Abstract
Introduction:
Dermoscopy of mucosa is known as mucoscopy. Mucoscopy can aid in delineating minute aspects of mucosal lesions and will guide in the differentiation of similar-looking lesions. To date, there are only a few studies on mucoscopy of genital dermatoses especially from India.
Aim and Objectives:
The study aims to describe mucoscopic features and correlate histopathologically in various genital mucosal diseases.
Materials and Methods:
The study was conducted in a tertiary care center in Central India after IHEC approval between October 2020 and April 2022, and the sampling technique was based on a convenience purposive method. Any genital mucosal diseases were included in patients above 18 years of age. Sexually transmitted diseases in general were excluded, however, warts and molluscum contagiosum were included. All patients fulfilling the inclusion criteria were examined after proper informed consent, and the clinical images were photographed using iPhone 11. Dermoscopic images were taken using a DermLite DL4 dermoscope in polarized mode at 10X magnification.
Results:
A total of 206 patients were recruited, and mucoscopy features were analyzed. Dermoscopic findings of physiological conditions such as vestibular papillomatosis, pearly penile papules, and Fordyce spots were evaluated. Inflammatory conditions such as lichen planus, pemphigus, and psoriasis were analyzed. Mucoscopy of lichen sclerosus showed white structureless areas (100%), follicular plugs (35%), as well as dotted and linear vessels (80%). Circinate balanitis revealed regular red dotted vessels (100%), coalescing pustules in annular and polycyclic patterns (90%). Squamous cell carcinoma of the penis showed ulceration, serpentine, looped vessels, white structureless area, and yellow-brown crust in a pink background.
Limitations:
In our study, because of the inclusion of various diseases, sample size was inadequate, biopsies were not performed in all cases, and variations in mucoscopic features in patients who are already on therapy could not be assessed. Haziness while capturing pictures because of mist formation was hindering the quality of pictures. As patients with premalignant and malignant cases were less, the predicting features for malignant transformation or pathognomoniic signs could not be assessed.
Conclusion:
Various dermoscopies have been studied extensively, but the mucoscopy is still a gray area. The results of this study revealed the dermoscopic features of various genital disorders and histopathological correlation in few cases. However, biopsy was not performed in all mucosal disorders; hence, conclusive correlation could not be extrapolated.
Keywords: Dermoscopy, genital dermatoses, mucosal dermatoses, mucoscopy, nonvenereal dermatoses
Introduction
Dermoscope is a noninvasive diagnostic imaging tool with inbuilt illumination and magnifying systems that enables the visualization of superficial and deeper structures and various pigmentary and vascular patterns of the skin, nail, hair, and mucosa (mucoscopy).
Genital mucosal lesions are abnormal alterations in color, surface, presence of swelling, or loss of integrity of the mucosal and semimucosal surfaces. Sometimes mucosal dermatoses are difficult to distinguish clinically and can cause a diagnostic dilemma. Some of the disorders that can mimic each other are vestibular papillomatosis in females and pearly penile papules in males with verruca vulgaris. Fordyce spots with molluscum and lichen sclerosus et atrophicus with vitiligo vulgaris need to be differentiated. A literature search on mucoscopy showed limited case reports, case series, and observational studies on genital diseases. The main aim of our study was to describe the mucoscopic features in the various genital mucosal dermatoses, distinguish the similar-looking lesion, and summarize the characteristic features obtained in the study.
Mucoscopy can aid in delineating minute aspects of these lesions and will guide in the differentiation of similar-looking lesions. It can also help in selecting a representative site for the biopsy of suspicious lesions and can also aid in remote consultation. The primary objective of the study was to describe the mucoscopic features in various genital mucosal dermatoses, and the secondary objective was to correlate mucoscopic features with histopathology.
Materials and Methods
The study was conducted in tertiary care center in Central India after institutional ethics committee approval between October 2020 and April 2022, and sampling was based on a convenience purposive method. Any patients with mucosal disease receiving treatment or planned to receive treatment, of age more than 18 years were included. The patients with clinically diagnosed cases of sexually transmitted diseases except for warts and molluscum were excluded. All patients fulfilling the inclusion criteria were examined after proper informed consent and the clinical images were photographed using iPhone 11. Dermoscopic images were taken using a DermLite DL4 dermoscope in both polarized and nonpolarized mode at 10X magnification. Under proper sterile conditions, after local anesthesia, a punch/excision biopsy was performed from the suspected site. The vascular pattern such as dotted vessels, linear vessels, telangiectasia, hairpin, and glomeruloid vessels was analyzed. Nonvascular patterns such as ovoid structures, dots, globules, structureless areas, pigment networks, and margins were described. The dermoscopic features were compared with histopathological slides in the presence of a pathologist.
Statistical analysis: All the data were collected in a proforma, which were entered into Excel sheet. The percentage (proportion) appearance of positive mucoscopic features in various mucosal disorders were analyzed.
Results
The distribution of various mucosal diseases and demographic details were tabulated in Table 1. Of 206 patients, 71 were females, and the rest were males with a 1.8:1, male-to-female ratio. Of 206 cases, 41 patients underwent biopsy, and the rest of 165 patients denied genital biopsy.
Table 1.
The demographic details and distribution of various mucosal diseases
| Disease | n (200) | % | Male: Female | Average age |
|---|---|---|---|---|
| Lichen sclerosus et atrophicus | 27 | 13.5 | 15:12 | 37.29±14.27 |
| Warts | 24 | 12 | 17:5 | 47.67±17.9 |
| Vitiligo | 22 | 11 | 14:8 | 42±13.5 |
| Circinate balanitis | 21 | 10.5 | 21:0 | 35.23±12.56 |
| Vestibular papillomatosis | 14 | 7 | 0:14 | 29.5±7.95 |
| Pemphigus vulgaris | 12 | 6 | 8:4 | 44.85±16.60 |
| Pseudoepitheliomatous keratotic micaceous balanitis | 12 | 6 | 12:0 | 67±5.85 |
| Zoon’s balanitis | 11 | 5.5 | 11:0 | 57±5.05 |
| Pearly penile papules | 9 | 4.5 | 9:0 | 25.34±6.83 |
| Lichen Planus | 6 | 3 | 2:4 | 48±16 |
| Psoriatic balanitis | 6 | 3 | 6:0 | 30.83±9.06 |
| Squamous cell carcinoma | 6 | 3 | 5:1 | 53.67±9.16 |
| Bowen | 6 | 3 | 0:6 | 39.5±14.5 |
| Lymphangioma circumscriptum | 5 | 2.5 | 5:0 | 24.85±16.60 |
| Hansen | 5 | 2.5 | 5:0 | 54.16±18.44 |
| Molluscum contagiosum | 4 | 2 | 0:4 | 32±9.88 |
| Fordyce spots | 3 | 1.5 | 0:3 | 35.23±12.56 |
| Steven Johnson syndrome | 2 | 1 | 1:1 | 39.87±11.58 |
| Fixed drug eruption | 2 | 1 | 2:0 | 26.5±7.18 |
| Hidradenoma papilliferum | 2 | 1 | 0:2 | 50±10 |
| Granular cell tumor | 1 | 0.5 | 0:1 | 45 |
Physiological conditions
-
Fordyce spots:
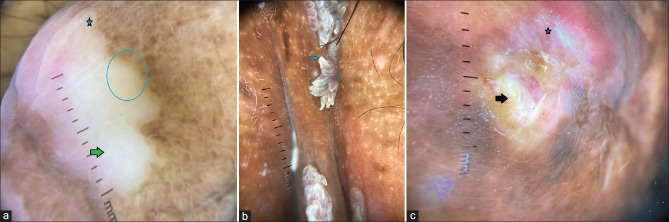
On mucoscopy of Fordyce spots, white yellow discrete globule (100%) and central white dots (33.34%) were noted. Linear vessels (33.34%) were the most common vasculature seen [Figure 1a].
-
Pearly penile papules [PPP]:
The mucoscopy features showed transparent white structureless areas (100%), with hairpin vessels (22.23%)/linear curved vessels (33.34%)/dotted vessels (33.34%) with bulbous tips (100%), and separate bases (100%) [Figure 1b].
-
Vestibular papillomatosis:
Mucoscopy features of fourteen cases of vestibular papillomatosis were finger-like transparent projection (100%) with round tips and individual bases with a dichotomous or linear fibrovascular core (71.43%). Of 14 cases, two cases underwent biopsy, in which finger-like projections corresponded to papillary projections, and linear vascular structure correlated with the fibrovascular core histologically [Figure 1c]
Figure 1.
(a) Mucoscopy of Fordyce spots over labia revealing white yellow discrete dots [circle] with linear vessels at the periphery (DermLite DL4, polarized mode, 10x). (b) Mucoscopy of pearly penile papules showing transparent white structureless projections (blue arrow), dot vessels (red star), with bulbous tips and separate bases (DermLite DL4, Polarized mode 10x). (c) Mucoscopic features of vestibular papillomatosis showing finger-like transparent projection (green arrow) with round tips and individual bases with linear vascular core (red arrow) [DermLite DL4, polarized mode 10x]
Inflammatory mucosal disorders
-
Circinate balanitis:
All cases recruited were clinically confirmed cases of reactive arthritis. Mucoscopy showed coalescing pustules in an annular to polycyclic fashion (100%), with regular red dotted vessels (100%) [Figure 2a].
-
Pemphigus vulgaris: (novel)
Blood spots (100%), red structureless area (100%), and red dots (71%), with violaceous radial lines at the periphery (78%), were noted from the erosions not from intact bullae of the pemphigus lesions. The presence of violaceous radial lines at the periphery mimics erosive lichen planus hence labeled as pseudo-Wickham.
-
Lichen planus:
Reticulate lichen planus, erosive, and annular variants of lichen planus were seen in our study in decreasing order of frequency.
The dermoscopic features of lichen planus were white structureless areas (41%), white radial lines (65%), and Wickham’s striae in reticulate variant and annular (4 cases). However, tricolor pattern [1) structureless veil-like gray-white to bluish white areas, 2) bright red slightly depressed areas, and 3) interspersed violaceous-to-brown clods] were seen in erosive variant (2 cases).
-
Lichen sclerosus et atrophicus:
Among 27 patients recruited in our study, itching (59.28%) and ulceration (59.28%) were the most common symptoms. Purpuric red dots and globules (59.26%), linear vessels (59.26%), white structureless area (100%), follicular plugging (44.45%), and occasional gray-blue dots in clustering pattern (59.26%) were seen [Figure 2b]. The mucoscopic features of the white structureless area corresponds to underlying dermal sclerosis, gray-blue dots correlate with dermal melanophages, superficial erosion corresponded to epithelial discontinuity, and follicular plugging was analogous to keratin plug histopathologically [Supplementary Figures 1 (355.3KB, tif) and 2 (226.6KB, tif) ].
-
Psoriatic balanitis:
We observed dermoscopic features of psoriatic balanitis as homogeneously distributed, dotted vessels (100%), with white scales (50%) in red background (100%).
Figure 2.
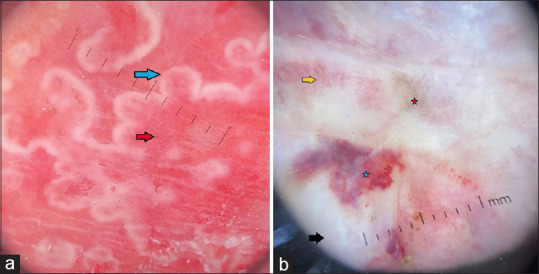
(a) Mucoscopic features of circinate balanitis showing coalescing pustules in annular to polycyclic fashion (blue arrow), with regular red dotted vessels (red arrow) [DermLite DL4, polarized mode 10x]. (b) Mucoscopic features in late LSA showing purpuric red dots, blotches (blue star), white structureless area (black arrow), occasional gray-blue dots in peppering pattern (red star), and linear and hairpin vessels (yellow arrow) [DermLite DL4, polarized mode, 10x]
Pigmentary dermatoses
-
Vitiligo:
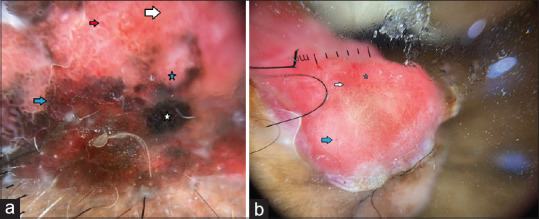
Dermoscopy features were absent pigment network (100%), diffuse white structureless areas (100%), with scalloped margin (77%), satellite white macules (54.54%), and micro koebnerization (22.72%) among 22 patients [Figure 3a].
Figure 3.
(a) The mucoscopic features of vitiligo showing trichrome pattern (blue circle), white glow (green arrow), and scalloped margin (blue star) [DermLite DL4, polarized mode 10x]. (b) Mucoscopy of verruca vulgaris depicting hyperkeratotic pointed tips (blue arrow), fused base (blue circle). [DermLite DL4, Polarized 10x]. (c) Mucoscopy of Hansen disease revealing yellow white structureless area (black arrow) and orange yellow hue (blue star) [DermLite DL4, Polarized 10x]
Infectious dermatoses
-
Molluscum contagiosum:
Dermoscopy of six cases of molluscum showed a central white structureless area (100%), with crown vessels (50%), which correspond to cytoplasmic inclusions and ectatic vessels, respectively. Rosette was seen in all cases (100%).
-
Mucosal warts
Verruca showed white perpendicular nontranslucent projections with pointed hyperkeratotic tips and fused base [Figure 3b].
-
Hansen’s disease: [Novel]
Dermoscopy from the glans of all male patients showed a yellow-white area and orange hue (100%) with brown scales (50%) [Figure 3c].
Vascular and lymphatic mucosal dermatoses
-
Lymphangioma circumscriptum/lympangiectasia:
Dermoscopy revealed pale yellow structureless areas with white lines.
Premalignant and malignant disorders
-
Bowen’s disease:
All the mucosal Bowen’s disease involves the vulva. Itching and burning were the most common symptoms seen. Black radial lines (100%), black interlacing pattern (83.34%), and characteristic coiled vessels (83.34%), with occasional comedo-like openings (16.67%), were noted. In our study, the mucoscopy feature of coiled vessels and dotted vessels correspond to underlying vasculature, and reticular network correlates with basal hyperpigmentation [Figure 4, Supplementary Figure 3 (234.3KB, tif) ].
-
Squamous cell carcinoma:
Mucoscopic features such as yellow-white crust, polymorphic vessels, erythematous structureless area, and red dots correspond to fibrin, vasculature, crust, squamous eddies, and RBCs exudate histologically [Figure 4b].
-
Granular Cell Tumor:
A single case of an asymptomatic skin-colored palpable nodule over right labia majora measuring 0.5 × 0.5 cm reveals a yellowish-white to yellow structureless area with the peripheral hyperpigmented rim on mucoscopy, which correspond to nests of granular cells histologically.
-
Hidradenoma papilliferum:
Two cases of vulval HP on mucoscopy showed central linear curved vessels with pink structureless areas with peripheral shiny white areas. Here, central linear curved vessels correspond to the fibrovascular core, and pink structureless areas correspond to the cystic space histopathologically [Figure 5a, Supplementary Figure 4 (238.3KB, tif) ].
-
Pseudoepitheliomatous Keratotic Micaceous Balanitis:
Mucoscopic features were half white area (100%), heaped-up yellow scales (100%), hairpin vessels (33%), red dots (25%), and polymorphic vessels (25%). The appearance of polymorphic vessels and hairpin vessels was suggestive of underlying premalignant condition [Figure 5b]. Biopsy was performed in all cases to rule out lichen sclerosus and malignant changes.
Figure 4.
(a) Mucoscopic features of Bowens disease depicting blue gray dots and globules (blue arrow), hair pin vessels (red arrow), red structureless areas (white arrow), white structureless areas (blue star), and black structureless areas (white star) [DermLite DL4, Polarized 10x]. (b) Mucoscopy of SCC revealing polymorphic vessels (star area), blood spots (white arrow), and erythematous structureless area (blue arrow) [DermLite DL4, polarized 10X]
Figure 5.
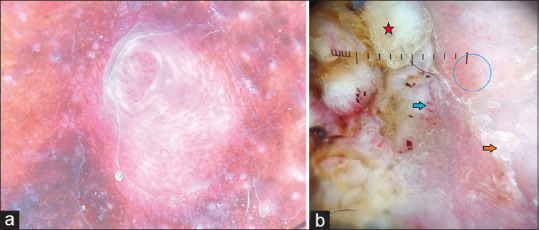
(a) Hidradenoma papilliferum on mucoscopy showing central irregular linear vessels with pink structureless areas with peripheral shiny white areas [DermLite DL4, Polarized 10X] (b) Mucoscopy of PKMB showing red dots in irregular pattern (blue circle), heaped up yellow crust (red star), hair pin vessels (blue arrow) with half white structureless areas (yellow arrow) [DermLite DL4, polarized 10x]
Drug reactions
-
Fixed Drug Eruption
Blue-gray dots to brown-black dots in a random pattern at the central part of the pigmented region of plaque and red structureless area with red dots at the periphery were recorded in a single case.
-
Steven Johnson Syndrome: (novel)
Dermoscopy was nonspecific, which showed red structureless area (100%), dotted vessels (62.5%), and blood spots (37.5%). The mucoscopic features of various genital mucosal dermatoses were summarized in Table 2. Table 3 summarizes the dermoscopic and histopathological correlation of lesions of genital mucosa.
Table 2.
The dermoscopic features of various mucosal dermatoses
| Type | Disorders | Dermoscopic features |
|---|---|---|
| Physiological | Vestibular papillomatosis | Fingerlike transparent projection with round tips individual bases with dichotomous or linear fibrovascular core |
| Pearly penile papules | Transparent white structureless areas with hairpin vessels/comma/dot vessels with bulbous tips, separate bases | |
| Fordyce spots | White yellow discrete ovoid structures (clods) with central opacity (dots) with or without linear and branching vessels at the periphery | |
| Inflammatory | Pemphigus vulgaris | No specific features were identified, bleeds heavily on placing dermoscope in most cases. Blood spots, red structureless area, red dots, with violaceous streaks at periphery (pseudo-Wickham’s) |
| Lichen planus | Tricolor pattern, Wickham’s striae, with violaceous background. | |
| Lichen sclerosus et atrophicus | Purpuric red dots, blotches, white structureless area, follicular plugging, occasional gray blue dots in peppering pattern | |
| Circinate balanitis | Coalescing pustules in annular to polycyclic fashion, with regular red dotted vessels. | |
| Zoon’s balanitis | Orange/red area with serpiginous vessels. | |
| Psoriatic balanitis | Homogeneously distributed red dotted vessels with or without white scales. | |
| Infectious conditions | Warts | Hyperkeratotic pointed tips with fused bases, with central thrombosed capillaries, few are giving mosaic appearance. |
| Molluscum contagiosum | Central pore-like structure with crown vessels. | |
| Hansen’s disease | Yellow-white area and orange hue with or without scales. | |
| Pigmentary dermatoses | Vitiligo | White structureless area, diffuse white glow with scalloped margin, comet tail and leukotrichia. |
| Premalignant and malignant disease | Bowens | Pigment streaks, reticular network, characteristic glomerular vessels, with occasional comedo-like openings. |
| Squamous cell carcinoma | Milky red structureless areas, keratin scale, polymorphous (dotted and linear) vessels. | |
| Hidradenoma papilliferum | Irregular serpiginous telangiectasias, pink lacunae, shiny white areas. | |
| Drug reactions | Fixed drug eruption | Blue-gray dots to brown-black dots in pigmented area in random pattern and red structureless area with red dots. |
| Steven Johnson syndrome | Nonspecific features such as red structureless area and comma vessels with areas of blood spots. | |
| Vascular abnormalities | Angiokeratoma | Purple-red lacunae with a white veil. |
| Lymphangioma | Red translucent lacunae with hypopyon sign. |
Table 3.
The dermoscopic and histopathological correlation of various mucosal dermatoses
| Clinical conditions | Dermoscopy | Histopathology |
|---|---|---|
| Vestibular papillomatosis | Finger-like projections | Papillomatosis |
| Vascular core | Fibrovascular core | |
| Pemphigus vulgaris | Blood spots | Fibrin and red blood cells (RBCs) |
| Structureless red area | Erosions or epithelial discontinuity | |
| Red dots | Dilated blood vessels | |
| Violaceous peripheral streaks | Acanthosis | |
| Lichen planus | White reticular lines | Wedge hypergranulosis |
| Tricolor pattern | Wedge hypergranulosis, erosion, acanthosis | |
| Violaceous background | inflammatory infiltrate | |
| Superficial crust | Erosion, fibrin | |
| Dotted vessels | Dilated vessels | |
| Lichen sclerosus et atrophicans | White structureless area | Acanthosis and fibrosis |
| Telangiectataic and dotted vessels | Dilated vessels | |
| Purpuric-to-red globules and blotches | Extravasation of RBC and hemosiderin | |
| Superficial erosion | Epithelial discontinuity | |
| Follicular plugging | Keratin plug | |
| Gray-blue dots in peppering pattern | Pigment incontinence | |
| Hansen disease | Orange yellow hue | Granuloma |
| Red structureless area | Inflammatory infiltrate | |
| White scales | Parakeratosis | |
| Molluscum contagiosum | Central white structureless area | Cytoplasmic inclusions |
| Crown vessels | Ectatic vessels | |
| Bowen disease | Pigmented streaks | Pigment incontinence |
| Glomeruloid vessels (coiled vessels) | Vasculature | |
| Dotted vessels | Vasculature | |
| Reticular network | Basal hyperpigmentation | |
| Squamous cell carcinoma | Yellow-white crust | Fibrin crust |
| Polymorphic vessels | Vasculature | |
| Erythematous structureless area | Squamous eddies | |
| Blood spots | Serous and RBCs exudate | |
| Hidradenoma papilliferum | Central irregular serpiginous vessels | Fibrovascular core |
| Pink lacunae | Cystic space |
Discussion
Application of dermoscopy in visualizing mucosa is gaining importance. Mucoscopy of genital dermatoses is less studied. Mucoscopy of Fordyce spots showed a white yellow discrete globule with central white dots. The vascular morphology seen in our study was a linear type. These features were in concordance with the case reported by Jakhar et al.[1] Micali et al.[2] described the video-dermoscopic features, which showed a garland-like arrangement of vessels around a yellow bunch of lobules, which was not found in our patients.
The mucoscopy features of pearly penile papules showed transparent white structureless areas (100%), with hairpin vessels (22.23%)/linear (33.34%)/dot vessels (33.34%) with bulbous tips (100%), and separate bases (100%). These findings were in concordance with the study performed by Kamat et al. and Micali et al.[2,3,4] Although the female counterpart i.e., vestibular papillomatosis revealed finger-like projections correspond to papillary projections, linear vascular structure correlates with the fibrovascular core histologically. Similar findings were seen in the dermoscopy of vestibular papillomatosis by Kamat et al.[3] and Thakare et al.[5]
Patients with classic reactive arthritis fulfilling the diagnostic criteria having circinate balanitis showed coalescing pustules in an annular to polycyclic fashion (100%), with regular red dotted vessels (100%), which was in concordance with the findings of Errichetti et al.[6] The dermoscopic features of pustules and dotted vessels correlated with histopathological features such as dense dermal neutrophilic infiltrates and increased upper dermal capillary dilatation, respectively. The correlation was not performed in our study as patients denied for histopathological evaluation.
Mucoscopic features were not specific for the diagnosis of genital pemphigus, except for the fact that the lesion bled heavily on placing dermoscope. Blood spots (100%), red structureless area (100%), and red dots (71%), with violaceous streaks at the periphery (78%), were noted. The presence of violaceous streaks at the periphery mimics erosive LP named hence labeled as pseudo-Wickham. Of 57 pemphigus cases enrolled, 11 mucosal biopsies were performed, and the blood spots correspond to fibrin and extravasated erythrocytes; the structureless red area correlates with an epithelial discontinuity on histology. Red dots and violaceous streaks correlated with dilated blood vessels and acanthosis, respectively. We could not find literature on genital mucoscopy, and also, these findings were inconsistent with an observational study conducted by Kaur et al. (2021)[7] where the mucoscopy of seven oral pemphigus vulgaris patients showed a light red area as the most common vascular pattern with nonspecific features.
Purpuric red dots, blotches (59.26%); telangiectasia (59.26%), white structureless area (100%), follicular plugging (44.45%), and occasional gray-blue dots in peppering pattern (59.26%) were seen on mucoscopy of genital lichen sclerosus et atrophicus. The mucoscopic findings and white structureless area correspond to underlying dermal sclerosis, gray-blue dots correlate with dermal melanophages, superficial erosion corresponded to epithelial discontinuity, and follicular plugging correspond to keratin plug histopathologically. These findings were in concordance with Liu et al. study,[8] where mucoscopy of genital lichen sclerosus (LS) showed irregular arrangement, pink structureless areas, white structureless areas, white shiny lines, brown structureless areas, purple dots, follicular plugs, and rosette signs. The correlation of dermoscopy of LSA with histology in our study was a similar study performed by Borghi et al.[9] where a white to pinkish structureless area corresponds to dermal sclerosis. Gray-blue dots arranged in a peppering pattern correlate with dermal melanophages, and purpuric to red globules represent blood spots secondary to scratching.
We observed mucoscopic features of psoriatic balanitis as homogeneously distributed, dotted vessels (100%), with white scales (50%) in the red background (100%). The vascular pattern analyzed by Ankad et al.[10] revealed red dots arranged regularly and homogeneously at 20x magnification, a ring pattern of red dots was observed at 70x globules were seen to be arranged in a glomerular pattern at ×120 magnification on videodermoscopy, which was not seen in our handheld dermoscope. These findings were in concordance with Lacarrubba et al. and Enzo Errichetti et al. where a monomorphic pattern, with diffusely distributed dotted vessels, was seen with white scaling.[6,11]
Dermoscopic features of genital vitiligo revealed absent pigment network (100%), diffuse white glow (100%), with scalloped margin (77%), satellite macules (54.54%), comet tail (13.64%), and micro koebnerization (22.72%) among 22 patients recruited. These findings were in concordance with the study conducted by Veronesi et al.[12] To differentiate vulvar LSA and vulval vitiligo Veronesi et al.[12] did a study where vulvar LSA showed a whipped cream-like appearance, linear or dotted vessels, chrysalis-like structures, erosions, and red purpuric blotches, whereas vulvar vitiligo showed reduced pigment network or absence of pigment, intralesional residual pigmentation spots, and telangiectasia. The mucoscopic features in molluscum contagiosum showed central white structureless area (100%) and crown vessels (50%). Histological feature of the central white structureless area correlates with keratinocytes with intracytoplasmic inclusion bodies and crown vessels with the underlying vasculature histologically. Both dermoscopic and histopathological features were similar to the study performed by Ianhez et al.[13] in 211 patients.
Mucoscopy of Hansen disease involving genital mucosa revealed yellow-white area, orange hue (100%) with white scales (50%). Biopsy of half of the cases showed granuloma which corresponds to an orange-yellow hue on mucoscopy. And, these findings were in concordance with Mohta et al.[14] study, where he included 73 patients, and a correlation between dermoscopic findings and histopathology was noted where orangish-yellow and white structureless areas, steadily throughout the spectrum, depicting dermal granuloma. Vascular structures such as branching, linear, and crown vessels result from the pressure of granuloma pushing the dilated vessels upwards. However, crown vessels with a central whitish-yellow structureless area and peripheral hyperpigmentation were reported by Acharya et al.,[15] which was not seen in our patients.
Mucosal FDE showed blue-gray to brown-black dots in a random pattern at the center of the plaque and red structureless area with red dots at the periphery. These features were in concordance with oral mucoscopy by Rather et al.[16] Dermoscopy of SJS in our study was nonspecific, which showed red structureless area (100%), dotted vessels (62.5%) with areas of blood spots (37.5%). Mucoscopy of SJS has not yet been described, but cutaneous SJS reported by Rossi et al.[17] shows black dots or necrotic area (100%), erythema (83%), and epidermal detachment (83%) in six cases.
Limitations
In our study, because of inclusion of various diseases, sample size was inadequate, biopsies were not performed in all cases, and variations in mucoscopic features in patients who are already on therapy could not be assessed. Haziness while capturing pictures because of mist formation was hindering the quality of pictures. Premalignant and malignant cases were less to provide the mucoscopy features in predicting the risk of conversion.
Conclusion
Various studies on dermoscopy have been published till date, but the mucoscopy is still a gray area. The results of this study revealed the dermoscopic features of various genital disorders and histopathological correlation was performed in few diseases. However, a biopsy was not performed in all mucosal disorders; hence, conclusive correlation could not be extrapolated.
Declaration of Patient consent
Taken.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Histopathology of early LSA revealing papillary dermal inflammatory infiltrate (blue arrow), upper and mid dermal fibrosis (blue star), dilated blood vessels (black circle), and extravasated RBCs (red arrow) [H and E, 4X]
Late LSA (phimosis) revealing focal areas of lichenoid infiltrate with pigment incontinence (blue arrow), dilated blood vessels (red arrow), and whole dermal fibrosis (yellow star) [H and E 4X]
Bowens disease revealing full-thickness atypical keratinocytes, superficial dermal lymphocytic infiltrate, dilated papillary vessels (red circle), and pigment incontinence (white arrow) [H and E 10x]
Histopathology of hidradenoma papilliferum depicting well circumscribed dermal arborizing proliferation lined by luminal tall columnar cells with decapitations and underlying cuboidal cells associated with plasma cell infiltrates [H and E, 4X]
References
- 1.Jakhar D, Kaur I. Mucoscopy of Fordyce's spots on lips. Indian Dermatol Online J. 2019;10:498–9. doi: 10.4103/idoj.IDOJ_185_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Micali G, Lacarrubba F. Augmented diagnostic capability using videodermatoscopy on selected infectious and non-infectious penile growths. Int J Dermatol. 2011;50:1501–5. doi: 10.1111/j.1365-4632.2011.05087.x. [DOI] [PubMed] [Google Scholar]
- 3.Kamat D, Vinay K. Dermatoscopy of nonvenereal genital dermatoses: A brief review. Indian J Sex Transm Dis AIDS. 2019;40:13–9. doi: 10.4103/ijstd.IJSTD_20_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Watanabe T, Yoshida Y, Yamamoto O. Differential diagnosis of pearly penile papules and penile condyloma acuminatum by dermoscopy. Eur J Dermatol. 2010;20:414–5. doi: 10.1684/ejd.2010.0944. [DOI] [PubMed] [Google Scholar]
- 5.Thakare SA, Udare S. Importance of dermoscopy to diagnose vulvar vestibular papillomatosis vs. warts. Indian Dermatol Online J. 2020;11:680–1. doi: 10.4103/idoj.IDOJ_463_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Errichetti E, Lallas A, Di Stefani A, Apalla Z, Kyrgidis A, Lacarrubba F, et al. Accuracy of dermoscopy in distinguishing erythroplasia of Queyrat from common forms of chronic balanitis: Results from a multicentric observational study. J Eur Acad Dermatol Venereol. 2019;33:966–72. doi: 10.1111/jdv.15359. [DOI] [PubMed] [Google Scholar]
- 7.Kaur V, Kaur T, Malhotra SK. Dermoscopic patterns of oral mucosal lesions: New dimensions to mucoscopy. Eur J Mol Clin Med. 2021;8:1482–8. [Google Scholar]
- 8.Liu J, Hao J, Liu Y, Lallas A. Dermoscopic features of lichen sclerosus in Asian patients: A prospective study. J Eur Acad Dermatol Venereol. 2020;34:e720–1. doi: 10.1111/jdv.16540. [DOI] [PubMed] [Google Scholar]
- 9.Borghi A, Virgili A, Corazza M. Dermoscopy of inflammatory genital diseases: Practical insights. Dermatol Clin. 2018;36:451–61. doi: 10.1016/j.det.2018.05.013. [DOI] [PubMed] [Google Scholar]
- 10.Ankad BS, Madarkar M. Red dots caught red handed: Dermoscopy of genital psoriasis. Clin Dermatol Rev. 2017;1:25–6. [Google Scholar]
- 11.Lacarrubba F, Verzì AE, Ardigò M, Micali G. Handheld reflectance confocal microscopy, dermatoscopy and histopathological correlation of common inflammatory balanitis. Skin Res Technol. 2018;24:499–503. doi: 10.1111/srt.12460. [DOI] [PubMed] [Google Scholar]
- 12.Veronesi G, Virdi A, Leuzzi M, Gurioli C, Chessa MA, Guglielmo A, et al. Vulvar vitiligo and lichen sclerosus in children: A clinical challenge. Pediatr Dermatol. 2021;38:1012–9. doi: 10.1111/pde.14771. [DOI] [PubMed] [Google Scholar]
- 13.Ianhez M, Cestari Sda C, Enokihara MY, Seize MB. Dermoscopic patterns of molluscum contagiosum: A study of 211 lesions confirmed by histopathology. An Bras Dermatol. 2011;86:74–9. doi: 10.1590/s0365-05962011000100009. [DOI] [PubMed] [Google Scholar]
- 14.Mohta A, Jain SK, Agrawal A, Kushwaha RK, Sharma P, Sethia K, et al. Dermoscopy in leprosy: A clinical and histopathological correlation study. Dermatol Pract Concept. 2021;11:e2021032. doi: 10.5826/dpc.1102a32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Acharya P, Mathur MC. Clinicodermoscopic study of histoid leprosy: A case series. Int J Dermatol. 2020;59:365–8. doi: 10.1111/ijd.14731. [DOI] [PubMed] [Google Scholar]
- 16.Rather S, Shah AA, Shah FY, Kaur S, Bhat MA, Reyaz S, et al. Dermoscopy of oral mucosal lesions: Experience from a tertiary care center in North India and review of literature. Indian Dermatol Online J. 2022;13:346–60. doi: 10.4103/idoj.idoj_661_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rossi G, da Silva Cartell A, Marchiori Bakos R. Dermoscopic aspects of cutaneous adverse drug reactions. Dermatol Pract Concept. 2021;11:e2021136. doi: 10.5826/dpc.1101a136. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Histopathology of early LSA revealing papillary dermal inflammatory infiltrate (blue arrow), upper and mid dermal fibrosis (blue star), dilated blood vessels (black circle), and extravasated RBCs (red arrow) [H and E, 4X]
Late LSA (phimosis) revealing focal areas of lichenoid infiltrate with pigment incontinence (blue arrow), dilated blood vessels (red arrow), and whole dermal fibrosis (yellow star) [H and E 4X]
Bowens disease revealing full-thickness atypical keratinocytes, superficial dermal lymphocytic infiltrate, dilated papillary vessels (red circle), and pigment incontinence (white arrow) [H and E 10x]
Histopathology of hidradenoma papilliferum depicting well circumscribed dermal arborizing proliferation lined by luminal tall columnar cells with decapitations and underlying cuboidal cells associated with plasma cell infiltrates [H and E, 4X]