Abstract
Background:
Primary leptomeningeal gliomatosis (PLG) is a rare neoplasm characterized by the diffuse spread of glial tumor cells throughout the leptomeninges without any evidence of a primary tumor source in the brain or spinal cord parenchyma. Here, we present a case of PLG potentially linked to prior interventional radiotherapy.
Case Description:
The patient was a 75-year-old woman with a history of interventional radiology for a left internal carotid cavernous sinus fistula 13 years before presentation. Routine follow-up fluid-attenuated inversion recovery magnetic resonance imaging revealed a high intensity region spreading from the deep white matter of the subventricular zone (SVZ) to the insular cortex and medial temporal lobe. Subsequently, contrast-enhanced T1-weighted imaging revealed an enhanced effect consistent with extensive leptomeninges extending from the basilar cistern to the left Sylvian fissure. The patient underwent surgery, and subsequently histological examination of extracted tissue revealed a glioblastoma (GBM). Despite postoperative concurrent chemoradiotherapy and adjuvant temozolomide chemotherapy, the tumor increased in size, and the patient died 2 months postoperatively.
Conclusion:
This case highlights the importance of careful follow-up and early therapeutic intervention in PLG, as it can be difficult to diagnose leptomeningeal lesions alone. This case also raises the possibility of radiation-induced GBM, and the criteria for diagnosis were fully met. The progression of PLG from the SVZ to the leptomeningeal site was tracked using imaging, providing valuable insights into the pattern of spread of this rare condition.
Keywords: Glioblastoma, Primary leptomeningeal gliomatosis, Radiation-induced glioblastoma, Subventricular zone
INTRODUCTION
Leptomeningeal diseases are known complications of metastatic cancers, including melanoma and breast, lung, and gastrointestinal cancer. Primary central nervous system (CNS) tumors, lymphoma, leukemia, and multiple myeloma are all common neoplastic tumors associated with leptomeningeal disease.[15] Conversely, leptomeningeal gliomatosis (LG) is rare due to its rapid progression.[15] LG is a morphological variation of the spreading pattern of central nervous neoplasms. Primary leptomeningeal gliomatosis (PLG) is a neoplastic condition in which glial tumor cells extend diffusely throughout the leptomeninges without any evidence of a primary tumor in the brain or spinal cord parenchyma.[1,14] PLG has a poor prognosis, while diagnosis is difficult. By the time PLG is detected, it is often advanced and only diagnosed by imaging. There have been several reports of cases of PLG, but none have tracked its pattern of progression. Herein, we report a case of PLG in which the extended PLG pattern could be followed by imaging.
CASE DESCRIPTION
The patient was a 75-year-old woman with a history of interventional radiology (IVR) for a left internal carotid cavernous sinus fistula (CCF) 13 years before presentation [Figure 1a]. The patient visited our hospital each year to undergo follow-up, throughout which time, magnetic resonance imaging (MRI) showed no recurrence of the CCF or any other lesions on fluid-attenuated inversion recovery (FLAIR) [Figure 1b]. However, routine follow-up MRI revealed a region of high intensity extending from the deep white matter of the subventricular zone (SVZ) to the insular cortex and medial temporal lobe on FLAIR, while contrast-enhanced T1-weighted imaging (CE-T1WI) revealed an enhanced enhancing effect consistent with extensive leptomeninges from the basilar cistern to the left Sylvian fissure [Figures 1c and d]. The cerebral blood volume was not elevated. Vasculitis and metastatic lesions could also be considered on the radiographs of the hand and knee joints. Computed tomography (CT) of the torso was performed, but no obvious abnormal findings were noted. Blood test results were normal.
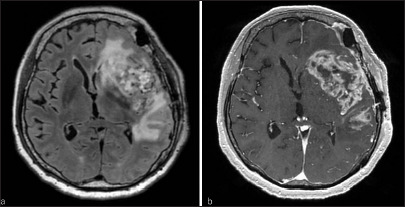
Figure 1:
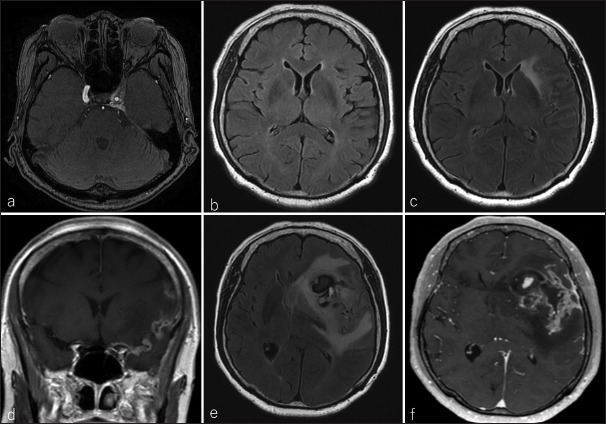
(a) Magnetic resonance angiography in the axial view revealed a left internal carotid cavernous sinus fistula (CCF) 13 years before the presentation; (b) imaging 1 year before presentation showed no occurrence of CCF or abnormal signal in the left subventricular zone (SVZ). (c) At presentation, the SVZ was highly intense on fluid-attenuated inversion recovery (FLAIR), and (d) extensive leptomeninges from the basiler cistern to the left Sylvian fissure could be observed on contrast-enhanced T1 weighted imaging (CE-T1WI). After 2 months, the tumor was enlarted and bled on (e) FLAIR and (f) CE-T1WI images.
After 2 months, the patient was admitted due to motor aphasia and right hemiparesis, at which point an MRI revealed a contrast-enhanced, enlarged leptomeningeal lesion [Figures 1d-f]. Subsequently, the patient underwent surgery through a left frontotemporal craniotomy involving an opening of the Sylvian fissure, which was strongly adherent due to previous IVR. The lesion exhibited strong fluorescence following administration of 5-aminolevulinic acid. A tumor lesion with a mixed hematoma in the left frontal lobe was excised [Figures 2a-d]. Histological examination revealed the proliferation of atypical oval or polygonal cells with hyperchromatic irregularly shaped nuclei and variable amounts of eosinophilic cytoplasm with necrotic areas, palisading necrosis, and microvascular proliferation [Figure 3]. Immunohistochemistry further revealed positive staining for glial fibrillary acidic protein (GFAP) and O6-methylguanine- DNA methyltransferase. Mitotic figures were readily detected while staining for isocitrate dehydrogenase (IDH) 1 was negative. The patient was diagnosed with glioblastoma (GBM), IDH-wild type (World Health Organization CNS grade 4). A postoperative Stupp regimen, including concurrent chemoradiotherapy (CRT) (40 Gy in 15 fractions) followed by adjuvant temozolomide (TMZ) (75 mg/m2) chemotherapy, was administered as therapy. At the end of CRT, MRI revealed an increase in tumor size from the left frontal lobe to the temporal lobe [Figure 4]. Her symptoms rapidly worsened, and she died 2 months after surgery.
Figure 2:
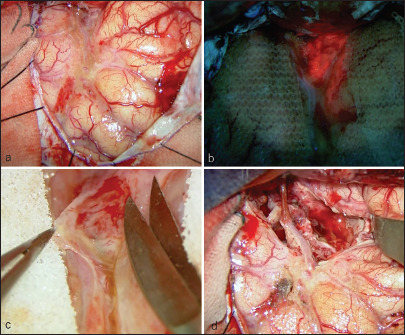
Intraoperative images. (a) After opening the dura mater, (b) the lesion showed strong fluorescence with 5-aminolevulinic acid. (c) The sylvian fissure was strongly adherent because of previous interventional radiology, and (d) the tumor was removed to the maximum extent possible.
Figure 3:
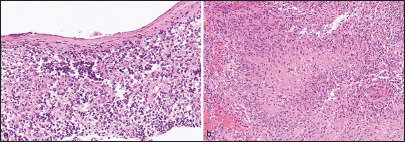
Histopathological findings of the surgical specimen in the leptomeningeal layer. (a) (×200) Hematoxylin and eosin (HE) staining reveled atypical oval or polygonal cells with hyperchromatic irregularly shaped nuclei and (b) (HE ×100) necrosis.
Figure 4:
One month after surgery, the tumor increased in size from the left frontal lobe to the temporal lobe on (a) fluid-attenuated inversion recovery and (b) contrast-enhanced T1-weighted imaging.
DISCUSSION
PLG is defined as a neoplasm confined to the meninges without any evidence of a primary tumor in the brain or spinal cord parenchyma, which develops in heterotopic glial cells within the meninges. Heterotopic glial cells can be observed in up to 1% of the normal population but have been noted in up to 25% of those with coexisting CNS malformations.[2] A prior study characterized the distribution of these heterotopic cells as follows: cortex, 4%; midbrain, 10.5%; pons, 15%; medulla, 57%; cervical, 10.3%; thoracic, 10.5%; and lumbosacral, 20%.[7] MRI results of such lesions generally include enhancement of the exclusive lesions in the pia mater, which are prone to involvement in the posterior fossa, basilar cistern, spinal cord, peri-ventricular lesions, ventricular enlargement, and effacement of the cortical sulcus.[10,18] However, visualization of the invasion of diffuse gliomas is difficult using imaging.[6] Histological findings of the PLG showed neoplastic glial cells abutting the dura. The high-grade type showed microvascular proliferation; however, necrosis was limited to only a few cells. Immunostaining is generally positive for GFAP and vimentin, and sometimes the S100 protein and oligodendrocyte transcription factor 2.[2,12] Molecular biology studies are not uniform.[2,12] Although the median survival of patients with PLG is extremely poor (8 months), TMZ can extend survival to 15 months,[8] and its efficacy is promising.
In our case, the patient underwent MRI annually, and after 13 years of treatment, the CCF showed a high signal on FLAIR of the SVZ. CE-T1WI revealed no obvious intraparenchymal tumor but did indicate leptomeningeal enhancement. Vasculitis and metastatic lesions were considered differential diagnoses; however, blood tests and CT revealed no associated abnormalities. There are three diagnostic criteria for PLG: (1) no attachment of the tumor to the brain parenchyma, (2) no evidence of intra-axial lesions, and (3) leptomeningeal encapsulation of the tumor.[17] MRI confirmed that all of these criteria had been fulfilled. SVZ localization in GBM is associated with a high rate of leptomeningeal dissemination and a decreased overall survival.[3,13] In the present case, PLG was visible on MRI from the SVZ disease, extending into the leptomeningeal site. Diagnosis of PLG from only leptomeningeal lesions was difficult, resulting in treatment delay. In such cases, careful follow-up and early therapeutic intervention are important.
Radiation-induced neoplasms of the CNS are rare and include meningiomas, sarcomas, gliomas, and gliosarcomas. Gliomas are the second most frequently identified radiation-induced CNS neoplasm.[9] There are four criteria for diagnosis: tumor generally occurs within the irradiated field; a sufficient latency period must exist between irradiation and tumor incidence; the radiation-induced tumor must be proven to be of a different histological type from the original neoplasm; and the patient must not have any other pathologies favoring the development of tumors.[5,16] The mean irradiation dose associated with such tumors is 37.6 ± 20 Gy. In contrast, the mean time from cranial irradiation to the onset of disease is 9 years. However, it has been please reported that approximately 10% of all cases developed at an irradiation dose of <16 Gy.[11,16] In terms of tumor site, the frontal, temporal, and occipital lobes predominate, with incidences of 32.7%, 26.9%, and 22.8%, respectively.[16] In this case, the patient had received IVR treatment 13 years before diagnosis, and the tumor had developed at the site of irradiation. Furthermore, no other tumors were present, and there were no pathologies favoring tumor development. This tumor, therefore, satisfied the criteria for diagnosis as a radiation-induced CNS neoplasm.
There have been no prior reports of radiation-induced GBM extending to the leptomeningeal dissemination. However, studies have indicated that glioma cells migrate from the initial site along the brain vessels to the subpial, subarachnoid, and subependymal spaces and tend to invade individuals or small groups in distant territories and abuse pre-existing supply lines.[4,6] It has previously been suggested that some PLG include gliomas that originate in the SVZ and extend into leptomeningeal dissemination.
CONCLUSION
PLG is thought to be caused by ectopic glial cells. However, radiation-induced GBM can occur in the SVZ and spread to the leptomeningeal site, resulting in PLG, as in the present case. Because PLG can present during the developmental process, as in the present case, careful follow-up and early therapeutic intervention are important.
Footnotes
How to cite this article: Nomura N, Nagasaka S, Suzuki K, Yamamoto J. Imaging-tracked progression of primary leptomeningeal gliomatosis: A case report. Surg Neurol Int. 2024;15:411. doi: 10.25259/SNI_759_2024
Contributor Information
Noriaki Nomura, Email: noriaki11230@med.uoeh-u.ac.jp.
Shohei Nagasaka, Email: sn-2ki-88@med.uoeh-u.ac.jp.
Kohei Suzuki, Email: s-kohei@clnc.uoeh-u.ac.jp.
Junkoh Yamamoto, Email: yama9218@med.uoeh-u.ac.jp.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Autran D, Barrie M, Matta M, Monserrat C, Campello C, Petrirena G, et al. Leptomeningeal gliomatosis: A single institution study of 31 patients. Anticancer Res. 2019;39:1035–41. doi: 10.21873/anticanres.13210. [DOI] [PubMed] [Google Scholar]
- 2.Bathla G, Gupta S, Moritani T. Primary leptomeningeal glioblastoma with systemic metastases-case report and review of literature. Clin Imaging. 2015;39:672–6. doi: 10.1016/j.clinimag.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 3.Battista F, Muscas G, Dinoi F, Gadda D, Della Puppa A. Ventricular entry during surgical resection is associated with intracranial leptomeningeal dissemination in glioblastoma patients. J Neurooncol. 2022;160:473–80. doi: 10.1007/s11060-022-04166-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Birzu C, Tran S, Bielle F, Touat M, Mokhtari K, Younan N, et al. Leptomeningeal spread in glioblastoma: Diagnostic and therapeutic challenges. Oncologist. 2020;25:e1763–76. doi: 10.1634/theoncologist.2020-0258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cahan WG, Woodard HQ, Higinbotham NL, Stewart FW, Coley BL. Sarcoma arising in irradiated bone: Report of eleven cases 1948. Cancer. 1998;82:8–34. doi: 10.1002/(sici)1097-0142(19980101)82:1<8::aid-cncr3>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 6.Claes A, Idema AJ, Wesseling P. Diffuse glioma growth: A guerilla war. Acta Neuropathol. 2007;114:443–58. doi: 10.1007/s00401-007-0293-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cooper IS, Kernohan JW. Heterotopic glial nests in the subarachnoid space; histopathologic characteristics, mode of origin and relation to meningeal gliomas. J Neuropathol Exp Neurol. 1951;10:16–29. doi: 10.1097/00005072-195110010-00002. [DOI] [PubMed] [Google Scholar]
- 8.Hansen N, Wittig A, Hense J, Kastrup O, Gizewski ER, Van de Nes JA. Long survival of primary diffuse leptomeningeal gliomatosis following radiotherapy and temozolomide: Case report and literature review. Eu J Med Res. 2011;16:415–9. doi: 10.1186/2047-783X-16-9-415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hill MD, Mackenzie I, Mason WP. Radiation-induced glioma presenting as diffuse leptomeningeal gliomatosis: A case report. J Neuro Oncol. 2001;55:113–6. doi: 10.1023/a:1013337802429. [DOI] [PubMed] [Google Scholar]
- 10.Ishige S, Iwadate Y, Ishikura H, Saeki N. Primary diffuse leptomeningeal gliomatosis followed with serial magnetic resonance images. Neuropathology. 2007;27:290–4. doi: 10.1111/j.1440-1789.2007.00760.x. [DOI] [PubMed] [Google Scholar]
- 11.Lee JW, Wernicke AG. Risk and survival outcomes of radiation-induced CNS tumors. J Neurooncol. 2016;129:15–22. doi: 10.1007/s11060-016-2148-3. [DOI] [PubMed] [Google Scholar]
- 12.Lepreux S, Sagnier S, Perez JT, Léger F, Sibon I, Vital A. Primary diffuse leptomeningeal gliomatosis: Do we miss the diagnosis? Clin Neuropathol. 2017;36:222–6. doi: 10.5414/NP301018. [DOI] [PubMed] [Google Scholar]
- 13.Mistry AM, Kelly PD, Gallant JN, Mummareddy N, Mobley BC, Thompson RC, et al. Comparative analysis of subventricular zone glioblastoma contact and ventricular entry during resection in predicting dissemination, Hydrocephalus, and survival. Neurosurgery. 2019;85:E924–32. doi: 10.1093/neuros/nyz144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Narayan V, Savardekar A, Mohammed N, Patra DP, Georgescu MM, Nanda A. Primary focal intracranial leptomeningeal glioma: Case report and review of the literature. World Neurosurg. 2018;116:163–8. doi: 10.1016/j.wneu.2018.04.080. [DOI] [PubMed] [Google Scholar]
- 15.Nayar G, Ejikeme T, Chongsathidkiet P, Elsamadicy AA, Blackwell KL, Clarke JM, et al. Leptomeningeal disease: Current diagnostic and therapeutic strategies. Oncotarget. 2017;8:73312–28. doi: 10.18632/oncotarget.20272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamanaka R, Hayano A, Kanayama T. Radiation-induced gliomas: A comprehensive review and meta-analysis. Neurosurg Rev. 2018;41:719–31. doi: 10.1007/s10143-016-0786-8. [DOI] [PubMed] [Google Scholar]
- 17.Yamasaki K, Yokogami K, Ohta H, Yamashita S, Uehara H, Sato Y, et al. Case of primary diffuse leptomeningeal gliomatosis. Brain Tumor Pathol. 2014;31:177–81. doi: 10.1007/s10014-014-0176-2. [DOI] [PubMed] [Google Scholar]
- 18.Zhu M, Zheng J, Zhu Y, Wan H, Wu Y, Hong D. Diffuse leptomeningeal gliomatosis initially presenting with intraventricular hemorrhage: A case report and literature review. BMC Neurol. 2015;15:77. doi: 10.1186/s12883-015-0341-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


