Abstract
Background
Existing literature supports the efficacy of PAOO in augmenting alveolar bone volume and facilitating orthodontic tooth movement. However, there is a paucity of literature addressing its application in the treatment of adults with skeletal Class III malocclusion. This retrospective clinical study aimed to compare the clinical efficacy of camouflage orthodontic treatment combined with and without PAOO in adult patients presenting with skeletal Class III malocclusion.
Methods
A retrospective study was performed in 38 patients with mild to moderate skeletal Class III malocclusion who underwent orthodontic treatment. Patients were divided into two cohorts: the experimental group, which underwent the PAOO procedure combined with orthodontic treatment, and the control group, which received traditional camouflage orthodontic treatment alone. Radiographic assessments, including lateral cephalograms and cone-beam computed tomography (CBCT) scans, were conducted before treatment (T0) and after treatment (T1) to evaluate changes in maxillary incisor inclination, alveolar bone thickness, and various skeletal and soft tissue parameters.
Results
The experimental group exhibited a significant reduction in the axial inclination of the maxillary incisors after treatment (P < 0.05; U1-PP, -4.97 ± 5.23°). The root apex of the maxillary incisors moved labially, and the A-point moved forward. In contrast, the control group demonstrated significant proclination of the maxillary incisors (P < 0.05; U1-PP, 6.80 ± 7.89°). The ANB assessments demonstrated significant improvements (P < 0.05; 3.03 ± 1.62°), with a significant difference between groups that favored the experimental group. Nasolabial angle and G Vert-Sn increased significantly only in the experimental group (P < 0.05; Nasolabial A, 9.47 ± 12.67°; G Vert-Sn, 2.19 ± 2.56 mm). Compared with T0, labial bone thickness significantly increased in the experimental group at T1, while it decreased significantly in the control group.
Conclusion
The integration of PAOO with orthodontic treatment appears to enhance labial alveolar bone augmentation and facilitate the labial movement of maxillary incisor roots in patients with skeletal Class III malocclusion. Concurrently, it results in significant improvements in patients’ aesthetics of both soft and hard tissue profiles.
Keywords: Skeletal class III, Camouflage orthodontic, PAOO, Alveolar bone augmentation, Aesthetic
Background
Skeletal Class III malocclusion represents a prevalent yet intricate craniomaxillofacial dysplasia characterized by a prognathic mandible and maxillary hypoplasia, as evidenced by insufficient soft tissue in the subnasal region [1, 2]. Additional dental features commonly observed include anterior crossbite or significant proclination of maxillary incisors, impacting both mastication and smile esthetics [3, 4].
In addressing skeletal Class III malocclusion in non-growing patients, the preferred therapeutic approach typically involves a combination of orthodontic and orthognathic treatments to rectify dental and soft tissue anomalies [5]. However, acceptance of orthognathic surgery varies due to factors such as surgical risks and financial considerations. Consequently, for cases of mild or moderate skeletal Class III malocclusion, camouflage treatment using orthodontic appliances presents a practical alternative, albeit with inherent drawbacks. Camouflage orthodontic interventions entail the deliberate displacement of teeth to compensate for the inherent disharmony between the maxilla and mandible, often resulting in undesired excessive labial proclination of the upper incisors [6, 7]. This can compromise the health and stability of the stomatognathic system and yield only marginal improvements in hard and soft tissue esthetics. Furthermore, in the context of Chinese individuals with skeletal Class III malocclusion, anterior dental morphology reveals a prevalence of 16.1% for labial alveolar bone fenestration and 20.7% for dehiscence [8]. The risk of periodontal deterioration and the limitation of bodily labial movement for upper incisors during camouflage orthodontic treatment is greatly increased due to the delicate and tenuous alveolar bone of skeletal Class III malocclusion. Given these challenges, meticulous attention to periodontal safety is imperative in the orthodontic management of adult patients with skeletal Class III malocclusion, emphasizing the necessity for stringent precautions to mitigate periodontal risks and optimize treatment outcomes.
Periodontal accelerated osteogenic orthodontics (PAOO) integrates corticotomy, particulate grafting, and orthodontic forces [9]. Existing literature supports PAOO’s efficacy in expanding tooth movement feasibility, augmenting alveolar bone volume, and fortifying the periodontium [10–12]. It has demonstrated superior outcomes compared to traditional orthodontic treatment due to its ability to increase tooth movement without elevating the risk of apical root resorption while simultaneously reshaping the alveolar bone [9]. Furthermore, a prior meta-analysis also demonstrated its effectiveness in accelerating specific tooth movements and reducing orthodontic relapse [13]. However, in the context of PAOO’s application for skeletal Class III malocclusion, research has predominantly focused on mandibular anterior teeth decompensation and their labial periodontal hard tissue changes, leaving a significant gap in empirical knowledge regarding its use on the maxilla to facilitate the movement of maxillary incisors [14].
Given the underlying biological mechanisms, PAOO for upper front teeth emerges as an advanced adjunctive methodology for managing skeletal Class III malocclusion with a retrognathic maxilla. Further investigations, specifically addressing PAOO’s nuanced impact on the labial movement of maxillary incisor roots and subnasal soft tissue aesthetics, are warranted to inform its clinical application in skeletal Class III malocclusion.
This retrospective clinical study aimed to compare the clinical efficacy of camouflage orthodontic treatment combined with and without PAOO in adult patients presenting with skeletal Class III malocclusion. Specifically, it assessed the movement of maxillary central incisors and alveolar bone thickness using cone-beam computed tomography (CBCT), along with variations in overlaying hard and soft tissues using lateral cephalograms. The findings aimed to offer valuable insights for future clinical research and guide treatment strategies for skeletal Class III malocclusion in adults.
Methods
Selection of the sample
This retrospective study involved patients with mild to moderate skeletal Class III malocclusion who underwent orthodontic treatment at Hangzhou Dental Hospital from January 2018 to September 2023. Approval was obtained from the institutional review board of Hangzhou Dental Hospital in Hangzhou, Zhejiang, China (2023LL08). Based on the inclusion and exclusion criteria, 19 adult patients were enrolled as the experimental group (with PAOO; 5 men, 14 women; mean age, 27.32 ± 5.48 years). Matched with age, sex, and FH-MP, additional 19 adult patients were enrolled as the control group (without PAOO; 5 men, 14 women; mean age, 28.21 ± 5.78 years). Based on the results of the pre-experiment, selecting U1-PP angle as the main outcome measure, the difference between the experimental group and the control group is 6.07, and the standard deviation is 5.67, a minimum sample size of 19 subjects in each group was required to conduct a statistical analysis with a significance level of 0.05 and a statistical power of 90%.
Inclusion criteria were as follows: aged>18 years; skeletal Class III malocclusion with maxillary hypolasia (-5°< ANB<0°, APDI>89°, Wits<-1 mm, SNA ≤ 80°); maxillary mild-moderate crowded; crown-to-root ratios of maxillary central incisor<1; without severe facial asymmetry (>5 mm of lower midline deviation from the facial midline); dental Class I relationship at the end of orthodontic treatment; complete CBCT images and X-ray lateral cephalograms before and after orthodontic treatment.
The exclusion criteria were severe periodontal disease, gingival recession over the upper anterior teeth heavily, endodontic treatment or crown restoration on the upper anterior teeth, maxillary trans-verse deficiency heavily, simple functional crossbite, temporomandibular joint disease, smoking, pregnant or lactating, previous orthodontic or orthognathic treatment, use of any medication that could affect bone metabolism, cleft lip, or palate or other craniofacial syndromes.
Treatment procedures
Orthodontic treatment procedures
In the control group, all patients underwent maxillary non-extraction orthodontic treatment. Metal active self-ligating brackets of the 0.022 × 0.028-inch slot (3 M Minnesota, United States) with standard Roth values were used for all patients. Both dental arches were leveled with continuous nickel-titanium archwires and working up to 0.019 × 0.025-inch stainless steel wires. Anterior crossbites or mild overjet were corrected through controlled buccolingual tipping movements of the anterior teeth using Class III elastics and temporary anchorage devices (TADs). During the finishing stage, final detailing of the occlusion was performed. Fixed retainers were delivered to secure the stability of both arches.
In the experimental cohort, all patients also underwent maxillary non-extraction orthodontic treatment. The orthodontic brackets and archwires utilized were consistent with those employed in the control group. However, prior to PAOO surgery, the brackets on the upper incisors were repositioned inversely on the tooth surfaces to induce negative torque. Upon achieving adequate space and elimination of occlusal interferences for significant movement of the upper anterior teeth, corticotomy with bone grafting surgery was performed on the maxilla. Immediate orthodontic forces were applied to the maxillary anterior teeth post-surgery to control the labial root torque. The major orthodontic treatment of the maxillary anterior teeth lasted for 3 to 5 months, with adjustments every 2 weeks. Meanwhile, class III elastics and TADs as mandible anchorage devices were employed if necessary. Subsequent treatments mirrored those in the control group.
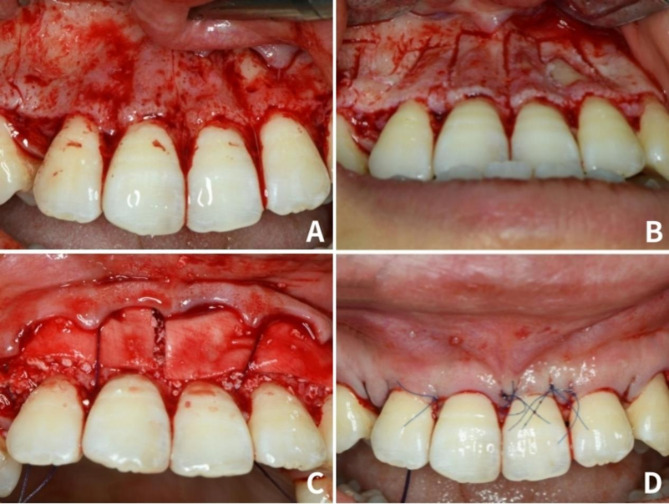
PAOO Surgical procedures
The surgical procedures were carried out by the same periodontist (DY Xuan) for all cases in the experimental cohort. Following local anesthesia administration, crevicular incisions were made on the labial aspect (from the maxillary left first premolar to the right first premolar) using a #15 surgical blade. Full-thickness flaps were raised, and vertical corticotomy was executed in the labial cortical plate between the teeth utilizing a piezoelectric surgical device (UltraSurgery Led, Woodpecker, China). The vertical corticotomy ranged from 2 to 3 mm below the crest of the alveolar bone to 2 to 3 mm below the apex, complemented by a horizontal corticotomy performed 2 to 3 mm below the apices (Fig. 1A and B). Subsequently, bone graft material (Bio-Oss, Geistlich, Switzerland) was applied to the labial aspect of the decorticated anterior cortical bone. A bioabsorbable collagen membrane (Bio-Gide, Geistlich, Switzerland) was employed to cover the graft site entirely. Flaps were repositioned with single-sling sutures and interrupted interdental sutures utilizing non-absorbable 5.0 polyvinylidene fluoride (Asflex, Crownjun, Japan; Fig. 1C and D).
Fig. 1.
Surgical procedure for corticotomy with bone grafting in a subject with skeletal Angle Class III malocclusion. (A) After local anesthesia of the maxillary, full-thickness flaps were elevated on the labial aspect; (B) vertical corticotomy was performed in the cortical plate between the teeth; (C) bone derivative material was placed onto the labial area, then bioabsorbable collagen membrane was placed to completely cover the graft site; (D) flaps were repositioned and sutured
Method of measurements
X-ray lateral cephalogram and large field-of-view (FOV) CBCT imaging using New Tom GiANO (Aperio Services, Verona, Italy) were taken before treatment (T0) and after treatment (T1). CBCT images were recorded in full scan mode (110 kVp; 2.05 mA; 0.15-mm voxel size; scan time, 3.6 s; and FOV of 15*3*12 cm).
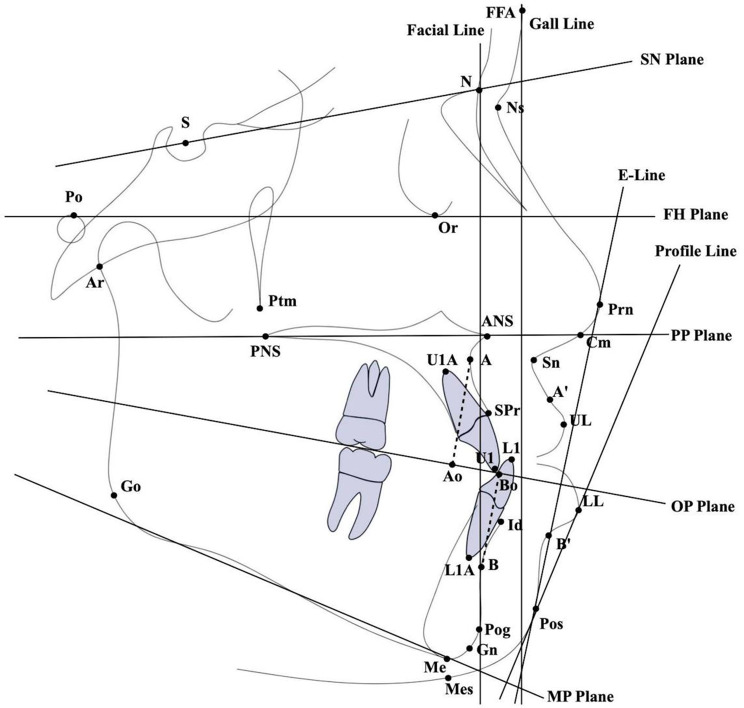
A total of 9 angular measurements and 5 linear measurements were evaluated in both T0 and T1 lateral cephalometric images. The definitions of the 14 measurements are shown in Table 1; Fig. 2.
Table 1.
Description of the cephalometric measurements
| Measurements | Description |
|---|---|
| FH-MP (°) | Angle between FH plane and MP plane |
| SNA (°) | Angle between S-N line and N-point A line |
| ANB (°) | Angle between N-point A line and N-point B line |
| NA-APo (°) | Angle between N-A line and A-Pog line |
| APDI (°) | Facial plane to FH plane ± facial plane to AB ± FH plane to palatal plane |
| Wits (mm) | Wits appraisal (Ao to Bo) |
| U1-NA (°) | Angle formed by the intersection of tooth axis of upper incisor and N-point A line |
| U1-NA (mm) | Distance between the incisal tip of upper incisor and N-point A line |
| U1-PP (°) | Angle formed by the intersection of tooth axis of upper incisor and ANS-PNS line |
| U1-SN (°) | Angle formed by the intersection of tooth axis of upper incisor and S-N line |
| UL-EP (mm) | Distance from point UL to E-line |
| Nasolabial A (°) | Angle formed by intersection of Cm-Sn line and Sn-Ls |
| G Vert-Sn (mm) | Distance from point Sn to Gall line |
| U1-A perp (mm) | Distance between the most labial point of upper incisor and perpendicular line from point A to the FH plane |
Fig. 2.
Landmarks of cephalometric image and lateral cephalometric measurement items used in this study
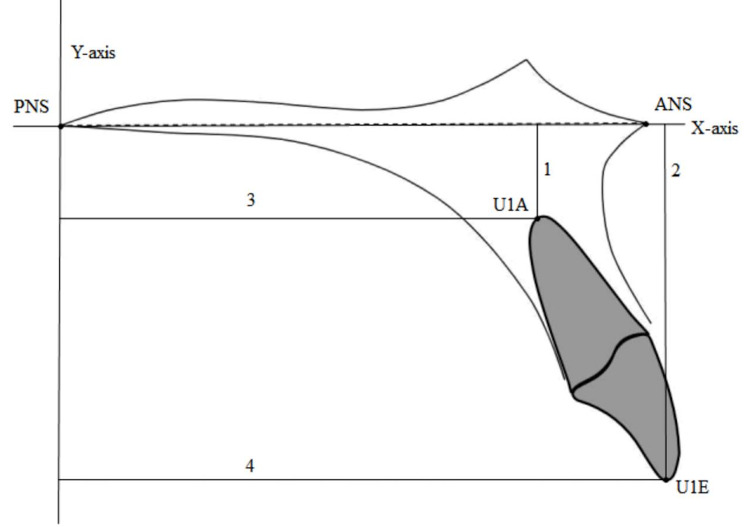
The movement of the maxillary central incisor was assessed by analyzing the displacement of specific landmarks. The anterior nasal spine (ANS)-posterior nasal spine (PNS) line was designated as the X-axis, and the line perpendicular to the X-axis at the PNS was defined as the Y-axis [15]. The following measurements were recorded: (1) U1E-sag, the distance from the incisal tip of the maxillary central incisor (U1) to the Y-axis; (2) U1A-sag, the distance from the root apex of U1 to the Y-axis; (3) U1E-ver, the distance from the incisal tip of U1 to the X-axis; and (4) U1A-ver, the distance from the root apex of U1 to the X-axis (Fig. 3).
Fig. 3.
Landmarks and measurement items of maxillary central incisors. ANS: Anterior Nasal Spine. PNS: Posterior Nasal Spine. U1E: Incisal tip of central incisor. U1A: Root apex of central incisor. X-axis: The line connecting ANS and PNS. Y-axis: The line perpendicular to the X-axis at the PNS. 1: U1A-ver, the distance from the root apex of U1 to the X-axis. 2: U1E-ver, the distance from the incisal tip of U1 to the X-axis. 3: U1A-sag, the distance from the root apex of U1 to the Y-axis. 4: U1E-sag, the distance from the incisal tip of U1 to the Y-axis
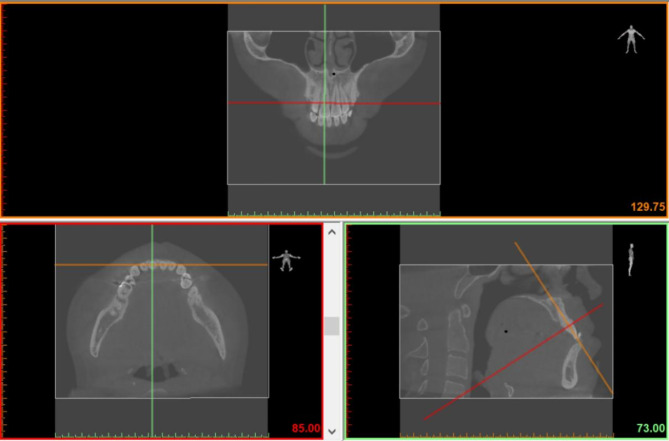
Alveolar bone thickness (ABT) of the maxillary central incisor was measured by importing DICOM files into Mimics software (versus 20.0; Materialise Mimics Medical, Belgium) and selecting axial, coronal, and sagittal visualization displays [16]. The coronal, cross-sectional, and sagittal planes were displayed on the 2D multiplanar reconstructed interface, with three distinct colored lines representing different cross-sections: red for the cross-sectional plane, orange for the coronal plane, and green for the sagittal plane. The image was adjusted so that the orange line on the sagittal plane passed through the incisal edge and apical point, the red line intersected the cementoenamel junction (CEJ), and the green line traversed the midpoint of the edge and apical point on the coronal plane. The sagittal plane was selected as the measurement plane (Fig. 4). The following radiographic data were collected: horizontal ABT on the labial and palatal sides at 3, 6, and 9 mm from the CEJ, which was designated as crestal, mid-root, and apical third (Fig. 5).
Fig. 4.
CBCT image reconstruction and processing. The red line represents the cross-section, the orange line represents the coronal plane, and the green line represents the sagittal plane
Fig. 5.
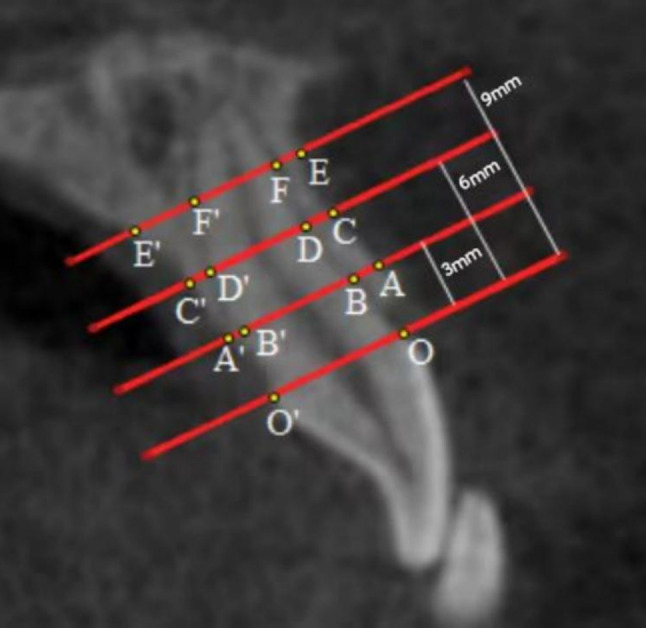
Illustration of measurements and reference points used to evaluate alveolar bone thickness (ABT) based on CBCT examination. O = labial aspect of the cementoenamel junction, O’ = palatal aspect of the cementoenamel junction; A = limit of the labial cortical surface at 3 mm under cementoenamel junction (CEJ-3 mm), A’ = limit of the palatal cortical surface at CEJ-3 mm, B = labial aspect of the root at CEJ-3 mm, B’ = palatal aspect of the root at CEJ-3 mm, C = limit of the labial cortical surface at 6 mm under cementoenamel junction (CEJ-6 mm), C’ = limit of the palatal cortical surface at CEJ-6 mm, D = labial aspect of the root at CEJ-6 mm, D’ = palatal aspect of the root at CEJ-6 mm, E = limit of the labial cortical surface at 9 mm under cementoenamel junction (CEJ-9 mm), E’ = limit of the palatal cortical surface at CEJ-9 mm, F = labial aspect of the root at CEJ-8 mm, F’ = palatal aspect of the root at CEJ-9 mm. The AB, CD, and EF distances were measured as the horizontal bone thickness of the labial aspect at CEJ-3 mm, CEJ-6 mm and CEJ-9 mm, respectively. The A’B’, C’D’, and E’F’ distances were measured as the horizontal bone thickness of the palatal aspect at CEJ-3 mm, CEJ-6 mm, and CEJ-9 mm, respectively
During the measurement period, the identity information of each patient was anonymized to prevent bias. Two examiners performed all the measurements. After a two-week interval, the same examiners repeated the measurements. The intraclass correlation coefficient (ICC) analyzed for interrater agreement ranged from 0.813 to 0.927, thereby confirming the repeatability and reliability of the radiographic evaluation. The differences ranged from 0.12 to 0.29 mm for linear measurements, from 0.34 to 1.45 for angular measurements, according to Dahlberg’s formula.
Statistical analysis
For the measurements derived from CBCT, the mean values of the two maxillary central incisors were utilized in this study. Continuous variables were described as mean ± standard deviation. The normality of the distribution of the variables was assessed by the Shapiro-Wilks test. The independent t test was performed for the comparisons between the two groups, the paired t test was used for the comparisons between baseline and after orthodontic treatment in each group. The P < 0.05 level of significance was chosen for all tests. All statistical analyses were performed with SPSS statistical software (version 21; IBM, Armonk, NY).
Results
The average duration from postoperative PAOO to the completion of orthodontic treatment in the experimental group was 19.40 ± 7.56 months. The overall average treatment duration was 22.85 ± 6.59 months. The average treatment duration in the control group was 32.79 ± 5.08 months.
Change in position of the maxillary central incisor
Table 2 illustrates the movement of the maxillary central incisors. In the experimental group, the incisal tip moved backward while the root apex moved forward. Conversely, in the control group, the incisal tip moved forward while the root apex moved backward, with the movement of the incisal tip being significantly greater than that of the root apex.
Table 2.
Changes in maxillary anterior tooth movement
| Experimental group(n = 19) | Control group(n = 19) | Comparison between groups | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurements | T0 | T1 | T1-T0 | P value | T0 | T1 | T1-T0 | P value | P value | ||
| At T0 | At T1 | T1-T0 | |||||||||
| U1E-ver(mm) | 25.01 ± 3.28 | 25.40 ± 2.44 | 0.39 ± 1.71 | 0.330 | 26.26 ± 3.62 | 25.39 ± 2.83 | -0.88 ± 2.26 | 0.109 | 0.268 | 0.991 | 0.059 |
| U1A-ver(mm) | 8.93 ± 2.05 | 8.47 ± 2.21 | -0.46 ± 1.23 | 0.121 | 8.27 ± 2.50 | 8.68 ± 1.94 | 0.41 ± 1.52 | 0.253 | 0.374 | 0.764 | 0.060 |
| U1E-sag(mm) | 50.14 ± 2.82 | 49.36 ± 1.95 | -0.78 ± 1.71 | 0.061 | 50.64 ± 3.78 | 53.40 ± 2.80 | 2.77 ± 2.71 | < 0.001* | 0.652 | < 0.001* | < 0.001* |
| U1A-sag(mm) | 38.59 ± 2.35 | 39.95 ± 2.00 | 1.35 ± 1.59 | 0.002* | 38.98 ± 1.97 | 37.99 ± 2.39 | -0.99 ± 1.89 | 0.035* | 0.588 | 0.010* | < 0.001* |
Note. Values are presented as mean ± standard deviation. *Statistically significant differences between groups (P < 0.05)
Change in alveolar bone thickness
Dentoalveolar changes surrounding the maxillary central incisors were visible in the CBCT images. As listed in Table 3, the control group exhibited significant labial alveolar bone loss at 3 mm from CEJ (P < 0.05; 0.49 ± 0.35 mm). At 6 mm and 9 mm from CEJ, minimal changes were observed in labial alveolar bone thickness, whereas a significant reduction in palatal alveolar bone thickness was noted (P < 0.05). In the experimental group, significant increases in labial alveolar bone thickness were observed at 3 mm, 6 mm, and 9 mm from CEJ (P < 0.05). Regarding the palatal alveolar bone, there was a slight increase, which was not statistically significant except at 9 mm from CEJ. Furthermore, at the end of orthodontic treatment, the labial and palate alveolar bone thickness at 9 mm from CEJ in the experimental group was substantially greater than in the control group.
Table 3.
Alveolar bone thickness of maxillary central incisors
| Experimental group(n = 19) | Control group(n = 19) | Comparison between groups | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurements | T0 | T1 | T1-T0 | P value | T0 | T1 | T1-T0 | P value | P value | ||
| At T0 | At T1 | T1-T0 | |||||||||
| Labial CEJ-3 mm | 1.09 ± 0.49 | 1.43 ± 0.46 | 0.34 ± 0.53 | 0.011* | 1.01 ± 0.50 | 0.52 ± 0.42 | -0.49 ± 0.35 | < 0.001* | 0.623 | < 0.001* | < 0.001* |
| Labial CEJ-6 mm | 1.00 ± 0.43 | 1.77 ± 0.73 | 0.78 ± 0.90 | 0.001* | 1.28 ± 0.50 | 1.12 ± 0.41 | -0.16 ± 0.37 | 0.073 | 0.071 | 0.002 | < 0.001* |
| Labial CEJ-9 mm | 1.40 ± 0.62 | 2.81 ± 0.97 | 1.42 ± 0.85 | < 0.001* | 1.56 ± 0.63 | 1.95 ± 1.18 | 0.40 ± 0.93 | 0.077 | 0.435 | 0.019* | 0.001* |
| Palatal CEJ-3 mm | 1.39 ± 0.68 | 1.33 ± 0.79 | -0.06 ± 0.41 | 0.496 | 1.30 ± 0.51 | 1.13 ± 0.50 | -0.17 ± 0.53 | 0.182 | 0.618 | 0.355 | 0.503 |
| Palatal CEJ-6 mm | 2.50 ± 1.16 | 2.61 ± 1.36 | 0.11 ± 0.87 | 0.596 | 2.64 ± 0.93 | 2.27 ± 0.89 | -0.37 ± 0.62 | 0.018* | 0.696 | 0.363 | 0.058 |
| Palatal CEJ-9 mm | 4.33 ± 1.58 | 5.34 ± 1.52 | 1.01 ± 0.72 | < 0.001* | 4.25 ± 1.30 | 3.04 ± 1.38 | -1.21 ± 0.90 | < 0.001* | 0.865 | < 0.001* | < 0.001* |
Note. Values are presented as mean ± standard deviation. *Statistically significant differences between groups (P < 0.05)
Change in skeletal and soft tissues
Table 4 presents the variations in various measurements from T0 to T1 for both the experimental and control groups. Significant changes in ANB were observed in both groups (P < 0.05). In the experimental group, the average change of ANB was 3.03° (from − 3.58° to -0.55°), whereas in the control group, it was 0.73° (from − 3.30° to -2.57°). The variation in APDI and Wits was statistically significant only in the experimental group, with an average change of -5.90° (from 92.26° to 86.36°) for APDI and 3.74 mm (from − 7.65 mm to -3.91 mm) for Wits. This indicates that the experimental group showed more significant improvement in inherent disharmony between the maxilla and mandible compared to the control group.
Table 4.
Changes of measurement items of the cephalometric measurements
| Experimental group(n = 19) | Control group(n = 19) | Comparison between groups | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measurements | T0 | T1 | T1-T0 | P value | T0 | T1 | T1-T0 | P value | P value | ||
| At T0 | At T1 | T1-T0 | |||||||||
| FH-MP | 27.51 ± 7.56 | 28.14 ± 6.88 | 0.64 ± 2.39 | 0.261 | 24.56 ± 5.00 | 25.54 ± 5.78 | 0.98 ± 2.24 | 0.071 | 0.165 | 0.215 | 0.647 |
| SNA | 77.38 ± 3.05 | 80.15 ± 3.25 | 2.77 ± 1.61 | < 0.001* | 77.73 ± 2.98 | 77.94 ± 3.22 | 0.21 ± 1.14 | 0.443 | 0.725 | 0.042* | 0.000* |
| ANB | -3.58 ± 2.27 | -0.55 ± 1.46 | 3.03 ± 1.62 | < 0.001* | -3.30 ± 1.66 | -2.57 ± 2.26 | 0.73 ± 1.25 | 0.022* | 0.656 | 0.003* | 0.000* |
| NA-APo | -8.23 ± 4.86 | -2.72 ± 3.39 | 5.51 ± 2.79 | < 0.001* | -7.19 ± 4.40 | -6.03 ± 4.94 | 1.16 ± 1.79 | 0.011* | 0.493 | 0.021* | 0.000* |
| APDI | 92.26 ± 6.48 | 86.36 ± 4.59 | -5.89 ± 5.99 | 0.000* | 92.32 ± 5.42 | 90.75 ± 5.18 | -1.57 ± 6.42 | 0.301 | 0.976 | 0.009* | 0.039* |
| Wits (mm) | -7.65 ± 2.57 | -3.91 ± 2.20 | 3.74 ± 1.92 | 0.000* | -6.39 ± 2.14 | -5.78 ± 1.98 | 0.61 ± 1.31 | 0.057 | 0.108 | 0.009* | 0.000* |
| U1-SN (°) | 113.98 ± 4.83 | 109.66 ± 5.02 | -4.33 ± 5.59 | 0.003* | 110.95 ± 10.72 | 117.77 ± 6.51 | 6.82 ± 9.34 | 0.005* | 0.272 | < 0.001* | 0.000* |
| U1-NA (mm) | 9.17 ± 3.29 | 6.17 ± 1.43 | -3.00 ± 2.80 | < 0.001* | 8.10 ± 3.67 | 10.43 ± 2.81 | 2.33 ± 3.39 | 0.008* | 0.351 | 0.000* | 0.000* |
| U1-NA (°) | 36.46 ± 5.90 | 29.71 ± 5.26 | -6.75 ± 5.69 | < 0.001* | 32.96 ± 10.44 | 39.82 ± 7.79 | 6.86 ± 9.00 | 0.004* | 0.214 | < 0.001* | 0.000* |
| U1-PP(°) | 124.72 ± 4.03 | 119.74 ± 4.31 | -4.97 ± 5.23 | 0.001* | 120.52 ± 9.49 | 127.32 ± 7.53 | 6.80 ± 7.89 | 0.001* | 0.089 | 0.001* | 0.000* |
| UL-EP (mm) | -3.40 ± 2.43 | -3.38 ± 1.59 | 0.02 ± 1.43 | 0.949 | -3.13 ± 2.36 | -2.42 ± 1.40 | 0.71 ± 1.49 | 0.052 | 0.727 | 0.055 | 0.154 |
| U1-A perp (mm) | 7.16 ± 2.25 | 5.01 ± 1.10 | -2.15 ± 2.68 | 0.003* | 6.30 ± 3.80 | 8.55 ± 2.15 | 2.25 ± 3.54 | 0.012* | 0.398 | 0.000* | 0.000* |
| G Vert-Sn (mm) | 4.09 ± 2.96 | 6.28 ± 2.79 | 2.19 ± 2.56 | 0.001* | 4.06 ± 3.49 | 4.18 ± 2.78 | 0.12 ± 2.95 | 0.866 | 0.980 | 0.025* | 0.026* |
| Nasolabial A (°) | 84.14 ± 12.29 | 93.61 ± 9.57 | 9.47 ± 12.67 | 0.004* | 85.21 ± 12.64 | 81.64 ± 12.73 | -3.57 ± 7.70 | 0.059 | 0.794 | 0.002* | 0.001* |
Note. Values are presented as mean ± standard deviation. *Statistically significant differences between groups (P < 0.05)
The change in the maxillary central incisor palatal plane angle demonstrated a statistically significant proclination of the maxillary incisors in the control group, with a mean proclination of 6.80° (from 120.52° before treatment to 127.32° after treatment). In contrast, U1-PP decreased significantly in the experimental group, with a mean change of -4.97° (from 124.72° before treatment to 119.74° after treatment).
Regarding soft tissue indicators, the G Vert-Sn and the nasolabial angle exhibited significant changes only in the experimental group, with all increasing after treatment (P < 0.05).
When comparing the measurement changes between the experimental group and the control group, all measurements showed significant differences except FH-MP and UL-EP.
Discussion
This study investigated the clinical changes in the position of maxillary central incisors and the surrounding alveolar bone in adult patients with skeletal Class III malocclusion after PAOO for the first time. For patients with skeletal Class III malocclusion, traditional camouflage orthodontic treatment is often implemented to address the anteroposterior discrepancy between the maxilla and mandible [17]. However, this treatment typically results in increased proclination of the maxillary incisors due to limitations in alveolar housing [18]. Consistent with previous studies, the control group in this study exhibited forward movement of the incisal tip of maxillary central incisors and backward movement of the root apex [19, 20]. Fortunately, the experimental group demonstrated a significant reduction in the axial inclination of the maxillary incisors and noticeable forward movement of the root apex. The biomechanics of PAOO, involving corticotomy and grafting of regenerative material, effectively reduced labial cortex resistance and widened the fragile-thin alveolar bone [11, 21]. This predictably allowed for the completion of historically considered unfavorable teeth movements of upper incisors. Research indicates that the decompensation of maxillary incisors’ inclination would improve smile attractiveness, especially in profile photographs [22]. Additionally, it was observed that in a few cases within the experimental group, there was no difference in the inclination of the maxillary incisors before and after treatment. These cases exhibited a normal inclination of the maxillary incisors but had an anterior crossbite prior to treatment. Therefore, PAOO in such cases may promote the bodily movement of the upper incisors forward while maintaining their normal inclination. Moreover, the U1-NA measurement in the experimental group at T1 (29.71 ± 5.26°) was closer to the normal value (22.00 ± 5.00°) compared to T0 (36.46 ± 5.90°), which is more appropriate for the anterior teeth.
To prevent periodontal side effects and root resorption, 3-dimensional positioning of the roots inside the bony envelope at the end of the treatment becomes an asset of orthodontic treatment [23]. In our study, PAOO has demonstrated the promotion of periodontal support tissue, specifically alveolar bone. Labial bone thickness at 3 mm, 6 mm, and 9 mm from CEJ of the central incisors significantly increased in the experimental group. Conversely, the control group did not exhibit any augmentation in bone mass; instead, labial bone thickness at 3 mm from CEJ and palatal alveolar bone thickness at 6 mm and 9 mm from CEJ significantly decreased. This outcome may be attributed to the labial tipping movement of maxillary incisors and the limited reconstruction of alveolar bone in the control group [24]. Consequently, PAOO in patients with skeletal Class III malocclusion appears to be an effective method for minimizing the risk of marginal bone resorption and fenestration by augmenting bone mass following the labial movement of the upper incisors outside the original cortical plane. It is crucial to note that our research focused solely on the two central incisors and their alveolar bone. Further validation of our findings requires data from a larger sample of anterior teeth.
Moreover, the substantial remodeling of alveolar bone signifies a breakthrough in the bone boundary for patients with skeletal Class III malocclusion [25]. Following orthodontic treatment, there was a significant increase in ANB in both cohorts. Notably, the Anteroposterior Pysplasia Indictor (APDI) [26], the most correlated indicator for assessing anteroposterior discrepancy, decreased exclusively in the experimental group. A pivotal discovery in our research is the significant forward movement of point A in the experimental group, attributed to prominent remodeling and augmentation of labial alveolar bone. Conversely, there was no apparent change in the SNA value after traditional camouflage orthodontic treatment, corroborating with previous studies [27]. However, one study did report a slight increase in the SNA angle after camouflage treatment [19].
Regarding soft tissue aesthetics, patients with skeletal Class III malocclusion typically exhibit a retrusive point-Sn and a smaller nasolabial angle due to the retrognathic maxilla and compensatory labial inclination of the upper anterior teeth [2]. Some studies suggest that maintaining the nasolabial angle within the normal range is the most aesthetically pleasing for the profile [28, 29]. In the experimental group, the increased fullness of the anterior maxillary alveolar base and improved inclination of the maxillary incisors after treatment resulted in the forward advancement of the onlay point-Sn of the soft tissue, leading to an increase in the nasolabial angle. These outcomes suggest that combining camouflage orthodontic treatment with maxillary PAOO for skeletal Class III patients could enhance bone augmentation in the subnasal region, thereby improving the overall profile and overcoming the limitations of traditional camouflage treatment on soft tissue aesthetics.
One limitation of this study may be attributed to the relatively short follow-up duration. Although postoperative CBCT images revealed a prominent continuous radiopaque line in the treated area, indicative of the formation of a cortical bone structure, the follow-up period in this study was insufficient, and the stability of the observed outcomes necessitates further investigation. Secondly, due to the limited number of eligible cases in the experimental group, the samples were not ample, potentially undermining the robustness of the conclusions drawn. Nonetheless, given the scarcity of research in this specific field, the content of this article may still serve as a valuable and uncommon reference for subsequent related studies. Thirdly, quantifying improvements in facial soft tissue aesthetics in the midface can be challenging using traditional methods. In our research, evaluation was solely based on lateral cephalometry. For future studies, a more comprehensive assessment could be conducted through alternative methods such as subjective aesthetic evaluation or 3D image evaluation [30–32].
Conclusion
PAOO holds promise as an approach to enhance topographical anatomy and address deficiencies in periodontal soft and hard tissues.
• PAOO can effectively increase labial bone thickness, thereby protecting periodontal tissue.
• In adult patients with skeletal Class III malocclusion, camouflage orthodontic treatment combined with PAOO significantly reduced the axial inclination of the maxillary incisors, with a noticeable forward movement of the root apex. This treatment also resulted in the forward movement of point A, thereby improving the inherent anteroposterior discrepancy between the maxilla and mandible.
• Aesthetically, the increased fullness of the anterior maxillary alveolar base led to the forward movement of the soft tissue point-Sn, resulting in an increased nasolabial angle and a significant improvement in the overall facial profile.
Acknowledgements
We wish to acknowledge the participation of all study participants. Department of orthodontics and periodontology, Hangzhou Stomatology Hospital; provided the study premises and technical equipment. We thank the Alliance of Dental Implant and Periodontology of Hangzhou Medical College for its support during the preparation of the study.
Abbreviations
- PAOO
Periodontally accelerated osteogenic orthodontics
- CBCT
Cone beam CT
- FOV
Field-of-view
- ABT
Alveolar bone thickness
- CEJ
Cementoenamel junction
- APDI
Anteroposterior pysplasia indictor
- TAD
Temporary anchorage device
Author contributions
All authors have made substantial contributions to conception and design of the study. J.J., WK.Y., JY.Y. have collected cases. J.J. and JJ.W. have collected important background information. DY.X., JY.F. and ZY.X. have been involved in data collection and data analysis. J.J., JJ.W., Q.X. and DX.L have been involved in data interpretation, drafting the manuscript and revising it critically. All authors have read and given final approval of the version to be published.
Funding
This study did not use any funds.
Data availability
The data that provide the basis for the present study is available by contact to the corresponding author. Restrictions apply to the availability of these data and to a certain time period, as the data were used under license for the current study, and so are not publicly available.
Declarations
Ethics approval and consent to participate
This study was approved by the human subjects ethics board of the Ethics Committee of Hangzhou Stomatology Hospital (2023LL08) and was conducted in accordance with the Helsinki Declaration of 1975, as revised in 2013. The informed consent was obtained from all the participants enrolled in the present study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jing Jiang and Jiajing Wu are joint first authors and contributed equally to this work.
Dongying Xuan and Jianying Feng contributed equally to this work.
References
- 1.Fernandez CCA, Pereira CVCA, Luiz RR, Vieira AR, De Castro Costa M. Dental anomalies in different growth and skeletal malocclusion patterns. Angle Orthod. 2018;88:195–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu W, Tan H, Meng X, Ming Y, Wang T, Zheng L. Three-dimensional analysis of lip soft tissue changes and related jaw changes in patients with skeletal class III malocclusion and facial asymmetry. XST. 2021;29:903–16. [DOI] [PubMed] [Google Scholar]
- 3.Reis GM, de Freitas DS, Oliveira RC, de Oliveira RCG, Pinzan-Vercelino CRM, Freitas KMS, et al. Smile attractiveness in class III patients after orthodontic camouflage or orthognathic surgery. Clin Oral Investig. 2021;25:6791–7. [DOI] [PubMed] [Google Scholar]
- 4.Coppola G, Christopoulou I, Gkantidis N, Verna C, Pandis N, Kanavakis G. The effect of orthodontic treatment on smile attractiveness: a systematic review. Prog Orthod. 2023;24:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alhammadi MS, Almashraqi AA, Khadhi AH, Arishi KA, Alamir AA, Beleges EM, et al. Orthodontic camouflage versus orthodontic-orthognathic surgical treatment in borderline class III malocclusion: a systematic review. Clin Oral Investig. 2022;26:6443–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park JH, Yu J, Bullen R. Camouflage treatment of skeletal class III malocclusion with conventional orthodontic therapy. Am J Orthod Dentofac Orthop. 2017;151:804–11. [DOI] [PubMed] [Google Scholar]
- 7.Lingxia LIU, Yuxin GUAN, Xiuping WU. Soft and hard tissue changes in adults with skeletal class III malocclusion before and after camouflage therapy. J Oral Sci Res. 2020;36(11):1074–8. 10.13701/j.cnki.kqyxyj.2020.11.020. [Google Scholar]
- 8.Jing W-D, Xu L, Li X-T, Xu X, Jiao J, Hou J-X, et al. Prevalence of and risk factors for alveolar fenestration and dehiscence in the anterior teeth of Chinese patients with skeletal class III malocclusion. Am J Orthod Dentofac Orthop. 2021;159:312–20. [DOI] [PubMed] [Google Scholar]
- 9.Wilcko WM, Wilcko T, Bouquot JE, Ferguson DJ. Rapid orthodontics with alveolar reshaping: two case reports of decrowding. Int J Periodontics Restor Dent. 2001;21:9–19. [PubMed] [Google Scholar]
- 10.Wang C, Yu S, Mandelaris GA, Wang H. Is periodontal phenotype modification therapy beneficial for patients receiving orthodontic treatment? An American Academy of Periodontology best evidence review. J Periodontol. 2020;91:299–310. [DOI] [PubMed] [Google Scholar]
- 11.Brugnami F, Caiazzo A, Mehra P. Can corticotomy (with or without bone grafting) expand the limits of safe orthodontic therapy? J Oral Biology Craniofac Res. 2018;8:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alsino HI, Hajeer MY, Burhan AS, Alkhouri I, Darwich K. The effectiveness of Periodontally Accelerated Osteogenic Orthodontics (PAOO) in accelerating tooth Movement and supporting alveolar bone thickness during Orthodontic Treatment: a systematic review. Cureus. 2022. 10.7759/cureus.24985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zimmo N, Sal MHA, Sinjab K, Wang C-W, Mandelaris G, Wang H-L. Corticotomy-assisted Orthodontics for Canine distalization: a systematic review and Meta-analysis of clinical controlled trials. J Int Acad Periodontol. 2018;20:153–62. [PubMed] [Google Scholar]
- 14.Jing W, Jiao J, Xu L, Hou J, Li X, Wang X, et al. Periodontal soft- and hard‐tissue changes after augmented corticotomy in Chinese adult patients with skeletal Angle Class III malocclusion: a non‐randomized controlled trial. J Periodontol. 2020;91:1419–28. [DOI] [PubMed] [Google Scholar]
- 15.Chen H, Liu L, Han M, Gu Y, Wang W, Sun L, et al. Changes of maxillary central incisor and alveolar bone in Class II Division 2 nonextraction treatment with a fixed appliance or clear aligner: a pilot cone-beam computed tomography study. Am J Orthod Dentofac Orthop. 2023;163:509–19. [DOI] [PubMed] [Google Scholar]
- 16.Sun L, Mu C, Chen L, Zhao B, Pan J, Liu Y. Dehiscence and fenestration of Class I individuals with normality patterns in the anterior region: a CBCT study. Clin Oral Invest. 2022;26:4137–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ngan P, Moon W. Evolution of Class III treatment in orthodontics. Am J Orthod Dentofac Orthop. 2015;148:22–36. [DOI] [PubMed] [Google Scholar]
- 18.Troy BA, Shanker S, Fields HW, Vig K, Johnston W. Comparison of incisor inclination in patients with Class III malocclusion treated with orthognathic surgery or orthodontic camouflage. American Journal of Orthodontics and Dentofacial Orthopedics. 2009;135:146.e1-146.e9. [DOI] [PubMed]
- 19.Martinez P, Bellot-Arcís C, Llamas JM, Cibrian R, Gandia JL, Paredes-Gallardo V. Orthodontic camouflage versus orthognathic surgery for class III deformity: comparative cephalometric analysis. Int J Oral Maxillofac Surg. 2017;46:490–5. [DOI] [PubMed] [Google Scholar]
- 20.Hisano M, Chung CJ, Soma K. Nonsurgical correction of skeletal class III malocclusion with lateral shift in an adult. Am J Orthod Dentofac Orthop. 2007;131:797–804. [DOI] [PubMed] [Google Scholar]
- 21.Amit G, Jps K, Pankaj B, Suchinder S, Parul B. Periodontally accelerated osteogenic orthodontics (PAOO) - a review. J Clin Exp Dent. 2012;4(5):e292–296. [DOI] [PMC free article] [PubMed]
- 22.Ghaleb N, Bouserhal J, Bassil-Nassif N. Aesthetic evaluation of profile incisor inclination. Eur J Orthod. 2011;33:228–35. [DOI] [PubMed] [Google Scholar]
- 23.Horiuchi A, Hotokezaka H, Kobayashi K. Correlation between cortical plate proximity and apical root resorption. Am J Orthod Dentofac Orthop. 1998;114:311–8. [DOI] [PubMed] [Google Scholar]
- 24.Ahn H-W, Seo D-H, Kim S-H, Park Y-G, Chung K-R, Nelson G. Morphologic evaluation of dentoalveolar structures of mandibular anterior teeth during augmented corticotomy-assisted decompensation. Am J Orthod Dentofac Orthop. 2016;150:659–69. [DOI] [PubMed] [Google Scholar]
- 25.Sun L, Yuan L, Wang B, Zhang L, Shen G, Fang B. Changes of alveolar bone dehiscence and fenestration after augmented corticotomy-assisted orthodontic treatment: a CBCT evaluation. Prog Orthod. 2019;20:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fatima F, Fida M, Shaikh A. Reliability of overbite depth indicator (ODI) and anteroposterior dysplasia indicator (APDI) in the assessment of different vertical and sagittal dental malocclusions: a receiver operating characteristic (ROC) analysis. Dent Press J Orthod. 2016;21:75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Burns NR, Musich DR, Martin C, Razmus T, Gunel E, Ngan P. Class III camouflage treatment: What are the limits? American Journal of Orthodontics and Dentofacial Orthopedics. 2010;137:9.e1-9.e13. [DOI] [PubMed]
- 28.Lo FD, Hunter WS. Changes in nasolabial angle related to maxillary incisor retraction. Am J Orthod. 1982;82:384–91. [DOI] [PubMed] [Google Scholar]
- 29.Nandini S, Prashanth C, Somiah SK, Reddy S. An Evaluation of Nasolabial Angle and the relative inclinations of the nose and Upper Lip. J Contemp Dent Pract. 2011;12:152–7. [DOI] [PubMed] [Google Scholar]
- 30.He D, Gu Y, Sun Y. Correlations between objective measurements and subjective evaluations of facial profile after orthodontic treatment. J Int Med Res. 2020;48:300060520936854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang M, Lyu L, Li J, Yan H, Zhu Y, Yu T, et al. Subjective evaluation of facial asymmetry with three-dimensional simulated images among the orthodontists and laypersons: a cross-sectional study. BMC Oral Health. 2023;23:500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chaves LB, Barbosa TL, Casagrande CPM, Alencar DS, Capelli J, de Carvalho F. Evaluation of two stereophotogrametry software for 3D reconstruction of virtual facial models. Dent Press J Orthod. 2022;27:e2220230. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that provide the basis for the present study is available by contact to the corresponding author. Restrictions apply to the availability of these data and to a certain time period, as the data were used under license for the current study, and so are not publicly available.