Abstract
Acute Severe Hypertension (ASH), presenting as a Hypertensive Emergency (HE) or Hypertensive Urgency (HU), is a frequent reason for emergency department (ED) admissions. This study sought to assess the prevalence of ASH among adult ED patients in Pakistan and investigate all-cause mortality and hospitalization rates over six months. We conducted a prospective single-center cohort study in Karachi, Pakistan, from June 3, 2019, to September 22, 2020. We enrolled all adult male and non-pregnant female patients presenting to the emergency department with a systolic blood pressure of ≥180 mm Hg or diastolic blood pressure of ≥120 mm Hg. Telephonic follow-ups were conducted at one, three-, and six months post-discharge from the hospital. The Cox Regression Model was used to identify the risk factors for mortality. Of 49,431 ED visits during the study period, 1,525 (3.1%) met the inclusion criteria, and 1,161 (76.2%) were enrolled. A total of 356 patients (30.6%) were diagnosed with HE, and 805 (69.2%) with HU. Among follow-up patients, 14.6% with HE and 4.7% with HU experienced mortality within six months. Notably, the risk of mortality was higher in patients aged >65 years (aRR = 1.90, 95% CI = 1.20 to 3.02) and those suffering from stroke (aRR = 2.09, 95% CI = 1.21 to 3.61) or acute kidney injury (aRR = 1.82, 95% CI = 1.09 to 3.04). Conversely, regular blood pressure monitoring (aRR = 0.08, 95% CI = 0.03-0.19) and adherence to antihypertensive medications (aRR = 0.23, 95% CI = 0.09-0.56) significantly lowered the risk HE resulted in heightened mortality at six months, while HU, traditionally deemed benign, also led to substantial morbidity and mortality. This underscores the ED visit for ASH as a crucial opportunity for preventing short-term and longer-term health complications.
Introduction
Hypertension is the leading preventable risk factor for cardiovascular disease and all-cause mortality worldwide, affecting one-third of the global population, especially in low and middle-income countries (LMICs) [1–3]. Effective blood pressure control is a major public health objective aligned with the global Sustainable Development Goals [4].
Despite effective and affordable treatment, nearly a billion people globally have uncontrolled hypertension [5], and approximately 2% of these patients develop severe hypertension and represent up to 5% of emergency department (ED) admissions in some regions [6]. Data from high-income countries show an increasing trend for hypertension-related emergency visits and admissions [7, 8].
The diagnosis of Acute Severe Hypertension (ASH) or Hypertensive Crisis is assigned to individuals with systolic blood pressure > 180 mmHg or diastolic blood pressure > 120 mmHg. ASH is further stratified into Hypertensive Emergency (HE) or Hypertensive Urgency (HU), based upon the presence or absence of damage to vital end-organ such as the brain, retina, heart, blood vessels, or kidneys. While immediate and careful treatment of HE significantly improves outcomes, “urgency” in HU is increasingly scrutinized due to the absence of demonstrable benefits and the potential risks associated with immediate intervention for this "Markedly elevated BP" in acute settings [9, 10].
While Hypertensive Emergencies (HEs) are known to cause high in-hospital mortality rates, prospective data on the post-acute care outcomes of patients with HE and HU are notably absent, especially in LMICs [11–14]. Existing studies with follow-up data are predominantly derived from high-income countries, relying on retrospective and secondary data sources. Notably, these studies have limited follow-up periods, and only a few address patients with HU [15–23]. Our investigation aimed to address this gap in knowledge by assessing the prevalence of Acute Severe Hypertension (ASH) among adult patients presenting to the ED in Pakistan and quantifying all-cause mortality and hospitalizations over six months following their initial visits to the emergency department.
Methods
Study design and study population
This prospective observational study was conducted at the ED of Aga Khan University Hospital (AKUH) in Karachi, Pakistan, from June 3, 2019, to September 22, 2020, with an exclusion period from March 16, 2020, to July 28, 2020, due to the COVID-19 pandemic.
Setting
AKUH, a 710-bed private, fee-for-service teaching, and major referral hospital, meets the diverse healthcare needs of Karachi, a city with a population exceeding 20 million. AKUH’s ED annually attends to around 65,000 patients, representing a small yet notably sick and complex patient group, primarily composed of individuals from middle- and high-income groups. In contrast, most patients in Karachi depend on lower-cost government or neighborhood private health facilities for emergency care. The numbers seen in the ED decreased significantly during the COVID-19 pandemic. The care in the ED is provided by emergency medicine trainees/residents under the supervision of attendings/consultants 24/7. On arrival at the ED, triage nurses prioritize and document vital signs on all patients using the Emergency Severity Index (ESI) [24]. Those who are too unstable to wait at triage are brought directly to the resuscitation room as per the institutional protocol. Triage information, including vital signs, laboratory results, radiology reports, and pharmacy orders, are electronically recorded, while physician and nursing assessments are documented manually in paper files.
Participants
This study included all patients aged 18 years or older with triage systolic blood pressure readings of ≥180 mm Hg or diastolic blood pressure readings of ≥120 mm Hg. Only single blood pressure reading was taken at triage as obtaining multiple blood pressure readings for each patient during their initial assessment might introduce delays in patient care and require significantly increased resources. We excluded patients <18 years of age, pregnant women, and those who did not consent to participate or were triaged but admitted to the hospital without treatment in the ED. Pregnant patients were excluded as they followed a different care pathway in the ED. Written consent was obtained from all eligible patients or their next of kin. The data presented herein constitutes a segment of an intervention study designed to assess the impact of implementing an ED checklist on the practices and outcomes of patients presenting with acute severe hypertension. The primary findings from the intervention study will be detailed in a separate publication.
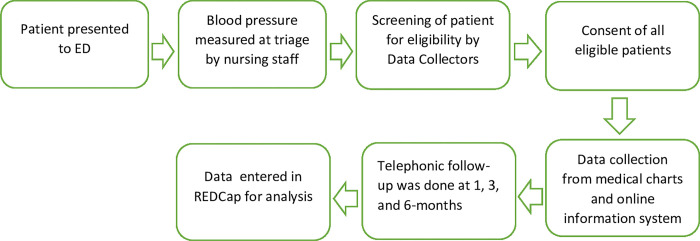
Data collection
Trained Research Assistants (RAs) conducted the 24/7 prospective enrollment of patients, identifying eligible individuals through electronically available triage vital signs. Data were not collected for 28 days due to public/religious holidays and during the initial 4 months and 12 days of the COVID-19 pandemic when all research was temporarily stopped to respond to the pandemic. Upon identifying a patient through triage records, the RAs introduced themselves to the patients or their families, explained the study’s purpose, answered questions, obtained written consent, and confirmed follow-up contact information. During the peak of the COVID-19 pandemic, verbal telephone-based consent was obtained in adherence to institutional guidelines and Institutional Review Board (IRB) approval.
RAs systematically collected demographic and clinical data during the ED visit, utilizing ED medical records for participants who consented to participate in the study. The clinical course was extracted from medical charts using study-specific data collection forms for patients admitted to the hospital. Patient outcomes at 1, 3, and 6 months were gathered prospectively via a structured questionnaire during telephonic interviews. All data was entered into the Research Electronic Data Capture (RED-Cap) [25].
To ensure data accuracy and consistency, all RAs underwent comprehensive training before data collection, covering study implementation processes and data collection procedures and using RED-Cap’s data entry functions. RAs were not blinded to the outcomes. A refresher training session addressed any issues encountered during data collection or entry. A project coordinator’s daily audit of all data forms served as a quality control measure.
After discharge from the ED or inpatient units, RAs called each patient at 1, 3, and 6 months post-discharge using the provided telephone numbers. To minimize loss to follow-up during telephonic follow-ups, RAs called patients three times on day 1, twice on days 2 and 3, and once each from days 4 to 14. Patients were deemed lost to follow-up if contact was not established within 14 days.
To mitigate the risk of over-diagnosing HE, each patient’s medical record underwent a thorough review by one of the two Emergency Medicine faculty members who were residency-trained and worked as supervising clinicians in the ED. The goal was to identify individuals with preexisting chronic kidney disease or a history of prior stroke to avoid misclassifying them as having a new end-organ damage as thus over-estimating the rates of HE. This was done through a joint review of medical records through in-person meetings by RAs and faculty members. Both Emergency Medicine faculty members were integral members of the study team and were familiar with the case definition as well as the inclusion and exclusion criteria. It is important to note that they were not blinded to the study objectives, and we did not formally assess the interrater reliability or agreement.
Study measures
HE was defined as triage SBP ≥180 mmHg or DBP ≥120 mm Hg associated with evidence of any of the following: hypertensive heart failure, cardiac ischemia evident by complaint of typical chest pain or angina equivalent symptoms associated with new electrocardiogram changes or elevated troponins, transient ischemic attack, hypertensive encephalopathy, subarachnoid hemorrhage, ischemic or hemorrhagic stroke, acute kidney injury as per the Kidney Disease Improving Global Outcome-KDIGO criteria, grade 3 to 4 hypertensive retinopathy and aortic dissection. Specifically, the KDIGO criteria (increase in serum creatinine of ≥ 0.3mg/dl within 48hrs; or increase in serum creatinine to ≥ 1.5 times of baseline which is known or presumed to have occurred within the prior 7 days; or urine volume <0.5 ml/kg/h for 6 hours) was used to define AKI [26]. Patients with SBP ≥180 mmHg or DBP ≥120 mm Hg at triage and no evidence of end-organ damage were labeled as HU. During the ED visit, we obtained data on age, gender, triage category, presenting complaint, comorbidities, use of antihypertensive medications and BP at triage, first BP when the patient was brought in the treatment area and a BP at the time of discharge or admission to the hospital. During telephone follow-ups, we collected data on outcomes such as death, readmissions to hospitals, frequency of monitoring of blood pressure (on a seven-point scale from daily BP checks to rarely), adherence to antihypertensive medications (yes vs. no), and follow-up with the primary physicians (three possible responses; visited once after discharge, visited twice after discharge, visited more than twice after discharge) (S1 File).
Statistical analysis
All data were collected on (REDCap) and analyzed using Stata-14 for statistical analysis [27]. After checking normality assumptions, descriptive statistics (mean, standard deviation, minimum, maximum, numbers, and percentage) were reported for continuous variables. We calculated frequencies for categorical variables and applied Kaplan-Meier plots to visualize the survival patterns. After selecting confounding indicators for the study, we did the univariate analysis, taking mortality as a dependent variable and selecting significant variables in the univariate model. Independent variables with a p-value of <0.2 were used in a multiple survival Cox regression model. We built multivariate models using the stepwise backward selection. The first set of models included all risk factors up to discharge from the hospital (e.g., male gender, age > 65, acute myocardial infarction, etc.)The second set of models included all risk factors till the follow-up (e.g., lack of home blood pressure monitoring, non-adherence to antihypertensive medications, lack of regular follow-up with primary care physician). Only variables with a p-value of ≤ 0.05 were kept in the model. The results were reported as relative risk (RR) with a 95% confidence interval. We performed sensitivity analysis where applicable, e.g., for HE and HU patients separately.
Ethics approval for the study was obtained by IRBs at the Aga Khan University and Johns Hopkins University.
Results
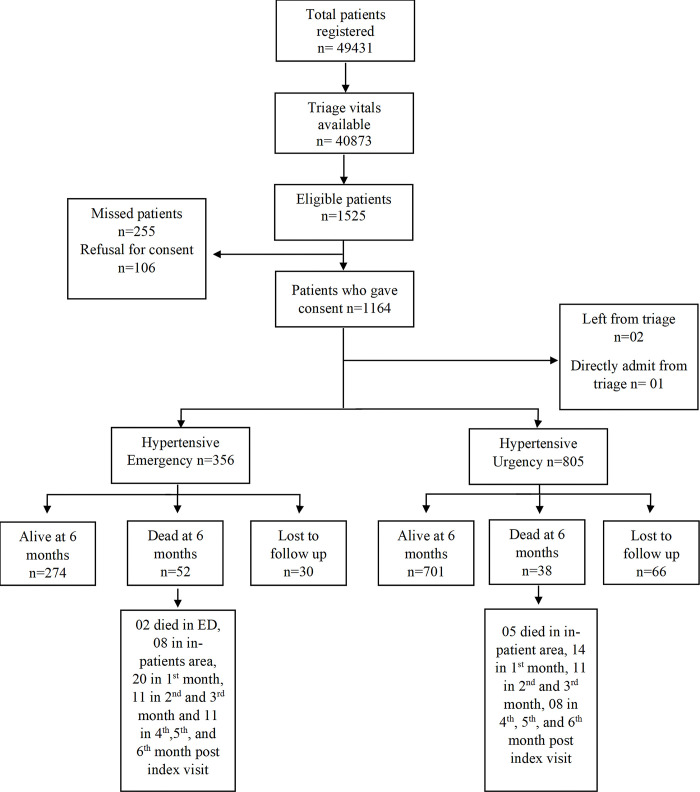
During the study period, 49,431 adult patients visited the ED, with triage vitals available for 40,873. Among them, 1,525 patients (3.7%) met the inclusion criteria. Due to the limited availability of RAs during holidays and some weekends, we approached 1270 patients, of which 1,164 patients (91.6%) provided consent for participation. Of these, two left ED after triage, and one was admitted directly to the hospital without any further ED management. The final cohort included 356 patients (30.6%) diagnosed with HE and 805 (69.2%) with HU. Six-month follow-up data was available for 1,065 patients (91.7%), with 326 (91.6%) in the HE and 739 (91.8%) in the HU group (Fig 1).
Fig 1. Patient enrollment and data collection information.
The mean age of the patients was 60.4 years (±14.33). Over half of the patients were females (n = 680, 59%), and 1007 (86.7%) were triaged as priority 1 and 2 on the ESI triage scale. The most common presenting complaint was nausea and vomiting (n = 177, 15.2%), followed by abdominal pain (n = 174, 15%) and chest pain (n = 143, 12.3%). Around 108 patients (9.1%) were asymptomatic at presentation. Most patients had a past medical history of hypertension (n = 972, 83.7%), and half had a history of diabetes (n = 569, 49%). Only 438 patients (37.7%) were taking antihypertensive medications. The most common end-organ damage was kidney (n = 153, 13.1%) followed by brain (n = 115, 9.9%) and heart (n = 109, 9.3%) (Table 1).
Table 1. Demographic and baseline health characteristics, and new-onset end-organ damage of the sample population (n = 1161).
| Characteristics | Results |
|---|---|
| Age in years (n, %) | |
| 18-34 | 52 (4.5) |
| 35-64 | 615 (53) |
| ≥65 | 494 (42.5) |
| Gender (n, %) | |
| Male | 481 (41.4) |
| Female | 680 (58.6) |
| Triage Category (n, %) | |
| -ESI 1 | 377 (32.5) |
| ESI 2 | 630 (54.3) |
| ESI 3 | 154 (13.3) |
| Presenting complaints (n, %) * | |
| Nausea and vomiting | 177 (15.2) |
| Abdominal pain | 174 (15) |
| Chest pain | 143 (12.3) |
| Shortness of breath | 142 (12.2) |
| Anxiety or vague discomfort (Ghabrahat in the Urdu language) | 120 (10.3) |
| High blood pressure | 108 (9.3) |
| Unilateral limb weakness | 92 (7.9) |
| Headache | 87 (7.5) |
| Injury/Accident/Fall | 86 (7.4) |
| Altered mental state | 80 (6.9) |
| Vertigo | 68 (5.9) |
| Fever | 63 (5.4) |
| Pain | 61 (5.2) |
| Generalized weakness | 46 (3.9) |
| Dysuria/Burning micturition | 43 (3.7) |
| Constipation/Diarrhea | 39 (3.3) |
| Others† | 109 (9.3) |
| Comorbidities (n, %) | |
| Hypertension | 972 (83.7) |
| Diabetes | 569 (49.0) |
| Ischemic heart disease | 213 (18.3) |
| Chronic kidney disease | 121 (10.4) |
| Cerebrovascular accident | 91 (7.8) |
| History of surgery | 53 (12) |
| Cancer | 52 (4.47) |
| Others ‡ | 210 (18.0) |
| Patients taking antihypertensive medications | 438 (37.7) |
| End organ damage (EOD) (n, %) | |
| Kidney | 153 (13.1) |
| Brain | 115 (9.9) |
| Heart | 109 (9.3) |
* Patient had the option of providing multiple responses.
† Slurring of speech, facial deviation/ swelling, GI/GU bleeding, epistaxis, decreased urine output, blurred vision, bilateral leg swelling, each under 2% of the total presenting chief complaints.
‡ Musculoskeletal disorders, asthma, thyroid disorders, chronic liver disease, dyslipidemia, smoking, psychiatric disorders, neurological disorders, hepatitis, chronic pulmonary obstructive pulmonary disease, overweight/ obesity, blood disorders, eye, interstitial lung disease, congenital disease each under 2% of all self-reported comorbidities
ESI: Emergency Severity Index
Regarding the outcomes, 52 patients (14.6%) with HE had passed away within the six months. Among these, two patients died in the ED, and eight during hospital admission. A significant portion of deaths occurred within the initial month (38.4%), followed by 21.1% in the second and third months, and another 21.1% in months 4-6 post-index visits.
In contrast, among patients with HU, 701 (87.0%) remained alive, while 38 (4.7%) had died and 66 (8.3%) were lost to follow-up. The majority of HU-related deaths occurred in the first-month post-discharge (36.8%), with additional occurrences between 1-3 months (28.9%) and 4-6 months (21.0%) post-index visits (Fig 2).
Fig 2. Patient distribution and outcomes.
Patients with HE had a three times higher risk of death than those with HU. Additionally, HE patients had a higher readmission rate (17.0%) compared to HU patients (11.6%). The primary causes of readmission included raised blood pressure (20.8%), acute myocardial infarction (7.1%), and kidney failure (9.4%).
More than 85% (n = 985) of all follow-up patients self-reported regularly monitored their blood pressure, and 84.1% (n = 930) of the patients also reported to be adherent with their antihypertensive medications prescribed at the time of discharge. The average medication adherence rate increased from 1st month to 3rd month for both HE and HU groups (83.7% to 93% and 87.4% to 93.9%). However, only 19.9% (n = 220) of the patients followed up with their primary physician during the six-month follow-up period (Table 2).
Table 2. Cumulative outcomes at six months follow-up.
| Outcomes | 1-month follow-up * | 3 months follow-up † | 6 months follow-up ‡ | |||
|---|---|---|---|---|---|---|
| N = 1051 | N = 1024 | N = 994 | ||||
| HE | HU | HE | HU | HE | HU | |
| 310 (30.0%) | 741 (70.0%) | 301 (29.3%) | 723 (70.7%) | 285 (28.6%) | 709 (71.4%) | |
| Checking BP regularly (n, %) | 277 (83.7) | 674 (87.4) | 280 (93.0) | 679 (93.9) | 266 (93.3) | 661 (93.2) |
| Taking antihypertensive medications regularly (n, %) | 270 (87.1) | 602 (81.2) | 268 (89.0) | 587 (81.2) | 255 (89.5) | 563 (79.4) |
| Followed-up with a primary physician (n, %) | 88 (28.4) | 177 (23.9) | 83 (27.6) | 180 (24.9) | 76 (26.7) | 150 (21.2) |
| Required admission to hospital (n, %) | 29 (9.4) | 31 (4.2) | 29 (9.6) | 44 (6.1) | 27 (9.5) | 44 (6.2) |
| Death (n, %) | 20 (6.5) | 14 (1.9) | 11 (3.7) | 11 (1.5) | 11 (3.9) | 8 (1.1) |
* 8.3% (n = 95) lost to follow-up at 1 month.
† 10.9% (n = 122) lost to follow-up at 3 months.
‡ 13.9% (n = 152) lost to follow-up at 6 months.
Univariate Cox regression analyses revealed a higher mortality risk for those aged 65 or older, with acute myocardial infarction, acute kidney injury, stroke, ED length of stay >6 hours, and a hospital stay >48 hours. Regular blood pressure monitoring, following up with a primary care physician, and adhering to antihypertensive medications were associated with reduced mortality risk (Table 3 and S1 Fig). Multivariable Cox regression identified age >65, stroke, acute kidney injury, non-monitored bed admission, and hospital stay >48 hours as predictors of higher mortality. Regular blood pressure monitoring and adherence to antihypertensive medications were associated with significantly lower mortality risk. Sensitivity analyses showed similar trends in HE and HU patients (Table 3).
Table 3. Univariate and multivariate Cox regression analysis for mortality.
| Factors before discharge | Mortality at six months | Univariate | Multivariate* | Multivariate† | |
|---|---|---|---|---|---|
| n | % | RR [95% CI] | RR [95% CI] | RR [95% CI] | |
| Male gender | 35 | 8 | 1.23 [0.78 -1.94] | - | - |
| Age ≥ 65 years | 43 | 10 | 2.22 [1.41 -3.50] | 1.90 [1.20 to 3.02] | - |
| Acute myocardial infarction | 13 | 12 | 2.84 [1.63 -4.81] | - | - |
| Acute Kidney Injury | 22 | 15 | 2.67 [1.62 -4.40] | 1.82 [1.09 to 3.04] | - |
| Stroke | 13 | 18 | 2.84 [1.67 -4.83] | 2.09 [1.21 to 3.61] | - |
| Admit to intensive care / special care | 18 | 16 | 1.11 [0.66 -1.89] | - | - |
| Admission to ward | 45 | 15 | 4.27 [2.69 -6.78] | 2.50 [1.48 to 4.24] | - |
| Length of hospital stay ≥ 48 hours | 51 | 13 | 4.11 [2.53 -6.69] | 1.95 [1.12 to 3.42] | - |
| Length of ER Stay ≥ 6 hours | 51 | 9 | 2.05 [1.26 -3.34] | - | - |
| Factors after discharge | |||||
| Readmission | 9 | 6 | 0.84 [0.42-1.69] | - | - |
| Regular monitoring of blood pressure | 16 | 2 | 0.03 [0.01-0.04] | - | 0.08 [0.03-0.19] |
| Followed up with primary care physician | 2 | 1 | 0.11 [0.03-0.44] | - | |
| Taking antihypertensive medications regularly | 15 | 2 | 0.04 [0.02-0.07] | - | 0.23 [0.09-0.56] |
* Risk factors prior to discharge
† Risk factors after discharge
The risks for mortality were much lower for those who regularly monitored their blood pressure (aRR = 0.08, 95%CI = 0.03-0.19) or reported adherence to antihypertensive medications (aRR = 0.23, 95%CI = 0.09-0.56) (Table 3). Sensitivity analyses showed similar trends in HE and HU patients (not shown as associations were not significant because of underpowered sample sizes).
Discussion
Our study reveals a remarkably high prevalence of Acute Severe Hypertension (ASH) in patients presenting to the study ED in Karachi, Pakistan. Of concern were the elevated six-month admission and mortality rates, observed not only among individuals with HE but also among patients with HU. Notably, one in six patients with HE and one in twenty with HU had succumbed during the six-month follow-up period. These findings underscore the pronounced short-term morbidity and mortality risks associated with hypertensive emergencies and urgencies, highlighting the critical importance of regular blood pressure monitoring and strict adherence to antihypertensive medications. This bears particular significance in the context of Pakistan, wheremore than 70% of the hypertensive population receiving treatment exhibits poorly controlled blood pressure [28].
The prevalence of Acute Severe Hypertension (ASH) among ED patients exhibits substantial global variation. In our study, which utilized triage blood pressure readings for patient inclusion, we identified a notable ASH prevalence of 37.3 per 1000 cases. This contrasts with reported rates ranging from 58 per 1000 ED visits in South Korea [17] to 0.64 per 1000 in Thailand [22]. The staggering 100-fold difference is unlikely to reflect a genuine discrepancy in prevalence across the general population in these regions but rather suggests methodological variations in the studies. These differences encompass factors such as the timing of blood pressure measurements during ED care, type of hospital, inclusion criteria, and patient demographics, particularly the average age of the ED population. Importantly, our study was conducted in a major referral center known for managing patients referred from other regional hospitals due to the complexity and acuity of illness, which may have potentially amplified the observed prevalence. To some extent, these differences also highlight a significant gap in hypertension management in primary care in different settings [29]. Addressing these discrepancies is crucial for a comprehensive understanding of ASH prevalence and ensuring effective hypertension management strategies across diverse healthcare settings.
We found a concerning six-month mortality rate amongst patients with ASH, including those with HU. In fact, in our population, mortality associated with HU was about 12 times the expected mortality in the general population [30]. Like prevalence, mortality rates across diverse settings exhibit significant variation due to differences in case definitions, follow-up duration, average age, preexisting morbidity, and the quality and availability of post-acute care in both inpatient and outpatient settings [15, 16, 18–20, 23]. Our inpatient mortality from HE aligns with high-resource settings [7, 19] and notably falls below reported rates in low-resource settings [13, 29]. Importantly, increased mortality in our population occurs during the post-discharge phase, emphasizing the potential impact of frequency of close post-discharge follow-up and the quality of care during the follow-up including inducement and encouragement regarding lifestyle changes and management of other cardiovascular risk factors using well-known evidence-based interventions [31]. We observed a higher mortality rate among patients admitted to the non-monitored bed. This was likely influenced by families choosing to restrict resuscitation measures for patients with low prospects of meaningful survival. Furthermore, AKUH is a private setup and individuals are required to pay directly for medical services. The increased financial burden associated with ICU care may influence families’ decisions regarding the level of care provided to their loved ones, particularly if they perceive limited prospects for meaningful recovery.
Our study carries significant implications for emergency care delivery, system design, and future research. Firstly, aligning with a growing body of literature, we assert that ED visits for patients with hypertensive urgencies represent a pivotal opportunity to identify high-risk individuals and intervene to prevent catastrophic outcomes [10, 21, 32, 33]. Achieving this necessitates the improved integration of EDs and primary care services through the adaptation of proven active and passive mechanisms. These include establishing ED-based follow-up clinics, implementing rapid scheduling of appointments for discharged patients [34], deploying care navigators to facilitate identification and referral to appropriate primary care settings [35], and using community resources such as community health workers [36]. Once engaged with primary care providers, there is a need to advocate for practical and feasible lifestyle modifications, particularly for individuals residing in high-density urban environments, while also recognizing and aggressively addressing cardiovascular complications [37].
For the research community, achieving harmonization in ED-based diagnoses and case definitions is essential for advancing the field. While discarding the term "Hypertensive Urgency" is appropriate to prevent aggressive blood pressure lowering in the acute care setting, it remains crucial to emphasize that the condition is urgent, requiring close outpatient follow-up. Further exploration is warranted to understand barriers hindering the successful transition of care, encompassing factors such as cost, transportation, and patient awareness. Additionally, elucidating the role of newer options, particularly telemedicine, holds significance, especially for individuals with hypertensive urgencies, and combining them with the traditional role of community health workers who could assist with ensuring follow-up with primary care and sustainable lifestyle changes.
Lastly, given the constraints of critical care resources, there is merit in sub-categorizing patients with hypertensive emergencies who can be managed in alternative settings outside of an intensive care unit without worsening outcomes. This categorization could serve as a valuable guide for resource allocation, optimizing patient care in situations where critical care resources are limited.
Our study is subject to several limitations. Firstly, being a single-center study based at a fee-for-service, referral center, it likely represents a sicker and relatively higher-income urban population. This may not fully capture the socio-economic diversity across urban and rural areas of Pakistan. Nevertheless, given the relatively privileged socio-economic group seen in this ED, we suspect that rates of undiagnosed and untreated hypertension and challenges in ensuring follow-up are likely higher in less privileged populations.
Secondly, our follow-up data on compliance with BP measurement and medication adherence were self-reportedand appear to be higher than reported for the general population [38]. However, only 21-28% of the patients followed up with their primary physician. In Pakistan, medications are readily available without prescription at pharmacies which could explain the disparity between follow-up with doctors and medication usage. Moreover, these patients had a perceived life-threatening event requiring an ED visit which could have played a role in higher compliance. Additionally, we observed an increase in self-reported compliance with BP home monitoring and medication adherence during subsequent calls, possibly influenced by the Hawthorne effect or patients’ over-reporting for fear of judgment by the interviewers or social desirability bias [39–41]. Also, we recognizethat the interpretation of “taking medications regularly” and "regularly monitored blood pressure" may vary among patients. The term "regularly" may have been subject to individual interpretation, leading to potential misclassification bias in self-reported responses.
Finally, due to the limitation of telephone conversations, we opted to limit the call duration and only collect data on rates of death, and self-reported causes of death without getting details surrounding the circumstances of death. This limitation hinders the direct attribution of death to cardiovascular complications and, consequently, the assessment of the preventability of these deaths. The study identifies potential health system weaknesses, but further specific information elucidating the breaks in the care pathway and understanding the circumstances surrounding readmission and death need to be investigated. Additionally, we acknowledged the occurrence of COVID-19 during the study, comparing mortality before and during the pandemic, revealing no significant differences between the two populations. Nevertheless, the elevated all-cause mortality and readmission rates underscore the necessity for a more profound understanding of the circumstances surrounding readmission and death.
Conclusion
In summary, our investigation revealed a high prevalence of acute severe hypertensionin our patient cohort-, concomitant with increased six-month mortality and hospitalization rates. This emphasizes the ED visit for Acute Severe Hypertension (ASH) as a potential critical opportunity for averting both short-term and longer-term health complications. The results underscore the significance of a more in-depth exploration of the determinants leading to poor outcomes and advocate for the implementation of established interventions for outpatient management of hypertension among patients discharged from ED.
Supporting information
(TIFF)
(PDF)
Data Availability
The data on Weill Cornell Medicine(WCM) data catalog is accessible through WCM login credentials or through the request. Please find attached the link to our data repository: https://datacore.weill.cornell.edu/datacatalog/datasets/125.
Funding Statement
Research reported in this publication was supported by the Fogarty International Center of the National Institutes of Health under Award Number R21TW011175 to JR. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Olsen MH, Angell SY, Asma S, Boutouyrie P, Burger D, Chirinos JA, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. The Lancet. 2016;388(10060):2665–712. doi: 10.1016/S0140-6736(16)31134-5 [DOI] [PubMed] [Google Scholar]
- 2.Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16(4):223–37. doi: 10.1038/s41581-019-0244-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398(10304):957–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Organization WH. Global NCD target: reduce high blood pressure. World Health Organization; 2016. [Google Scholar]
- 5.Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134(6):441–50. doi: 10.1161/CIRCULATIONAHA.115.018912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Janke AT, McNaughton CD, Brody AM, Welch RD, Levy PD. Trends in the incidence of hypertensive emergencies in US emergency departments from 2006 to 2013. Journal of the American Heart Association. 2016;5(12):e004511. doi: 10.1161/JAHA.116.004511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deshmukh A, Kumar G, Kumar N, Nanchal R, Gobal F, Sakhuja A, et al. Effect of Joint National Committee VII report on hospitalizations for hypertensive emergencies in the United States. The American journal of cardiology. 2011;108(9):1277–82. doi: 10.1016/j.amjcard.2011.06.046 [DOI] [PubMed] [Google Scholar]
- 8.Polgreen LA, Suneja M, Tang F, Carter BL, Polgreen PM. Increasing trend in admissions for malignant hypertension and hypertensive encephalopathy in the United States. Hypertension. 2015;65(5):1002–7. doi: 10.1161/HYPERTENSIONAHA.115.05241 [DOI] [PubMed] [Google Scholar]
- 9.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr., Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):2199–269.29146533 [Google Scholar]
- 10.Miller J, McNaughton C, Joyce K, Binz S, Levy P. Hypertension Management in Emergency Departments. Am J Hypertens. 2020;33(10):927–34. doi: 10.1093/ajh/hpaa068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Almas A, Ghouse A, Iftikhar AR, Khursheed M. Hypertensive crisis, burden, management, and outcome at a tertiary care center in karachi. International journal of chronic diseases. 2014;2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abdallah T, Ibrahem A, A A, G A, A A. Clinico-epidemiological characteristics and survival outcome of patients with hypertensive crisis at Kassala Hospital, Eastern Sudan. Journal of Clinical Intensive Care and Medicine. 2018;3:029–34. [Google Scholar]
- 13.García GM, Miúdo V, Lopes CdGAM, Gomes JV. Characterization of patients aged 45 or under admitted with hypertensive emergencies in the Hospital do Prenda. Revista Portuguesa de Cardiologia (English Edition). 2014;33(1):19–25. [DOI] [PubMed] [Google Scholar]
- 14.Kadima JN, Bavhure B, Sepa JD, Murhura D. Hypertensive urgencies or emergencies and co-morbidities in Bukavu Referral Hospitals: clinical profile, management regimens, outcomes and drug related problems. Journal of Basic and Clinical Pharmacy. 2018;9(1). [Google Scholar]
- 15.Merlo C, Bally K, Martina B, Tschudi P, Zeller A. Management and outcome of severely elevated blood pressure in primary care: a prospective observational study. Swiss medical weekly. 2012;142(0304). doi: 10.4414/smw.2012.13507 [DOI] [PubMed] [Google Scholar]
- 16.Guiga H, Decroux C, Michelet P, Loundou A, Cornand D, Silhol F, et al. Hospital and out‐of‐hospital mortality in 670 hypertensive emergencies and urgencies. The Journal of Clinical Hypertension. 2017;19(11):1137–42. doi: 10.1111/jch.13083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim BS, Kim HJ, Shin JH, Lee JH, Kim W, Park JK, et al. Sex Differences in Long-Term Mortality of Patients with Hypertensive Crisis Visiting the Emergency Department. J Womens Health (Larchmt). 2022. Aug;31(8):1137–1144. doi: 10.1089/jwh.2021.0430 Epub 2021 Dec 2. . [DOI] [PubMed] [Google Scholar]
- 18.Shin JH, Kim BS, Lyu M, Kim HJ, Lee JH, Park JK, et al. Clinical Characteristics and Predictors of All-Cause Mortality in Patients with Hypertensive Urgency at an Emergency Department. J Clin Med. 2021;10(19). doi: 10.3390/jcm10194314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Katz JN, Gore JM, Amin A, Anderson FA, Dasta JF, Ferguson JJ, et al. Practice patterns, outcomes, and end-organ dysfunction for patients with acute severe hypertension: the Studying the Treatment of Acute hyperTension (STAT) registry. Am Heart J. 2009;158(4):599–606.e1. doi: 10.1016/j.ahj.2009.07.020 [DOI] [PubMed] [Google Scholar]
- 20.Lin YT, Liu YH, Hsiao YL, Chiang HY, Chen PS, Chang SN, et al. Pharmacological blood pressure control and outcomes in patients with hypertensive crisis discharged from the emergency department. PLoS One. 2021;16(8):e0251311. doi: 10.1371/journal.pone.0251311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oras P, Häbel H, Skoglund PH, Svensson P. Elevated Blood Pressure in the Emergency Department: A Risk Factor for Incident Cardiovascular Disease. Hypertension. 2020;75(1):229–36. doi: 10.1161/HYPERTENSIONAHA.119.14002 [DOI] [PubMed] [Google Scholar]
- 22.Kotruchin P, Mitsungnern T, Ruangsaisong R, Imoun S, Pongchaiyakul C. Hypertensive Urgency Treatment and Outcomes in a Northeast Thai Population: The Results from the Hypertension Registry Program. High Blood Press Cardiovasc Prev. 2018;25(3):309–15. doi: 10.1007/s40292-018-0272-1 [DOI] [PubMed] [Google Scholar]
- 23.Vlcek M, Bur A, Woisetschläger C, Herkner H, Laggner AN, Hirschl MM. Association between hypertensive urgencies and subsequent cardiovascular events in patients with hypertension. J Hypertens. 2008;26(4):657–62. doi: 10.1097/HJH.0b013e3282f4e8b6 [DOI] [PubMed] [Google Scholar]
- 24.Shelton R. The Emergency Severity Index 5-level triage system. Dimens Crit Care Nurs. 2009;28(1):9–12. doi: 10.1097/01.DCC.0000325106.28851.89 [DOI] [PubMed] [Google Scholar]
- 25.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clinical Practice. 2012. Oct 1;120(4):c179–84. doi: 10.1159/000339789 [DOI] [PubMed] [Google Scholar]
- 27.StataCorp L. Stata statistical software. College Station TX. 2009. [Google Scholar]
- 28.Jafar TH, Gandhi M, Jehan I, Naheed A, de Silva HA, Shahab H, et al. Determinants of uncontrolled hypertension in rural communities in South Asia—Bangladesh, Pakistan, and Sri Lanka. American journal of hypertension. 2018;31(11):1205–14. doi: 10.1093/ajh/hpy071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shao PJ, Sawe HR, Murray BL, Mfinanga JA, Mwafongo V, Runyon MS. Profile of patients with hypertensive urgency and emergency presenting to an urban emergency department of a tertiary referral hospital in Tanzania. BMC cardiovascular disorders. 2018;18(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pakistan TWB. [Available from: https://data.worldbank.org/country/pakistan.
- 31.Kim H-J, Kim BS, Shin J-H. Clinical characteristics and prognosis of patients with very severe acute hypertension visiting the emergency department. Clinical Hypertension. 2022;28(1):23. doi: 10.1186/s40885-022-00208-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pierin AMG, Flórido CF, Santos JD. Hypertensive crisis: clinical characteristics of patients with hypertensive urgency, emergency and pseudocrisis at a public emergency department. Einstein (Sao Paulo). 2019;17(4):eAO4685. doi: 10.31744/einstein_journal/2019AO4685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goldberg EM, Wilson T, Saucier C, Brody AM, Levy PD, Eaton CB, et al. Achieving the BpTRUth: emergency department hypertension screening and the Centers for Medicare & Medicaid Services quality measure. J Am Soc Hypertens. 2017;11(5):290–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carmel AS, Steel P, Tanouye R, Novikov A, Clark S, Sinha S, et al. Rapid Primary Care Follow-up from the ED to Reduce Avoidable Hospital Admissions. West J Emerg Med. 2017. Aug;18(5):870–877. doi: 10.5811/westjem.2017.5.33593 Epub 2017 Jul 14. ; PMCID: PMC5576623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jiang LG, Zhang Y, Greca E, Bodnar D, Gogia K, Wang Y, et al. Emergency Department Patient Navigator Program Demonstrates Reduction in Emergency Department Return Visits and Increase in Follow-up Appointment Adherence. Am J Emerg Med. 2022. Mar;53:173–179. doi: 10.1016/j.ajem.2022.01.009 Epub 2022 Jan 12. . [DOI] [PubMed] [Google Scholar]
- 36.Dye CJ, Williams JE, Evatt JH. Improving Hypertension Self-Manageement With Community Health Coaches. Health Promotion Practice. 2015. Mar;16(2): 271–281 [DOI] [PubMed] [Google Scholar]
- 37.Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75(6):1334–57. doi: 10.1161/HYPERTENSIONAHA.120.15026 [DOI] [PubMed] [Google Scholar]
- 38.Choudhry N.K., Kronish I.M., Vongpatanasin W., Ferdinand K.C., Pavlik V.N., Egan B.M., et al. 2022. Medication adherence and blood pressure control: a scientific statement from the American Heart Association. Hypertension, 79(1), pp.e1–e14. doi: 10.1161/HYP.0000000000000203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stirratt MJ, Dunbar-Jacob J, Crane HM, Simoni JM, Czajkowski S, Hilliard ME, et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med. 2015 Dec;5(4):470–82. doi: 10.1007/s13142-015-0315-2 Epub 2015. Jul 9. ; PMCID: PMC4656225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. 2014. Mar;67(3):267–77. doi: 10.1016/j.jclinepi.2013.08.015 Epub 2013 Nov 22. ; PMCID: PMC3969247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Adams S. A., Matthews C. E., Ebbeling C. B., Moore C. G., Cunningham J. E., Fulton J., et al. (2005). The effect of social desirability and social approval on self-reports of physical activity. American Journal of Epidemiology, 161(4), 389–398. doi: 10.1093/aje/kwi054 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIFF)
(PDF)
Data Availability Statement
The data on Weill Cornell Medicine(WCM) data catalog is accessible through WCM login credentials or through the request. Please find attached the link to our data repository: https://datacore.weill.cornell.edu/datacatalog/datasets/125.