Abstract
Background
In rural Nepal, poor road and transport networks and few testing laboratories impede tuberculosis diagnosis. A drone transport system was established to transport sputum samples to laboratories with advanced molecular diagnostic machines – GeneXpert MTB/RIF. This study explored the perceptions of using drones for tuberculosis diagnosis among community stakeholders, female community health volunteers, and healthcare providers from communities with drones implemented and without drone programs.
Methods
In December 2019, we conducted focus group discussions in two drone-implemented and three without drone programs. We purposively selected 40 participants: Female community health volunteers (n=16), community stakeholders (n=18), and healthcare providers (n=6). Focus group discussions employed semi-structured questions, which were audio-recorded, transcribed, and translated into English. Codebook thematic analysis was performed and charted using three levels of the socioecological model: individual, community, and health system.
Results
We identified four themes (i) Trust in drones underpins successful use for tuberculosis diagnosis; (ii) Drone-based sample transport optimised connectivity and accessibility for people with tuberculosis and healthcare providers; (iii) Drones create opportunities to improve community and health system, and (iv) External factors impede the use of drones to facilitate tuberculosis diagnosis. The study reported, at an individual level, people’s trust in drones mainly through community-based events. For local healthcare providers, drones reduce transport time, opportunity costs, and immediate cash costs of transport. At the community level, drone use creates opportunities to increase the skills of local people as drone pilots. At the health system level, drone transport increases efficient sputum sample delivery and provides opportunities to transport medicines and other biomedical samples. Perceived challenges of using drones were adverse weather, limitations in skilled human resources, and financial resources to operate drones sustainably.
Conclusions
Healthcare providers, female community health volunteers, and community stakeholders reported high levels of trust in drones and perceived their use for tuberculosis diagnosis and care to substantially benefit people with tuberculosis and providers in rural Nepal. There was a high level of demand for application to other healthcare services and wider geographical coverage, demonstrating drones as a potential tool for enhancing access to healthcare in geographically remote communities.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-024-11824-0.
Keywords: Tuberculosis, Drone, GeneXpert MTB/RIF, Active case finding, Nepal
Background
Tuberculosis (TB), despite being a preventable and curable disease, kills 1.4 million people every year [1]. In 2021, the World Health Organization (WHO) reported that of the estimated 10.6 million people who developed TB, only 7.1 million were diagnosed by the national TB programs (NTP) [1]. Approximately 80% of this mortality and morbidity occurs among people from low- and middle-income countries (LMICs) due to a myriad of factors including remote geographical terrain and poor road networks, wide use of insensitive diagnostic tools for TB, centralized laboratory services, and inadequate knowledge of TB [1]. All these conditions hinder access to health centres and timely diagnosis of TB [2–4]. Undiagnosed TB cases or incomplete treatment contribute to increased transmission, resistance to drugs, catastrophic costs, mortality and chronic ill-health [5–7]. Therefore, locally appropriate, innovative, and comprehensive multidisciplinary strategies are needed to address these barriers and achieve the goals of the END TB plan by 2030 [8].
Drones, or uncrewed aerial vehicles, are increasingly used in environmental science, emergency response, disaster management, and health to overcome logistic impediments and deliver services in geographically remote areas [9]. Drones have been tested to deliver medicine and vaccines in emergencies and in geographically challenging terrains to improve health care. They are also used in the transfer of biomedical samples to improve disease diagnosis and to map vectors to identify possible disease transmission and prevent it [10–12]. Drones can reduce the time for healthcare access and delivery as well as healthcare costs both for patients and the health system [13, 14]. They are a potentially efficient technology to deliver services and improve access to healthcare [10, 15].
In Nepal, a lower-middle-income country in South Asia, TB is a major public health problem and the seventh leading cause of death. Every year approximately 69,000 Nepali people develop active TB but less than 50% are diagnosed through the NTP [16]. The NTP system largely relies on passive case finding, in which people who experience TB symptoms self-present at health centers to be assessed and diagnosed with the disease. This approach is a barrier to accessing health services, resulting in delayed diagnosis, particularly for people living in rural areas [4, 17–19]. Delays of 40–60 days for TB diagnosis for people living in rural Nepal [20, 21] impose a significant financial burden of diagnostic, treatment costs and poor health outcomes for people with TB and their families and also amplify negative social consequences such as stigma, and poor mental health conditions such as anxiety and depression [4, 22–24]. To address these challenges and accelerate the diagnosis of TB, the WHO Global TB Programme recommends intensified research and innovation through the integration of digital health technologies into TB prevention, diagnosis, and management to reach END TB targets [25, 26]. One such technology is drone transport systems.
In Nepal, drones have been widely used for personal or professional photographs and videography but also their uses in agriculture, geographical mapping, conservation and health care are increasing. Following the 2015 Gorkha earthquake, drones have been extensively used for damage assessment, mapping of humanitarian crises, and search and rescue operations [27]. However, the use of drones in healthcare is limited, yet increasingly being explored. Thapa (2021) conducted a feasibility study showing that cargo drones, capable of carrying up to 12 kg, were successful in test flights to deliver COVID-19 vaccines in the remote Humla district. The report concluded that drones could be an effective tool to safely transport vaccines, save time and reduce transportation costs [28]. Similarly, Berninzon and Vongasemjit discussed the potential benefits of drones for vaccine delivery and saving children’s lives in rural communities in Nepal [29]. However, despite the broad potential, the implementation of drones for healthcare delivery in remote rural Nepal is in its infancy.
TB programmes have tested using drones in remote geographical environments in Nepal, Papua New Guinea, Madagascar, and Malawi to transport sputum samples for TB tests [11, 15, 30]. In Nepal, Birat Nepal Medical Trust (BNMT), a national non-government organization working on TB with over 50 years of experience in Nepal, piloted the use of drones to improve TB diagnosis by transporting sputum samples [31]. The use of drones was integrated within its community-based active TB case-finding programme. Utilizing drones in TB diagnosis and treatment may potentially minimize opportunity costs associated with transportation and time for both people with TB and healthcare providers and thus contribute to improved person-centered TB care and equity of access for people in rural communities.
The use of unauthorized drones in Nepal over restricted heritage sites and security-sensitive areas prompted the government to rapidly implement strict flight procedural guidelines for drone operations [32]. Drones are restricted in populated zones and areas notified by local, state, or federal governments. Additionally, operations within 5 km of aerodromes, over emergency service operations, or in controlled airspace require special permissions. Drones are classified by maximum take-off weight into four categories: very low risk (under 250 gm), low risk (250 gm to 2 kg), regulated low risk (2 kg to 25 kg), and regulated high risk (above 25 kg) and those weighing more than 25 kg are not permitted for operation [33].
Furthermore, despite the documented advantages of using drones, initial applications within military and surveillance programs as well as their misuse for privacy invasion have raised concerns about safety and privacy [10, 11]. The World Health Organisation (WHO) guidance on ‘Ethics and governance of artificial intelligence for health’ recommends that the successful application of artificial intelligence technologies such as drones and computer-aided detection for TB diagnosis requires an understanding of users and providers’ perspectives on acceptability, respecting their rights and autonomy to decide on health choices and providing context-specific information to stakeholders [34]. Therefore, to launch a new technology such as drones in communities, people’s trust is crucial to success [35–37]. Programs should engage with local contexts in close consultation with community members before, during, and after project implementation to ensure the program aligns with local needs and expectations [38, 39].
This study explored community stakeholders’, Female Community Health Volunteers (FCHVs), and healthcare providers’ perceptions towards using drones for TB diagnosis in communities with (drone experienced) and without (drone-naïve) drone operation [11, 14, 36].
Methods
Study design
We conducted an exploratory descriptive qualitative study using semi-structured focus group discussions (FGD) to explore the perception of community stakeholders, FCHVs, and healthcare providers of using drones for TB diagnosis in the Pyuthan district of Nepal. This design is suitable for the study as it enabled us to explore the perceptions of drone and TB stakeholders within the context of Nepal and permitted the description of similar or contrasting viewpoints held by the participants [40]. We used the COnsolidated criteria for REporting Qualitative research (COREQ) Checklist to report the study (Additional file I) [41].
Conceptual framework
The study used the socioecological framework to explore the perception of using drones in TB diagnosis at three levels: (a) individual level: related to or having an impact at individual (b) community level: related to interactions, relationships, and engagement with community people as well as the geographical context of that area, and (c) health system level: related to or impact on broader health system diagnosis and care [42]. The framework enables us to improve our understanding of the multi-level perspectives of using drones in the community and the contextual factors that impact behaviour and the environment. Consequently, this knowledge can help to inform the design of locally appropriate health promotion interventions.
Study setting
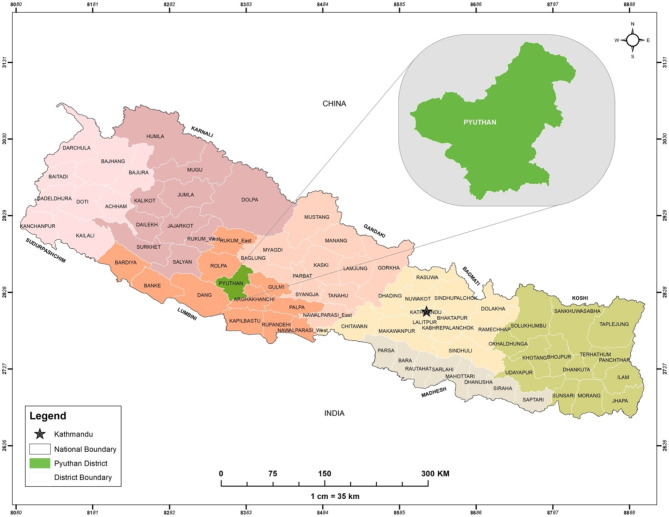
The study was conducted in two municipalities of Pyuthan district, namely Pyuthan Municipality and Jhimrukh Rural Municipality. Pyuthan is a mid-hills district in Nepal (Fig. 1) with a population of 232,019 (2021 census). The population includes a significant proportion of migrant workers, with low literacy levels, and low human development index [43, 44]. The district encompasses remote high hills with altitudes ranging from 305 to 3659 m above sea level. Human settlements in the district do not have adequate road networks, thus limiting people’s access to roads and public transportation. Pyuthan district is classified by the NTP as having a medium TB burden, with 275 cases reported to the NTP in 2017 [45].
Fig. 1.
Map of Nepal showing Pyuthan district
Intervention: drone optimised Therapy System (DrOTS) project
BNMT implemented the DrOTS project as a pilot intervention in the Pyuthan district in June 2019 to facilitate access to advanced molecular diagnostic testing for TB (GeneXpert MTB/RIF) in rural areas. The project established a drone network by linking remote health posts to testing laboratory hubs. The project was approved by 13 authorities of Nepal, including government ministries as well as provincial and local governmental bodies. Prior to implementation, BNMT organized a one-day consultative meeting with local government representatives, including municipal and ward leaders, healthcare providers, district officials, and the NTP, to discuss project plans and activities. Throughout the implementation phase, the BNMT team closely collaborated with district and local healthcare facilities, including TB centers, ensuring alignment with local authorities and health services. The DrOTS project aimed to establish whether drone sample transport was a feasible strategy for rural Nepal to reduce the severe urban/rural divide in access to health services. FCHVs verbally screened close contacts of index patients for TB symptoms, collected sputum samples where indicated, and delivered the samples to local health facilities through a process known as ‘active case finding’. The DrOTS project enabled health providers to expand access to GeneXpert MTB/RIF molecular testing for TB to remote areas of the district.
The drone transport network used two DJI M600 drones (SZ DJI Technology Co., Ltd, Shenzen, China) to transport samples from eight remote local health centers to two testing hubs at Bhingri Primary Health Care Center (PHCC) and the Pyuthan District Hospital (in Pyuthan municipality), where GeneXpert MTB/RIF molecular diagnostic machines were installed. Drone flights were conducted approximately once a week for each health center to a fixed schedule. Between June and November 2019, two drones completed a total of 220 flights, with an average of 18 flights per month, transporting 1,915 sputum samples of presumptive TB cases for GeneXpert testing. Sixty-two new TB cases were diagnosed and enrolled to treatment. The average flight time recorded between a local health center and a GeneXpert center was 5.8 min.
Prior to using drones for sample transportation, BNMT conducted a one-day orientation program separately for healthcare providers, FCHVs, and community stakeholders including school teachers, community leaders, and the local people. The program informed people about the use of drones in the community and discussed the potential risks, benefits, and safety measures of using drones.
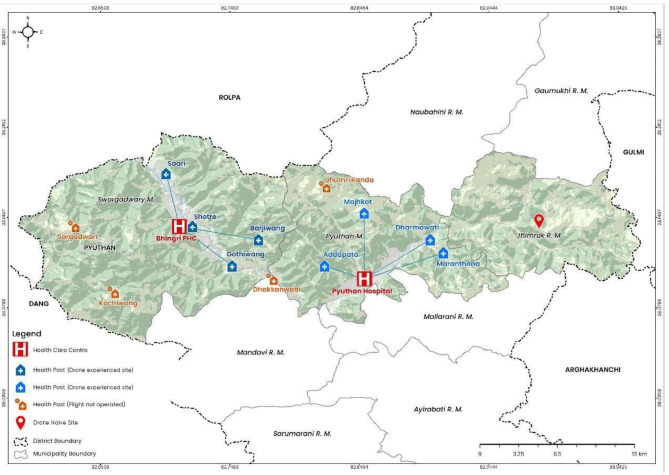
This qualitative study, embedded within the DrOTS project was conducted after six months of drone flights in Pyuthan municipality, (drone-experienced), and in Jhimrukh rural municipality where there is no current implementation of drones (drone-naïve) (Fig. 2).
Fig. 2.
Map of Pyuthan showing drone-experienced and drone-naive sites
Study participants
To include diverse viewpoints from the participants, the FGDs were conducted with purposively selected community stakeholders (local people, community leaders, school teachers), FCHVs, and healthcare providers (Table 1). FCHVs were trained for symptomatic screening for TB. The volunteers verbally screened close contacts of index patients for TB symptoms, collected sputum samples where indicated, and delivered the samples to local health facilities through a process known as ‘active case finding’. Healthcare providers included all the staff of the health post such as In-charge of the health post, auxiliary health worker, and auxiliary nurse midwives, and laboratory assistants. These participants were identified as important stakeholders in the DrOTS project. Healthcare providers have an important role in sample collection and transport via drones. Therefore, we also conducted an additional FGD with all the available healthcare providers at the health center of drone naive site to understand their perception of using drones in the future.
Table 1.
Participants in the focus group discussion (FGD) and their study area
| FGD participants | Study area | Number of participants | Drone experienced site | |
|---|---|---|---|---|
| Female | Male | |||
| FCHVs | Pyuthan municipality | 8 | 0 | Yes |
| Jhimrukh rural municipality | 8 | 0 | No | |
| Community stakeholders (community people and community leaders) | Pyuthan municipality | 5 | 5 | Yes |
| Jhimrukh rural municipality | 4 | 4 | No | |
| Healthcare providers | Jhimrukh rural municipality | 4 | 2 | No |
FCHV: Female Community Health Volunteer
The community stakeholders and FCHVs were selected in consultation with the DrOTS district team and included residents of the study sites, aged 18 years or older. FCHVs with over five years of working experience in health or DrOTS project were selected and invited to the FGD. The number of FGDs required for the study was informed by information power and methodological guidelines for focus group research [46–48]. All the participants were approached either by telephone conversation or in-person and the purpose of their participation in the study was explained to them. Of the 43 people invited, 40 individuals accepted to participate, two male community stakeholders of Pyuthan municipality and one male healthcare provider did not attend the FGD due to lack of time.
Data collection
In December 2019, data were collected by KD (female, Research Manager and a PhD student (at the time of writing) and trained in qualitative research) and BR (male, Research Associate, Bachelor in Public Health) from five FGDs: two FGDs in drone-experienced sites and three in drone-naïve sites. The topic, context, and format of the FGD were explained to the participants, and participants were provided an opportunity to ask any questions. Written informed consent was provided by all the participants. Participants received Rs 500 (approximately 4 USD) for their time contribution.
The FGDs were conducted in the Nepali language at the health centers, using semi-structured topic guides for each participant group. The guides were developed in English language, translated into Nepali, by bilingual speakers, and piloted within the research group (Additional File II). The FGDs collected information on three domains: (i) individual perception of using drones in community, (ii) perceived benefits of using drones and (iii) perceived challenges to operationalizing drones in TB care. The researchers allowed new themes to emerge in the discussion. FGDs were stopped when KD and BR felt no new information emerged and data saturation was reached. Each FGD was audio-recorded and conducted for approximately one hour. Member checking was done by listing and summarizing key points of discussion for participants, to ensure information accurately reflected the discussion. KD and BR conducted a debriefing meeting after every FGD.
Analysis
Data were manually analysed using codebook thematic analysis [49]. FGDs were transcribed verbatim in the Nepali language and translated into English by KD. KD and BR read the transcripts thoroughly and initially conducted open coding independently. Coding involved an iterative process, which matched, updated, and compared the responses within and among the groups. KD listed all the codes and grouped them into categories in close consultation with KSA (Associate professor and KD PhD supervisor, Karolinska Institute), which were then mapped to appropriate levels on the socio-ecological framework. Categories were charted and grouped to develop meaningful predominant themes. An illustration of the coding structure is shown in Table 2.
Table 2.
Example of coding structure applied in the analysis
| Code | Categories | Framework level | Theme | Quotes |
|---|---|---|---|---|
| Less physical mobility; no fear of missing buses; not required to work in haste; drone made work easier | Reduce providers’ travel time, costs and fear | Individual level | Drone-based sample transport optimised connectivity and accessibility for people with TB and healthcare providers | “The use of drones has been very effective to me. There is less physical mobility for volunteers. We do not fear the risk of missing buses to go home or doing our work in haste. This has made the work easier.” |
Results
We identified four main themes from the study, which are summarized in Table 3.
Table 3.
Categories and themes identified during codebook thematic analysis
| S.N. | Themes | Categories | |
|---|---|---|---|
| 1. | Trust in drones underpins successful use for TB diagnosis | 1.1 | Seeing drones physically and understanding their uses build trust |
| 1.2 | Prior knowledge of the use of drones determined trust | ||
| 1.3 | Information on drone use develops trust in TB interventions | ||
| 2. | Drone-based sample transport optimised connectivity and accessibility for people with TB and healthcare providers | 2.1 | Reduce distance and travel time |
| 2.2 | Reduce providers’ travel time, costs and anxiety | ||
| 2.3 | Overcome transportation obstructions | ||
| 2.4 | Improve recording of TB diagnosis | ||
| 2.5 | Efficient delivery of sputum samples for TB diagnosis | ||
| 3. | Drones create opportunities to improve community and healthcare system | 3.1 | Opportunities to develop skills using new technology |
| 3.2 | Opportunity to improve knowledge of drones and TB among the community | ||
| 3.3 | Opportunities for improved communication | ||
| 3.4 | Adapting experience of drone implementation beyond TB diagnosis | ||
| 3.5 | Capitalizing local human resources to improve TB diagnosis | ||
| 4 | External factors impede the use of drones to facilitate TB diagnosis | 4.1 | TB-related stigma discouraged sample collection |
| 4.2 | Drone flights are delayed by adverse weather | ||
| 4.3 | Costs and human resources to operate drones are limited | ||
Theme 1: Trust in drones underpins successful use for TB diagnosis
Participants emphasized that trust in drones was necessary prior to their use to support TB diagnosis. Participants perceived that trust in drones was strengthened after seeing the drones physically, receiving trusted information or having prior knowledge.
Individual level
Seeing drones physically and understanding their uses builds trust
In the drone-experienced sites, the majority of the participants were not aware of drones before seeing them in the community. Participants reported subsequently developing trust that the drones would be used appropriately for better healthcare with increased familiarity. People who saw drones for the first time wondered about the uncrewed mechanism of drones:
“I was surprised to see a helicopter-like object [drone] can fly without human driving it”. FCHV, Drone experienced site.
Knowledge of drones among participants expanded by attending community events such as drone launching and local festivals where drones were flown. Such events increased understanding of the appearance of drones, their uncrewed flight mechanism, and maximum payload. Community stakeholders and FCHVs claimed that flying drones by displaying TB awareness messages increased awareness of the drone technology and people’s willingness to be tested for TB because they perceived advanced technology healthcare was being applied:
“It has been easier to receive sputum samples from people as they believe that sputum diagnosis will be done in a better technology machine”. FCHV, Drone experienced site.
FCHVs also shared that when they saw drones transporting sputum samples from one health center to another without incident, it reassured them that drones could be used for safe and efficient delivery of sputum samples:
“I used to walk to health centers to deliver collected sputum samples. I saw sputum samples put inside that box [drones] and it flew away so high. After some time, I received a phone call from the health office that it was delivered. I was so happy to know it was delivered so fast”. FCHV, Drone experienced site.
Participants from both sites did not express any fears of drones flying in the community. Participants were confident that the drones were being used for healthcare purposes and that they would not capture pictures or videos. A community stakeholder stated:
“Drone is new for us but has no risks. No one is scared because there are also airplanes and helicopters flying in the sky. So, the drone also does not disturb. If it was moving on the road, it might scare us”. Community stakeholders, female, Drone experienced site.
Prior knowledge of the use of drones determined trust
At the drone-naïve sites, a few participants who had prior awareness of various applications of drones expressed trust in them. A few community stakeholders were aware from media sources, word-of-mouth or seeing drones used for geological mapping, that drones could take images and record information. One healthcare provider knew that drones were being used for multiple purposes. Having seen drones used in multiple sectors, they believed that drones are an innovation of science, and described them as effective and reliable machines to transport [samples] quickly, which they perceived as a priority need for improved health in Pyuthan district.
“Drone is a trustworthy machine to transport sputum samples of presumptive TB patients to laboratory centers and we can also receive test reports immediately. It will help us to diagnose more TB cases”. Healthcare provider, Female, Drone-naïve site.
-
b.
Community level
Information on drone use develops trust in TB interventions
Participants from both sites suggested prioritizing community-level awareness programs on drones to build a positive attitude toward the drone transport system. Community stakeholders from drone-experienced sites emphasized informing people about the purpose of drones in TB diagnosis, proper handling of drones, and activities that damage the drone equipment or hinder flight operations. It was suggested such information should be disseminated through trusted sources such as schools, local radio channels, and television, to improve awareness and promote trust in both drones and the TB programme:
“School level awareness activities on drones developed understanding of drones among our [secondary level government] school students as well as helped to raise awareness on knowing the symptoms of TB and people could be diagnosed with TB”. (Community stakeholder, Female, Drone experienced site)
Theme 2: Drone-based sample transport optimised connectivity and accessibility for people with TB and healthcare providers
Individual level
Reduce distance and travel time
Participants from both sites believed that drones overcame geographical barriers by increasing the accessibility of health services for people in remote communities. Community stakeholders and healthcare providers perceived drones reduced peoples’ visits to health centers by transporting sputum samples from communities among high-altitude hills with poor road networks. This service particularly benefitted people with TB and/or disabilities and elderly people who struggle to walk long distances, especially in rural terrain. A community stakeholder expressed this advantage:
“If drones go to places where buses are not available, then people do not need to walk for a long time to receive care. It will be beneficial, especially to people with physical disability or discomfort, old aged people, and people living in minimum socio-economic conditions”. (Community stakeholder, Male, Drone-naïve site)
Drones also assisted FCHVs in transporting large numbers of sputum samples from communities to diagnostic centers, with more accurate molecular testing in less time. FCHVs discussed that the drones also reduced their waiting time for sample preparation, storage and provided quick diagnostic reports:
“The drone has saved my time. I do not have to wait long time at health centers to receive the reports, and people with positive TB can also start medicines immediately when the drone brings back the report.” FCHV, Drone experienced site.
Reduce providers’ travel time, costs and anxiety
In addition, FCHVs reported drones substantially reduced travel time and opportunity costs. FCHVs often deliver sputum samples at diagnostic centers using public transportation that departs from a designated location only once or twice a day. Samples need to be labeled and stored in the laboratories which required significant time at the health centers. They therefore experienced frequent transportation-related issues such as missing local buses, working in haste to complete their work and catch public transport, or having to arrange and pay out-of-pocket for private transportation, or asking someone to drop them off at a specific place. FCHVs underscored the benefits of using drones at work as it reduced their fear, worry, anxiety or stress regarding transportation availability:
“The use of drones has been very effective to me. There is less physical mobility for volunteers. We do not fear the risk of missing buses to go home or doing our work in haste. This has made the work easier.” FCHV, Drone experienced site.
One FCHV also emphasized that because drones reduced their working hours, they were able to spend more time with family, complete their household chores, and support the family in their agricultural work. This improved interpersonal relationships and family support for their professional work.
-
b.
Community level
Overcome transportation obstructions
Participants from drone naïve sites perceived that drones could be used in adverse weather conditions to provide uninterrupted TB diagnosis. Community stakeholders and FCHVs discussed the detrimental effects of persistently high rainfall in Pyuthan district, which is a frequent occurrence during the Nepal monsoon. Roads in Nepal are frequently obstructed due to natural disasters such as floods, earthquakes and landslides. Participants suggested that drones could be used to transport healthcare products when roads or paths are blocked for multiple days.
-
c.
Health system level
Improve recording of TB diagnosis
Participants perceived that using drones in TB programs offers wider benefits to the health system. FCHVs claimed that drones integrated with GeneXpert MTB/RIF machines make the TB diagnosis, testing, and reporting process efficient, including tracking the records of samples that are delivered and tested. One FCHV participant shared her experience:
“After the use of drones and TB diagnosing machines in our area, there has been improvement in monitoring of presumptive TB people because we collect on-spot sputum samples and it takes only one-day visit to get the report.” FCHV, Drone experienced site.
Efficient delivery of sputum samples for TB diagnosis
FCHVs compared the time taken by volunteers to deliver the sputum samples versus the drones and concluded that drones transport samples much quicker without compromising the quality of sputum samples and were thus perceived to improve TB diagnosis.
FCHVs recommended using drones as an ‘on-demand’ service, rather than a fixed flight schedule to diagnose more people with TB. Furthermore, providers and FCHVs mentioned that increasing the number of flights and sputum collection centers according to the demand of health centers would increase TB diagnosis. Community stakeholders, particularly teachers, suggested using schools as the collection centers in hard-to-reach areas where drones can easily take off and land and suggested teachers could facilitate the sputum collection and transportation to drones.
Theme 3: Drones create opportunities to improve community and healthcare system
a. Community level
Opportunities to develop skills using new technology
The commonly perceived benefits of using drones within the TB program were opportunities for community development. Community stakeholders of the drone-naïve site perceived the drone transport system integration would bring new services for better health and develop technological knowledge and skills of health workers:
“I felt that new technologies are used in Pyuthan, it is a sign of development in that area. People like us and those working in health services will see and get opportunities to learn using it”. Community stakeholders, Male, Drone-naive site.
Opportunity to improve knowledge of drones and TB among the community
FCHVs and Community stakeholders believed that operating drones to facilitate TB diagnosis could make use of local human capacity and community resources, which a participant described as ‘gaining two for the price of one’. They felt that individuals such as community leaders, healthcare providers, and FCHVs could have instrumental roles in spreading positive awareness about both drones and promoting TB diagnosis and care seeking. FCHVs stressed using the well-established network of FCHVs and Mothers groups would help to develop or increase trust with local communities, which will ultimately increase utilization of local health services.
b. Health System level
Opportunities for improved communication
FCHVs shared that when drones transported sputum samples, it allowed them to spend more time with people with TB, to communicate about medicine adherence, side effects, infection control, and adopting healthy behavior to cope with TB illness.
Adapting experience of drone implementation beyond TB diagnosis
The healthcare providers, FCHVs and community stakeholders perceived that knowledge gained by using drones for transporting sputum samples in the TB program is an opportunity to widen the use of drones beyond TB diagnosis. Healthcare providers stressed the need for drones in rural areas to deliver people-centered care and hoped to expand the use to deliver medicines and biological samples such as blood, urine, and stool samples. The drone transport system was commonly perceived to potentially benefit people with TB by decreasing necessary visits to distant health centers:
“People when come to health facilities with TB symptoms, are already very weak. They come from high hills. Sometimes people carry the sick people in ‘doko’ [a large bamboo basket carried on people’s back] and bring them here. It is difficult for them, especially until their second month, to adhere to treatment regularly. Transporting medicines from drones will reduce this problem.” Healthcare provider, Male, Drone-naïve site.
Capitalizing local human resources to improve TB diagnosis
FCHVs in drone-experienced sites reflected that the ongoing advocacy activities around drones also helped increase recognition of the work of FCHVs in the community and healthcare. A participant mentioned that if health programs inform people about the work FCHVs are doing, it would collectively increase the credibility of their work, build trust among people and facilitate people receiving better quality of healthcare from their services. Community stakeholders deemed mobilizing local resources to operate drones to be a potential avenue toward the sustainability of the use of drones in TB and broader health programs. FCHVs also expressed their willingness to operate drones. Collectively, FCHVs perceived the integration of drones into the TB program as an opportunity to improve the skills and capacity of the healthcare providers:
“We can also operate drones if we are provided training”. FCHV, Drone experienced site.
Theme 4: External factors impede the use of drones to facilitate TB diagnosis
Individual level
TB-related stigma discouraged sample collection
Participants reported the challenges of using drones in TB diagnosis include the deep-rooted stigma associated with TB disease in the community and people’s hesitancy to provide sputum samples for testing. FCHVs mentioned that many people are still unwilling to give their sputum samples to volunteers for testing, take TB medicines, or deny the fact that they have a cough or other symptoms of TB. Therefore, before using drones for TB diagnosis, the group recommended conducting complementary knowledge enhancing interventions by educating people on the signs and symptoms of TB, ways to prevent it and the importance of testing for TB when symptomatic.
-
b.
Community level
Drone flights are delayed by adverse weather
FCHVs mentioned that adverse weather conditions such as foggy weather or heavy rain that are typical during monsoon season (mid-June to early September) can be a challenge for stable takeoff, aerial flights and landings.
-
c.
Health system level
Costs and human resources to operate drones are limited
Community stakeholders from drone-experienced sites expressed concerns that drone flights are limited by the project duration and external financial support. Sustainability and cost-effectiveness were perceived as important issues:
“I assume the financial investment is high. My concern is its use in implementation. Is the money spent worth the outcome? How can we make sure we use drones after the project completes?” Community stakeholder, Male, Drone experienced site.
FCHVs mentioned that drone use is new in Nepal’s healthcare and raised the issue of inadequate human resources to handle the technical aspects of the drone. One FCHV explained the need for a drone pilot to operate the drone software at the time of take-off and landing caused delays in initiating the drone operation if the pilot was not available:
“Sometimes, we need to wait for a long waiting time for a drone to take off due to delays caused by the pilot. They are not present sometimes or take time to start”. FCHV, Drone experienced site.
By contrast, other FCHVs expressed an eagerness to be trained as drone operators to solve this issue.
Discussion
The study demonstrated that irrespective of the study sites, healthcare providers, FCHVs, and community stakeholders perceived drones as beneficial to overcome barriers to accessing TB care in the rural hills of Nepal.
Our study highlights the importance of developing community trust when integrating new technologies, such as drones, into health services. Studies of acceptance by people of healthcare interventions have shown that trust is an important element which influences the utilization of novel technology services [50–52]. Engagement and information from trusted community figures such as healthcare providers and leaders, enhance trust which was also emphasized by our participants as crucial to building trust and raising awareness among the public [53]. Seeing drones physically at community-organized events, having prior knowledge of the varied uses of drones, and receiving transparent information on the purpose, uses, and risks of drones developed positive trust. Unlike other settings, we did not identify concerns regarding either privacy or misuse of drones for terrorism [10, 14, 15, 35–37, 54]. Of note, drone implementation projects that have incorporated community engagement prior to deployment have also reported that people did not perceive drones as threatening [11, 15, 36]. This proactive involvement may have helped dispel potential fears and fostered a positive reception because communities were better informed about the technology’s purpose and potential benefits. Conversely, limited information on new interventions or technology is likely to evoke myths, misinformation, and hesitancy among the public and may influence their acceptance and perceived benefits [54, 55]. Early and meaningful community engagement has proved effective in building trust, promoting equitable access to healthcare services and improving health outcomes [56, 57].
This study also demonstrated that the use of drones in the hills of Pyuthan was perceived as beneficial in reducing the distance, time, and costs of accessing or providing TB care. Using drones to transport sputum samples was perceived to reduce long walking distances to the health centers and particularly benefit elderly people or people with disabilities who face difficulties in walking. It was also regarded as beneficial for FCHVs as it reduced the time required to physically transport sputum samples from one health center to another. reduced personal transport costs, walking times, and the fear of missing buses or public transport availability. A multi-country study on patient pathway analyses recommended the need to establish a transport network from health centers to centralized laboratories to improve diagnostic capacity since three-quarters of people access health centers where there are no laboratory testing services [58]. Poor transport infrastructure and road networks are well-documented challenges for people who are ill to access health care in Nepal and other low- and middle-income countries [4, 19, 59], and our study highlights the potential role of drone transport networks to decrease the formidable transport challenges faced by health providers in rural areas of Nepal. Addressing the transportation barriers in geographically remote terrain is crucial to promoting equitable access to health services, improving health outcomes, and reducing financial burden.
Similar to studies conducted across countries in Asia and Africa, our study also identified that drone use benefits the health system [15, 60]. Drones were perceived to facilitate prompt sample delivery and preserve the quality of sputum samples by overcoming poor road connections or frequent road obstructions due to natural disasters. However, it is also important to note that the perceived benefits of drones for early diagnosis may have been reflecting knowledge of the linkage to advanced molecular GeneXpert TB testing facilitated by drones rather than drones per se. Our findings of the perceived benefits of using drones also mirror results from other studies that show drones in healthcare have been perceived to improve access to healthcare and reduce sample delivery time, sample wastage, and costs for people accessing care [10, 15, 61–63].
Drones were perceived to offer broader advantages for healthcare providers at their personal level and as an opportunity for development. Drones freed their working hours by reducing sample delivery times, which even improved interpersonal relationships. This is similar to a study that reported drones reduced working hours for healthcare providers and healthcare costs for patients as benefits of using drone transport systems [15]. In our study, demands were raised for expanded geographical coverage, wider scope of application, and increased frequency of flight, reflecting the highly positive reception of the drone transport system. Expansion of drone services with scarce external resources would require the need to develop local capacity [15]. We found that providers were enthusiastic to receive skill-enhancement training to operate drones. In Nepal, the active mobilization of healthcare providers, community stakeholders, and FCHVs are proven effective strategies to increase healthcare access and reduce patient-related costs [6, 7]. Therefore, developing the capacity of FCHVs and other healthcare providers to operate drones would be an opportunity to expand the application of drones for wider healthcare applications, increase the cost-effectiveness of using drones, and develop safer sample or vaccine transport mechanisms during future emergencies such as the aftermath of earthquakes or the COVID-19 pandemic [14, 64, 65].
The study findings encompass multifaceted challenges including combating TB stigma, adapting the technology to the environmental conditions and terrain, and overcoming financial resources and human capacity constraints. TB-related stigma and its consequences are a known barrier to diagnosing and curing TB in Nepal and other LMICs [4, 66–70]. Therefore, the implementation of drones for TB diagnosis requires contextual understanding and addressing stigma to empower people to be tested for TB. Operating drones in geographically challenging areas during rainfall and windy conditions and with limited technical expertise and financial resources are also commonly reported challenges in other countries using drones for medical transportation [11, 36, 71]. Thus, the study underscores the importance of implementing comprehensive contextual strategies to successfully apply innovative technology for medical services.
Strengths and limitations
This is the first study in Nepal to explore perceptions of community stakeholders and healthcare providers using drones for health service delivery, contributing to global evidence on stakeholder experiences with drone implementation for healthcare [36, 37, 54]. The study establishes knowledge regarding the lived experience of applying drone technology in Nepali healthcare, and can inform strategies and recommendations for future deployment of drones for healthcare applications in LMICs, including Nepal.
The study was limited to the area where the drone project was implemented, and a nearby municipality, and therefore represents a limited group among Nepal’s many ethnically and culturally diverse communities. Further research should include perceptions from religious and political leaders. Although our study revealed gender-specific benefits, we did not conduct an in-depth exploration with a gender lens during the FGDs. Additionally, we did not explore the perception of higher-level government policymakers in the current study, whose engagement is crucial in planning and designing interventions. Analysis of the policy landscape and stakeholder perceptions of policy strengths and limitations is an important topic which also merits in depth analysis as the field of cargo drone legal regulation is rapidly evolving globally. Similarly, people with TB were not included in the FGDs. The inclusion of service end-users perspectives would provide additional perspectives on the challenges to access TB and other healthcare services, and the use of drones to facilitate disease diagnosis in Nepal. Future qualitative evaluations should include community service users. We have described the project location and context to facilitate the transferability of the findings to other similar settings. The location for the drone project was initially selected due to the experience of BNMT with the local community, which identified the community and government stakeholders as being receptive to the implementation of novel technologies, and engaged and committed collaborators for projects that directly address community-identified needs. We anticipate that the recall bias was minimal for the participants as the study was conducted during the period of drone implementation. The project team from Nepal Flying Labs and Birat Nepal Medical Trust conducted numerous community engagement events in partnership with local community leaders, at the implementation site, both before and during drone implementation. This is likely to have enhanced the overwhelmingly positive community perceptions reported during the FGDs, with some influence also on the drone naïve site.
Conclusions
Healthcare providers, FCHVs, and community stakeholders reported high levels of trust in drones and perceived their use for TB diagnosis to substantially benefit people with TB and healthcare providers through efficient delivery of samples, improved diagnostic services, and reduced travel time. There was a high level of demand for application to other healthcare services and wider geographical coverage, demonstrating drones as a potential tool for enhancing access to healthcare in geographically remote communities. Contextual community engagement is a critical factor in the successful implementation of novel technologies for health services.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to acknowledge all the participants who contributed to the study. We would also like to thank the Health office team of Pyuthan district, authorities and healthcare providers, and female health community volunteers of Pyuthan municipality and Jhimrukh rural municipality. Respective Ministries and departments for timely providing approval and recommendation letters and the National Tuberculosis Control Center for the support during the study.
Abbreviations
- BNMT
Birat Nepal Medical Trust
- COREQ
COnsolidated criteria for REporting Qualitative research
- DOTS
Directly Observed Treatment Shortcourse
- DrOTS
Drone Optimised Therapy System
- FCHV
Female Community Health Volunteers
- FGD
Focus Group Discussion
- HCP
Health Care Provider
- LMIC
Low- and middle-income country
- NTP
National Tuberculosis Program
- PHCC
Primary Health Care Center
- TB
Tuberculosis
- WHO
World Health Organization
Authors’ contributions
K.D. and B.R. collected the data. K.D. and B.R. analyzed and interpreted findings with support from K.S.A. K.D. and R.P. drafted the manuscript. R.D., S.C.G., P.S., P.M., and MC contributed to study design and KD and KSA designed the research question. GM, RD, SA, GRB, PP, SCG, BS, PL, UP, PS, and JB contributed to the project implementation. SCG, RD, MC, PS, and PM contributed to the funding acquisition of the project. MC and KSA edited and proofread the final draft. All authors read and approved the final manuscript.
Funding
KD received research funding from the Farrar Foundation for the qualitative study. The DrOTS project was funded by the Nick Simons Foundation. MC, RD, KD and SCG were funded by EU Horizon 2020 project Impact TB 733174. SA was funded by TB REACH wave V.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The approval for the use of drones for sputum sample transportation was received from twelve government Ministries and Departments policy and guidelines. The study received ethical approval from the Nepal Health Research Council (Approval number: 251–2019). The study provided a participant information sheet detailing the description of the study, objectives, risks and benefits of participating in the study, funding agencies, and their ability to withdraw at any point of time during the study period. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization (WHO). Global Tuberculosis Report 2022 [Internet]. 2022 [cited 2022 Nov 3]. https://www.who.int/teams/global-tuberculosis-programme/tb-reports/global-tuberculosis-report-2022.
- 2.Storla DG, Yimer S, Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health [Internet]. 2008 [cited 2020 Jul 22];8:1–9. https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-8-15. [DOI] [PMC free article] [PubMed]
- 3.de Vries SG, Cremers AL, Heuvelings CC et al. Barriers and facilitators to the uptake of tuberculosis diagnostic and treatment services by hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review of qualitative literature. Lancet Infect Dis [Internet]. 2017 May [cited 2020 Jan 28];17(5):e128–43. https://linkinghub.elsevier.com/retrieve/pii/S147330991630531X. [DOI] [PubMed]
- 4.Dixit K, Biermann O, Rai B, et al. Barriers and facilitators to accessing tuberculosis care in Nepal: a qualitative study to inform the design of a socioeconomic support intervention. BMJ Open. 2021;11(10):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Health Organization. Global tuberculosis report 2020. Geneva; 2020. [Google Scholar]
- 6.Gurung SC, Rai B, Dixit K, et al. How to reduce household costs for people with tuberculosis: a longitudinal costing survey in Nepal. Health Policy Plan. 2020;2020:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gurung SC, Dixit K, Rai B et al. The role of active case finding in reducing patient incurred catastrophic costs for tuberculosis in Nepal. Infect Dis Poverty [Internet]. 2019;8(1):99. https://idpjournal.biomedcentral.com/articles/10.1186/s40249-019-0603-z. [DOI] [PMC free article] [PubMed]
- 8.Stop TB. Partnership. The Global Plan to End TB 2016–2020: The Paradigm Shift [Internet]. 2015. http://www.stoptb.org/assets/documents/global/plan/GlobalPlanToEndTB_TheParadigmShift_2016-2020_StopTBPartnership.pdf.
- 9.Bahrainwala L, Knoblauch AM, Andriamiadanarivo A et al. Drones and digital adherence monitoring for community-based tuberculosis control in remote Madagascar: A cost-effectiveness analysis. PLoS One [Internet]. 2020 Jul 1 [cited 2021 Jun 2];15(7 July):e0235572. 10.1371/journal.pone.0235572. [DOI] [PMC free article] [PubMed]
- 10.Laksham KB. Unmanned aerial vehicle (drones) in public health: A SWOT analysis [Internet]. Vol. 9, Journal of Family Medicine and Primary Care. Hindawi Publishing Corporation; 2019 [cited 2022 Oct 23]. pp. 342–6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6436288/pdf/JFMPC-8-342.pdf. [DOI] [PMC free article] [PubMed]
- 11.Knoblauch AM, De La Rosa S, Sherman J et al. Bi-directional drones to strengthen healthcare provision: Experiences and lessons from Madagascar, Malawi and Senegal. BMJ Glob Health [Internet]. 2019 Jul 1 [cited 2021 Jun 4];4(4):1541. http://gh.bmj.com/. [DOI] [PMC free article] [PubMed]
- 12.Fornace KM, Drakeley CJ, William T et al. Mapping infectious disease landscapes: Unmanned aerial vehicles and epidemiology [Internet]. Vol. 30, Trends in Parasitology. Elsevier Ltd; 2014 [cited 2023 Apr 28]. pp. 514–9. https://www.cell.com/trends/parasitology/fulltext/S1471-4922(14)00146-9?_returnURL=https%3A%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS1471492214001469%3Fshowall%3Dtrue. [DOI] [PubMed]
- 13.Haidari LA, Brown ST, Ferguson M, et al. The economic and operational value of using drones to transport vaccines. Vaccine. 2016;34(34):4062–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poljak M, Šterbenc A. Use of drones in clinical microbiology and infectious diseases: current status, challenges and barriers. Clinical Microbiology and Infection. Volume 26. Elsevier B.V.; 2020. pp. 425–30. [DOI] [PubMed] [Google Scholar]
- 15.Jeyabalan V, Nouvet E, Meier P et al. Context-specific challenges, opportunities, and ethics of drones for healthcare delivery in the eyes of program managers and field staff: A multi-site qualitative study. Drones [Internet]. 2020 Sep 1 [cited 2022 Dec 25];4(3):1–20. https://www.mdpi.com/2504-446X/4/3/44.
- 16.Annual Report- 2076/77 (2019/20) – Department of Health Services [Internet]. [cited 2022 May 17]. https://dohs.gov.np/annual-report-2076-77-2019-20/.
- 17.Mahato RK, Laohasiriwong W, Vaeteewootacharn K et al. Major delays in the diagnosis and management of tuberculosis patients in Nepal. Journal of Clinical and Diagnostic Research [Internet]. 2015 Oct 1 [cited 2021 Jun 3];9(10):LC05–9. Available from: www.jcdr.net. [DOI] [PMC free article] [PubMed]
- 18.Li Y, Ehiri J, Tang S et al. Factors associated with patient, and diagnostic delays in Chinese TB patients: A systematic review and meta-analysis. BMC Med [Internet]. 2013 Jun 2 [cited 2021 Jun 6];11(1):156. /pmc/articles/PMC3699418/. [DOI] [PMC free article] [PubMed]
- 19.Marahatta SB, Yadav RK, Giri D et al. Barriers in the access, diagnosis and treatment completion for tuberculosis patients in central and western Nepal: A qualitative study among patients, community members and health care workers. PLoS One [Internet]. 2020 [cited 2020 Sep 13];15(1):e0227293. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0227293. [DOI] [PMC free article] [PubMed]
- 20.Mahato RK, Laohasiriwong W, Vaeteewootacharn K. Major Delays in the Diagnosis and Management of Tuberculosis Patients in Nepal. Journal of Clinical and Diagnostic Research [Internet]. 2015 [cited 2020 Feb 1];9(10):5–9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4625264/#:~:text=reduce such delays.-,Conclusion,facilities%2 C poor knowledge on TB. [DOI] [PMC free article] [PubMed]
- 21.Laohasiriwong W, Mahato RK, Koju R et al. Delay for First Consultation and Its Associated Factors among New Pulmonary Tuberculosis Patients of Central Nepal. Tuberc Res Treat [Internet]. 2016;2016:4583871. http://downloads.hindawi.com/journals/trt/2016/4583871.pdf. [DOI] [PMC free article] [PubMed]
- 22.Gurung SC, Rai B, DIxit K et al. How to reduce household costs for people with tuberculosis: A longitudinal costing survey in Nepal. Health Policy Plan [Internet]. 2021 Jun 1 [cited 2021 Jul 2];36(5):594–605. https://academic.oup.com/heapol/article/36/5/594/6042349. [DOI] [PMC free article] [PubMed]
- 23.Gurung SC, Dixit K, Rai B et al. The role of active case finding in reducing patient incurred catastrophic costs for tuberculosis in Nepal. Infect Dis Poverty [Internet]. 2019 Dec 3 [cited 2021 Jul 2];8(1):1–15. https://link.springer.com/articles/10.1186/s40249-019-0603-z. [DOI] [PMC free article] [PubMed]
- 24.Wingfield T, Tovar MA, Huff D, et al. Beyond pills and tests: addressing the social determinants of tuberculosis. Clin Med. 2016;16:s79–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.WHO | The End TB Strategy. WHO [Internet]. 2017 [cited 2021 Jun 6]; http://www.who.int/tb/strategy/end-tb/en/.
- 26.WHO | Digital health for the End TB Strategy. - an agenda for action. WHO [Internet]. 2016 [cited 2021 Jun 4]; http://www.who.int/tb/publications/digitalhealth-TB-agenda/en/.
- 27.Pageni B, Pudasaini U, Pudasaini D et al. Evolution of Unmanned Aerial Vehicles in Nepal [Internet]. Journal on Geoinformatics. 2020 [cited 2024 Aug 23]. https://www.nepjol.info/index.php/NJG/article/view/50963/38067.
- 28.Thapa P. Potential Use of UAVs in COVID19 Vaccination: A Case Study of Nepal. Res Sq [Internet]. 2021; 10.21203/rs.3.rs-568371/v1.
- 29.Berninzon AL, Vongasemjit O. Potential Benefits of Drones for Vaccine Last-Mile Delivery in Nepal. 2021.
- 30.Médecins Sans Frontières. Innovating to reach remote TB patients and improve access to treatment. 2014. https://www.msf.org/papua-new-guinea-innovating-reach-remote-tb-patients-and-improve-access-treatment.
- 31.Birat Nepal Medical Trust. DrOTS Nepal (Drone Optimised Therapy System). 2024.
- 32.Hern A. Nepal moves to limit drone flights following earthquake. The Guardian. 2015. https://www.theguardian.com/technology/2015/may/06/nepal-moves-to-limit-drone-flights-following-earthquake.
- 33.Civil Aviation Authority of Nepal. Unmanned Aircraft System Requirements (UASR) [Internet]. Kathmandu. 2021 Apr [cited 2024 Oct 8]. https://caanepal.gov.np/storage/app/media/drone/sep%2024%202022/UAS%20Requirement%20final.pdf.
- 34.World Health Organization. Ethics and governance of artificial intelligence for health: WHO guidance [Internet]. 2021 [cited 2023 Jul 14]. https://www.who.int/publications/i/item/9789240029200.
- 35.Lidynia C, Philipsen R, Ziefle M. Droning on About Drones—Acceptance of and Perceived Barriers to Drones in Civil Usage Contexts [Internet]. Vol. 499. Springer, Cham; 2017 [cited 2023 Jul 14]. 317–329 p. https://link.springer.com/chapter/10.1007/978-3-319-41959-6_26.
- 36.Truog S, Maxim L, Matemba C, et al. Insights before flights: how community perceptions can make or break medical drone deliveries. Volume 4. Drones. MDPI AG; 2020. pp. 1–14. [Google Scholar]
- 37.Hardy A, Proctor M, MacCallum C et al. Conditional trust: community perceptions of drone use in malaria control in Zanzibar. Technol Soc. 2022;68:101895. 10.1016/j.techsoc.2022.101895. [DOI] [PMC free article] [PubMed]
- 38.Stop TB, Partnership. Unmanned Aerial Vehicles: A Tool for Tuberculosis Care [Internet]. [cited 2024 Jan 2]. https://www.stoptb.org/sites/default/files/unmanned_aerial_vehicles-_a_tool_for_tb_care.pdf.
- 39.Adhikari B, Pell C, Cheah PY. Community engagement and ethical global health research. Global Bioethics [Internet]. 2020 Jan 1 [cited 2024 Jan 2];31(1):1–12. https://www.tandfonline.com/doi/full/10.1080/11287462.2019.1703504. [DOI] [PMC free article] [PubMed]
- 40.Hunter DJ, Mccallum J, Howes D. Defining Exploratory-Descriptive Qualitative (EDQ) research and considering its application to healthcare. Journal of Nursing and Health Care [Internet]. 2019;4(1). http://eprints.gla.ac.uk/180272/http://eprints.gla.ac.uk.
- 41.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care [Internet]. 2007 [cited 2020 Jul 22];19(6):349–57. 10.1093/intqhc/mzm042. [DOI] [PubMed]
- 42.McLeroy KR, Bibeau D, Steckler A et al. An Ecological Perspective on Health Promotion Programs [Internet]. 1988 [cited 2023 Jul 14]. https://journals.sagepub.com/doi/epdf/10.1177/109019818801500401. [DOI] [PubMed]
- 43.National Planning Commission. Government of Nepal. Nepal Human Development Report 2014 [Internet]. [cited 2023 Apr 30]. https://www.npc.gov.np/images/category/NHDR_Report_2014.pdf.
- 44.Ministry of Labour E and SSecurityG of N. Nepal Labour Migration Report 2020 [Internet]. [cited 2023 Apr 30]. https://www.developmentaid.org/api/frontend/cms/file/2020/12/Migration-Report-2020-English.pdf.
- 45.Department of Health Services, National Tuberculosis Centre. National Tuberculosis Program Nepal Annual Report-2018. 2018;75:1–148.
- 46.Malterud K, Siersma VD, Guassora AD. Sample Size in Qualitative Interview Studies : Guided by Information Power. Qualitative Heath Research [Internet]. 2016 [cited 2020 May 11];26(13):1753–60. https://pubmed.ncbi.nlm.nih.gov/26613970/. [DOI] [PubMed]
- 47.Hennink MM, Kaiser BN, Weber MB, Sizes in Focus Group Research. What Influences Saturation? Estimating Sample. Qual Health Res [Internet]. 2019 Aug 1 [cited 2024 Jan 2];29(10):1483–96. https://journals.sagepub.com/doi/epub/10.1177/1049732318821692. [DOI] [PMC free article] [PubMed]
- 48.Hennink M, Kaiser BN. Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Soc Sci Med [Internet]. 2022 Jan 1 [cited 2024 Jan 2];292. https://www.sciencedirect.com/science/article/pii/S0277953621008558?via%3Dihub. [DOI] [PubMed]
- 49.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol [Internet]. 2006 [cited 2020 Sep 11];3(2):77–101. https://www.tandfonline.com/doi/abs/10.1191/1478088706qp063oa.
- 50.Fan W, Liu J, Zhu S et al. Investigating the impacting factors for the healthcare professionals to adopt artificial intelligence-based medical diagnosis support system (AIMDSS). Ann Oper Res [Internet]. 2020 Nov 1 [cited 2024 Mar 27];294(1–2):567–92. https://link.springer.com/article/10.1007/s10479-018-2818-y.
- 51.Adhikari B, Yeong Cheah P, von Seidlein L. Trust is the common denominator for COVID-19 vaccine acceptance: A literature review. Vaccine X [Internet]. 2022 Dec 1 [cited 2024 Mar 27];12. https://www.sciencedirect.com/science/article/pii/S2590136222000730. [DOI] [PMC free article] [PubMed]
- 52.Shevtsova D, Ahmed A, Boot IWA, et al. Trust in and Acceptance of Artificial Intelligence Applications in Medicine: mixed methods study. JMIR Hum Factors. 2024;11:e47031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Latkin CA, Dayton L, Yi G et al. Trust in a COVID-19 vaccine in the U.S.: A social-ecological perspective. Soc Sci Med [Internet]. 2021 Feb 1 [cited 2024 Mar 27];270. https://www.sciencedirect.com/science/article/pii/S0277953621000162. [DOI] [PMC free article] [PubMed]
- 54.Clothier RA, Greer DA, Greer DG et al. Risk Perception and the Public Acceptance of Drones. Risk Analysis [Internet]. 2015 Jun 1 [cited 2023 Dec 7];35(6):1167–83. https://onlinelibrary.wiley.com/doi/epdf/10.1111/risa.12330?saml_referrer. [DOI] [PubMed]
- 55.World Health Organization. Vaccination and trust: How concerns arise and the role of communication in mitigating crises [Internet]. Denmark; 2017 [cited 2024 Mar 27]. https://www.who.int/publications/i/item/vaccination-and-trust.
- 56.Gilson L. Trust and the development of health care as a social institution. Soc Sci Med [Internet]. 2003 [cited 2024 Mar 27];56:1453–68. https://www.sciencedirect.com/science/article/pii/S0277953602001429?via=ihub. [DOI] [PubMed]
- 57.Birkhäuer J, Gaab J, Kossowsky J et al. Trust in the health care professional and health outcome: A meta-analysis. PLoS One [Internet]. 2017 Feb 1 [cited 2024 Mar 30];12(2). https://journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0170988&type=printable. [DOI] [PMC free article] [PubMed]
- 58.Hanson C, Osberg M, Brown J et al. Finding the Missing Patients with Tuberculosis: Lessons Learned from Patient-Pathway Analyses in 5 Countries. Journal of Infectious Diseases [Internet]. 2017 [cited 2024 Apr 1];216:S686–95. https://pubmed.ncbi.nlm.nih.gov/29117351/. [DOI] [PMC free article] [PubMed]
- 59.Kaiser N, Barstow CK. Rural Transportation Infrastructure in Low-and Middle-Income Countries: A Review of Impacts, Implications, and Interventions [Internet]. Vol. 14, Sustainability MDPI. 2022 [cited 2024 Mar 31]. https://www.mdpi.com/2071-1050/14/4/2149.
- 60.Ayamba Kandodo. Drone technology boosts TB control efforts in Mangochi. The Nation [Internet]. 2023 Nov 23 [cited 2024 Jan 2]; https://mwnation.com/drone-technology-boosts-tbcontrol-efforts-in-mangochi/.
- 61.Nisingizwe MP, Ndishimye P, Swaibu K et al. Effect of unmanned aerial vehicle (drone) delivery on blood product delivery time and wastage in Rwanda: a retrospective, cross-sectional study and time series analysis. Lancet Glob Health [Internet]. 2022 Apr 1 [cited 2024 Jan 11];10(4):e564–9. https://www.thelancet.com/action/showPdf?pii=S2214-109X%2822%2900048-1. [DOI] [PubMed]
- 62.Amukele T. Current State of Drones in Healthcare: Challenges and Opportunities. Journal of Applied Laboratory Medicine [Internet]. 2019 Sep 1 [cited 2024 Jan 11];4(2):296–8. https://www.researchgate.net/publication/374673787_Drone_medical_deliveries_in_low_and_moderate_income_countries_insights_from_Vanuatu_Malawi_Rwanda_and_Ghana. [DOI] [PubMed]
- 63.Sachan D. The age of drones: what might it mean for health? Lancet. 2016;387(10030):1803–4. [DOI] [PubMed] [Google Scholar]
- 64.Kunovjanek M, Wankmüller C. Containing the COVID-19 pandemic with drones - feasibility of a drone enabled back-up transport system. Transp Policy (Oxf). 2021;106:141–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sylverken AA, Owusu M, Agbavor B et al. Using drones to transport suspected COVID-19 samples; experiences from the second largest testing centre in Ghana, West Africa. PLoS ONE. 2022;17(11):e0277057. [DOI] [PMC free article] [PubMed]
- 66.Chang SH, Cataldo JK. A systematic review of global cultural variations in knowledge, attitudes and health responses to tuberculosis stigma [Internet]. Vol. 18, International Journal of Tuberculosis and Lung Disease. 2014 [cited 2023 May 23]. pp. 168–73. https://www.ingentaconnect.com/content/iuatld/ijtld/2014/00000018/00000002/art00008#. [DOI] [PubMed]
- 67.Juniarti N, Evans D. A qualitative review: The stigma of tuberculosis. J Clin Nurs [Internet]. 2011 Jul [cited 2023 May 7];20(13–14):1961–70. https://onlinelibrary.wiley.com/doi/epdf/10.1111/j.1365-2702.2010.03516.x?saml_referrer. [DOI] [PubMed]
- 68.Kamble B, Singh S, Jethani S, et al. Social stigma among tuberculosis patients attending DOTS centers in Delhi. J Family Med Prim Care. 2020;9(8):4223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cremers AL, Laat MM, De, Kapata N et al. Assessing the Consequences of Stigma for Tuberculosis Patients in Urban Zambia. PLoS One [Internet]. 2015 [cited 2020 Apr 19];10(3). https://pubmed.ncbi.nlm.nih.gov/25806955/. [DOI] [PMC free article] [PubMed]
- 70.Jing Teo AK, Jin Tan RK, Smyth C, et al. Characterizing and measuring tuberculosis stigma in the community: a mixed-methods study in Cambodia. Open Forum Infect Dis. 2020;7(10):p.ofaa422. https://academic.oup.com/ofid/article/7/10/ofaa422/5906589. [DOI] [PMC free article] [PubMed]
- 71.Zailani MAH, Sabudin RZAR, Rahman RA, et al. Drone for medical products transportation in maternal healthcare: a systematic review and framework for future research. Medicine. 2020;99(36):e21967. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.