Abstract
Background:
The United States (US) has one of the highest rates of gunshot-related incidents in the world. Gunshot wounds to the head (GSWH) in the pediatric population are also common, with high morbidity and mortality rates.
Methods:
We performed a retrospective study to analyze if there was a notable change in trends in pediatric GSWH at our Level 1 Pediatric Trauma Center due to the COVID-19 pandemic. A retrospective study was conducted including patients under the age of 18 presenting with GSWH from January 2014 to May 2023. Variables assessed included demographics, interventions, and outcomes. Data from the county’s Child Death Review Team Annual Report on mortality related to gunshot-related deaths from January 2014 to June 2023 were analyzed.
Results:
In total, thirty-five patients were evaluated at our institution for GSWH. Nineteen patients were treated during the 6 years before the pandemic and sixteen during the 3-year pandemic. Nine patients died at the hospital, with an overall increase during the pandemic. In the county, seventy-two children were killed from gun violence, with 58% (42) from GSWH. Death from GSWH increased in the county cohort during the pandemic.
Conclusion:
The pandemic affected the outcomes of patients with GSWH at our institution with an overall increase in rates of self-inflicted and drive-by shootings, a doubling of neurosurgical interventions, an increase in acuity of care for long-term disposition, and an increase in mortality. At a county level, there was an increase in overall deaths from GSWHs, the majority of which were nonaccidental.
Keywords: COVID-19 pandemic, Gunshot wound to the head, Pediatric trauma

INTRODUCTION
The United States (US) has the highest rate of gunshot-related deaths in all age groups among high-income countries.[1,10] The rate of firearm deaths in the US reached up to 14.5/per 100,000 people in 2022.[23] In the pediatric population, firearm-associated violence is a significant cause of morbidity and mortality and accounts for up to 20% of fatalities of all injury mechanisms and up to 26% of fatalities in those up to 10 years of age.[27] In addition, it is estimated that 20 to 60% of children with gunshot wounds to the head (GSWH) do not survive.[6,7] While the more likely mechanism of firearm-related injury in adolescents is homicide and suicide, younger children are more prone to accidental injury at home, which is the leading cause of GSWH in children <12 years of age.[4,7] More specifically, in the US, unintentional injury is the number one cause of death in those <12 years of age, and firearm injuries make up more than a quarter of these numbers.[4] Gunshot wounds (GSWs) in the pediatric population are, in part, exacerbated by the accessibility of firearms at home, with the prevalence of firearms ranging from 18% up to 64% in the US.[7]
The COVID-19 pandemic was a new major stressor that had a negative impact on children and may have amplified firearm-related injuries. Stay-at-home mandates and school closures precipitated feelings of loneliness, anxiety, depression, and increased tension at home.[4,15] In addition, the COVID-19 pandemic also saw increased rates of firearm ownership and purchases. This, in combination with COVID-19-related financial strain, psychosocial stress, and anxiety, may have contributed to the increased rates of firearm violence and injuries in the pediatric age group during this time.[4]
The pandemic proved to be especially burdensome to low-income and violence-prone communities. San Bernardino County is a diverse geographic and socioeconomic landscape that includes populations of low socioeconomic status (SES), remote living conditions, and poor healthcare access.[5,13] It is also home to high crime rates, with the violent crime rate in San Bernardino in 2021 involving 584 victims of violent crime/100,000 people in comparison to the rate of 481.2 victims/100,000 in California.[13,18] The violent crime rate in San Bernardino increased 15% from 2018 to 2019, and the number of homicide victims increased from 126 victims in 2018 to 181 victims in 2020.[13] Trends in the number of victims of assault with firearms followed a similar pattern, increasing from 609 victims in 2019 to 865 victims in 2020.[1] These patterns correlate with the beginning of the COVID-19 pandemic, suggesting that it may have magnified the already present disparity in violent crime rates in this region. Our Children’s Hospital is in the southwest corner of San Bernardino County, so we sought to analyze the mortality associated with GSWH in the pediatric population in our region and identify any changes in patterns associated with the COVID-19 pandemic.
MATERIALS AND METHODS
Following Institutional Review Board approval [IRB# 5230304], we identified and analyzed the cases of children up to 18 years of age who presented to our hospital with GSWH between January 2014 and May 2023. Patient data collection included demographics, prehospital course, presentation, resuscitation efforts, incident details, interventions, length of hospital stay, mortality, and organ donation in those who died.
To understand the greater problem in our county, we also obtained data from the Children’s Network Child Death Review Team Annual Report regarding all GSW-related pediatric mortalities from January 2014 to June 2023 in San Bernardino County. Variables available through this data include the date of the accident, the age of the victim, the location of GSW on the body, and whether the context of the GSW was an accident, homicide, or suicide. We isolated GSWHs from this data and analyzed the total number of pediatric GSWH deaths and their patterns in relation to the COVID-19 pandemic.
RESULTS
Hospital cohort overview
Our total hospital cohort of pediatric patients with GSWH was 35. Nineteen patients were cared for in the 6 years before the pandemic, from January 2014 to December 2019. Sixteen were treated from January 2020 to May 2023 [Graph 1].
Graph 1:
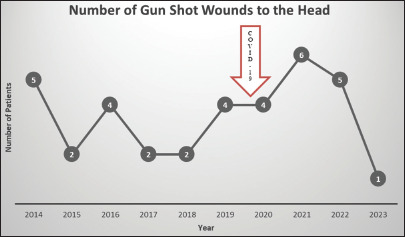
Hospital gunshot wounds to the head per year.
Hospital cohort demographics
The average age of our patients was 13 years, with a range of 2–17. The average age increased from 13.1 before the pandemic to 14.7 during the pandemic. We found that most patients were male: 82.8%. As for insurance status, two patients did not have health insurance, two had private insurance, twenty-five had Medicaid or Medical, and six had a Health Maintenance Organization.
Hospital cohort incident location and timing
The site of the incident occurred at 18 different zip codes, spanning three counties [Figure 1].
Figure 1:
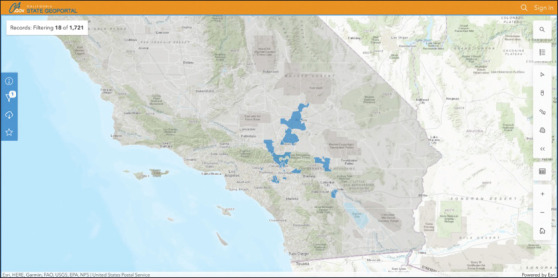
Zip codes of incidents, Courtesy of California State Geoportal.
Before the pandemic, 74% of incidents occurred between the hours of 6 pm and midnight. During the pandemic, this increased to 80%.
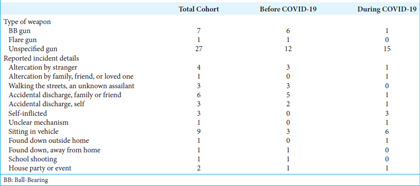
Hospital cohort incident intention and background
From patient, family, or social work reports, information regarding the details of the shooting was abstracted. Before the pandemic, 31% (6) of GSWH were from Ball-Bearing (BB) guns. In addition, 37% (7) of shootings were accidental during this time, with 5 occurring from accidental discharges by family or friends and 2 due to accidental discharge by self. One patient was shot during a school shooting. Other common causes were an altercation with a stranger (3), an unknown assailant on the street (3), and an unknown assailant while in a car (3). There were no self-inflicted GSWHs in the prepandemic cohort.
During the pandemic, the total amount of accidental shootings decreased, with 13% (2) of all patients presenting after accidents. Most incidents during the pandemic, or 38% (6), were related to assault by an unknown assailant while sitting in a vehicle. The percentage of self-inflicted incidents was 19% (3). The number of GSWH while sitting in a vehicle doubled from three to six, while being shot outside on the street by an unknown assailant predominantly occurred before the pandemic with three victims [Table 1].
Table 1:
Hospital cohort incident details.
Hospital cohort means of arrival
Nearly 60% (21) of our patients were transferred from outside hospitals. Before the pandemic, 63% (12) of patients were transferred, with only a slight decrease to 56% (9) of patients during the pandemic [Table 2].
Table 2:
Hospital arrival information.
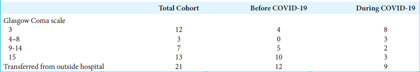
Hospital cohort arrival Glasgow Coma Scale (GCS)
Prepandemic, 21% (4) of patients arrived with an initial GCS of 3 and 53% (10) with a GCS of 15. During the pandemic, 50% (8) of patients arrived with a GCS of 3 and 19% (3) with a GCS of 15. In summary, there was an overall decrease in the number of patients presenting with a GCS of 15 between the cohorts, and there was an increase in patients with a GCS of 3, suggesting an increase in injury severity [Table 2].
Hospital computed tomography review
For the majority of patients who arrived, 77% (27) underwent computed tomography of the head (CTH). Of the patients who eventually died as a result of their injuries, only 67% (6) underwent a CTH [Table 3], as the remaining were declared deceased before imaging was performed. In the deceased patients, CTH findings were notable for all patients having injuries that crossed the midline. All patients had at least six lobes involved, with an average of eight lobes. The common lobes involved in all patients were the right cerebellar and the left temporal. Figure 2 demonstrates the coronal findings of Patient 1, showing the crossing of the midline.
Table 3:
Hospital CT head lobe involvement for deceased patients.
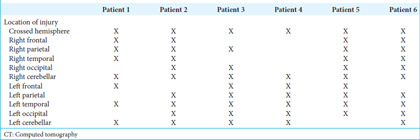
Figure 2:
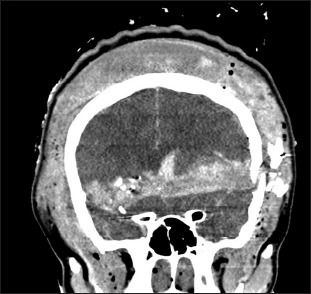
Coronal view of computed tomography of the head of the deceased patient showing crossing of the midline.
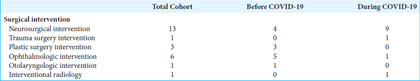
Hospital surgical intervention
Neurosurgical intervention was required in 37% (13) of the total cohort. Before the pandemic, 21% (4) of patients required a neurosurgical intervention, which more than doubled to 56% (9) of patients during the pandemic. Ophthalmology and plastic surgery interventions primarily occurred before the pandemic [Table 4]. In addition, during the pandemic, blood product requirements and ventilation days increased.
Table 4:
Hospital surgical intervention.
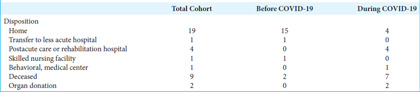
Hospital length of stay and disposition
Before the pandemic, the majority, or 79% (15) of patients’ length of stay was <1 week. Prolonged stays of up to 1 month occurred in ~11% (2) and >1 month in 5% (1). During the pandemic, the rate of prolonged hospital stays increased. Just over half of patients, or 56% (9), were admitted for less than a week, while 25% (4) stayed for up to 1 month and 13% (2) for over 1 month.
There was a notable change in disposition between cohorts. For GSWH before the pandemic, 79% (15) of patients were discharged home. This decreased to only 25% (4) of patients during the pandemic. In addition, 25% (4) were discharged to a postacute care rehabilitation hospital and 6% (1) to a behavioral medical center. The remainder of the pandemic cohort, or 44% (7), died from their injuries. Of the seven patients who died, two became organ donors. During the pandemic, the rate of mortality from GSWH more than tripled [Table 5].
Table 5:
Hospital disposition.
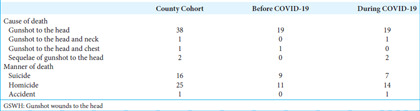
County cohort data
During the 9 years from January 2014 to June 2023, 72 children were killed by all forms of gun violence in the county of San Bernardino. Of the 72 deaths, 42 deaths, or 58%, resulted from GSWH. Twenty deaths occurred over the 6 years from January 2014 to December 2019, and twenty-two deaths occurred over the 3.5 years from January 2020 to June 2023. Overall, 38% (16) of GSWH deaths were a result of self-inflicted injury, and 60% (25) were classified as homicide.
Before the pandemic, 45% (9) of children were killed by self-infliction, while during the pandemic, that decreased to 32% (6) of deaths. Homicide accounted for 55% (11) of deaths before the pandemic and 64% (14) of deaths after. One patient was killed during the pandemic because of an accident [Table 6]. County data demonstrated an overall increase in mortality from GSWH. However, the county data’s manner of death noted a decrease in self-inflicted deaths and an increase in homicide. This slight difference in the manner of death between hospital and county data could be reflected in the lack of accounting for the other major counties our hospital serves.
Table 6:
San Bernardino county GSWH deaths.
DISCUSSION
In the US, unintentional injury is the number one cause of death in the pediatric population and the fourth cause of death in those under 1 year old.[26] Within this category, GSW injury is a leading cause of trauma death in children, second only to motor vehicle accidents, and more than 45% of children discharged following a GSW injury are estimated to have acquired a new disability.[3] Further, GSWH accounts for 21–46% of inpatient deaths following pediatric traumatic brain injury.[7] These numbers are magnified in areas of increased violent crime, with 42 children killed from GSWH in San Bernardino County over just 9 years. Nine of these deaths were declared at our hospital.
Our hospital’s data reveal an exacerbation in the prevalence and severity of pediatric GSWH during the COVID-19 pandemic. Multiple studies have reported increased rates of firearm-related injuries, child-involved shootings, and firearm homicides during the same period.[4,9,16] Orantes et al. presented a 47% increase in firearm homicides in those <18 years of age from 2019 to 2020.[16] Our study showed an increase in GSWH during the COVID-19 pandemic associated with increased case severity and higher mortality rates. The worsened initial GCS scores evidence this: the doubled rate of neurosurgical interventions and the increased average length of stay, mortality rate, and blood product utilization.
The demographic patterns examined in this study resemble national patterns associated with GSW violence. Of those treated for GSWH at our hospital, 83% were male. In addition, 71% of patients had Medicaid or Medi-Cal coverage, suggesting lower SES. These patterns are consistent with nationwide firearm violence reports citing >83% male involvement accompanied by high rates of government-funded insurance plans.[12,21] The COVID-19 pandemic served to exacerbate problems of violence, poverty, and drug abuse in areas of high baseline rates, such as San Bernardino County, leading to increased rates of gun violence.[2,14]
The negative impacts exerted by COVID-19 on the general population were pronounced in children and may explain the rise in GSWH in this age group. Stay-at-home mandates introduced feelings of loneliness, fear, and worry surrounding personal safety and well-being, including economic concerns and financial stress that impacted the entire household.[11,15,20,25] Physical isolation increases the prevalence of mental health conditions, including depression, anxiety, mood disorders, sleep disorders, and panic disorders, along with low self-esteem.[11] Increased frequency of mental health conditions may have contributed to a significant increase in self-injurious behavior and suicidality. This was demonstrated in a longitudinal study in China that documented a rise in self-injurious behavior and suicidal attempts following school closure in grades 4–8.[25] Similarly, our hospital saw an overall increase in the number of self-inflicted GSWH during the pandemic.
Aside from mental and physical health, additional challenges may have contributed to the heightened prevalence of GSWH during the pandemic. Increased use of psychoactive or illicit substances coupled with limited access to detoxification centers added to rising psychological distress, ultimately leading to more deviant and violent behavior.[28] In addition, the pandemic saw a significant increase in firearm purchases from 21.28/100,000 before the COVID-19 pandemic to 33.12/100,000 during.[4,16] There was also an accompanying rise in 1st-time gun ownership during the pandemic.[9] Many 1st-time buyers were reported not to be safely storing their firearms, facilitating access by children, and potentially contributing to the rise in gun violence.[16]
GSW injuries contribute to the burden of communities beyond mortality alone. Consequences include disabilities involving premature physeal arrest, long-term bullet retention, paralysis, survivor’s guilt, and mental illness.[3,22] These factors are associated with increased healthcare costs and economic burden due to additional surgeries, rehabilitation, medical specialists, healthcare services, special accommodations in school, and the inability to contribute to the workforce. [8,17,24] Pulcini et al. found an increase of $16.5 million in health expenditures in their entire cohort of patients 1 year postfirearm injury, a majority of which was spent on inpatient health encounters.[19] This economic and social impact was indirectly reflected in the increase in illness severity of GSWH at our hospital during the COVID-19 pandemic.
Increased stress experienced during the pandemic, compounded by increased firearm purchases and 1st-time gun ownership rates, may explain the rise in pediatric GSWH during this period. Efforts to combat this growing problem have focused on legislative reform, as states with stronger gun laws demonstrate decreased child-involved shooting incidents compared to states with weaker laws.[3,9]
However, because multiple factors such as mental health, socioeconomic challenges, drug abuse, and firearm safety contribute to the prevalence of gun violence, targeting each of these issues are necessary to decrease gun-related injuries in children in our community.
CONCLUSION
There was a notable effect of the COVID-19 pandemic on GSWH in our hospital cohort, with an increase in self-inflicted and drive-by shootings, a doubling of neurosurgical interventions, an increase in acuity of care for long-term disposition, and an increase in mortality. At a county level, there was an increase in overall deaths from GSWHs during the pandemic, the vast majority of which were nonaccidental. Our goal in this research is twofold: (1) to bring awareness to the reality that gun violence has claimed 72 children’s lives in our county over the past 9 years and (2) to encourage action to better support the mental and social health of our patients and communities with increased discourse about gun access and reform because seventy-two is seventy-two too many.
Acknowledgments
We would like to thank our hospital’s Pediatric Trauma Service Support Team for their contributions to data acquisition.
Footnotes
How to cite this article: Sawaya J, McRae JJL, Mladenov G, Larson JM, Radulescu A, Minasian T. Effect of COVID-19 on pediatric gunshot wounds to the head at a level 1 trauma center. Surg Neurol Int. 2024;15:405. doi: 10.25259/SNI_717_2024
Contributor Information
Jessica Sawaya, Email: jsawaya@students.llu.edu.
Joyce J. L. H. McRae, Email: jmcrae@llu.edu.
Georgi Mladenov, Email: gmladenov@llu.edu.
Joseph Michael Larson, Email: jlarson@students.llu.edu.
Andrei Radulescu, Email: aradulescu@llu.edu.
Tanya Minasian, Email: tminasian@llu.edu.
Ethical approval
The research/study was approved by the Institutional Review Board at Loma Linda University, number 5230304, dated July 13, 2023.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Bernardino CoS. Crime statistics - 2023. City of San Bernardino. 2023. Available from: https://www.sbcity.org/city_hall/police_department/crime_statistics/about_ucr_statistics/crime_statistics/crime_statistics_-_2023 [Last accessed on 2024 Aug 15]
- 2.Bureau USC. Quick facts: San Bernardino County. California, United States. United States Census Bureau. 2022. Available from: https://www.census.gov/quickfacts/fact/table/sanbernardinocitycalifornia,US/RHI725223 [Last accessed on 2024 Aug 15]
- 3.Carter CW, Sharkey MS, Fishman F. Firearm-related musculoskeletal injuries in children and adolescents. J Am Acad Orthop Surg. 2017;25:169–78. doi: 10.5435/JAAOS-D-15-00642. [DOI] [PubMed] [Google Scholar]
- 4.Cohen JS, Donnelly K, Patel SJ, Badolato GM, Boyle MD, McCarter R, et al. Firearms injuries involving young children in the United States during the COVID-19 pandemic. Pediatrics. 2021;148:e2020042697. doi: 10.1542/peds.2020-042697. [DOI] [PubMed] [Google Scholar]
- 5.County SB. 2020 Community health status data report. San Bernardino County. 2020. Available from: https://www.sbcounty.gov/uploads/DPH/Documents/2021/04/SBCCVS__OCVS_Report20_v5.1.pdf [Last accessed on 2024 Aug 15]
- 6.DeCuypere M, Muhlbauer MS, Boop FA, Klimo P., Jr Pediatric intracranial gunshot wounds: The Memphis experience. J Neurosurg Pediatr. 2016;17:595–601. doi: 10.3171/2015.7.PEDS15285. [DOI] [PubMed] [Google Scholar]
- 7.Deng H, Yue JK, Winkler EA, Dhall SS, Manley GT, Tarapore PE. Pediatric firearm-related traumatic brain injury in United States trauma centers. J Neurosurg Pediatr. 2019;24:498–508. doi: 10.3171/2019.5.PEDS19119. [DOI] [PubMed] [Google Scholar]
- 8.DiScala C, Sege R. Outcomes in children and young adults who are hospitalized for firearms-related injuries. Pediatrics. 2004;113:1306–12. doi: 10.1542/peds.113.5.1306. [DOI] [PubMed] [Google Scholar]
- 9.Donnelly MR, Grigorian A, Swentek L, Arora J, Kuza CM, Inaba K, et al. Firearm violence against children in the United States: Trends in the wake of the COVID-19 pandemic. J Trauma Acute Care Surg. 2022;92:65–8. doi: 10.1097/TA.0000000000003347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goel R, Zhu X, Makhani S, Petersen MR, Josephson CD, Katz LM, et al. Blood transfusions in gunshot-wound-related emergency department visits and hospitalizations in the United States. Transfusion. 2021;61:2277–89. doi: 10.1111/trf.16552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, et al. Epidemiology of mental health problems in COVID-19: A review. F1000Res. 2020;9:636. doi: 10.12688/f1000research.24457.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hughes BD, Cummins CB, Shan Y, Mehta HB, Radhakrishnan RS, Bowen-Jallow KA. Pediatric firearm injuries: Racial disparities and predictors of healthcare outcomes. J Pediatr Surg. 2020;55:1596–603. doi: 10.1016/j.jpedsurg.2020.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Indicators SBCC. Crime rate. San Bernardino County Community Indicators. 2021. Available from: https://indicators.sbcounty.gov/safety/crime-rate [Last accessed on 2024 Aug 15]
- 14.Indicators SBCC. Substance abuse. San Bernardino County Community Indicators. 2021. Available from: https://indicators.sbcounty.gov/wellness/substance-abuse [Last accessed on 2024 Aug 15]
- 15.Luijten MA, van Muilekom MM, Teela L, Polderman TJ, Terwee CB, Zijlmans J, et al. The impact of lockdown during the COVID-19 pandemic on mental and social health of children and adolescents. Qual Life Res. 2021;30:2795–804. doi: 10.1007/s11136-021-02861-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Orantes C, Chan HK, Walter D, Chavez S, Ugalde IT. Pediatric firearm injury epidemiology at a level 1 trauma center from 2019 to 2021: Including time of the COVID-19 pandemic. Inj Epidemiol. 2023;10:41. doi: 10.1186/s40621-023-00448-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Orlas CP, Thomas A, Herrera-Escobar JP, Price MA, Haider AH, Bulger EM, et al. Long-term outcomes of firearm injury survivors in the United States: The national trauma research action plan scoping review. Ann Surg. 2021;274:962–70. doi: 10.1097/SLA.0000000000005204. [DOI] [PubMed] [Google Scholar]
- 18.Program FUCR. Federal Bureau of investigation crime data explorer. FBI Uniform crime reporting program; 2022. Available from: https://cde.ucr.cjis.gov/LATEST/webapp/#/pages/explorer/crime/crime-trend [Last accessed on 2024 Aug 15]
- 19.Pulcini CD, Goyal MK, Hall M, Gruhler De Souza H, Chaudhary S, Alpern ER, et al. Nonfatal firearm injuries: Utilization and expenditures for children pre-and postinjury. Acad Emerg Med. 2021;28:840–7. doi: 10.1111/acem.14318. [DOI] [PubMed] [Google Scholar]
- 20.Rodrigues M, Silva R, Franco M. COVID-19: Financial stress and well-being in families. J Fam Issues. 2023;44:1254–75. doi: 10.1177/0192513X211057009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sakran JV, Nance M, Riall T, Asmar S, Chehab M, Joseph B. Pediatric firearm injuries and fatalities: Do racial disparities exist? Ann Surg. 2020;272:556–61. doi: 10.1097/SLA.0000000000004390. [DOI] [PubMed] [Google Scholar]
- 22.Schaechter J, Alvarez PG. Growing up-or not-with gun violence. Pediatr Clin North Am. 2016;63:813–26. doi: 10.1016/j.pcl.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 23.Statistics NCfH. All injuries U.S Department of Health and Human Services. 2024. Available from: https://www.cdc.gov/nchs/fastats/injury.htm [Last accessed on 2024 Aug 15]
- 24.Vella MA, Warshauer A, Tortorello G, Fernandez-Moure J, Giacolone J, Chen B, et al. Long-term functional, psychological, emotional, and social outcomes in survivors of firearm injuries. JAMA Surg. 2020;155:51–9. doi: 10.1001/jamasurg.2019.4533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang G, Zhang Y, Zhao J, Zhang J, Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395:945–7. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilson RF, Mintz S, Blair JM, Betz CJ, Collier A, Fowler KA. Unintentional firearm injury deaths among children and adolescents aged 0-17 years-National Violent Death Reporting system, United States, 2003-2021. MMWR Morb Mortal Wkly Rep. 2023;72:1338–45. doi: 10.15585/mmwr.mm7250a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Woodruff G, Palmer L, Fontane E, Kalynych C, Hendry P, Thomas AC, et al. Nine years of pediatric gunshot wounds: A descriptive analysis. Prev Med Rep. 2022;28:101890. doi: 10.1016/j.pmedr.2022.101890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zaami S, Marinelli E, Varì MR. New trends of substance abuse during COVID-19 pandemic: An international perspective. Front Psychiatry. 2020;11:700. doi: 10.3389/fpsyt.2020.00700. [DOI] [PMC free article] [PubMed] [Google Scholar]


