Abstract
Background:
Combination therapy with BRAF and MEK inhibitor holds promise for treating gliomas harboring the BRAF V600E mutation; however, the development of acquired resistance remains a challenge.
Case Description:
We describe a case of repeated recurrent BRAF-mutant pleomorphic xanthoastrocytoma (central nervous system World Health Organization grade 3) treated with combination therapy with BRAF and MEK inhibitor. The patient received dabrafenib (BRAF inhibitor) and trametinib (MEK inhibitor); however, she developed resistance to the combination therapy. Remarkably, incidental drug discontinuation contributed to the disappearance of the resistant tumor. The same phenomenon was repeatedly observed after that. Genetic analysis demonstrated that the resistant tumor had BRAF V600E amplification; the resistant tumor remained BRAF→MEK→ERK pathway dependent, and drug resistance might be due to elevated BRAF V600E expression. We speculated that ERK1/2 signal extremes caused by the discontinuation of the combination therapy affected the resistant tumor survival.
Conclusion:
This case study provides important insights into novel treatment strategies and their underlying mechanisms for gliomas with BRAF mutations.
Keywords: Anaplastic pleomorphic xanthoastrocytoma, BRAF, Dabrafenib, Drug holiday, Trametinib

INTRODUCTION
Combination therapy with BRAF and MEK inhibitor shows promise for treating BRAF V600E mutation-harboring gliomas, yet developing acquired resistance remains challenging. The median response duration to the combination therapy for central nervous system (CNS) World Health Organization (WHO) grade 3 pleomorphic xanthoastrocytoma (PXA) is 6 months due to drug resistance.[7] A study using high-grade glioma patient-derived xenograft models revealed that these inhibitors deregulate negative feedback mechanisms, leading to MAPK pathway reactivation and drug resistance.[6] In vitro studies with BRAF V600E-mutant colorectal cancer cell lines showed BRAF V600E amplification as a resistance mechanism.[2] Together, resistant tumor cells remain BRAF→MEK→ERK pathway dependent, and drug resistance is due to elevated BRAF V600E expression.[3]
CASE PRESENTATION
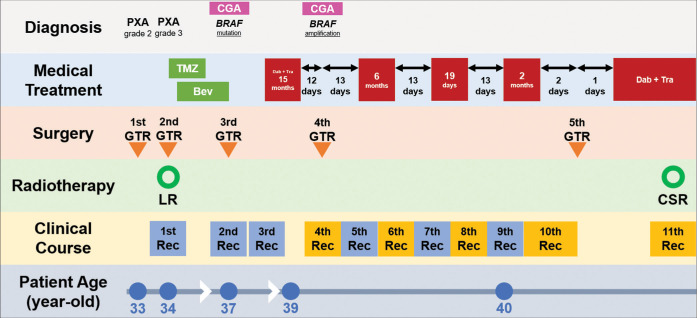
Here, we describe a female patient with CNS WHO grade 3 PXA who experienced repeated recurrences of resistance to combination therapy with BRAF and MEK inhibitors. The patient’s clinical course and management timeline are shown in Figure 1 and Table 1.
Figure 1:
Treatment Timeline. Timeline summarizing the treatment course of our patient, including surgery, chemotherapy, radiation therapy, and molecular-targeted therapy. The red box indicates dabrafenib + trametinib; gaps in the red boxes indicate drug holidays. The yellow boxes indicate resistant tumors. PXA: Pleomorphic xanthoastrocytoma, CGA: Comprehensive genetic analysis, Rec: Recurrence, GTR: Gross total resection, TMZ: Temozolomide, Bev: Bevacizumab, LR:Local radiation, CSR: Craniospinal radiation.
Table 1:
Timeline summarizing the treatment course of our patient, including surgery, chemotherapy, radiation therapy, and molecular-targeted therapy.
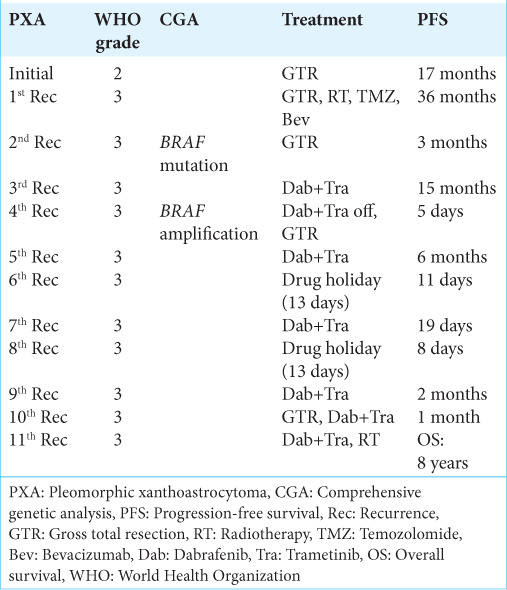
The recurrent tumor harbored a BRAF V600E mutation, and the patient participated in a pan-cancer multidrug off-label treatment trial, BELIEVE (NCCH1901, jRCTs031190104).[4] Dabrafenib and trametinib, provided free of charge by the company, were effective for 15 months. Similarly to previous preclinical studies,[2] the drug-resistant tumor harbored a BRAF V600E amplification [Figure 1].
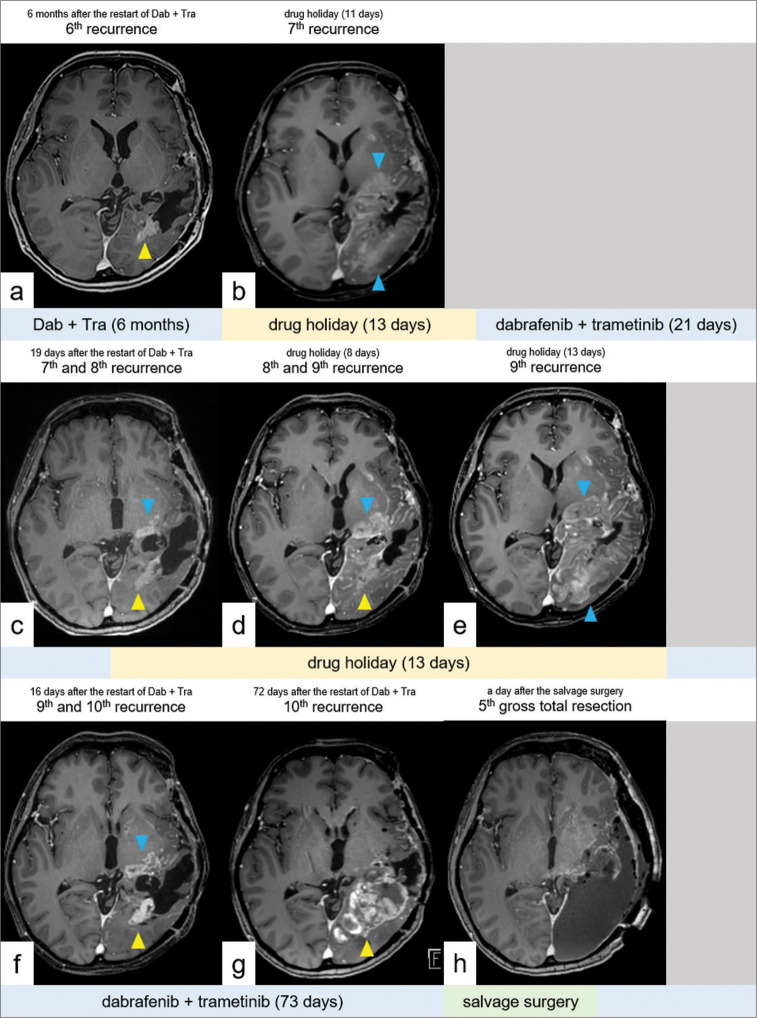
A subsequent restart of the combination therapy was effective for 6 months, but the drug-resistant tumor reappeared at the atrium [Figure 2a]. At this point, the combination therapy had to be discontinued due to creatine kinase level elevation. Remarkably, the drug-resistant tumor at the atrium disappeared during this drug holiday [Figure 2b], with a diffuse faint contrast effect appearing in the temporo-occipital lobe [Figure 2b].
Figure 2:
The key imaging course of drug holiday. (a) CET1WI on MRI showed the sixth recurrence. (b) CET1WI on MRI showed the seventh recurrence with the disappearance of the sixth recurrence. (c) CET1WI on MRI showed the eighth recurrence with regression of the seventh recurrence due to restarting the combination therapy. (d and e) CET1WI on MRI showed the ninth recurrence with gradual dissipation of the eighth recurrence during drug holiday. (f) CET1WI on MRI showed the tenth recurrence with dissipation of the ninth recurrence. (g) CET1WI on MRI showed the tenth recurrence. (h) CET1WI on MRI after the salvage surgery. The yellow arrowhead indicates a recurrent tumor that acquired resistance to combination therapy with BRAF and MEK inhibitors. The blue arrowhead indicates a drug-sensitive tumor. CET1WI: Contrast-enhanced T1-weighted imaging, MRI: magnetic resonance imaging.
After the creatine kinase level improved, the combination therapy was once again effective against the diffuse tumor [Figure 2c]. However, the drug-resistant tumor reappeared at the atrium upon restarting the combination therapy. At this point, the combination therapy had to be discontinued due to anemia. Notably, a similar change occurred during the drug holiday, with the drug-resistant tumor at the atrium gradually disappearing and the drug-sensitive tumor expanding over the temporo-occipital lobe [Figures 2c-e]. Following this, the restart of the combination therapy was effective, as expected [Figure 2f]. However, the resistant tumor gradually grew, accompanied by an intratumoral hemorrhage [Figure 2g]. The fifth resection was performed with three drug holidays, including the day of resection [Figure 2h]. After the resection, the patient’s condition stabilized with the combination therapy for about 6 months. Unfortunately, the resistant tumor gradually grew, and the patient died 8 months after the resection.
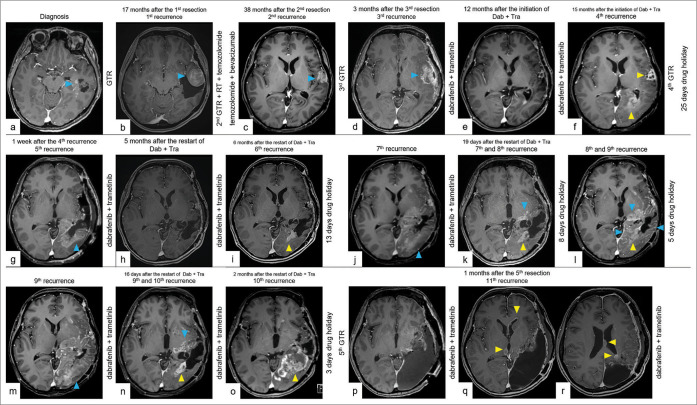
Figure 3 depicts the imaging course with other multiple recurrences, and Figure 4 illustrates the excised specimens’ microscopic characteristics. With each resection, recurrent tumors showed increased mitotic activity, with cell features imparting a close resemblance to epithelioid glioblastoma.
Figure 3:
The full imaging course with repeated recurrences. (a) CET1WI on MRI showed a 2.6 cm cystic tumor (blue arrowhead) in the left temporal lobe at the time of diagnosis. (b) CET1WI on follow-up MRI 17 months after the first resection showing the first local recurrent tumor (blue arrowhead). (c) CET1WI on follow-up MRI 38 months after the second resection showing the second local recurrent tumor (blue arrowhead) after GTR of the first recurrent tumor, radiotherapy, temozolomide, and bevacizumab. (d) CET1WI on follow-up MRI 3 months after the third resection showing the third local recurrent tumor (blue arrowhead) after GTR of the second recurrent tumor. Dab + Tra was initiated 2 months after the diagnosis of the third recurrence. (e) CET1WI on follow-up MRI 12 months after the initiation of Dab + Tra, showing tumor regression. (f) CET1WI on follow-up MRI 15 months after the initiation of Dab + Tra showing the fourth local recurrence-resistant tumor (yellow arrowheads). Dab + Tra was then discontinued. (g) CET1WI on follow-up MRI 1 week after the fourth recurrence showing the fifth diffuse recurrent tumor (blue arrowhead) after GTR of the fourth recurrent tumor. Dab + Tra was restarted 25 days after the drug holiday. (h) CET1WI on follow-up MRI 5 months after restarting Dab + Tra showing stable disease. (i) CET1WI on follow-up MRI 6 months after restarting Dab + Tra, showing the sixth local recurrent-resistant tumor (yellow arrowhead). Dab + Tra was then discontinued. (j) CET1WI on follow-up MRI after 10 days of drug holiday showing the seventh diffuse recurrent tumor (blue arrowhead) with the disappearance of the sixth recurrent tumor. Dab + Tra was resumed 13 days after the drug holiday. (k) CET1WI on follow-up MRI 19 days after the second restart of Dab + Tra showing the eighth local recurrent-resistant tumor (yellow arrowhead), with a reduction in the contrast effect of the seventh tumor (blue arrowhead). Dab + Tra was then discontinued. (l) CET1WI on follow-up MRI after 7 days of drug holiday showing the ninth diffuse recurrent tumor (blue arrowheads) with gradual dissipation of the contrast effect of the eighth recurrent tumor (yellow arrowheads). (m) CET1WI on follow-up MRI after 12 days of drug holiday showing the ninth diffuse recurrent tumor (blue arrowhead) with the disappearance of the eighth recurrent tumor. Dab + Tra was resumed 13 days after the drug holiday. (n) CET1WI on follow-up MRI 16 days after the third restart of Dab + Tra showing the tenth local recurrent-resistant tumor (yellow arrowhead), with a reduction in the contrast effect of the ninth tumor (blue arrowhead). Dab + Tra was then administered. (o) CET1WI on follow-up MRI 2 months after the third restart of Dab + Tra showing the growing tenth recurrent-resistant tumor (yellow arrowhead) and an intratumoral hemorrhage. (p) CET1WI on follow-up MRI a day after the fifth resection. Dab + Tra was restarted on the same day. (q) CET1WI on follow-up MRI a month after the fifth resection, showing the eleventh disseminated recurrence in the ventricular wall (yellow arrowheads). (r) CET1WI on follow-up MRI a month after the fifth resection, showing the eleventh disseminated recurrence around the resection cavity and in the ventricular wall (yellow arrowheads). CET1WI: Contrast-enhanced T1-weighted imaging, MRI: Magnetic resonance imaging, GTR: Gross total resection, RT: radiotherapy, Dab: Dabrafenib, Tra: Trametinib.
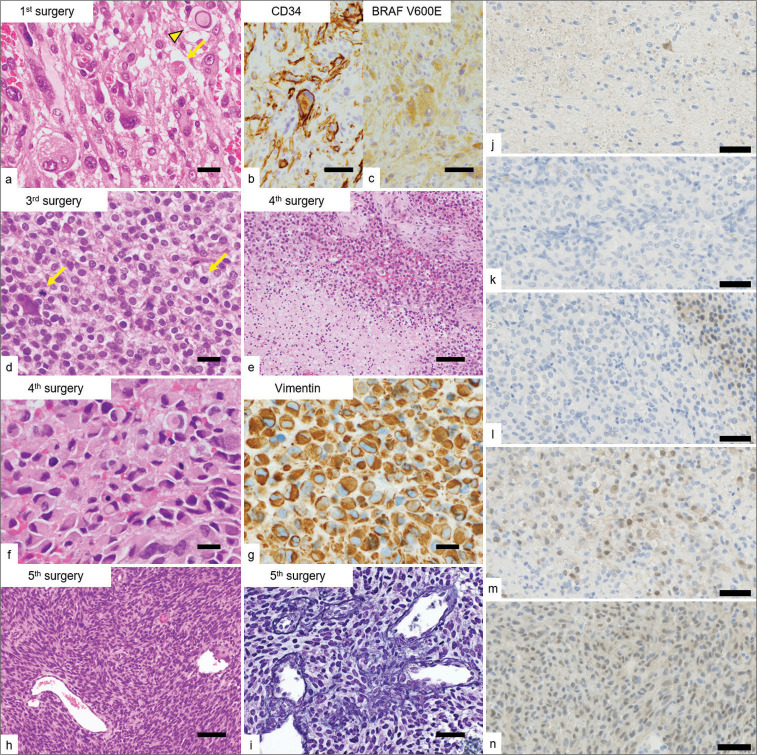
Figure 4:
Microscopic appearances of the resected specimens. (a) The proliferation of pleomorphic and spindle cells with occasional intranuclear pseudo-inclusions (arrowhead) and eosinophilic granular bodies (arrow) in the initially resected specimen. (b and c) Immunohistochemically, the tumor cells were positive for CD34 and BRAF V600E-mutant proteins. (d) The proliferation of tumor cells with epithelioid features showing brisk mitotic activity (arrows) in the recurrent tumor (3rd resection). (e) Coagulative tumor necrosis in the recurrent tumors (4th resection). (f and g) The proliferation of rhabdoid cells with vimentin-positive cytoplasmic inclusions in the recurrent tumors (4th resection). (h) The proliferation of spindle cells in an interlacing fascicular pattern with occasional intervening reticulin fibers in the recurrent tumor, imparts a sarcomatoid appearance (5th resection). (i) Reticulin staining (5th resection). (j-n) ERK1/2 staining (each resection). The ERK1/2 signaling of drug-resistant tumors was expressed strongly despite the presence of the combination therapy with BRAF and MEK inhibitor. (m and n) Scale bars (a, d, f, g) 20 µm, (b, c, i, j, k, l, m, n) 50 µm, and (e, h) 100 µm.
DISCUSSION
The most remarkable aspect of this case study was that incidental drug discontinuation contributed to the control of the resistant tumor repeatedly.
A preclinical model demonstrated that resistant melanomas become drug dependent for proliferation and regress when BRAF inhibitor is attenuated. ERK1/2 signal, which is downstream of BRAF, operates within a tightly defined fitness threshold to drive tumor proliferation. Drug discontinuation causes ERK1/2 signal extremes, leading to cell cycle arrest or apoptosis.[3] Based on these results, the SWOG S1320 trial surveyed the effectiveness of intermittent administration of the combination therapy on a 3-week-off, 5-week-on schedule in melanoma patients. Contrary to preclinical studies, the clinical trial found that intermittent administration did not improve progression-free survival. One of the reasons for this result was the possibility that an inappropriate drug administration schedule could diminish the pharmacodynamic effect of drug holidays.[1]
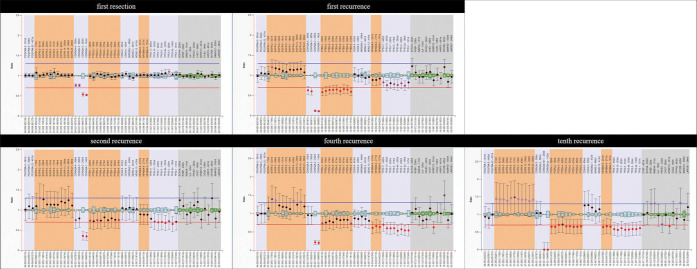
In our patient, drug-resistant tumors were controlled only by incidental drug holidays, although for a limited time. As this is a single case report, any discussion of the mechanism of the clinical course is speculative; however, preclinical studies seemed to reflect our patient’s clinical course.[2,3] To understand the mechanisms, molecular analyses of five resected specimens were performed using multiplexed ligation probe amplification (MLPA). The copy numbers of the glioblastoma-related genes were evaluated using a commercial MLPA kit (P105-D3; MRC-Holland, Amsterdam, Netherlands) containing specific probes and 13 reference probes (SALSA® MLPA® Probemix P105-D3 Glioma-2; MRC-Holland). MLPA results showed an accumulation of gain or loss of the glioblastoma-related genes (EGFR, TP53, CDKN2A, PTEN) with each recurrence, which could be one of the reasons for acquired resistance [Figure 5].[5] These genomic alterations also seemed to be consistent with histological changes [Figure 4a-i] showing gradually epithelioid glioblastoma-like morphologies.
Figure 5:
Analyzed ratio chart of MLPA results obtained using assay P105. Ratio charts indicate an accumulation of gain or loss of glioblastoma-related genes with each recurrence. MLPA: Multiplex ligation-dependent probe amplification.
On the other hand, ERK1/2 staining showed increased positivity in resistant tumors [Figure 4j-n], which seemed to be consistent with a preclinical study arguing that upregulation of the BRAFogies.RK pathway was the mechanism of acquired resistance.[2,3] In addition, a comprehensive genetic analysis showing BRAF V600E amplification in the resistant tumor, which was not identified before the combination therapy, supported this hypothesis [Figure 1 and Table 1].
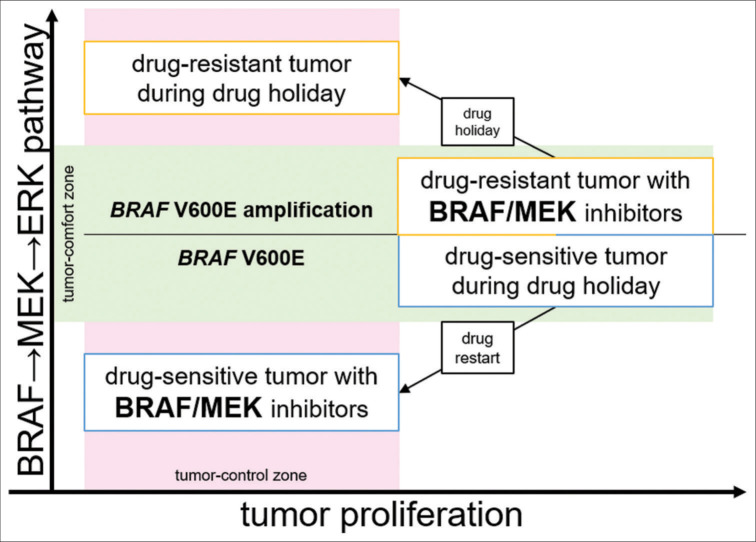
The preclinical study showed drug discontinuation with upregulated BRAFy, supported this hypothesis ds) containing specifiulting in cell cycle arrest or apoptosis.[3] We speculated that the clinical course of our patient might also be consistent with this mechanism [Figure 2]. Malignant gliomas are tumors with high heterogeneity, and we hypothesized that at least two subclones coexisted in our patient: the combination therapy sensitive subclone and the resistant subclone. These subclones might have repeated clonal expansion or contraction in response to the changing tumor environment in the presence or absence of the combination therapy [Figure 6]. This suggests the importance of exploring appropriate drug administration methods to prevent lethal drug resistance and prolong drug sensitivity.
Figure 6:
Concept of appropriate drug administration. An appropriate combination of drug holiday and drug restart may exist to control the aggressive tumor. BRAF: B-Raf proto-oncogene, serine/threonine kinase, MEK: Mitogen-activated protein kinase kinase, ERK: Extracellular signal-regulated kinase.
CONCLUSION
Herein, we report the case of a patient with CNS WHO grade 3 PXA who developed resistance to combination therapy with BRAF and MEK inhibitors. Incidental drug discontinuation contributed to the control of the resistant tumor. This case study provides important insights into novel treatment strategies and their underlying mechanisms for gliomas with BRAF mutations. Owing to the rarity of this tumor and the paucity of previous reports, the unique clinical course of our patient is worth reporting. Further molecular studies may help to understand whether the appropriate administration method of molecularly targeted therapy may delay the acquired resistance or control tumors.
Footnotes
How to cite this article: Inoue H, Kuroda J, Fujioka Y, Hata N, Mizoguchi M, Yoshii D, et al. Drug-resistant BRAF V600E-mutant recurrent pleomorphic xanthoastrocytoma, CNS WHO Grade 3 successfully resolved with incidental discontinuation of combined BRAF and MEK inhibitor therapy. Surg Neurol Int. 2024;15:417. doi: 10.25259/SNI_734_2024
Contributor Information
Hirotaka Inoue, Email: hiro2866@gmail.com.
Jun-Ichiro Kuroda, Email: jukuroda@kumamoto-u.ac.jp.
Yutaka Fujioka, Email: yutakafujioka19830816@yahoo.co.jp.
Nobuhiro Hata, Email: hatanobu66@oita-u.ac.jp.
Masahiro Mizoguchi, Email: mizoguchi.masahiro.223@m.kyushu-u.ac.jp.
Daiki Yoshii, Email: center.0922@gmail.com.
Hiroyuki Sueyoshi, Email: hiroyukisueyoshi1@gmail.com.
Yuki Takeshima, Email: yuki.take4ma@gmail.com.
Kenji Fujimoto, Email: schwarz_k1216@yahoo.co.jp.
Naoki Shinojima, Email: nshinojima@kuh.kumamoto-u.ac.jp.
Kuniko Sunami, Email: ksunami@ncc.go.jp.
Yoshiki Mikami, Email: mika@kuhp.kyoto-u.ac.jp.
Hideo Nakamura, Email: hnakamur@med.kurume-u.ac.jp.
Akitake Mukasa, Email: mukasa-nsu@umin.ac.jp.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Algazi AP, Othus M, Daud AI, Lo RS, Mehnert JM, Truong TG, et al. Continuous versus intermittent BRAF and MEK inhibition in patients with BRAF-mutated melanoma: A randomized phase 2 trial. Nat Med. 2020;26:1564–8. doi: 10.1038/s41591-020-1060-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Corcoran RB, Dias-Santagata D, Bergethon K, Iafrate AJ, Settleman J, Engelman JA. BRAF gene amplification can promote acquired resistance to MEK inhibitors in cancer cells harboring the BRAF V600E mutation. Sci Signal. 2010;3:ra84. doi: 10.1126/scisignal.2001148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Das Thakur M, Salangsang F, Landman AS, Sellers WR, Pryer NK, Levesque MP, et al. Modelling vemurafenib resistance in melanoma reveals a strategy to forestall drug resistance. Nature. 2013;494:251–5. doi: 10.1038/nature11814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ishimaru S, Shimoi T, Sunami K, Nakajima M, Ando Y, Okita N, et al. Platform trial for off-label oncology drugs using comprehensive genomic profiling under the universal public healthcare system: The BELIEVE trial. Int J Clin Oncol. 2024;29:89–95. doi: 10.1007/s10147-023-02439-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neilsen BK, Sleightholm R, McComb R, Ramkissoon SH, Ross JS, Corona RJ, et al. Comprehensive genetic alteration profiling in primary and recurrent glioblastoma. J Neurooncol. 2019;142:111–8. doi: 10.1007/s11060-018-03070-2. [DOI] [PubMed] [Google Scholar]
- 6.Sasame J, Ikegaya N, Kawazu M, Natsumeda M, Hayashi T, Isoda M, et al. HSP90 inhibition overcomes resistance to molecular targeted therapy in BRAFV600E-mutant high-grade glioma. Clin Cancer Res. 2022;28:2425–39. doi: 10.1158/1078-0432.CCR-21-3622. [DOI] [PubMed] [Google Scholar]
- 7.Wen PY, Stein A, van den Bent M, De Greve J, Wick A, de Vos FY, et al. Dabrafenib plus trametinib in patients with BRAFV600E-mutant low-grade and high-grade glioma (ROAR): A multicentre, open-label, single-arm, phase 2, basket trial. Lancet Oncol. 2022;23:53–64. doi: 10.1016/S1470-2045(21)00578-7. [DOI] [PubMed] [Google Scholar]