CASE REPORT
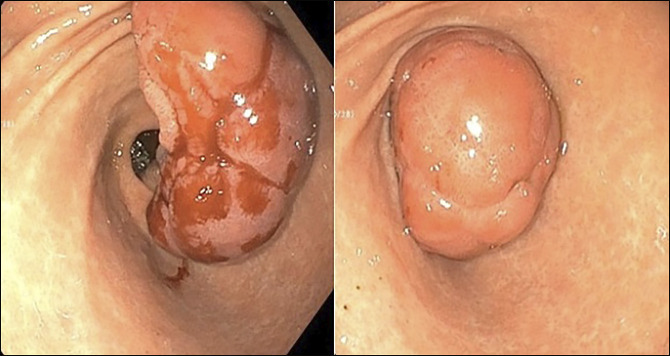
A 37-year-old healthy woman presented with symptoms of vomiting, abdominal pain, and gastric outlet obstruction evident on an abdominal computed tomography scan (Figure 1). Upper endoscopy revealed a large obstructing 7-cm pedunculated duodenal mass with a large stalk intermittently prolapsing and obstructing the pyloric channel. The mass was emanating from a posterior duodenal bulb (Figure 2).
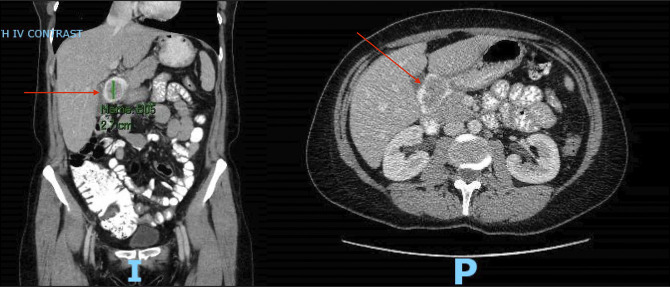
Figure 1.
Computed tomography scan images (coronal and axial views) showing an ovoid-filling defect in the duodenal bulb suspicious of a mass (arrow).
Figure 2.
Endoscopic view of duodenal polyp with stalk.
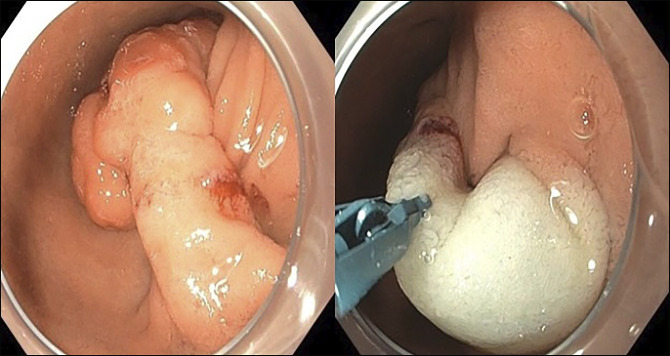
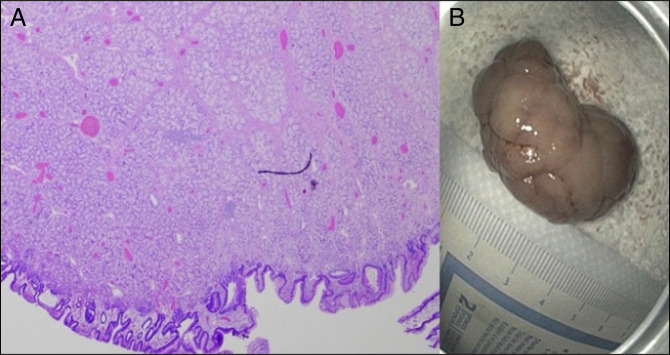
Traditional endoscopic mucosal resection by snare was attempted but was not possible because of the mobile nature and large size of the polyp; the largest available snare could not be wrapped around it for en-bloc resection. Endoscopic submucosal dissection (ESD) was performed because it provided more controlled resection at the thick base of the lesion. Given the thin muscular layer of the duodenal wall and the poor endoscopic operability, ESD is challenging in the duodenal bulb and requires highly technical skills. A scissor-type knife was mainly used, and ESD was performed successfully (Figure 3). The polyp was successfully retrieved. Only minimal bleeding was encountered during the procedure. An over-the-scope clip was placed prophylactically at the resection site to prevent delayed post-ESD bleeding. Histologic analysis confirmed a submucosal Brunner gland hyperplasia (Figure 4). No post-ESD complications were encountered. No recurrence on subsequent endoscopic surveillance was observed (Figure 5).
Figure 3.
Endoscopic view of the thick stalk of the duodenal polyp.
Figure 4.
(A) Histologic analysis showing submucosal Brunner gland hyperplasia. (B) Polyp after resection and retrieval.
Figure 5.

Endoscopic view during follow-up.
This case highlights the utility of ESD as an alternative safe and efficient approach in removing a large obstructing duodenal mass that could not be resected traditionally. This technique should be considered for the resection of similar polyps.
DISCLOSURES
Author contributions: C. Lahoud, M. Tawfik: manuscript writing. L. Deeb, S. Andrawes: concept development, manuscript editing, and review. C. Lahoud is the article guarantor.
Financial disclosure: None to report.
Informed consent was obtained for this case report.
Contributor Information
Mark Tawfik, Email: mtawfik@northwell.edu.
Liliane Deeb, Email: ldeeb1@northwell.edu.
Sherif Andrawes, Email: sandrawes@northwell.edu.