Abstract
Persistent hypoglossal artery (PHA) is a rare, anatomical variant in which the posterior cerebral circulation is primarily supplied by a branch of the carotid artery, rather than the vertebral arteries. This case report discusses carotid endarterectomy performed on a man, 67 years of age, with high-grade, asymptomatic carotid artery stenosis and ipsilateral PHA. Preoperative computed tomography angiography identified the PHA arising from the internal carotid artery, compensating for atretic bilateral vertebral arteries and providing primary perfusion to anterior spinal artery. A carotid endarterectomy with a bovine pericardial patch was executed under general anesthesia, incorporating preemptive shunting of the PHA and intraoperative electroencephalogram monitoring. The operation proceeded without complications, maintaining normal electroencephalogram readings, and the patient exhibited no focal neurological deficits postoperatively, although transient dysphagia was noted. Follow-up imaging at 4 months confirmed the patency of the internal carotid artery and PHA. This case underscores the necessity for meticulous surgical planning and monitoring in the presence of rare vascular anomalies to ensure successful outcomes. The key takeaway is that comprehensive, preoperative imaging, individualized surgical strategies, and vigilant postoperative monitoring are critical for managing rare vascular anomalies, such as PHA.
Keywords: TCAR, CEA, Transcarotid artery revascularization, Persistent hypoglossal artery, PHA, Stroke, Symptomatic lesion
Persistent hypoglossal artery (PHA) is a rare anatomical variant of the cerebral vasculature in which most of the posterior cerebral circulation is supplied by a branch of the carotid artery instead of the bilateral vertebral arteries. Recognition of this unusual vascular configuration can have significant implications in the setting of carotid artery revascularization. Herein, we present the surgical management of asymptomatic, high-grade stenosis via carotid endarterectomy (CEA) in a patient with an ipsilateral PHA as dominant perfusion to posterior cerebral circulation and primary perfusion to anterior spinal artery. We obtained informed consent to disclose individual clinical information from the subject of this case report.
Case report
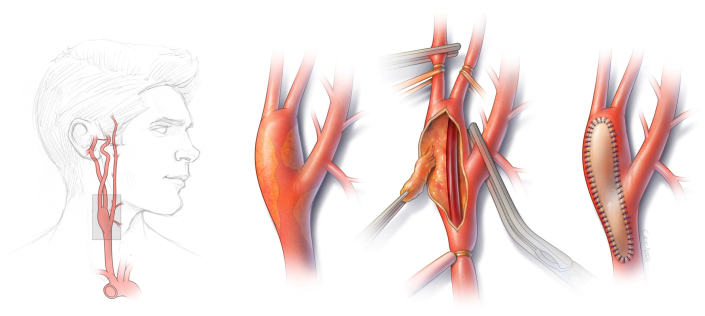
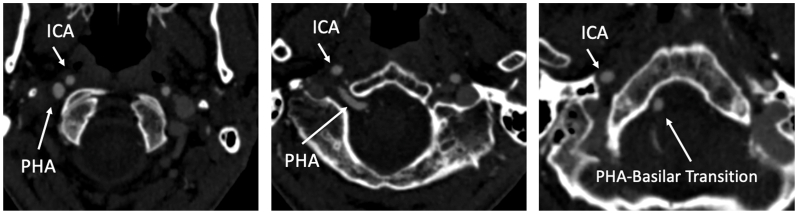
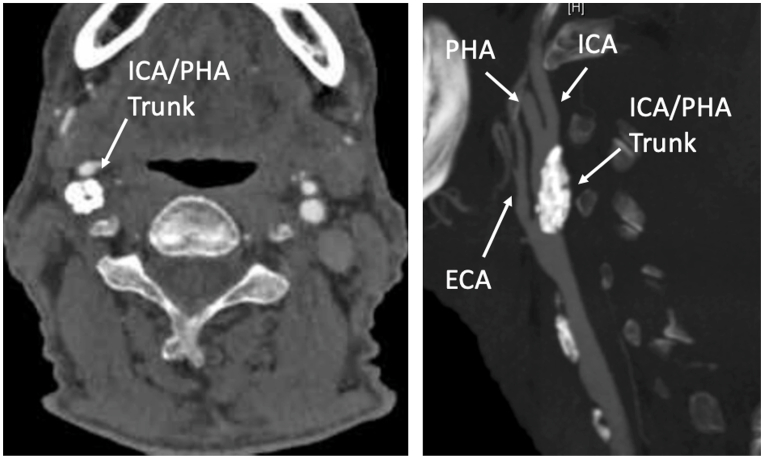
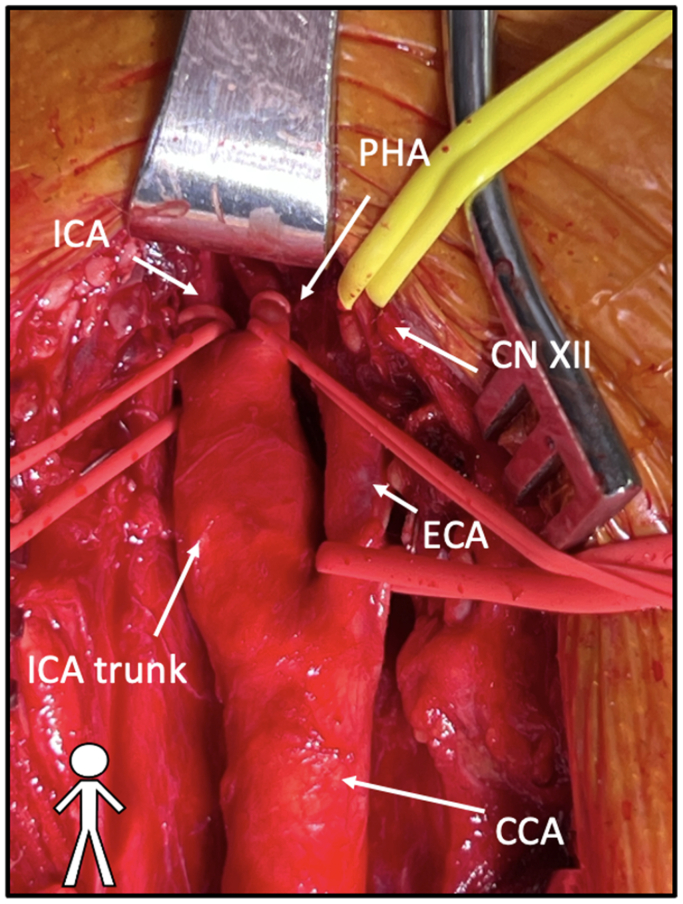
A man, 67 years of age, with a past medical history of hypertension, coronary artery disease, and aortoiliac occlusive disease, was found to have high-grade (>80%) asymptomatic carotid artery stenosis without significant contralateral disease (<50%). Preoperative computed tomography angiography (CTA) demonstrated PHA arising from the internal carotid artery (ICA) and providing sole supply to the posterior circulation in the setting of atretic bilateral vertebral arteries and primary perfusion to anterior spinal artery via sole origin of basilar artery (Figs 1 and 2). The plaque extended from the common carotid artery (CCA), into the common ICA/PHA trunk, to just proximal to the ICA/PHA bifurcation (Fig 3). A CEA with bovine pericardial patch was performed under general endotracheal anesthesia and intraoperative electroencephalogram (EEG) monitoring with plans to preemptively shunt the hypoglossal artery and preparations taken to place an additional shunt into the ICA pending potential EEG changes. Silastic vessel loop control was obtained at the proximal CCA, distal ICA, distal PHA, external carotid artery (ECA), and hypoglossal nerve (Fig 4). After sufficient heparinization (goal activated clotting time of >250), distal ICA, distal PHA, the proximal CCA, and ECA were clamped. CEA was performed in the standard fashion with a shunt to the PHA after an arteriotomy was performed from the distal CCA, past the takeoff of the ECA, to the common trunk of the ICA and persistent hypoglossal, just proximal to this second bifurcation (Fig 1). Given that the PHA was providing the dominant flow to the posterior circulation, it was of adequate size to support an 8F Argyle shunt. This was achieved without issue and secured. Next, intraoperative EEG monitoring was observed to be normal and, thus, the operation proceeded in standard fashion. The artery was then endarterectomized and bovine patch angioplasty performed.
Fig 1.
Carotid endarterectomy (CEA) illustration demonstrating persistent hypoglossal artery (PHA).
Fig 2.
Computed tomography angiography (CTA) axial series depicting internal carotid artery (ICA) and persistent hypoglossal artery (PHA) transition to basilar artery formation.
Fig 3.
Sagittal image of the stenosis in which plaque extended from the common carotid artery (CCA) into the common ICA/PHA trunk, to just proximal to the ICA/PHA bifurcation. ECA, external carotid artery; ICA, internal carotid artery; PHA, persistent hypoglossal artery.
Fig 4.
Intraoperative image of carotid artery demonstrating level of exposure and clamp sites. CCA, common carotid artery; CN XII, cranial nerve 12 hypoglossal; ECA, external carotid artery; ICA, internal carotid artery; PHA, persistent hypoglossal artery.
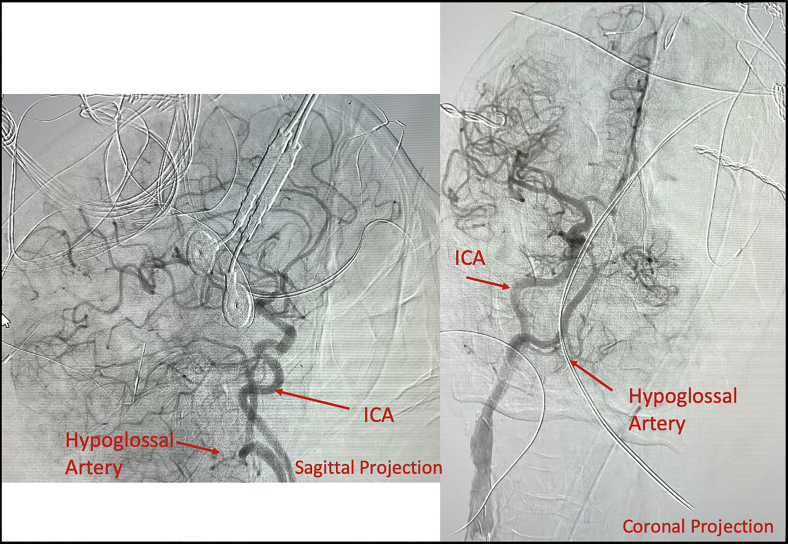
Given the aberrant anatomy, completion cerebral angiogram was performed to ensure patency of the posterior circulation (Fig 5). This revealed a widely patent patch, ICA, and PHA (Fig 5). Completion intraoperative transit time flow measurement via duplex ultrasound examination demonstrated normal continuous low-resistance ICA and PHA waveforms. The patient awoke without focal neurological deficits with no EEG changes noted throughout the case. However, the postoperative course was characterized by transient dysphagia. The patient remained neurologically intact at the 4-month follow-up, with CTA demonstrating good technical results with a widely patent ICA and hypoglossal artery.
Fig 5.
Intraoperative cerebral angiogram reveals a widely patent patch, internal carotid artery (ICA) and persistent hypoglossal artery (PHA).
Discussion
This case presents a rare and complex vascular anomaly involving a PHA providing the sole blood supply to the posterior circulation in the context of atretic bilateral vertebral arteries and is an exceedingly uncommon finding. Such anatomical variants pose significant challenges in surgical planning and execution, particularly in the instance of concomitant ICA stenosis.
The hypoglossal artery originates in an embryonic version as a vessel anastomosing the carotid-basilar system and typically regresses during development.1 Its presence past this point and provision as the sole supply to the posterior circulation are exceptionally rare, with an estimated incidence of 0.03% to 0.09%.2,3 Therefore, when considering ipsilateral CEA, meticulous planning is a necessity to ensure adequate antegrade posterior cerebral flow and spinal cord perfusion during the entirety of any planned ICA intervention. The anatomy of this variant is often difficult to assess on ultrasound examination, because it originates high in the cervical region of the neck, highlighting the added benefit of cross-sectional imaging, which was performed in this case.1 It is important to highlight that this patient's CTA demonstrated primary perfusion of the anterior spinal artery via unilaterally formed basilar originating from PHA, atretic bilateral vertebral arteries, and absent posterior inferior cerebellar arteries (Fig 2).
The decision to preemptively shunt the hypoglossal artery during CEA was necessitated by the imperative to maintain continuous blood flow to the posterior circulation and spinal cord. In tandem to this technique, traditional EEG cerebral monitoring was used, serving as an adjunct for identifying sufficient anterior circulation flow. Prior reports have identified successful parallel shunting of both the ICA and the PHA in these cases.2,4 Previous authors have described successful management of PHA without the use of shunting, or prepared for selective shunting based on stump pressure monitoring. However, their reports are lacking with regard to spinal cord perfusion supply.5,6 Nonetheless, the highly variable anatomy of PHA requires individualized planning with regard to maintenance of posterior cerebral perfusion and anterior spinal cord. The operators were also prepared for standard maneuvers of increased cephalic exposure, including nasotracheal intubation, division of the posterior belly of the digastric, 12th nerve mobilization, and styloidectomy. However, this case only required division of digastric and 12th nerve mobilization.5
Another consideration for treatment of ICA stenosis in this setting includes stenting. The efficacy of stenting vs endarterectomy has not been studied in this specific patient population, but there should be careful consideration given to the methodology of embolic protection and stent placement. Whether by means of balloon tamponade, reversal of flow, or filter wire protection, there are inherent risks with stroke associated with the standard cases of this procedure and, more so, with the single, posterior circulation supply from the hypoglossal artery. We felt the patient’s anatomy precluded a safe and adequate distal stent landing zone within the distal ICA/PHA trunk before the ICA/PHA bifurcation. In addition, stent placement in largely calcified plaque was unlikely to achieve sufficient stent expansion. Furthermore, it is not well-described how stent placement potentially across the origin of a PHA can affect flow dynamics, which may impose a stroke risk as well.7 Further documentation is needed to delineate these differences in settings where open carotid revascularization is prohibitive.
The postoperative course was characterized by transient dysphagia, a known complication of CEA with extensive cephalad dissection, which resolved without long-term deficits. The patient's neurological integrity was preserved, and follow-up imaging confirmed the patency of the ICA and hypoglossal artery, reflecting a favorable technical outcome. This case emphasizes the importance of comprehensive preoperative imaging, individualized surgical planning, and vigilant postoperative monitoring in achieving successful outcomes in patients with rare vascular anomalies.
Conclusions
CEA in the setting of PHA carries additional challenges related to intraoperative neuroprotection. Careful surgical planning and neuromonitoring allow for successful treatment, even in this anatomically challenging setting, which can require double shunt placement to preserve antegrade cerebral and spinal cord perfusion.
Disclosures
None.
Footnotes
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Srinivas M.R., Vedaraju K.S., Manjappa B.H., Nagaraj B.R. Persistent primitive hypoglossal artery (PPHA) — a rare anomaly with literature review. J Clin Diagn Res. 2016;10:TD13–T14. doi: 10.7860/JCDR/2016/15556.7116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanada T., Shirai W., Yamamoto S., Kinoshita M., Tokumitsu N. A case of carotid endarterectomy assisted with a three-way junction shunting tube for the internal carotid artery stenosis involving a persistent primitive hypoglossal artery. J Surg Case Rep. 2021;2021 doi: 10.1093/jscr/rjab362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ouriel K., Green R.M., DeWeese J.A. Anomalous carotid-basilar anastomoses in cerebrovascular surgery. J Vasc Surg. 1988;7:774–777. doi: 10.1067/mva.1988.avs0070774. [DOI] [PubMed] [Google Scholar]
- 4.Pride L.B., Lagergren E.R., Hafner D.H., Chervu A.A. Critical carotid artery stenosis involving a persistent primitive hypoglossal artery. J Vasc Surg Cases Innov Tech. 2020;6:177–180. doi: 10.1016/j.jvscit.2020.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Madden N.J., Calligaro K.D., Dougherty M.J., Maloni K., Troutman D.A. Persistent hypoglossal artery: challenges associated with carotid revascularization. Vasc Endovasc Surg. 2019;53:589–592. doi: 10.1177/1538574419859102. [DOI] [PubMed] [Google Scholar]
- 6.Fantini G.A., Reilly L.M., Stoney R.J. Persistent hypoglossal artery: diagnostic and therapeutic considerations concerning carotid thromboendarterectomy. J Vasc Surg. 1994;20:995–999. doi: 10.1016/0741-5214(94)90238-0. [DOI] [PubMed] [Google Scholar]
- 7.Zhang L., Song G., Chen L., Jiao L., Chen Y., Wang Y. Concomitant asymptomatic internal carotid artery and persistent primitive hypoglossal artery stenosis treated by endovascular stenting with proximal embolic protection. J Vasc Surg. 2016;63:237–240. doi: 10.1016/j.jvs.2014.04.066. [DOI] [PubMed] [Google Scholar]