Dear Editor,
A 75-year-old man presented with a rapidly growing subcutaneous induration without pain or tenderness in his left upper arm and scrotum. He received surgeries for left inguinal hernia at 25 years and sigmoid colon cancer at 60 years of age. He also received surgery for prostate cancer at 72 years of age. He has not experienced sexual activity, including masturbation, for 10 years. Since his prostate-specific antigen (PSA) level was rising, he was treated with a depot formulation of leuprorelin acetate (LA) injected into his left upper arm. Swellings appeared after 6 doses of a 1-month depot formulation of LA followed by 1 dose of a 3-month depot formulation.
The size of the subcutaneous nodule in the upper left arm was approximately 5.0 × 5.5 cm. The nodule, which demonstrated slight erythema, was attached to the skin, although it did not adhere to the underlying tissues [Figure 1a and b]. Additionally, a subcutaneous indurated mass (size 7.0 × 6.5 cm) was observed at the base of the penile shaft and scrotum [Figure 1c]. Blood tests revealed an elevated inflammatory response with moderate eosinophilia as follows: white blood cell count, 18,000/μl; eosinophils, 9.9%; C-reactive protein 4.51 mg/dl and PSA <0.01 ng/ml. Syphilis and chlamydia were negative.
Figure 1.

Clinical appearance. Subcutaneous induration with mild erythema on the left upper arm (a and b) and genitalia (c)
Sagittal and coronal T2-weighted magnetic resonance imaging of the penis revealed a low-signal-intensity heterogeneous lesion with indistinct margins surrounding the penis [Figure 2a and b]. No diffusion-limited areas were identified within the mass, suggesting that the tumor was benign [Figure 2c].
Figure 2.
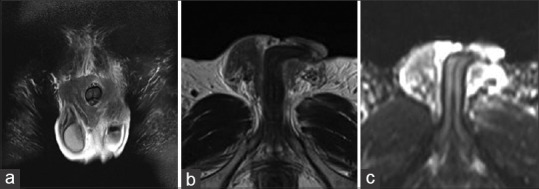
Magnetic resonance imaging findings. T2-weighted images of the penis revealed heterogeneous lesions with indistinct margins surrounding the penis. The mass was predominantly of low signal intensity (a and b). The apparent diffusion coefficient indicates no diffusion-limited areas within the mass (c)
Histopathological examination of skin biopsies from the left upper arm and scrotum revealed a non-caseating granuloma comprising lymphocytes, eosinophils, and neutrophils. Foreign body giant cells were visible in the subcutaneous adipose tissue with surrounding fibrosis. However, no evidence of malignancy was noted [Figure 3a-d].
Figure 3.
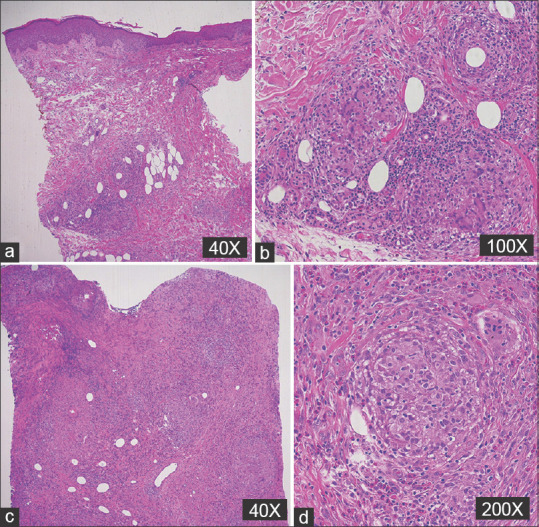
Histopathological findings. Noncaseating granuloma comprising lymphocytes, eosinophils, neutrophils, and foreign-body giant cells in the subcutaneous adipose tissue with surrounding fibrosis in the left upper arm, (H & E; 40x) (a) and (H & E; 100x) (b); and scrotum, (H & E; 40x) (c) and (H & E; 100x) (d)
Thus, the patient was diagnosed with a sclerosing lipogranuloma (SL) in the scrotum and foreign body granuloma in the left upper arm. Follow-up revealed that both subcutaneous indurations had reduced in size within a few weeks.
SL of the penis was originally described by Smetana and Bernhard in 1950 as a subcutaneous inflammatory response to endogenously degraded lipids following tissue injury.
Paraffin is often detected in lesions by spectrophotometric analysis.[1] Another possible mechanism is a secondary immune response to external lipids after injection of various substances, including autologous fat, polyacrylamide, fluid silicone, collagen, and hyaluronic acid.[2] These materials cannot be metabolized without lipolytic enzymes for exogenous lipids and can cause foreign body reactions in such cases.
LA is a highly potent agonist of uteinizing hormone-releasing hormone (LH-RH). Because oral delivery of peptide hormones are not feasible owing to the instability of peptide hormones against enzymatic degradation, daily subcutaneous injections are necessary. To overcome this problem, a microcapsule formulation was developed. Biodegradable polymers such as polylactic acid or polylactic-co-glycolic acid, which have well-established safety profiles as surgical sutures, were used as the microcapsule matrix. LA is currently available in three formulations: one month, three months, and six months. The monthly formulation utilizes a lactide/glycolide copolymer as the matrix, whereas the three- and six-month formulations employ a lactide polymer, thereby increasing the amount of both the matrix and active ingredients as the duration of action extends.
Recently, cases of granulomas developing at the injection site with LA, especially with a three-month formulation, have been reported. However, whether granuloma formation is caused by a matrix or active ingredient remains unclear. Manasco et al.[3] supported the hypothesis of a local reaction due to microcapsules by observing similar granuloma formation following the injection of microcapsules alone. Ouchi et al.[4] proposed that microcapsules may cause granuloma formation as vacuoles within multinucleated giant cells are of the same size (20 μm) and exhibit a similar morphology with microcapsules. Suzuki et al.[5] performed adipophilin staining to determine whether the vacuoles were caused by fat degeneration due to inflammation or a direct consequence of microcapsules. The vacuoles were negative for adipophilin, suggesting that they were microcapsules themselves.
In this case, the coexistence of subcutaneous granuloma at the injection site and intrascrotal SL might be attributed to that the microcapsules of LA accumulated and deposited around the scrotum, causing granulomas by the same mechanism as granulomas at the injection site. Alternatively, the subcutaneous injection of LA may have triggered an allergic reaction against the absorbable sutures, which have the similarity in composition with LA microcapsules, and was used in surgeries for inguinal hernia, sigmoid colon cancer, and prostate cancer remained around the scrotum. This is the first reported case of concurrent subcutaneous granuloma at the LA injection site and intrascrotal SL. However, further studies are required to clarify this phenomenon.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Oertel YC, Johnson FB. Sclerosing lipogranuloma of male genitalia. Review of 23 cases. Arch Pathol Lab Med. 1977;101:321–6. [PubMed] [Google Scholar]
- 2.Soebhali B, Felicio J, Oliveira P, Martins FE. Sclerosing lipogranuloma of the penis: A narrative review of complications and treatment. Transl Androl Urol. 2021;10:2705–14. doi: 10.21037/tau-21-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manasco PK, Pescovitz OH, Blizzard RM. Local reactions to depot leuprolide therapy for central precocious puberty. J Pediatr. 1993;123:334–5. doi: 10.1016/s0022-3476(05)81720-2. [DOI] [PubMed] [Google Scholar]
- 4.Ouchi T, Koyama T, Miyata N, Sugiura M. Granuloma caused by subcutaneous injection of leuprorelin acetate product: Case report and histopathological findings. J Dermatol. 2006;33:719–21. doi: 10.1111/j.1346-8138.2006.00167.x. [DOI] [PubMed] [Google Scholar]
- 5.Suzuki C, Shiiyama R, Anzai H. Subcutaneous granuloma formation due to the ingestion of leuprolelin acetate every three months. Rinsho Derma (Tokyo) 2021;63:562. [Google Scholar]


