Dear Editor,
An elderly male was referred by the otorhinolaryngology department for a 3 × 3 cm2 well-demarcated, indurated round plaque with a peripheral rim of erythema on the right shoulder, noticed 3 days previously [Figure 1]. The shape and location of the plaque suggested it was induced by an electrocardiogram (ECG) lead.
Figure 1.
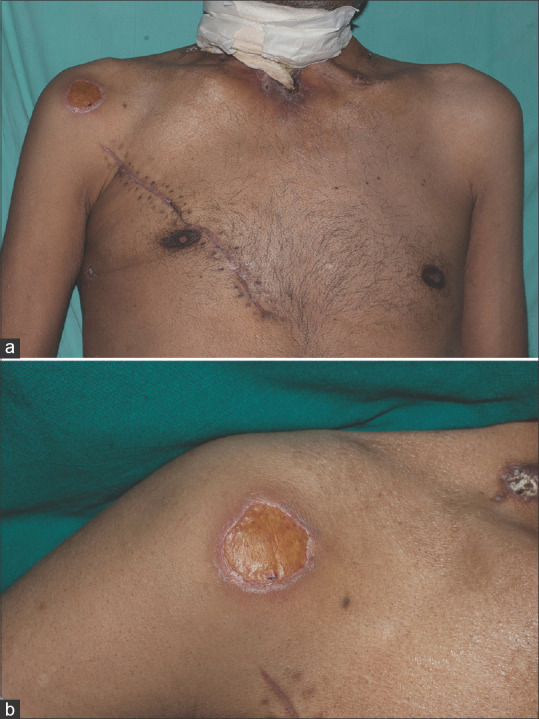
(a) Yellowish round plaque on the right shoulder corresponding to the placement of right limb ECG lead (lead II), with no involvement of skin beneath other ECG leads (b) Well-demarcated yellowish round plaque on right shoulder (zoomed-in). ECG = electrocardiogram
He had undergone total laryngectomy combined with partial pharyngectomy and bilateral neck lymph node dissection for carcinoma of the right parapharyngeal space, about 4 weeks previously, followed by a re-exploration for postoperative hematoma drainage 2 weeks previously. On both occasions, he stayed for 2–3 days in the high-dependency unit for postoperative supervision with continuous 12-lead electrocardiographic monitoring. (UNI-EM Cardiomin 3C ECG machine). He developed a burn on the shoulder below one electrode but did not have lesions beneath the other 11 electrodes.
Iatrogenic skin burns under monitoring electrodes used with electrocardiography leads and neuromonitoring leads are reported.[1] Burn injuries have also been reported in patients with ECG electrodes left in situ when undergoing magnetic resonance imaging (MRI) scanning, likely due to the interaction between electromagnetic radiation and the ECG electrode.[2] Contact hypersensitivity to adhesive gel or electrode material can also lead to skin changes localized to the site of electrode fixation.
Typically, these causes lead to changes under all electrodes.[3]
ECG amplifiers are used to convert weak electrical activity from the heart to stronger signals that can be detected as the machine output. The isolation amplifier is an important component of this system, which provides a barrier between the input and output circuitry of the signal processing. This separation protects the signal quality in the input circuit, and, more importantly, provides safety to the patient from any current leakages.[4] Sometimes, a malfunction in the isolation amplifier or a power surge may overwhelm the isolation amplifier, allowing some volume of current to flow back into the input circuit and reach the patient. This current leads to the electrolysis of moisture under the electrodes. Under a negative electrode, this electrolysis leads to the formation of a strongly alkaline medium, which corrodes the underlying skin, resulting in a caustic burn.[5] The burn in our patient occurred below the right limb lead, which is, by convention, the negative electrode as represented in Einthoven’s triangle.[6] This is the likely explanation for developing a single lesion.
The diagnosis of electrode-induced cutaneous changes is relatively easy when multiple sites are affected, but it should be recognized that changes may be confined to a single electrode in some cases.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Russell MJ, Gaetz M. Intraoperative electrode burns. J Clin Monit Comput. 2004;18:25–32. doi: 10.1023/b:jocm.0000025254.73456.db. [DOI] [PubMed] [Google Scholar]
- 2.Abdel-Rehim S, Bagirathan S, Al-Benna S, O’Boyle C. Burns from ECG leads in an MRI scanner: Case series and discussion of mechanisms. Ann Burns Fire Disasters. 2014;27:215–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Foti C, Lopalco A, Stingeni L, Hansel K, Lopedota A, Denora N, et al. Contact allergy to electrocardiogram electrodes caused by acrylic acid without sensitivity to methacrylates and ethyl cyanoacrylate. Contact Dermatitis. 2018;79:118–21. doi: 10.1111/cod.13015. [DOI] [PubMed] [Google Scholar]
- 4.Murugappan M, Thirumani R, Omar MI, Murugappan S. Development of cost effective ECG data acquisition system for clinical applications using LabVIEW,“ 2014. IEEE 10th International Colloquium on Signal Processing and its Applications, Kuala Lumpur, Malaysia. 2014:100–5. [Google Scholar]
- 5.Orpin JA. Unexpected burns under skin electrodes. Can Med Assoc J. 1982;127:1106. [PMC free article] [PubMed] [Google Scholar]
- 6.Ortega R, Mazzini M, Xue K, Espaillat D. Videos in clinical medicine. Electrocardiographic monitoring in adults. N Engl J Med. 2015;372:e11. doi: 10.1056/NEJMvcm1400705. [DOI] [PubMed] [Google Scholar]


