158 | Fox-Fuller, 202110 | |||
|---|---|---|---|---|
| WISC Indices | Carriers | Non-carrier cognitively healthy controls | Carriers | Non-carrier cognitively healthy controls |
| VIQ | 85 | 86 | 90 | 89 |
| PIQ | 86 | 91 | 92 | 92 |
| WMIQ | 88 | 88 | 91 | 92 |
| PSIQ | 92 | 84 | 86 | 87 |
| Total IQ | 86 | 84 | Not provided | Not provided |
VIQ, Verbal Intelligence Quotient; PIQ, Perceptual Intelligence Quotient; WMIQ, Working Memory Intelligence Quotient; PSIQ, Processing Speed Intelligence Quotient; Total IQ, Total Intelligence Quotient. Values provided above are M values for each group.
Adults
PSEN1 E280A carriers typically develop memory deficits in their late 30 s followed by progressive impairments in other cognitive domains, such as verbal fluency. Mild cognitive impairment sets in around age 45 and dementia by age 50.9 Most carriers develop dementia between age 45 and 50. A 35-year window has been documented, with rare cases experiencing onset as early as age 30 or as late as age 65.15,16 The median duration from onset of dementia to death is approximately 10 years, ranging from nine to 12 years, with 59 being the median age at death.17
Thirty-six of the 38 articles identified for this review focused on adults. We grouped this review by cognitive domain and the results of the respective subtests or sub scores included in each measure. It is important to note that many of the cognitive measures mentioned below can often belong to more than one domain (e.g., Trail Making Test [TMT] A can provide information about both processing speed and attention), as they may assess multiple cognitive processes. In these instances, we grouped the tests based on the way they were presented in their respective articles. We followed similar groupings from a previous article by Acosta-Baena et al. (2011) when specific domains were not provided.9 More information regarding cognitive tests and their respective domains in each study can be found in Supplementary Table 1.
Memory
Consortium to Establish a Registry for Alzheimer’s Disease Word List Learning
Memory was tested using several verbal and visual tests. One of the most used measures was the Consortium to Establish a Registry for Alzheimer’s Disease (CERAD) list learning, which includes three conditions: Word List Learning, Delayed Recall, and Word List Recognition. The CERAD Word List Learning is part of a neuropsychological screening battery originally developed in English18 that includes 7 subtests: MMSE, Semantic Fluency (Animals), Word List Learning, Word List Recall, Word List Recognition, Modified Boston Naming (15 items), and Constructional Praxis. This battery has been validated to distinguish between AD and cognitively normal aging.18,19 The Spanish CERAD has been standardized in Colombia.20 The Word List Memory task is divided into learning, free recall, and recognition.
First, participants are shown 10 cards with one word each over three trials and are instructed to read them aloud and memorize them. Each card is presented for two seconds. The score is calculated as the sum of words recalled correctly over three trials, for a maximum score of 30 points (Word List Learning). Intrusions are recorded and scored separately. After a 7-minute delay, participants are asked to recall the 10 words that were previously shown (Word List Delayed Recall). The total score is calculated as the total number of correct words for a maximum score of 10. Finally, participants are shown a list of 20 words (10 target words and 10 distractors) and are asked to indicate whether they recognized the target words. The total score is calculated as the sum of correct “yes” and ‘no” answers minus 10 (Word List Recognition). Negative totals are given a score of zero.20 Different conditions of CERAD scores exhibited different sensitivity depending on if the PSEN1 E280A carriers were cognitively unimpaired or cognitively impaired. In articles that examined differences between cognitively unimpaired carriers and non-carrier healthy controls, there were no group differences in CERAD Word List Learning condition, Word List Delayed Recall and Word List Delayed Recognition scores.21–25 The Delayed Recall Condition was more sensitive to memory changes in cognitively impaired carriers, who performed more poorly than non-carrier cognitively healthy controls.9,12,26 In a longitudinal study, there were declines in CERAD Word List Learning Scores across a period of eighteen months in participants ranging in age from 45–60.27 Further, cognitively impaired carriers produced more phonemic, semantic, and non-related intrusions than their cognitively unimpaired carrier counterparts across both learning and recall trials on the CERAD Word List Learning test.28 In a longitudinal study, Aguirre-Acevedo et al. (2016) found that CERAD Word List Learning scores were more sensitive than confrontation naming as measured by the Boston Naming Test (BNT) in detecting cognitive decline in this population. The CERAD Word List learning was able to detect cognitive decline 12 years before the onset of MCI and 17 years before the onset of dementia.21
The Free and Cued Selective Reminding Task
The Free and Cued Selective Reminding Task (FCRST)29 was also commonly used to assess memory in this population. The FCSRT is a neuropsychological test designed to assess associative memory and is often used in the context of AD and related memory disorders. The FCSRT consists of two main conditions: Total Recall and Delayed Recall.29,30 In the Free Recall condition of the FCSRT, the individual is initially presented with a list of words to remember. These items are typically organized into semantic categories, such as animals, fruits, or common objects. The person is asked to recall as many items from the list as possible, without any specific cues or prompts. This condition measures the individual’s ability to spontaneously retrieve and recall information from their memory. Immediately after, they are provided with cues or category names to help trigger their memory and a Total Recall score is generated. The Total Recall score is the sum of words participants recalled with and without semantic cues. The Total Recall condition provides insight into a person’s immediate or short-term memory and their ability to retain and retrieve information with external cues. In the Delayed Recall condition of the FCSRT, there is a delay introduced after the initial presentation of the list of items. After a set period of time (often 30 min), the individual is asked to recall as many items from the original list as they can remember, and a Delayed Free Recall score is generated. Then they are provided with cues or category names to help trigger their memory and a total delayed recall score is generated. The Delayed Recall condition assesses the person’s ability to retrieve information from their long-term memory with the assistance of cues.29 This test is helpful in distinguishing between executive-related deficits and temporal dysfunction. It differentiated between cognitively impaired mutation carriers and non-carriers. However, it did not distinguish cognitively unimpaired mutation carriers from non-carriers. Regarding AD-related pathology in cognitively unimpaired mutation carriers, worse performance on the Free and Cued Selective Reminding Test (FCRST), specifically the free delayed recall scores, predicted greater cortical amyloid and tau burden in the entorhinal cortex. Additionally, worse immediate Free Recall (FR) and Delayed Free Recall (dFR) scores predicted tau burden in both the entorhinal cortex and the inferior temporal cortex. These findings support the idea that FCRST scores are sensitive to early pathology burden in the preclinical stage of AD.12
In a separate sample of 48 cognitively unimpaired carriers (mean [M] age [SD]: 37.4 [7.2]) and 51 healthy non-carrier controls (M age [SD]: 36.2 [6.0]), carriers had poorer performance on total immediate, delayed free and cued recall scores on the FCRST than non-carriers.31 Finally, in a sample of 167 carriers and 75 non-carrier cognitively healthy controls ages 30–53, cognitively unimpaired female carriers showed better verbal memory than male carriers when mildly cognitively impaired carriers were included. There was no difference in performance on other cognitive tests (constructional praxis, Multilingual Naming Test (MINT), and Raven Progressive Matrices) between females and males in non-carrier cognitively healthy controls.32
Initial Verbal Memory Tasks
There were several visual memory tasks that were also able to distinguish between carriers and non-carrier healthy controls. Arango-Lasprilla et al. (2007) reported on a task that showed participants photos of culturally relevant famous faces.33 This task was created specifically for this study and consisted of presenting the participant with photos of the faces of 30 famous Colombians. Each photo was presented on a separate page, and the person was asked to name the person. The dependent variable was the number of faces for which first and last names were correctly identified. The investigators used this task with a sample of 19 cognitively unimpaired carriers (M age 43.2, SD = 3.0) and 21 noncarriers (M age 45.3, SD = 3.7) They found that this was the only test that elicited significant differences between carriers and non-carriers, with no differences found in performance of the eleven other tasks of lexical and semantic memory, including word reading, dictation of words, naming of action and object drawings, word drawing matching, and others. These findings align with previous research by Vogel et al. (2005) and Estevez-Gonzalez et al. (2004), both of which studied individuals with mild cognitive impairment but without dementia. Vogel and colleagues identified deficits in naming famous faces during the preclinical phase of AD. Estevez-Gonzalez and colleagues found that performance on a famous people naming task was the best predictor of a clinical diagnosis of probable AD two years later.34,35 It is important to note some limitations for this latter study. The sample size was small and may not have been representative of the total population of individuals with this particular mutation; the task was developed in Colombia for this specific ADAD population; and reports on validity and reliability were not included in the original text. Additionally, both the carriers and noncarriers had very low educational levels, and therefore the results may not be generalizable to individuals with AD with more years of formal schooling.
The Visual Short Term Memory Binding Test
The Visual Short Term Memory Binding (VSTMB) Test is a task of binding, or the ability to integrate an object’s features to temporarily retain their identity.36 In the short term, binding underpins the temporary retention of associations of features as complex objects and in the long term, binding mediates the learning of association of meaningful events.37 During this task, individuals are shown a trio of colored polygons on a computer screen followed by a blank screen and then another trio of polygons. They then must indicate whether the second trio of polygons was different from or the same as the first trio. This task has three conditions: color only (CO) requires recognition of only color, shape only (SO) requires recognition of only shape, and color shape binding (CSB) requires recognition of both shape and color.38 VSTMB performance has been shown to be impaired in older individuals with subjective cognitive decline and with MCI, as well as individuals with sporadic AD.39,40
In a study by Parra et al. (2015), this measure was administered to 19 cognitively unimpaired carriers with ADAD, 18 cognitively unimpaired mutation carriers, and 21 of their healthy control counterparts (non-carrier family members) with an age range of 24–66.41 Scores on the VSTMB test distinguished between carriers and non-carrier cognitively healthy controls in the CSB condition but not the CO or SO conditions. Patterns of performance were consistent in both cognitively impaired mutation carriers and cognitively unimpaired mutation carriers, with highest performance on the color-only task, followed by shape only, and weakest performance on the CSB condition. In non-carrier healthy controls, performance was best on CO, while performance on SO and CSB conditions was similar. Performance on this task, specifically CSB conditions, was able to discriminate cognitively unimpaired carriers from non-carrier cognitively healthy controls even when other neuropsychological measures of memory could not. These results suggest a differential and specific impairment in visual short-term memory binding in PSEN1 E280A carriers and cognitively unimpaired carriers characterized by a loss of the ability to represent objects integrated as a whole in visual short-term memory. Additionally, the results suggest that short-term memory binding deficits in AD do not seem to be restricted to specific types of information (visual and verbal stimuli) or to a specific retrieval process (recall and recognition).40,42
Relatedly, findings from Norton et al. (2020) indicated that when comparing cognitively unimpaired carriers and non-carrier healthy controls, VSTMB performance was impaired for cognitively unimpaired carriers, but the impairment was not unique to the CSB condition, as it was in earlier studies. In this study, VSTMB performance strongly correlated with markers of AD pathology and disease progression such as entorhinal cortex tau, though the relation was stronger for the SO condition than the CSB condition.43 Results from both of these studies indicate that both shape-only and color- and shape-binding conditions of the VSTMB task can potentially serve as a sensitive measure to early memory decline in preclinical stages of AD.
The Rey–Osterrieth Complex Figure
In the Rey–Osterrieth Complex Figure (ROCF), individuals are presented with a picture of a complex geometrical figure and are asked to copy the figure and later produce it from memory after a short delay.44 There are three conditions of this task: Copy, Immediate Recall, and Delayed Recall. In the Copy condition, participants are presented with a picture and asked to copy the figure. In the Immediate Recall condition, after a short delay, the examinee is asked to reproduce the figure from memory.44 In the Delayed Recall condition, after a longer delay (20–30 min), the examinee may again be asked to draw the figure from memory. Examinees are not told beforehand that they will be asked to draw the figure from memory; the Immediate and Delayed Recall conditions are therefore tests of incidental memory. Each copy is scored for the accurate reproduction and placement of 18 specific design elements with a maximum of 36 points.44 Four hundred and fifty-nine asymptomatic PSEN1 E280A mutation carriers (mean age = 39.7 years) showed poorer cognitive performance than non-carrier healthy controls, but this was only observed in carriers who reported subjective memory complaints.9,45 In many of the studies, there were differences on the Immediate and Delayed Recall conditions of the ROCF between cognitively impaired carriers and cognitively unimpaired carriers, but not between non-carrier cognitively healthy controls and cognitively unimpaired carriers.46 It is also important to note that in other studies using ROCF there were no differences between any groups (cognitively impaired carriers, cognitively unimpaired carriers, and non-carrier healthy controls) in the Copy condition, providing further support that difficulty to reproduce the figure is related to memory problems and not to differences in visual construction or planning abilities.41,42 Demographics of studies mentioned in this section are in Tables 1 and 2.
The Latin American Spanish Version Face Name Associative Memory Test (LAS-FNAME)
This test measures memory changes along the AD spectrum and has been extensively validated to detect cognitive decline across time between clinically normal older adults and individuals with MCI.47,48 In this task, participants are shown a variety of different faces and asked to remember the name associated with each. Vila-Castelar et al. (2020) validated the measure with 59 clinically normal individuals from Medellin, Antioquia, Colombia with an age range of 27–83 years.25 After validation, this measure was tested on carriers (both cognitively impaired and cognitively unimpaired) and non-carrier cognitively healthy controls to confirm its sensitivity to pathological changes in preclinical ADAD.25 Results showed that cognitively unimpaired carriers who did not express cognitive concerns nevertheless showed lower scores on the LAS-FNAME total scores than non-carrier cognitively healthy controls, suggesting that this task is sensitive to very early memory changes. Additionally, across all carriers, higher levels of Aβ and regional tau in the entorhinal and inferior temporal cortices were associated with lower LAS-FNAME total scores.49
Memory for Semantically Related Objects (MESERO)
Memory tests of semantic language processing are also starting to show clinical sensitivity in PSEN1 E280A carriers who are cognitively unimpaired. This task was adapted electronically from the Delayed Matching to Sample paradigm (DMS) previously validated in an adult population from Spain and Colombia.50 In this visual working memory and semantic processing task, examinees are presented with several photos of objects and are later presented with more photos and asked whether they had seen the presented object before. This adapted measure includes both semantically related and unrelated objects.50 In this visual working memory and semantic processing task, examinees are presented with several photos of objects and are later presented with more photos and asked whether they had seen the presented object before. This measure includes both semantically related and unrelated objects.50 Prior research indicates that in AD, semantic memory is one of the cognitive aspects affected early in the disease’s progression.34 Specifically, access to superordinate semantic structures, such as the category ‘toys,’ tends to remain intact, whereas subordinate semantic concepts, such as ‘blocks,’ ‘doll,’ and ‘action figure,’ are susceptible to disruption.51 Individuals with AD often struggle with forming semantic associations.52 Fox-Fuller et al. (2022) used the MESERO measure in a group of 83 individuals including 37 non-carrier cognitively healthy controls (mean age 36.7) and 46 PSEN1 E280A carriers (41 cognitively unimpaired and 5 meeting criteria for MCI). Cognitively unimpaired carriers’ mean age was 30.0, and for MCI participants was 47.6. They found that cognitively unimpaired AD carriers had worse MESERO total scores than non-carrier family members, with results driven by worse performance on semantically-unrelated object sets.53
MAPP Room Memory Test
In this computerized spatial memory test, participants are asked to carefully scan and view a household room containing 5–7 items for 10 s and are not prompted as to what objects they need to remember. Three object recognition trials follow, where participants are shown the same household room and are asked to identify the object they saw among foils of a similar category. They are then shown one object that was in the room and asked to respond whether they remember where this object was located (yes/no) and how confident they are of their memory for its location on a 1–5 ordinal scale (1 = Not Confident, 5 = Very Confident).54 Participants are then prompted to freely place the object in its correct location in the room with their cursor. This process repeats for all 10 rooms. Placement is counted as correct based on whether the center of the placed object is within a 50-pixel radius of the original target coordinates. Participants are shown the target objects again and must select in which room, of three options, the target object was located.54 For these same objects, they are then asked whether they remember the object’s location (yes/no) and how confident they are of their memory for location (1 = Not Confident, 5 = Very Confident). Participants again proceed to freely place the object in its original location in the target room. This process repeats for 5 rooms. There are immediate and delayed recall and object placement conditions.54 In a group of 31 non-carrier cognitively healthy controls with a mean age of 38.9 and 15 cognitively unimpaired carriers with a mean age of 39.0, carriers had poorer delayed room recognition recall than non-carrier healthy controls. These results suggest that performance in spatial memory may be helpful in discriminating those individuals at an increased risk of dementia.54
Language
The tests that were used the most to assess language in this group were fluency tasks from the CERAD protocol (both phonemic and semantic); the abbreviated 15-item BNT; the MINT; and the Boston Aphasia Examination, specifically the Cookie Theft Picture.55–57
Fluency
The neuropsychological fluency task is a cognitive assessment used to measure verbal fluency. In phonemic fluency, individuals are asked to generate as many words as possible that begin with a specified letter (e.g., F, A, S) within a limited time period, typically one minute. In semantic fluency, individuals are asked to generate as many words as possible that fit within a particular category (e.g., animals) within a limited time period, typically one minute.58 Results from fluency tasks in this population have provided mixed results. Fluency scores decline as the disease progresses and relates to pathology accumulation, but scores do not distinguish between cognitively unimpaired carriers and their non-carrier control counterparts. Aguirre-Acevedo et al. (2016) found that fluency tasks scores declined over two years in 493 cognitively unimpaired carriers with a mean age of 33.4 (SD = 11.7).21 Initial articles that described the neuropsychological outcomes of PSEN1 E280A mutation carriers that used measures of both semantic (e.g., animals) and phonemic (e.g., PMR) fluency found that they did not distinguish between cognitively unimpaired carriers and non-carrier healthy controls.27,59 In a sample of 40 cognitively unimpaired carriers and 82 non-carrier cognitively healthy controls (M age = 44, SD = 12) there was no difference in performance on fluency tasks.59 Additionally in a separate sample of 12 cognitively unimpaired carriers (M age = 49.6, SD = 4.9) 15 non-carrier cognitively healthy controls (M age = 45, SD = 7.2) there were also no differences in fluency task performance.27 More recent research has corroborated these findings, wherein cognitively unimpaired carriers and non-carrier cognitively healthy controls showed no differences on verbal fluency measures.42,60–62
Yucebas, Fox-Fuller et al. (2024) found no differences in overall score on fluency tasks in cognitively unimpaired carriers, but reported that higher levels of Aβ and tau proteins were associated with fewer items listed within clusters.31 Clustering is an a priori categorization of animals into six main clusters that have previously been found to be sensitive to early AD.63 The clusters are as follows: wild land animals, animals that live in the water, animals found on a farm, birds, pets (non-farm), and insects. The aggregate of these results indicates that verbal fluency tasks, although commonly used in neuropsychological evaluations, may not be particularly sensitive to early cognitive changes in this population.31
Naming
Naming tasks are widely used neuropsychological assessments designed to evaluate an individual’s word retrieval abilities and naming skills. During the test, individuals are presented with a series of drawings of objects and are asked to name each one.57 Some of the more commonly used tasks with this population are the BNT and MINT.57,64 In the earliest work on naming tasks in the PSEN1 E280A kindred, Tirado et al. (2008) examined differences in overall score and frequent mistakes on the CERAD abbreviated 15-item BNT and found that neither overall score nor types of mistakes made by participants differentiated non-carrier cognitively healthy controls (M age = 40.9, SD = 10.5) from cognitively unimpaired carriers (M age = 38.4, SD = 7.0) or cognitively impaired carriers (M age = 49.8, SD = 3.0).28 This finding was supported by subsequent studies of cognitive outcomes in a larger sample with the full-length BNT (i.e., 60 items), where no group differences were found.59 In a separate sample, there were no group differences in the overall scores for the MINT and BNT, despite these being longer naming tasks with more items, some less common than those in the shorter versions, and considered more sensitive to clinical changes.65 Recent work on sex differences in cognitive functioning between carriers and non-carrier cognitively healthy controls confirmed that the MINT naming task did not distinguish cognitively unimpaired carriers from controls or between sexes in both carriers and non-carriers.32
Semantic and Grammatical Variation in Language
Measuring semantic and grammatical variations in language can be done using a variety of tasks. The Cookie Theft Picture from the Boston Diagnostic Aphasia Examination was used in several of the studies to probe the onset of language deficits.56 In this task individuals are given a line drawing of a child stealing a cookie while his mother washes the dishes and other events occur. The picture should evoke basic key vocabulary learned in childhood with distinct characters, time, and situations. The individual is asked to explain the situation to the tester verbally. Semantic and grammatical variables are evaluated as well as errors in verbal output.56 Cognitively impaired carriers have been shown to consistently produce fewer semantic units, objective situations, and inferences when describing the situation, although there were no differences between cognitively unimpaired carriers and non-carrier cognitively healthy controls in number of errors produced.45,59,66 It is important to note that the scores provided in Ardila et al. (2000) and Lopera et al. (1997) did not provide specific scores related to semantic and grammatical variables as in the Cuetos et al. (2007) article, which specifically quantified semantic and grammatical variables in the Cookie Picture Theft test and Boston Diagnostic Aphasia Examination verbal output.45,59,66 More recent work examining semantic processing using the Batería IV Woodcock-Muñoz Verbal Analogies and Text Comprehension subtests with 13 cognitively unimpaired carriers (M age: 36.9, SD = 4.9), 7 cognitively impaired carriers (M age: 45, SD = 2.7), and 17 family non-carrier cognitively healthy controls (M age: 36, SD = 6.4) showed that cognitively unimpaired mutation carriers showed worse semantic processing as measured by verbal responses than non-carrier cognitively healthy controls and that greater Aβ burden was associated with worse performance on Verbal Analogies, a task that measures fluid verbal reasoning and language processing.67 These results indicate that tasks that specifically measure semantic language processing could be more sensitive in detecting earlier changes than the Boston Diagnostic Aphasia Examination that was previously used.67
Visuospatial Abilities
Visuospatial ability generally refers to the ability to comprehend and conceptualize visual representations and spatial relationships in learning and performing tasks such as reading maps, navigating mazes, conceptualizing objects in space from different perspectives, and executing various geometric operations. These tasks can vary in complexity and can involve drawing objects on paper or building structures, and can involve 2-D or 3-D objects.68 In this review, visuospatial abilities were measured using the CERAD Constructional Praxis.
CERAD-Constructional Praxis Measure
The CERAD Constructional Praxis test is adapted from Rosen’s assessment of constructional praxis, and tests the ability to copy four geometric forms of varying difficulty (i.e., circle, overlapping rectangles, diamond and cube).68 This measure was effective in detecting differences between 9 cognitively impaired PSEN1 E280A carriers (M age = 49.6, SD = 4.9) and 9 non-carrier cognitively healthy controls (M age 37.7, SD = 5.6),69 but was not sensitive to differences between cognitively unimpaired carriers and their healthy counterparts.23,32 Given that the CERAD figures that individuals are asked to reproduce are relatively simple, and that more complex tests such as the Rey–Osterrieth Complex Figure Task (ROCF) were also found to be ineffective at detecting early changes in cognitively unimpaired carriers, even more complex computerized visual tasks may be necessary to detect subtle changes in cognitively unimpaired carriers.
Attention, Executive Functioning (EF), and Abstract Reasoning
These cognitive domains were measured by Raven Matrices, Wisconsin Card Sorting Test, and Trail Making Test Part A. These measures again are not only limited to domains of attention, EF, and abstract reasoning, but were classified in this way in the articles reviewed.
Raven’s Matrices
On this measure of abstract reasoning, individuals are presented with visual geometric designs that are missing a piece and are asked to fill in the correct piece from up to 8 different choices.70 In a study by Roselli et al. (2010) 12 patients with ADAD (M age = 49.6 years, SD = 5.0), and 15 matched controls (M age = 45.0, SD = 7.2), cognitively impaired carriers’ scores declined faster than those of their healthy counterparts over a period of 18 months.27 Most studies have shown that there are no differences in performance between cognitively unimpaired carriers and healthy adults, suggesting that this test might not be sensitive enough to detect preclinical cognitive changes.9,27,32,59 Finally, there were no differences in performance between men and women in a sample of 167 cognitively unimpaired carriers and 75 non-carrier cognitively healthy controls with an age range of 30–53.32
Trail Making Task Part A (TMT-A)
This is a test of psychomotor speed. There are 25 randomly distributed circles numbered one to twenty-five on a sheet of paper.71 Individuals are timed and asked to connect numbers in ascending order, as quickly as possible. Overall, studies have not found differences in total time between healthy control adults and cognitively unimpaired carriers on the TMT-A.42,60 Studies by Arango Lasprilla et al. (2003) and Lopera et al. (1997) found that cognitively impaired carriers took longer to complete the test and made more errors than their non-carrier healthy counterparts.45,69 As this test may not be sensitive to preclinical changes in this population, in the future including TMT part B may be preferred, as it has been proven to be more sensitive to executive dysfunction.72 and may be able to distinguish between cognitively unimpaired carriers and healthy adults.
Wisconsin Card Sorting Test (WCST)
On this test of abstract reasoning and cognitive flexibility, and executive functioning, participants are presented stimulus cards one at a time and asked to match each card to one of four key cards differing in elements (i.e., number, shape, and color). Participants are not told how to match the cards, and instead must use the feedback provided by the tester (who tells them “correct” or “incorrect”) to ascertain the rule of categorization, which changes periodically. Participants must adapt to the changing rules.73 This test yields multiple scores, including: Sorting Test Categories: Represents the number of times a participant successfully sorts 10 consecutive cards correctly according to the specified sorting rule. It indicates the individual’s ability to learn and flexibly switch between different sorting rules or categories. Total Errors: Includes both perseverative errors and non-perseverative errors. Perseverative errors occur when an individual continues to sort cards based on a previously learned rule after the rule has changed. Non-perseverative errors are errors made when the sorting rule has changed, and the person does not immediately adapt. Conceptual Level Responses: the participant’s ability to understand and articulate the underlying principles governing the card sorting task. It measures the depth of cognitive understanding in adapting to new rules. Trials to Complete First Category: the number of trials it takes for the participant to complete their first category. It provides information about the individual’s initial ability to understand and adapt to the sorting rules. Failure to Maintain Set: the number of times the participant was unable to maintain the correct sorting rule over a series of trials, even if they initially understood it. Studies have shown that the number of preservative errors was higher for cognitively unimpaired carriers versus non-carriers, and number of categories score was higher in 30 healthy adults as compared to 22 cognitively impaired carriers, but there was no difference in scores between cognitively impaired carriers and 30 cognitively unimpaired carriers between the ages of 23–58 years of age.41,42,60
Subjective Cognitive Decline
Subjective cognitive decline (SCD), frequently focusing on memory complaints, is an important aspect of cognitive decline in AD. SCD measures are often completed by both the individual experiencing the memory changes and a family member or significant other who spends a significant amount of time with this individual. SCD in this review was most often measured by the Memory Complaint Scale, a 15-question measure that uses an ordinal scale from 0 (no complaints) to 3, indicating maximum complaints, for a total of up to 45.74
Norton et al. (2017) found when studying SCD that a sample of 26 cognitively unimpaired carriers (M age 37.2, SD = 6.5) reported more memory complaints than 26 non-carrier cognitively healthy controls (M age 35.6, SD = 7.7); however, informants did not report high levels of SCD.75 In another study, SCD complaints were more frequent with older age in a separate sample of 21 carriers with a M age of 35.7 (SD = 5.4) and 27 non-carrier cognitively healthy controls with a M age of 35.6 (SD = 5.2) and were found to be associated with higher Aβ levels in cognitively unimpaired carriers.76 Researchers found that cognitively unimpaired female carriers reported greater levels of SCD than cognitively unimpaired male carriers, and females had higher levels of informant SCD reports than males as well.26 Greater SCD was also associated with poorer verbal memory as measured by CERAD Word List Delayed Recall in a sample of 310 cognitively unimpaired carriers (M age 31.5, SD = 10.4) and 1998 non-carrier cognitively healthy controls (M age 27.5, SD = 8.8), suggesting that SCD can be an indicator of cognitive decline.26
Global Cognition
Global cognition was assessed using the MMSE. This is an 11-question measure that tests orientation, concentration, attention, verbal memory, naming and visuospatial skills.77 MMSE scores were generally lower in cognitively impaired carriers than non-carrier cognitively healthy controls and cognitively unimpaired carriers.11,23,78,79
Cognitive Composite
Several composite cognitive outcomes have been proposed and validated in the literature for assessing cognitive decline in individuals with ADAD. The CERAD Total Score, initially proposed by Aguirre-Acevedo et al. (2016), demonstrated adequate sensitivity and specificity for cognitively impaired carriers. This composite score encompasses scores on various neuropsychological assessments, including measures of verbal fluency, language, constructional praxis, memory, and orientation. Moreover, it exhibited sensitivity in detecting cognitive decline even two years after identification by the Word List Recall test.21 Another composite cognitive test score proposed by Ayutyanont et al. (2014), as part of the Alzheimer’s Prevention Initiative, combined measures of episodic memory, executive function, language, attention, and visuospatial ability, providing a comprehensive assessment of cognitive functioning, and was sensitive in detecting subtle cognitive changes associated with preclinical AD.80 Additionally, Guzmán et al. (2018) constructed a three-dimensional model based on structural and confirmatory factor analysis, which discriminated between carriers and non-carriers and detected cognitive decline cross-sectionally. These dimensions included verbal memory, visuospatial memory, and executive functioning, serving as composite outcomes for assessing cognitive functioning in ADAD individuals. These composite outcomes offer valuable tools for tracking cognitive changes.60
DISCUSSION
This review synthesized the existing literature on neuropsychological assessments in the world’s largest kindred with ADAD due to PSEN1 E280A mutation throughout their lifespan and provides a comprehensive overview of cognitive outcomes in this population. Carriers of the PSEN1 E280A mutation allow researchers a unique opportunity to assess cognitive changes in ADAD across the lifespan, including during cognitively unimpaired stages of this disease. PSEN1 E280A mutation carriers are genetically determined to develop early onset AD with almost 100% certainty, and they have a well-characterized disease course and clinical profile, with MCI occurring at a median age of 44 years and dementia at 49 years.9,17 PSEN1 E280A produces Aβ deposition, hippocampal neuron loss, and tau accumulation with Aβ plaque deposition surfacing about a decade before the clinical onset of AD. This is followed by decreased cerebral perfusion and glucose metabolism in brain regions impacted by cortical Aβ deposition, suggesting a potential connection between cortical Aβ and decreased parietal, frontal, and temporal metabolic activity in preclinical ADAD.81–83 Pathophysiological and cognitive changes in ADAD are similar to sporadic AD, and findings from research on PSEN1 E280A carriers can be helpful in understanding disease trajectory in individuals with sporadic AD.17 Research on the Colombian kindred has included participants as young as nine years of age10,62 to individuals up to their 70 s, and provides an opportunity to examine the progression of the disease over the lifespan, as well as to develop and test measures that may identify early and subtle cognitive changes in people in the preclinical stage of AD.
Through this review we were able to identify which cognitive measures were effective in detecting differences in cognition between carriers of the PSEN1 E280A mutation and non-carrier cognitively healthy controls, and which ones differentiated between cognitively unimpaired carriers and non-carrier healthy controls. Findings across studies consistently showed that the measures of memory were the most effective at differentiating between cognitively unimpaired and cognitively impaired carriers, including the CERAD Word List Learning, FCSRT, LAS-FNAME, and the newly-developed tests related to semantic and spatial memory, MESERO and the MAPP Room Memory Task.49,53,54 The integration of diverse composite cognitive measures also provides valuable insights into tracking cognitive changes in ADAD. Additionally, many other tests that measured neuropsychological functioning (CERAD Delayed Word Recall, CERAD Constructional Praxis, Verbal Fluency, Raven Matrices, and MMSE) were effective at tracking clinical changes over time in mutation carriers versus non-carrier healthy controls, which is important for monitoring cognitive decline in AD.27 This information is valuable as it provides a starting point as to how and when these cognitive measures detect earliest cognitive changes in this population (Fig. 2). The findings can be used in the future to develop more precise measures that might be able to detect more subtle changes earlier in disease progression.
Fig. 2.

Cognitive tests most effective in identifying earliest changes of ADAD.
Future work is needed particularly for measures examining executive function, as the measures currently being used do not capture differences at the preclinical stages. This is important as executive function (EF) has been shown to be a precursor to episodic memory problems later in the disease progression.84 EF is a complex cognitive domain and there may be additional neuropsychological tests that have not yet been examined in carriers versus non-carriers that assess certain aspects of EF, such as color-word interference tasks (Stroop) or tasks of sustained attention (e.g., continuous performance task). Since executive function deficits typically occur before or at the same time as memory problems, it is likely that more precise measures are required to reveal the earliest changes in executive function within this group.53,85 It is also a possibility that executive disfunction is more specific to sporadic AD when individuals tend to be older at clinical symptom onset; perhaps given the younger age of the cohort with ADAD, executive dysfunction is not as apparent in this population regardless of the cognitive tests administered to measure this domain.
Relatedly, more research is needed focusing on children (ages 8–17) to track neurodevelopmental changes in PSEN1 E280A carriers and to examine whether the trajectory of cognitive performance in childhood/adolescence is different between carriers and non-carrier healthy controls, with implications of such results for later disease progression. Understanding the earliest cognitive signs of ADAD in childhood and adolescence will allow us to develop prevention research aimed at enhancing early life cognitive and educational experiences of ADAD cohort members.
This review underscores the importance of tailored assessments in clinical practice to enable comprehensive evaluation of cognitive changes over time. The expansion of clinical assessment tools to include more challenging and precise measures, such as the computerized tasks developed by our group (e.g., MAPP Room Memory Task, MESERO) offers the opportunity for a nuanced understanding of early disease progression, including preclinical stages.. By implementing such tests, clinicians may significantly improve early detection, monitoring, and intervention not only for ADAD but also for sporadic AD.
Limitations
Given that all articles included in this review paper focused on the same population, it is very difficult to distinguish how many distinct individuals are in any one sample. It is likely that there were individuals who participated in more than one study cited in this review. Further, future research would need to determine if some of these measures that are sensitive to familial AD are indeed useful in diagnosis of sporadic AD and other forms of dementia as well, for example the MAPP Room Memory Task developed specifically with ADAD participants.54
It is also crucial to acknowledge the cultural influences affecting outcomes on neuropsychological tests. Although most of the tests used were normed and validated to use with this specific population, it is important to address cultural biases in neuropsychological assessment to yield the best outcomes in these measures. There is a need for ongoing development and validation of new neuropsychological measures that are culturally sensitive and inclusive, ensuring accurate and equitable assessment across diverse populations.86
It would also be useful to examine cognitive differences between groups of PSEN1 E280A carriers and other familial dementia cohorts, specifically, the Dominantly Inherited Alzheimer Network (DIAN) and Longitudinal Early-Onset Alzheimer’s Disease Study (LEADS) cohorts, to determine if cognitive tests that were useful in identifying pre-clinical changes in PSEN1 E280A carriers are also clinically useful and show similar patterns in other cohorts.
Conclusions
This review provides an overview of the cognitive outcomes in children and adults who are carriers of the PSEN1 E280A mutation. We found that measures of verbal, semantic, episodic, and spatial memory were the most effective in identifying pre-clinical cognitive differences between this population and cognitively healthy adults. Our findings identify which current measures are more precise in detecting clinical changes in PSEN1 E280A carriers and indicate areas where further work is needed to develop measures capable of detecting more subtle changes in cognitively unimpaired carriers.
As highlighted throughout this review, many standard neuropsychological measures lack the sensitivity to reliably identify cognitively unimpaired mutation carriers in cross-sectional studies. This reveals a compelling need within the field for the development of more challenging and precise cognitive assessments. Such advanced tools are essential for the early detection of subtle cognitive dysfunctions in this population and for monitoring cognitive trajectories before overt clinical symptoms arise. Addressing this gap could significantly enhance our ability to intervene at earlier stages of neurodegenerative diseases, potentially improving patient outcomes. Additionally, continued development of tasks assessing other domains, such as executive function, and creating more sensitive measures for children, are needed to effectively identify preclinical markers of familial AD.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank the PSEN1 Colombian families for contributing their valuable time and effort, without which this study would not have been possible. We thank the research staff of the Group of Neuroscience of Antioquia for their help coordinating study visits to Boston.
FUNDING
YTQ was supported by the US National Institute on Aging (NIA) (grants no. R01 AG054671, RF1AG077627), the MGH Executive Committee on Research (MGH Research Scholar Award), and the Alzheimer’s Association. AG was supported by US National Institute on Neurological Disorders and Stroke (NINDS) (grant no. 1F31NS134277-01A1).
Footnotes
CONFLICT OF INTEREST
Dr. Quiroz serves as consultant for Biogen. All other authors have no conflict of interest to report.
SUPPLEMENTARY MATERIAL
The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JAD-240360.
DATA AVAILABILITY
The data supporting the findings of this particular study are not publicly available due to privacy concerns, but they can be accessed from the corresponding author upon reasonable request.
REFERENCES
- 1.2020 Alzheimer’s disease facts and figures. Alzheimers Dement 2020; 16: 391–460. [DOI] [PubMed] [Google Scholar]
- 2.Corey-Bloom J The ABC of Alzheimer’s disease: cognitive changes and their management in Alzheimer’s disease and related dementias. Int Psychogeriatr 2002; 14(Suppl 1): 51–75. [DOI] [PubMed] [Google Scholar]
- 3.Murman DL. The impact of age on cognition. Semin Hear 2015; 36: 111–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schindler SE, Fagan AM. Autosomal dominant Alzheimer disease: a unique resource to study CSF biomarker changes in preclinical AD. Front Neurol 2015; 6: 142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.PSEN1 E280A (Paisa), ALZFORUM, https://www.alzforum.org/mutations/psen1-e280a-paisa (accessed 8 October 2022).
- 6.Bateman RJ, Aisen PS, De Strooper B, et al. Autosomal-dominant Alzheimer’s disease: a review and proposal for the prevention of Alzheimer’s disease. Alzheimers Res Ther 2010; 3: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lopera F, Madrigal L, Kosik KS, et al. Demencia tipo Alzheimer con agregación familiar en Antioquia, Colombia. Acta Neurol Colomb 1994; 10: 173–187. [Google Scholar]
- 8.Quiroz YT, Schultz A, Chen K, et al. Brain imaging and blood biomarker abnormalities in children with autosomal-dominant Alzheimer’s disease: A cross-sectional Study. JAMA Neurol 2015; 72: 912–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acosta-Baena N, Sepulveda-Falla D, Lopera-Gómez CM, et al. Pre-dementia clinical stages in presenilin 1 E280A familial early-onset Alzheimer’s disease: a retrospective cohort study. Lancet Neurol 2011; 10: 213–220. [DOI] [PubMed] [Google Scholar]
- 10.Fox-Fuller JT, Artola A, Chen K, et al. Sex differences in cognitive abilities among children with the autosomal dominant Alzheimer disease presenilin 1 E280A variant from a Colombian cohort. JAMA Netw Open 2021; 4: e2121697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bobes MA, García YF, Lopera F, et al. ERP generator anomalies in presymptomatic carriers of the Alzheimer’s disease E280A PS-1 mutation. Hum Brain Mapp 2010; 31: 247–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guzmán-Vélez E, Zetterberg H, Fox-Fuller JT, et al. Associations between plasma neurofilament light, in vivo brain pathology and cognition in non-demented individuals with autosomal-dominant Alzheimer’s disease. Alzheimers Dement 2021; 17: 813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wechsler D Wechsler Intelligence Scale for Children. 4th, Spani ed. San Antonio: The Psychological Corporation, 2005. [Google Scholar]
- 14.Wechsler D, Padilla Sierra G. WISC-IV: escala Wechsler de inteligencia para niños-IV. México, D.F.: EL Manual Moderno, 2007. [Google Scholar]
- 15.Lopera F, Marino C, Chandrahas AS, et al. Resilience to autosomal dominant Alzheimer’s disease in a Reelin-COLBOS heterozygous man. Nat Med 2023; 29: 1243–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arboleda-Velasquez JF, Lopera F, O’Hare M, et al. Resistance to autosomal dominant Alzheimer’s disease in an APOE3 Christchurch homozygote: a case report. Nat Med 2019; 25: 1680–1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fuller JT, Cronin-Golomb A, Gatchel JR, et al. Biological and cognitive markers of presenilin1 E280A autosomal dominant Alzheimer’s disease: a comprehensive review of the Colombian kindred. J Prev Alzheimers Dis 2019; 6: 112–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morris JC, Heyman A, Mohs RC, et al. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part I. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology 1989; 39: 1159–1165. [DOI] [PubMed] [Google Scholar]
- 19.Welsh KA, Butters N, Mohs RC, et al. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part V. A normative study of the neuropsychological battery. Neurology 1994; 44: 609–614. [DOI] [PubMed] [Google Scholar]
- 20.Aguirre-Acevedo DC, Gómez RD, Moreno S, et al. Validez y fiabilidad de la batería neuropsicológica CERAD-Col. Rev Neurol Ed Impr 2007; 655–660. [PubMed] [Google Scholar]
- 21.Aguirre-Acevedo DC, Lopera F, Henao E, et al. Cognitive decline in a Colombian kindred with autosomal dominant Alzheimer disease: a retrospective cohort study. JAMA Neurol 2016; 73: 431–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baena A, Bocanegra Y, Torres V, et al. Neuroticism is associated with tau pathology in cognitively unimpaired individuals with autosomal dominant Alzheimer’s disease. J Alzheimers Dis 2021; 82: 1809–1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rios-Romenets S, Lopera F, Sink KM, et al. Baseline demographic, clinical, and cognitive characteristics of the Alzheimer’s Prevention Initiative (API) Autosomal-Dominant Alzheimer’s Disease Colombia Trial. Alzheimers Dement 2020; 16: 1023–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vannini P, Hanseeuw BJ, Gatchel JR, et al. Trajectory of unawareness of memory decline in individuals with autosomal dominant Alzheimer disease. JAMA Netw Open 2020; 3: e2027472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vila-Castelar C, Papp KV, Amariglio RE, et al. Validation of the latin American spanish version of the face-name associative memory exam in a colombian sample. Clin Neuropsychol 2020; 34(sup1): 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martinez JE, Delgado EP, Guzmán-Vélez E, et al. Subjective cognitive decline and its relation to verbal memory and sex in cognitively unimpaired individuals from a Colombian cohort with autosomal dominant Alzheimer’s disease. J Int Neuropsychol Soc 2022; 28: 541–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosselli M, Ardila A, Moreno S, et al. Cognitive decline in patients with familial Alzheimer’s disease associated with E280a presenilin-1 mutation: a longitudinal study. J Clin Exp Neuropsychol 2000; 22: 483–495. [DOI] [PubMed] [Google Scholar]
- 28.Tirado V, Motta M, Aguirre-Acevedo DC, et al. Analysis of intrusive errors in a memory test as possible pre-clinical marker of familial Alzheimer disease, in E280A presenilin-1 mutation carrier. Rev Neurol 2008; 47: 290–294. [PubMed] [Google Scholar]
- 29.Buschke H Selective reminding for analysis of memory and learning. J Verbal Learn Verbal Behav 1973; 12: 543–550. [Google Scholar]
- 30.Grober E, Lipton RB, Hall C, et al. Memory impairment on free and cued selective reminding predicts dementia. Neurology 2000; 54: 827–832. [DOI] [PubMed] [Google Scholar]
- 31.Yucebas D, Fox-Fuller JT, Cabrera AB, et al. Associations of category fluency clustering performance with in vivo brain pathology in autosomal dominant Alzheimer’s disease. J Int Neuropsychol Soc 2024; 30: 77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vila-Castelar C, Tariot PN, Sink KM, et al. Sex differences in cognitive resilience in preclinical autosomal-dominant Alzheimer’s disease carriers and non-carriers: Baseline findings from the API ADAD Colombia Trial. Alzheimers Dement 2022; 18: 2272–2282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arango-Lasprilla JC, Cuetos F, Valencia C, et al. Cognitive changes in the preclinical phase of familial Alzheimer’s disease. J Clin Exp Neuropsychol 2007; 29: 892–900. [DOI] [PubMed] [Google Scholar]
- 34.Vogel A, Gade A, Stokholm J, et al. Semantic memory impairment in the earliest phases of Alzheimer’s disease. Dement Geriatr Cogn Disord 2005; 19: 75–81. [DOI] [PubMed] [Google Scholar]
- 35.Estévez-González A, García-Sánchez C, Boltes A, et al. Semantic knowledge of famous people in mild cognitive impairment and progression to Alzheimer’s disease. Dement Geriatr Cogn Disord 2004; 17: 188–195. [DOI] [PubMed] [Google Scholar]
- 36.Vogel EK, Woodman GF and Luck SJ. Storage of features, conjunctions and objects in visual working memory. J Exp Psychol Hum Percept Perform 2001; 27: 92–114. [DOI] [PubMed] [Google Scholar]
- 37.Treisman A Object Tokens, binding and visual memory. In: Zimmer H, Mecklinger A, Lindenberger U (eds) Hand-book of Binding and Memory: Perspectives From Cognitive Neuroscience. Oxford University Press, 2006, pp. 315–338. [Google Scholar]
- 38.Brockmole JR, Parra MA, Della Sala S, et al. Do binding deficits account for age-related decline in visual working memory? Psychon Bull Rev 2008; 15: 543–547. [DOI] [PubMed] [Google Scholar]
- 39.Koppara A, Frommann I, Polcher A, et al. Feature binding deficits in subjective cognitive decline and in mild cognitive impairment. J Alzheimers Dis 2015; 48(Suppl 1): S161–S170. [DOI] [PubMed] [Google Scholar]
- 40.Parra MA, Abrahams S, Fabi K, et al. Short-term memory binding deficits in Alzheimer’s disease. Brain 2009; 132: 1057–1066. [DOI] [PubMed] [Google Scholar]
- 41.Parra MA, Saarimäki H, Bastin ME, et al. Memory binding and white matter integrity in familial Alzheimer’s disease. Brain 2015; 138: 1355–1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Parra MA, Abrahams S, Logie RH, et al. Visual short-term memory binding deficits in familial Alzheimer’s disease. Brain 2010; 133: 2702–2713. [DOI] [PubMed] [Google Scholar]
- 43.Norton DJ, Parra MA, Sperling RA, et al. Visual short-term memory relates to tau and amyloid burdens in preclinical autosomal dominant Alzheimer’s disease. Alzheimers Res Ther 2020; 12: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rey A and Osterrieth PA. Rey-Osterrieth Complex Figure Copying Test. APA PsycTests, 1941. [Google Scholar]
- 45.Lopera F, Ardilla A, Martínez A, et al. Clinical features of early-onset Alzheimer disease in a large kindred with an E280A presenilin-1 mutation. JAMA 1997; 277: 793–799. [PubMed] [Google Scholar]
- 46.Bocanegra Y, Fox-Fuller JT, Baena A, et al. Association between visual memory and in vivo amyloid and tau pathology in preclinical autosomal dominant Alzheimer’s disease. J Int Neuropsychol Soc 2021; 27: 47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Papp KV, Amariglio RE, Dekhtyar M, et al. Development of a psychometrically equivalent short form of the Face-Name Associative Memory Exam for use along the early Alzheimer’s disease trajectory. Clin Neuropsychol 2014; 28: 771–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rentz DM, Amariglio RE, Becker JA, et al. Face-name associative memory performance is related to amyloid burden in normal elderly. Neuropsychologia 2011; 49: 2776–2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vila-Castelar C, Muñoz N, Papp KV, et al. The Latin American Spanish version of the Face-Name Associative Memory Exam is sensitive to cognitive and pathological changes in preclinical autosomal dominant Alzheimer’s disease. Alzheimers Res Ther 2020; 12: 104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.García-Magariño I, Fox-Fuller JT, Palacios-Navarro G, et al. Visual working memory for semantically related objects in healthy adults. Rev Neurol 2020; 71: 277–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Giffard B The nature of semantic memory deficits in Alzheimer’s disease: New insights from hyperpriming effects. Brain 2001; 124: 1522–1532. [DOI] [PubMed] [Google Scholar]
- 52.Di Giacomo D, De Federicis LS, Pistelli M, et al. The loss of conceptual associations in mild Alzheimer’s dementia. J Clin Exp Neuropsychol 2012; 34: 643–653. [DOI] [PubMed] [Google Scholar]
- 53.Fox-Fuller JT, Martinez JE, Baena A, et al. Memory for semantically related objects differentiates cognitively unimpaired autosomal dominant mutation carriers from non-carrier family members. J Prev Alzheimers Dis 2023; 10: 322–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Giudicessi A, Aduen PA, Fox-Fuller JT, et al. The MAPP Room Memory Test: Examining contextual memory using a novel computerized test in cognitively-unimpaired individuals with autosomal dominant Alzheimer’s disease. J Prev Alzheimers Dis 2024; 11: 463–468. [DOI] [PubMed] [Google Scholar]
- 55.Gollan TH, Weissberger GH, Runnqvist E, et al. Self-ratings of spoken language dominance: A Multi-Lingual Naming Test (MINT) and preliminary norms for young and aging Spanish-English Bilinguals. Biling (Camb Engl) 2012; 15: 594–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Goodglass H, Kaplan E and Barresi B. The Boston Diagnostic Aphasia Examination: BDAE-3 long form kit. 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2001. [Google Scholar]
- 57.Kaplan E, Goodglass H and Weintraub S. Boston naming test. Philadelphia: Lea & Febiger, 1983. [Google Scholar]
- 58.Strauss E, Sherman EMS and Spreen O. A compendium of neuropsychological tests: Administration, norms, and commentary, 3rd ed. New York: Oxford University Press, 2006. [Google Scholar]
- 59.Ardila A, Lopera F, Rosselli M, et al. Neuropsychological profile of a large kindred with familial Alzheimer’s disease caused by the E280A single presenilin-1 mutation. Arch Clin Neuropsychol 2000; 15: 515–528. [PubMed] [Google Scholar]
- 60.Guzmán-Vélez E, Jaimes S, Aguirre-Acevedo DC, et al. A three-factor structure of cognitive functioning among unimpaired carriers and non-carriers of autosomal-dominant Alzheimer’s disease. J Alzheimers Dis 2018; 65: 107–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Quiroz YT, Budson AE, Celone K, et al. Hippocampal hyperactivation in presymptomatic familial Alzheimer’s disease. Ann Neurol 2010; 68: 865–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Quiroz YT, Willment KC, Castrillon G, et al. Successful scene encoding in presymptomatic early-onset Alzheimer’s disease. J Alzheimers Dis 2015; 47: 955–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Fagundo AB, López S, Romero M, et al. Clustering and switching in semantic fluency: predictors of the development of Alzheimer’s disease. Int J Geriatr Psychiatry 2008; 23: 1007–1013. [DOI] [PubMed] [Google Scholar]
- 64.Stasenko A, Jacobs DM, Salmon DP, et al. The Multilingual Naming Test (MINT) as a measure of picture naming ability in Alzheimer’s disease. J Int Neuropsychol Soc 2019; 25: 821–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Katsumata Y, Mathews M, Abner EL, et al. Assessing the discriminant ability, reliability, and comparability of multiple short forms of the Boston Naming Test in an Alzheimer’s disease center cohort. Dement Geriatr Cogn Disord 2015; 39: 215–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cuetos F, Arango-Lasprilla JC, Uribe C, et al. Linguistic changes in verbal expression: a preclinical marker of Alzheimer’s disease. J Int Neuropsychol Soc 2007; 13: 433–439. [DOI] [PubMed] [Google Scholar]
- 67.Ortiz SO, Ortiz JA and Devine RI. Chapter 12 - Assessment of culturally and linguistically diverse individuals with the Woodcock–Johnson IV. In: Flanagan DP, Alfonso VC (eds) WJ IV Clinical Use and Interpretation. San Diego: Academic Press, pp. 317–353. [Google Scholar]
- 68.Benton AL, Fogel ML. Three-dimensional constructional praxis: a clinical test. Arch Neurol 1962; 7: 347–354. [DOI] [PubMed] [Google Scholar]
- 69.Arango Lasprilla JC, Iglesias J, Lopera F. Neuropsychological study of familial Alzheimer’s disease caused by mutation E280A in the presenilin 1 gene. Am J Alzheimers Dis Other Demen 2003; 18: 137–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Raven JC. Raven’s progressive matrices. Melbourne: Australian Council for Educational Research, 1938. [Google Scholar]
- 71.Reitan RM. Validity of the Trail Making Test as an indicator of organic brain damage. Percept Mot Skills 1958; 8: 271–276. [Google Scholar]
- 72.O’Donnell JP, Macgregor LA, Dabrowski JJ, et al. Construct validity of neuropsychological tests of conceptual and attentional abilities. J Clin Psychol 1994; 50: 596–600. [DOI] [PubMed] [Google Scholar]
- 73.Heaton RK, Chelune GJ, Talley JL, et al. Wisconsin Card Sorting Test (WCST). Revised and expanded. Odessa, FL: Psychological Assessment Resources, 1993. [Google Scholar]
- 74.Vale FAC, Balieiro-Jr AP and Silva-Filho JH. Memory complaint scale (MCS). Proposed tool for active systematic search. Dement Neuropsychol 2012; 6: 212–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Norton DJ, Amariglio R, Protas H, et al. Subjective memory complaints in preclinical autosomal dominant Alzheimer disease. Neurology 2017; 89: 1464–1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gatchel JR, Lopera F, Norton DJ, et al. Association of subjective cognitive decline with markers of brain pathology in preclinical autosomal dominant Alzheimer’s disease. J Neurol Neurosurg Psychiatry 2020; 91: 330–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Folstein MF, Folstein SE and McHugh PR. Mini-Mental State Examination (MMS, MMSE). APA PsycTests, 1975. [Google Scholar]
- 78.Guzmán-Vélez E, Martínez J, Papp K, et al. Associative memory and in vivo brain pathology in asymptomatic presenilin-1 E280A carriers. Neurology 2020; 95: e1312–e1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Quiroz YT, Ally BA, Celone K, et al. Event-related potential markers of brain changes in preclinical familial Alzheimer disease. Neurology 2011; 77: 469–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ayutyanont N, Langbaum JBS, Hendrix SB, et al. The Alzheimer’s Prevention Initiative Composite Cognitive Test Score: sample size estimates for the evaluation of preclinical Alzheimer’s disease treatments in presenilin 1 E280A mutation carriers. J Clin Psychiatry 2014; 75: 652–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lemere CA, Lopera F, Kosik KS, et al. The E280A presenilin 1 Alzheimer mutation produces increased A beta 42 deposition and severe cerebellar pathology. Nat Med 1996; 2: 1146–1150. [DOI] [PubMed] [Google Scholar]
- 82.Velez-Pardo C, Arellano JI, Cardona-Gomez P, et al. CA1 hippocampal neuronal loss in familial Alzheimer’s disease presenilin-1 E280A mutation is related to epilepsy. Epilep-sia 2004; 45: 751–756. [DOI] [PubMed] [Google Scholar]
- 83.Quiroz YT, Sperling RA, Norton DJ, et al. Association between amyloid and tau accumulation in young adults with autosomal dominant Alzheimer disease. JAMA Neurol 2018; 75: 548–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Silverberg NB, Ryan LM, Carrillo MC, et al. Assessment of cognition in early dementia. Alzheimers Dement 2011; 7: e60–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Medina LD, Woo E, Rodriguez-Agudelo Y, et al. Reaction time and response inhibition in autosomal dominant Alzheimer’s disease. Brain Cogn 2021; 147: 105656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mindt MR, Byrd D, Saez P, et al. Increasing culturally competent neuropsychological services for ethnic minority populations: a call to action. Clin Neuropsychol 2010; 24: 429–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Parra MA, Abrahams S, Logie RH, et al. Visual short-term memory binding deficits in familial Alzheimer’s disease. Brain 2010; 133: 2702–2713. [DOI] [PubMed] [Google Scholar]
- 88.Tirado V, Muñoz C, Aguirre C, et al. Performance of carriers and non-carriers of the E280A mutation for familial Alzheimer’s disease in a naming test. Rev Neurol 2004; 39: 322–326. [PubMed] [Google Scholar]
- 89.Vila-Castelar C, Guzmán-Vélez E, Pardilla-Delgado E, et al. Examining sex differences in markers of cognition and neurodegeneration in autosomal dominant Alzheimer’s disease: preliminary findings from the Colombian Alzheimer’s Prevention Initiative Biomarker Study. J Alzheimers Dis 2020; 77: 1743–1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting the findings of this particular study are not publicly available due to privacy concerns, but they can be accessed from the corresponding author upon reasonable request.


