Abstract
Background
Health institutions advocate for psychosocial and recovery-oriented interventions alongside pharmacological treatment for severe mental illness. Participatory arts interventions appear promising in promoting personal recovery by fostering connectedness, hope, renegotiation of identity, meaning-making, and empowerment. Despite encouraging findings, however, the evidence base remains thin. Further, results from cognitive literature studies suggest possible impact on parameters of clinical recovery, but this has not been studied in clinical contexts. We developed REWRITALIZE, a structured, recovery-oriented, fifteen-session creative writing group intervention led by a professional author alongside a mental health professional. Participants engage with literary forms, write on them, share their texts, and partake in reflective discussions within a supportive, non-stigmatising environment, designed to promote self-expression, playful experimentation, agency, recognition, participatory meaning-making, renegotiation of identity and social engagement.
The aim of this project is to evaluate REWRITALIZE for persons with severe mental illness through a randomised controlled trial (RCT) focusing on personal recovery outcomes. Additionally, an embedded pilot RCT will explore additional outcomes i.e., clinical recovery for a subgroup with schizophrenia spectrum disorders.
Methods
The RCT is an investigator-initiated, randomised, two-arm, assessor-blinded, multi-center, waiting-list superiority trial involving 300 participants (age > 18) from six psychiatric centers in regions Capital and Zealand in Denmark, randomised to receive either the creative writing intervention combined with standard treatment or standard treatment alone. Assessments will be conducted before and after the intervention and at six months post intervention. The primary outcome is personal recovery at the end of intervention measured with the questionnaire of the process of recovery. Secondary outcomes include other measures of personal recovery, self-efficacy, mentalising, and quality of life. The pilot RCT, integrated within the RCT, will focus on 70 of the participants aged 18–35 with schizophrenia spectrum disorders, evaluating exploratory measures related to perspective-taking, social cognition, cognitive function, psychosocial functioning, and symptom pressure.
Discussion
This is the first RCT for creative writing groups. It assesses whether REWRITALIZE, as adjunct to standard mental healthcare, is more effective for personal recovery than standard care. If successful, it would provide evidence for the efficacy of REWRITALIZE, potentially enabling its implementation across mental health centers in Denmark.
Trial registration
Privacy (data protection agency): p-2023–14655.
Danish National Center for Ethics: 2313949.
Clinicaltrials.gov: NCT06251908. Registration date 02.02.2024.
Keywords: Participatory arts, Creative writing, Recovery, Psychosocial interventions, Severe mental illness, Schizophrenia spectrum disorders.
Background
Guidelines for aiding individuals with mental disorders stress the need to supplement pharmacological treatment with psychosocial interventions and recovery-oriented approaches [71–73, 106]. The implementation of recovery-oriented practices in mental healthcare is, however, still in an early phase.
Recovery comprises two main categories – clinical recovery and personal recovery. Clinical recovery refers to a reduction of symptoms of mental disorders and a restoration of functioning, including cognitive, social, and occupational functioning. Personal recovery refers to the process of constructing a personally meaningful life within and beyond the limits of one’s mental disorder [2, 5, 26, 103]. Five key aspects of personal recovery have been identified and summarised in the CHIME framework: development and maintenance of supportive relationships that facilitate the experience of belonging (Connectedness), motivation and belief in one’s ability to achieve change (Hope), building a positive self-conception and overcoming stigma (Identity), living a meaningful life with fulfilling activities (Meaning), and developing autonomy and taking responsibility and control over one’s life (Empowerment) [54]. People with severe mental illness understand recovery as a transformation from a negative self-conception marked by helplessness to a more positive self-conception of wellbeing and emphasise the importance of both clinical recovery and the CHIME processes of personal recovery for this transformation [27].
Recovery-oriented interventions that consider social difficulties for persons with severe mental illness are still not systematically implemented in mainstream psychiatry [25, 56, 85]. A recent review could only identify few recovery-oriented services [5]. Amongst them were art-based interventions [72]. Studies of different kinds of art therapy have shown mixed results (e.g. [22, 64]). Our focus is on participatory arts and how it can be used in mental healthcare. In participatory arts, the artistic activity is facilitated by artists in a group setting, the goal of the activity is understood as engaging in the artistic process, and the participants share and engage in reflective discussion about the produced art works ([96, 14, 77, 105]). A review of qualitative studies on recovery outcomes for participatory arts activities suggests that participatory arts might be beneficial for the CHIME processes [105]. A review of qualitative, quantitative, and mixed methods studies on art-based practices, including participatory arts, support positive effects on the CHIME processes Identity and Connectedness [110]. The evidence-base from quantitative studies on participatory arts is, however, thin: No randomised controlled trial has been conducted [36, 76]. Furthermore, regarding domains relating to clinical recovery, e.g. social and cognitive functioning, research is also lacking. Social and cognitive difficulties are especially challenging and pertinent for persons suffering from schizophrenia spectrum disorders, and interventions targeting these issues are recommended for this population, but available interventions and evidence for their effectiveness are scarce [4, 20, 31, 34, 62, 72]. Cognitive literature studies, investigating the impact of engaging with literature on cognition, suggest that reading literature may further social cognitive capacities [32, 33, 49, 50] and that writing literature is associated with higher levels of mentalising capacities [61, 68]. This has, however, neither been researched within a clinical population nor a controlled setting. Hence the evidence from empirical cognitive literature studies may be promising.
When it comes to creative writing interventions in healthcare contexts, writing in groups has been suggested to contribute to recovery [37, 51, 92]. A review on quantitative and qualitative findings regarding creative writing groups and recovery, indicated beneficial effects on the CHIME factors connectedness, empowerment, and identity [70]. The one study that considered participatory arts, i.e., creative writing groups led by a professional author, reported changes in wellbeing from pre to post intervention [113]. A metareview conducted by the British NHS, including studies on both somatic and mental disorders, suggested that writing that is not facilitated by a trained leader might not promote health, but that facilitated writing requires more exploration [76]. In line with this, further supporting the participatory arts format, others have underlined the importance of using professional authors as facilitators [51]. In conclusion, randomised controlled studies are needed to assess if there are beneficial effects of creative writing groups on recovery [18, 45, 70].
The current intervention, REWRITALIZE, is a creative writing group intervention that is conducted by a professional author and focuses on the text as aesthetic form (see Intervention). Participants are instructed to respect the narrative distance, i.e., the distance between the narrated self and the self who narrates [38] and discuss the text rather than the person who wrote it. The protective distance between text and personal experiences is meant to establish a safe space in which participants can engage with artistic work on their own terms and express themselves spontaneously in both writing and reflective discussions about others’ art works. This is expected to allow participants to put into words difficult feelings or experiences, to practice mentalisation in reflective sessions, i.e., to reflect on their own and others’ mental states, relate to a plurality of perspectives and integrate others’ perspective into their own outlook [28, 46, 110], and to promote their self-efficacy [8, 9, 112]. Together this may reduce self-stigmatisation and illness identity, stimulate participatory meaning-making, enhance connectedness between the participants and inspire renegotiation of identity into a more positive self-conception, thus contributing to personal recovery [30, 43, 55, 57–59, 65, 67, 81, 91, 94, 98, 110, 113, 118, 119, 117]. Following studies in non-clinical populations pointing to reading and writing literature having possible impacts on social cognitive factors, it will be valuable to explore if the characteristics of the REWRITALIZE creative writing group intervention may also contribute to clinical recovery, i.e. cognitive and psychosocial functioning and symptom reduction.
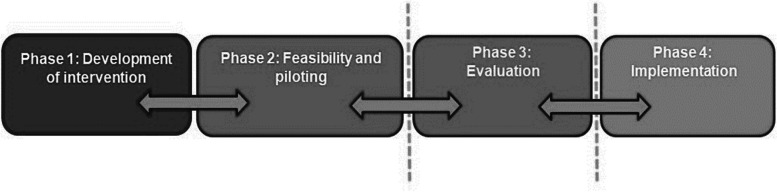
The present study is part of a larger research program that has developed recovery-oriented, manualised, participatory arts groups, including REWRITALIZE with creative writing as artistic format [16]. The four phased design of this research program (Fig. 1) is based on recommendations from an international group of leading artist, arts researchers, and healthcare researchers, promoting complex interventions in healthcare treatment [36, 101, 102].
Fig. 1.
The design of the research program
Phases 1 and 2 have been carried out. This protocol is a description of the research to be carried out in phase 3. The overarching aim of the present study is to evaluate the newly developed recovery-oriented, manualised, participatory writing group-format REWRITALIZE for persons with severe mental illness. The evaluation of effectiveness will be carried out as a randomised clinical controlled trial (RCT).
Objectives
Objective 1 of this study is to determine if REWRITALIZE as supplement to standard mental healthcare is more effective than standard mental healthcare alone for promoting personal recovery, as measured by the Questionnaire for the process of recovery (QPR) immediately after the end of the intervention, in a sample of individuals with severe mental illness.
Objective 2 is to investigate if REWRITALIZE as supplement to standard mental healthcare is more effective than standard mental healthcare alone in promoting mentalising, self-efficacy, functioning and quality of life, as measured at the end of the intervention, and in promoting personal recovery six months after the end of the intervention.
Objective 3 is to explore REWRITALIZE as supplement to standard mental healthcare for advancing clinical recovery variables, specifically cognition and social cognition, and pilot-test if REWRITALIZE leads to symptom reduction and improve psychosocial function in a smaller sample of participants with schizophrenia spectrum disorders.
Methods
The study is designed as an RCT with an embedded pilot RCT. Objective 1 and 2 will be investigated in the RCT, while objective 3 will be investigated in the pilot RCT. Below follows detailed description of the RCT and the pilot RCT.
RCT design
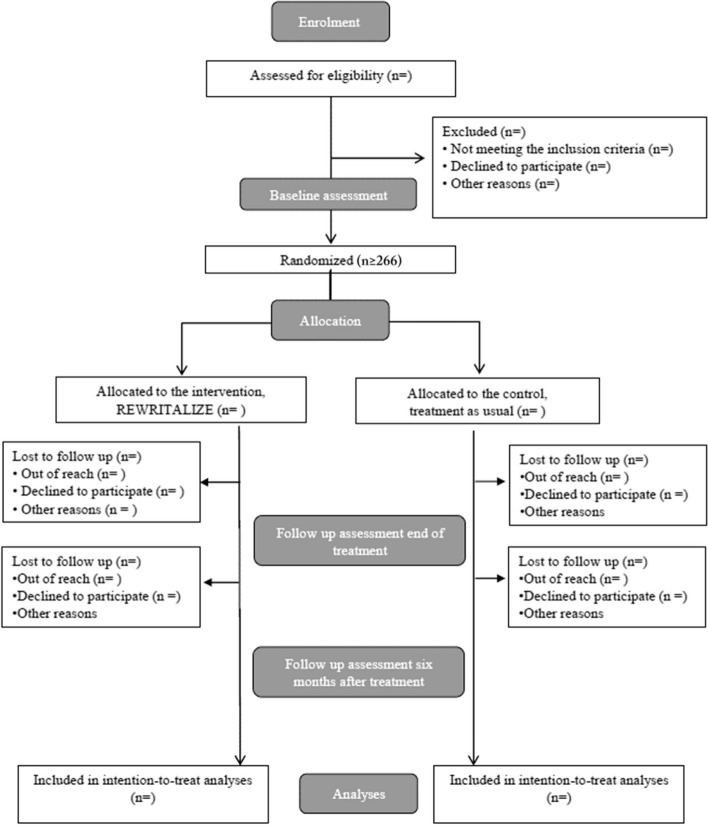
The RCT is designed as an investigator-initiated, randomised, two-arm, assessor-blinded, multi-center, waiting list-controlled superiority trial. The allocation ratio to active and control condition is 1:1. The participants (n = 300) will be randomised to active condition (REWRITALIZE plus standard treatment) or waiting list control condition (standard treatment) (see Randomisation below). As it is a waiting list control group, the persons randomised to the control group will be invited to participate in a creative writing group after the last assessment (within one year). To ensure high methodological quality, the trial is designed and will be reported according to the SPIRIT 2013 Statement and the modified CONSORT 2017 criteria for non-pharmacological trials [15, 17]. Data will be collected at baseline, at the end of the intervention (approximately 4.5 months after baseline) and six months after the end of the intervention (approximately 10.5 months after baseline). A flow chart of the study is provided in Fig. 2.
Fig. 2.
Trial flowchart
Pilot RCT design
The pilot RCT investigates whether the REWRITALIZE intervention may further social cognition, cognition, psychosocial functioning, and symptom reduction in a subsample of participants with schizophrenia spectrum disorders (n = 70). Given the novelty of this area, key uncertainties must be clarified [35] concerning feasibility of the chosen measures, data collection, and analysis. The pilot RCT thus investigates whether the measures on cognition and social cognition are feasible in this setting. The pilot RCT also measures key domain outcomes, i.e. mean, variation, between group differences at end of intervention and within group differences pre and post intervention. The pilot RCT will, furthermore, ascertain whether data will be normally distributed in this population using these measures, and whether ceiling effects may emerge. As the pilot RCT is embedded within the RCT it will follow the overall procedures regarding recruitment, randomisation, and data collection. Data will be collected at baseline and post-intervention follow-up.
Participants
Participants in the RCT will be included in the study if they are over 18 and diagnosed with a severe mental illness, i.e., schizophrenia, schizotypal, delusional, and other non-mood psychotic disorders, bipolar disorder, severe depression, posttraumatic stress disorder, or borderline personality disorder (F2, F31, F32.2, F32.3, F33.2, F33.3, F43.1, F60.3). Forensic psychiatric patients will be excluded. In all, 30–34 groups, 15–17 active groups and 15–17 control groups, will be carried out with 8–10 participants in each group. Although power calculations (see below: Sample size and power calculations) set the minimum sample size to 266 and the RCT intention-to-treat principle reduces the threat of drop-out for power, we will aim to include 300 participants. Considering the relatively high drop-out rate in similar interventions [64, 110], the enhanced inclusion enables us to aim for a higher number of real, as opposed to imputed, follow-up data, and to minimise the risk to end up with low power if participants were to retract their informed consent.
Participants in the pilot RCT will be included in the study if they are between 18 and 35 and fulfil the criteria for a schizophrenia spectrum disorder (F20, F21) according to the Present State Examination [87, 115].
Participants will be recruited from outpatient clinics’ OPUS programs (early intervention program for first episode psychosis) and F-ACT (Flexible Assertive Community Treatment) at Mental Health Centres in Regions Capital and Zealand in Denmark [40, 75, 109].
Intervention
REWRITALIZE is conceptualised as a hybrid between an art group and a group therapy intervention [16]. It is developed by an interdisciplinary group of professional authors, user experts, and researchers, and it is manualised (Bundesen B, Llambías P, Rosenbaum B: Manual for REWRITALIZE, forthcoming).
REWRITALIZE consists of 15 three-hour sessions, 14 weekly with an additional session after a one-month break to reduce the risk of adverse effects at the end of the intervention. During the sessions, the 8–10 participants are presented with literary forms that function as prompts for writing exercises. Participants write spontaneously on the presented form for 5–15 min. After each text is read out loud, the participants engage in a reflective discussion about the text. The primary conductor, a professional writer with teaching experience, secures high artistic standards. S/he is supplemented by a co-conductor with clinical expertise who participates in the group activities together with the other participants and ensures psychological safety. Together they constitute the conductor-tandem. The exercises are presented during the course of sessions to participants in an order securing adherence to group therapeutic principles.
The design of the intervention aims at providing a safe, non-judgmental, non-stigmatising space in which illness is not in focus, a space that demotes performance anxiety and promotes playfulness, spontaneous expression, openness to otherness and a plurality of perspectives. This is achieved by several characteristics. First, the leader of the course is a professional author, and the participants are presented to each other as readers and writers rather than by their diagnoses. This is meant to reduce participants' negative self-conception and self-stigmatisation and allow for other non-illness-dominated facets of their identity to be developed [21, 51, 105, 111, 117, 119]. Second, the co-conductor as co-participant allows participants to feel safe in the sense that they know that they themselves, and other participants, can get support if needed. Third, the course is given in a non-clinical community setting with a warm and welcoming, structured atmosphere, where the roles and rules of the activity are clear. Fourth, it is made explicit that the course is not about performing and already possessing writing skills, but about discussing literature and learning about writing forms. Fifth, it is explicitly stated that the narrative distance, i.e., the distance between the narrated self and the self who narrates, should be respected [38]. The reflective discussion thus concerns the text, and not the person who wrote it. This means that the group format differs from the kind of therapy that explicitly addresses personal experience [76, 83, 90]. The protective distance allows participants to share experiences and feelings without disclosing if they are personal. This is meant to reduce anxiety and the extent to which other participants’ reflections are experienced as invading, thus promoting playfulness and spontaneity in the engagement with the writing tasks and reflective sessions. The playful attitude is meant to allow for participants to put words on difficult feelings and experiences that may reveal new facets of themselves. During reflective sessions, the creative attitude is expected to allow participants to practice mentalising, i.e., the motivation and ability to reflect on one’s own and others’ mental states, taking a plurality of perspectives into account, and integrating others’ perspectives in one’s own outlook. This may enhance the experience of self-efficacy, enhance connectedness between the participants, reduce self-stigmatisation and stimulate self-esteem and renegotiation of identity [24, 55, 57, 94, 107, 110].
Treatment as usual
Participants are recruited from OPUS (i.e., outreach treatment of young persons with psychosis symptoms) and F-ACT (Flexible Assertive Community Treatment). OPUS is a nationally implemented 2-year-long early intervention for people with first-episode psychosis. F-ACT is a community-based treatment model that provides flexible, multidisciplinary support to individuals with severe mental illness. OPUS and F-ACT both involve enriched and flexible assertive community treatment, psychoeducation including medication and side effects, relapse prevention and family involvement [40, 75, 109]. In OPUS, a multidisciplinary team consisting of a psychiatrist, a psychologist, a psychiatric nurse, an occupational therapist, and a social worker are assigned to each patient with a 1:12 caseload. In F-ACT, a multidisciplinary team consisting of a psychiatrist, a psychiatric nurse, and a social worker are assigned to each patient. For both OPUS and F-ACT, a primary staff member is in regular contact with the patient and responsible for coordinating the treatment elements. The treatment is individual and contingent upon patients’ needs [40, 75, 109].
Adherence to the intervention
Adherence is enhanced by focusing on the conductor-tandem collaboration and the co-conductor’s communication with the participants. This has been improved continuously during the pilot study. Attendance at each session will be recorded by the co-conductor.
Outcomes and assessments
Baseline characteristics
Baseline characteristics of the participants are collected through self-report and register data; see Table 1. The baseline characteristics are collected to ensure that the active and control groups do not differ on any potentially biasing characteristics. For the pilot RCT the PSE will be administered for diagnostic validation.
Table 1.
Participant characteristics
| Variable | Source of collection |
|---|---|
| Age | Self-report |
| Sex | Self-report |
| Employment status | Self-report |
| Highest education | Self-report |
| Diagnoses | Register |
| Time since diagnosis | Register |
| Earlier use of mental health services | Register |
| Prior admissions (#) | Register |
| Antipsychotics | Register |
| Suicide attempt | Register |
| Admitted for alcohol and drug abuse | Register |
| Present state examination (pilot RCT) | Clinician rated |
Outcome measures
In Table 2 the primary and secondary outcome measures are listed. The primary outcome measure is the Questionnaire about the process of recovery (QPR) which measures personal recovery as understood within the CHIME framework [74, 99, 114] measured at the end of the intervention, i.e. approximately 4.5 months after baseline. Secondary outcome measures include QPR six months after the end of the intervention (10.5 months after baseline), as well as other measures of personal recovery, mentalising, self-efficacy, functioning and quality of life measured at 4.5 months.
Table 2.
Primary and secondary measures
| Outcome | Measure | Pre | Post (4.5 months) | Post (10.5 months) | Source of collection | |
|---|---|---|---|---|---|---|
| Primary | ||||||
| Overall personal recovery | QPR | x | x | SR | ||
| Secondary | ||||||
| Personal recovery | ||||||
| Overall personal recovery | QPR | x | x | SR | ||
| Connectedness | TBS | x | x | SR | ||
| Self-efficacy | SEPRS | x | x | SR | ||
| Functioning | WSAS | x | x | SR | ||
| Quality of life | MANSA | x | x | SR | ||
| Mentalising | ||||||
| Overall mentalising | MentS | x | x | SR | ||
| Alexithymia | TAS | x | x | SR |
SR self-report questionnaire; QPR Questionnaire for the process of recovery; TBS Thwarted belongingness scale; WSAS Work and Social Adjustment Scale; SEPRS Self-efficacy for personal recovery scale; MANSA Manchester Short Assessment of Quality of life; MentS Mentalization scale; TAS Toronto Alexithymia Scale
The explorative outcome measures are shown in Table 3. These include the secondary measures at the 10.5 months follow-up in the full sample. The outcome measures for the active group at 4.5 months and 10.5 months, respectively, will be compared to the outcome measures for the control group at 4.5 months and 10.5 months, respectively (see Data analysis).
Table 3.
Exploratory measures
| Outcome | Measure | Sample | Pre | Post (4.5 months) | Post (10.5 months) | Source of collection |
|---|---|---|---|---|---|---|
| Exploratory | ||||||
| Connectedness | TBS | full | x | x | SR | |
| Self-efficacy | SEPRS | full | x | x | SR | |
| Functioning | WSAS | full | x | x | SR | |
| Quality of life | MANSA | full | x | x | SR | |
| Overall mentalising | MentS | full | x | x | SR | |
| Alexithymia | TAS | full | x | x | SR | |
| Cognition | SCIP-D | subsample | x | x | T | |
| Social cueing | TASIT 2A | subsample | x | x | T | |
| Balancing of other-perspective | VISPT | subsample | x | x | T | |
| Positive and negative symptoms | PANSS-6 | subsample | x | x | CR | |
| Functioning | GAF-F | subsample | x | x | CR | |
SR self-report questionnaire; T task; CR clincian-rated; TBS Thwarted belongingness scale; WSAS Work and Social Adjustment Scale; SEPRS Self-efficacy for personal recovery scale; MANSA Manchester Short Assessment of Quality of life; MentS Mentalization scale; TAS Toronto Alexithymia Scale; SCIP-D Screen for cognitive impairment in psychiatry; TASIT 2A The awareness of social inference test; VISPT Visual perspective-taking task; PANSS-6 Positive and Negative Syndrome Scale; GAF-F Global Assessment of Functioning Scale
The additional explorative outcome measures of the pilot RCT are also shown in Table 3. These include measures of cognitive impairment, social cognition, balancing of other-perspective, psychosocial function, and symptom severity. The outcome measures will be compared between active and control group at 4.5 months, and between baseline and at 4.5 months to explore feasibility of the measures.
Safety measures
Safety measures are displayed in Table 4.
Table 4.
Safety measures
| Outcome | Measure | Pre | Post (4.5 months) | Post (10.5 months) | Source of collection |
|---|---|---|---|---|---|
| Safety measures | Admissions | x | x | register | |
| Deaths | x | x | register | ||
| Suicide | x | x | register |
Assessment tools
Personal recovery
Questionnaire for the process of recovery (QPR): Personal recovery is measured using the Questionnaire for the process of recovery (QPR), a validated 15-item measure of personal recovery as conceptualised within the CHIME framework and developed in Britain as a collaboration between clinicians and mental health service users [53, 54, 74, 99, 114]. Each item is answered using a 5-point Likert scale with anchors “strongly disagree” and “strongly agree”, resulting in a range of 0–60. A mean difference of 4 has been considered relevant [53].
Thwarted belongingness scale (TBS): The recovery dimension of connectedness is measured using Thwarted belongingness scale (TBS), a validated 8-item measure of the subjective feeling of isolation and connectedness [39, 60]. Each item is answered on a 7-point Likert scale with anchors “not at all true for me” and “true for me”, resulting in a range of 8–56. A mean difference of 14 has been considered relevant [60].
Self-efficacy
Self-efficacy for personal recovery scale (SEPRS): Self-efficacy is measured with the Self-efficacy for personal recovery scale (SEPRS) [112], which comprises 14 items on the form “How confident are you that you can…”. Each item is answered on a scale from 1–100, resulting in a range of 14–1400.
Functioning
The Work and Social Adjustment Scale (WSAS): Impairment in social functioning is measured by the validated Work and Social Adjustment Scale (WSAS) [69]. WSAS is a self-report 5-item scale that assesses functioning on a scale from zero to eight. The sum score ranges between 0 and 40. A mean difference of 9 has been considered relevant [69].
Quality of life
The Manchester Short Assessment of Quality of life (MANSA): Quality of life is measured using the Manchester Short Assessment of Quality of life (MANSA). MANSA is a validated 16-item self-report questionnaire, developed primarily for persons with schizophrenia spectrum disorders and comprising items on whether the person i) has a friend ii) has a friend that s/he has seen in the last week, iii) has been accused of a crime, and iv) has been the victim of violence, as well as 12 items on satisfaction with occupation, activities, relationships, health, and living and financial situation [12, 84, 88]. The 12 items are answered on a 7-point Likert scale with anchors “couldn’t be worse” and “couldn’t be better”, resulting in a sum score in the range 12–84. A mean difference of 4 points has been considered relevant [11].
Mentalising
Mentalization scale (MentS): Mentalising is measured with the Mentalization scale, which is a validated 28-item scale consisting of three subscales Self-Related Mentalisation, Other-Related Mentalisation, and Motivation to Mentalise [3, 29]. It is scored on a 5-point Likert scale, resulting in a score range of 28–140. A mean difference of 8 has been considered relevant [29].
Toronto Alexithymia Scale (TAS): Alexithymia is measured using Toronto Alexithymia Scale (TAS), a validated 20-item scale with three subscales: difficulty describing feelings, difficulty identifying feelings, and externally oriented thinking, i.e., low motivation and habit to reflect on feelings [6, 7, 47, 66, 108]. Each item is answered on a 5-point Likert scale with anchors “not at all true for me” and “to a high degree true for me”, resulting in a range of 20–100. A mean difference of 7 has been considered relevant [66].
Additional assessment tools for the pilot RCT
The Screen for cognitive impairment in psychiatry (SCIP): The Screen for cognitive impairment in psychiatry (SCIP-D, Danish version) is used to measure cognitive performance [89]. The SCIP-D is a validated screening tool for detecting cognitive impairment in persons with psychotic and affective disorders [10, 80, 93]. A low score signifies more impairment. A mean difference of 3.6 has been considered relevant [97].
Positive and Negative Syndrome Scale (PANSS-6): The severity of positive and negative symptoms is measured by the Positive and Negative Syndrome Scale (PANSS-6), which is a 6-item clinician-rated scale measuring delusions, conceptual disorganisation, hallucination, blunted affect, social withdrawal, and lack of spontaneity in conversation. Each item is rated from 1–7, giving a possible score between 6 and 42 [48, 78, 79].
Global Assessment of Functioning Scale – function (GAF-F): Social function is measured using the Global Assessment of Functioning Scale – function [82, 86]. GAF-F is an interview-based, clinician-rated estimate of social function including occupational function, for which 4 points on a 100-point scale has been proposed a minimum clinically relevant effect [1, 23].
The Awareness of Social Inference Test (TASIT): Social cueing is measured with The Awareness of Social Inference Test (TASIT) [13], subsection 2A [44, 63]. The TASIT assesses social cueing using videos of naturalistic everyday conversations in which two actors interact. Participants are asked questions about the communicative intentions of the people in the clips. The total accuracy score takes values in the range of 0–60. A mean difference in accuracy of 4 has been considered relevant [13].
Visual perspective-taking task (VISPT): Balancing of the other-perspective is measured with the Visual perspective-taking task (VISPT) [95]. A computer-based task measuring ability or tendency to ignore another person’s perspective in one’s visual perception, and ability or tendency to take another person’s perspective into account in one’s visual perception judgments. Participants view an avatar in a room, with a number of discs on the walls: in one condition (consistent) the avatar sees the same number as the participant, in the other (inconsistent) the number differs. Correct scores range from 0–36 with correctness on consistent compared to inconsistent trial computed as a ratio [52, 100].
Assignment of interventions
After baseline data are obtained, the participants are randomly allocated to either the control (standard mental healthcare) or active group (REWRITALIZE + standard mental healthcare) with a 1:1 allocation using the randomisation module in REDCap (Research Electronic Data Capture) [41, 42]. The randomisation sequence will be generated by an external researcher at Copenhagen Research Centre for Mental Health (CORE) and uploaded to REDCap. The randomisation is stratified by sites. Varying block sizes, unknown to the research team, are used. To ensure concealment, the randomisation schedule is stored away from the research team and the block sizes are not disclosed. Participants randomised to the control group will be set on a waiting list and will be informed that they will be offered to participate in a creative writing group within one year of the randomisation.
Blinding
Owing to the nature of the intervention, neither participants, nor staff can be blinded to allocation. Participants will be instructed not to disclose the allocation status to the researchers. Baseline data will be collected prior to randomisation and those who collect follow-up data will be blinded. An employee outside the research team will extract data from REDCap on study completion, and group allocation will be coded with A and B to ensure blinding of the researchers during analysis and interpretation of data, drawing conclusions, and writing reports.
Data collection and analysis
Data collection
Data will be collected at baseline and at follow-ups at 4.5 and at 10.5 months after baseline (see Table 5). After informed consent forms have been signed, participants can choose to fill out the questionnaires while the research assistant stays with them on Teams, or they can choose to do it after the meeting. Data collection for these active groups and their controls will commence approximately a month prior to group start and stop at the second follow-up at 10.5 months after group start. For each participant that drops out, the reason for drop-out will be registered. All participants who have not withdrawn their consent will be contacted for follow-ups, including those who decided to stop the intervention before it ended. For the pilot RCT data will be collected at baseline and follow-up at 4.5 months after baseline.
Table 5.
Schedule of enrolment, interventions, and assessments
| Study period | ||||||
|---|---|---|---|---|---|---|
| Enrolment | Allocation | Postallocation | Closeout | |||
| Time point | t-1 | t0 | t1 | t2 | t3 | t4 |
| Enrolment | ||||||
| Eligibility screen | x | |||||
| Informed consent | x | |||||
| Allocation | x | |||||
| Interventions | ||||||
| REWRITALIZE | x | |||||
| TAU | x | |||||
| Assessments | ||||||
| Baseline characteristics | ||||||
| Age | x | |||||
| Sex | x | |||||
| Employment status | x | |||||
| Highest education | x | |||||
| Diagnoses | x | |||||
| Time since diagnosis | x | |||||
| Earlier use of mental health services | x | |||||
| Prior admissions (#) | x | |||||
| Antipsychotics | x | |||||
| Suicide attempt | x | |||||
| Alcohol and drug abuse | x | |||||
| Outcome measures | ||||||
| Personal recovery QPR | x | x | x | |||
| Connectedness TBS | x | x | x | |||
| Self-efficacy SEPRS | x | x | x | |||
| Functioning WSAS | x | x | x | |||
| Quality of life MANSA | x | x | x | |||
| Overall mentalising MentS | x | x | x | |||
| Alexithymia TAS | x | x | x | |||
| Outcome measures (subset, exploratory) | ||||||
| Cognition SCIP-D | x | x | ||||
| Social cueing, TASIT 2A | x | x | ||||
| Balancing other-perspective VISPT | x | x | ||||
| Positive and negative symptoms PANSS-6 | x | x | ||||
| Functioning GAF-F | x | x | ||||
| Safety measures | ||||||
| Admissions | x | x | ||||
| Deaths | x | |||||
| Suicide attempt | x | x | ||||
QPR Questionnaire for the process of recovery; TBS Thwarted belongingness scale; SEPRS Self-efficacy for personal recovery scale; WSAS Work and Social Adjustment Scale; MANSA Manchester Short Assessment of Quality of life; MentS Mentalization scale; TAS Toronto Alexithymia Scale; SCIP-D Screen for cognitive impairment in psychiatry; TASIT 2A The awareness of social inference test; VISPT Visual perspective-taking task; PANSS-6 Positive and Negative Syndrome Scale; GAF-F Global Assessment of Functioning Scale
Table 5 shows the participant timeline and an overview of the data collection in agreement with the standard protocol items for randomised clinical trials, recommendations for intervention trials (SPIRIT) [17]. Data are collected and stored using REDCap, an electronic data capture tool hosted at the Capital Region of Denmark. REDCap is a secure, web-based software platform designed to support data capture for research studies [41, 42].
Sample size and power calculations
The minimum sample size is calculated based on the ability to detect a minimal but clinically significant difference between the active intervention group and the control group in the primary personal recovery QPR measure. The minimal clinically significant difference between the study groups has been estimated to 4 points [53]. Based on trials in similar populations, we assume a standard deviation of 10 in the study population, which corresponds to an effect size of Cohen’s d = 0.4 [104, 114]. To achieve a statistical power of 90% at a significance level of 5%, a total of 266 participants must be included in this study to detect a difference: 133 in each group. Based on the needed participants, power calculations for secondary outcomes were calculated and are presented in Table 6. Because of the relatively high drop-out rate in the pilot study and similar studies [64, 110], we will plan for a sample size of 150 participants in the active group and 150 participants in the control group. This should hence allow for at least a 90% power of finding a minimally clinically significant difference in the primary measure, i.e., the QPR measure of personal recovery.
Table 6.
Power
| Outcome | Measure | Alpha | Mean diff | SD | Cohen’s d | Power | n | Mean diff source | SD source | |
|---|---|---|---|---|---|---|---|---|---|---|
| Primary | 0,05 | |||||||||
| Personal recovery | QPR | 4 | 10 | 0,40 | 0,9 | 266 | [53] | [114] | ||
| Secondary | ||||||||||
| Connectedness | TBS | 0,05 | 14 | 14 | 1 | 1 | 266 | [60] | [60] | |
| Self-efficacy | SEPRS | 0,05 | xa | x | 0,40 | 0,9 | 266 | |||
| Functioning | WSAS | 0,05 | 5 | 7 | 0,71 | 1 | 266 | [69] | [69] | |
| Quality of life | MANSA | 0,05 | 4 | 11 | 0,36 | 0,83 | 266 | [11] | [11] | |
| Overall mentalising | MentS | 0,05 | 8 | 12 | 0,66 | 1 | 266 | [29] | [29] | |
| Alexithymia | TAS | 0,05 | 7 | 11 | 0,63 | 1 | 266 | [66] | [47] | |
See Table 5 and the assessment tool section for outcome measure abbreviations
aPower estimates for measures for which no relevant mean difference was identified are based on a moderate to small effect size of Cohen’s d=0.4
For the pilot RCT no calculation of sample size has been made as the primary aim for a pilot RCT is to explore design uncertainties before proceeding to a future RCT [35], here feasibility of chosen measures.
Data analyses
The main outcome measure is personal recovery measured by QPR. To test the research hypothesis, the differences at follow-up between the active intervention group and the control group will be analysed using independent-samples t-test. Effect sizes to judge clinical relevance will be estimated by Cohen’s d [19]. All variables are continuous. Secondary and exploratory measures will be tested by the same means. The significance level is set to 0.05 for all measures. If there, despite randomisation, are differences in any baseline measure between active and control groups, these differences will be adjusted for in the comparison between active and control groups using general linear models.
Data analyses will be based on the intention-to-treat principle. Data from all participants will thus be included in the analyses. In accordance with the principle, missing data from the follow-up will be imputed using multiple imputations by means of Markov Chain Monte Carlo methods in Stata. All co-variates of supposed prognostic significance will be used to impute a distribution of missing data. A prerequisite for multiple imputation is that data are missing at random. This will be examined by various means, e.g. by comparing prognostic baseline characteristics between the participants for whom follow-up data are missing and the participants for whom follow-up data have been collected.
As a supplementary analysis, the differences at follow-up between the active and control groups will be analysed including only observed data, i.e. data for whom follow-up data have been collected. A detailed statistical analysis plan will be prepared and uploaded to clinicaltrials.gov before initiating analyses.
For the pilot study mean, standard deviation, within and between group differences on the outcome measures will be calculated.
Monitoring
Data monitoring
Unexpected harms are collected during the study period through e-mail, telephone or face-to-face communication between participants and co-conductors. Unanticipated adverse events including drastic worsening of symptoms, aggressive behaviour or suicide in the writing group will be communicated by the co-conductor both to the clinicians at the psychiatric centre, and to the project group. The project group will discuss if measures need to be taken. Unexpected adverse events will be reported in trial publications.
Fidelity
A fidelity scale has been developed to ensure that the different centres and conductor-tandems (author + co-conductor pairs) comply with the REWRITALIZE design. The crucial features of the design that will be assessed include: i) The conductor-tandem is trained and supervised, and the author functions as leader and the co-conductor as one of the participants. ii) Participant are presented to each other as readers and writers rather than as persons with a diagnosis, and the sessions provide welcoming, calm, and structured spaces with snacks, coffee and providing of pens and paper. iii) It is emphasised that the discussion is about the text and not about the person, that playfulness, improvisation, and sharing and recognition is encouraged, and it is made clear that a multitude of perspectives is welcomed. iv) Participants are aware that the discussion is about the text and not about its author and that they do not have to reveal if a text is based on autobiographical material or not. Participants understand that it is about playfully trying out writing forms and discussing those and not about performing. v) Participants experience the space as safe and without focus on illness, and the co-conductor as someone they can talk to and trust. Participants experience the activity as meaningful. The program fidelity will be monitored by site approximately every six months.
Discussion: perspectivation and limitations
The aim of this RCT is to assess if REWRITALIZE as add-on to standard mental healthcare is more effective than standard mental healthcare alone for promoting personal recovery. This is the first RCT for creative writing groups and participatory arts. The study design closely follows the SPIRIT guidelines. With the planned sample size, it has at least 90% power of finding a medium to small effect size for the primary measure of personal recovery. If we can show that there is a difference between the active group and the control group, this would indicate that participation in REWRITALIZE increases participants’ chance of recovery. As this would constitute evidence for the efficacy of REWRITALIZE, it would allow the intervention to be offered by mental health centres across Denmark on evidence-based grounds. Since this is a multicentre study, this aspect of the study design may facilitate the implementation at mental health centres.
The kind of control group – the waiting list control – was chosen because this is the first RCT conducted for this intervention. To enable testing of the beneficial effect of the artistic activity per se, the control group should take part in another non-artistic social activity preferably involving non-artistic writing.
One first limitation of the current RCT is that the use of mental health services is not recorded. It may thus be that the use of mental health services differs between the active and control groups. Second, participants were not asked to refrain from participation in other participatory arts groups. It is hence possible that those allocated to the control group took part in other participatory arts groups outside of mental health centres. Third, since the candidate participants did not see a clinician prior to enrolment, no exclusion criteria could be implemented. Some patients may be excluded by the co-conductor after enrolment because they are judged to display antisocial behaviour or use alcohol and drugs in a way that hinders participation in the intervention. Lastly, the nature of the intervention was such that participants could not themselves be blinded to which group they were in.
Furthermore, the embedded pilot study is the first to address if the chosen measures are feasible for assessing potential effects of creative writing on social cognition and cognition in a clinical and controlled setting. Analyses of the pilot RCT will provide important knowledge regarding the available measures and inform the design of a full-scale trial investigating the possible effectiveness of a creative writing group intervention on cognitive, social cognitive and psychosocial functioning, and symptom reduction.
Acknowledgements
The authors would like to thank the funding bodies and the participants in the study.
Abbreviations
- CHIME
Connectedness, Hope, Identity, Meaning, Empowerment
- CORE
Copenhagen Research Centre for Mental Health
- F-ACT
Flexible Assertive Community Treatment
- GAF-F
Global Assessment of Functioning Scale-Function
- MANSA
Manchester Short Assessment of Quality of Life
- MentS
Mentalization Scale
- NHS
National Health Service
- PANSS
Positive and Negative Syndrome Scale
- PSE
Present State Examination
- QPR
Questionnaire for the Process of Personal Recovery
- REDcap
Research Electronic Data Capture
- RCT
Randomised Controlled Trial
- SCIP
Screen for Cognitive Impairment in Psychiatry
- SEPRS
Self-Efficacy for Personal Recovery Scale
- SPIRIT
Standard Protocol Items: Recommendations for Interventional Trials
- TAS
Toronto Alexithymia Scale
- TASIT
The Awareness of Social Inference Test
- TBS
Thwarted Belongingness Scale
- VISPT
Visual Perspective-Taking task
- WSAS
Work and Social Adjustment Scale
Authors’ contributions
Susanne Henningsson: Conceptualisation (supporting); methodology (supporting); writing – original draft (lead), review and editing (equal); formal analysis (lead). Jon Toke Brestisson: Conceptualisation (supporting); methodology (supporting); investigation (equal); writing – original draft (supporting); writing – review and editing (lead). Siv-Therese Bogevik Bjørkedal: Conceptualisation (supporting); methodology (supporting); writing – original draft (supporting); writing – review and editing (equal). Birgit Bundesen: Conceptualisation (lead); methodology (equal); funding (lead); investigation (equal); supervision (supporting); writing – review and editing (supporting). Keld Stehr Nielsen: Data curation (lead); project administration (equal). Bea Ebersbach: Data curation (equal); conceptualisation on fidelity (lead); project administration (equal). Carsten Hjorthøj: Formal analysis (supporting). Lene Falgaard Eplov: Conceptualisation (supporting); methodology (lead); supervision (lead). All authors have reviewed, revised, and approved the final manuscript.
Funding
Open access funding provided by Copenhagen University The study is funded by the philanthropic foundation Det Obelske Familiefond, and the funding granted after a peer-reviewed application process. The funders and the sponsor, Mental health services of Capital Region Denmark, have no role in study design, data collection, analysis, interpretation, or writing.
Availability of data and materials
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Information about the study is presented to all potential participants both verbally and in written form. At the information meeting and in the informed consent form it is made clear that the intervention is voluntary and safe, and that participants can stop their participation in the project at any time and withdraw their consent without consequences for the treatment they receive. If the participants wish to withdraw from the experiment during the intervention, there are three options: 1) They withdraw from the intervention but not from the study, therefore they will participate in the data collection at the follow-ups. 2) They withdraw from both the intervention and the study, but data from the baseline measures can be used in the research project. 3) They withdraw from both the intervention and the study, and their data will be deleted.
The study will be conducted in agreement with the Declaration of Helsinki [116]. The Regional Ethical Committee for the Capital Region has decided that the study is not required to seek approval under their legislation (2313949), which covers human participation in medical trials. We will adhere to all other ethical standards guiding good practice in research. The study has been registered with the Danish Data Protection Agency (p-2023–14655), and we will comply with data security and GDPR regulations. The study has been registered at clinicaltrials.gov (NCT06251908), registration date 02.02.2024. If any modifications are made to the data collection or data analyses, these protocol amendments will be reported to the Danish Data Protection Agency and to clinicaltrials.gov. The intervention is not expected to have any serious side-effects. This is supported by the pilot study and similar studies [64].
Consent for publication
N/a.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Amri I, Millier A, Toumi M. Minimum Clinically Important Difference in the Global Assessment Functioning in Patients with Schizophrenia. Value in Health. 2014;17(7):A765–6. 10.1016/j.jval.2014.08.285. [DOI] [PubMed] [Google Scholar]
- 2.Anthony WA. Recovery from mental illness: The guiding vision of the mental health service system in the 1990s. Psychosocial Rehabilitation Journal. 1993;16(4):11–23. 10.1037/H0095655. [Google Scholar]
- 3.Asgarizadeh A, Vahidi E, Seyed Mousavi PS, Bagherzanjani A, Ghanbari S. Mentalization Scale (MentS): Validity and reliability of the Iranian version in a sample of nonclinical adults. Brain and Behavior. 2023;13(8):1–9. 10.1002/brb3.3114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Austin SF. Promoting well-being in psychosis. Nord J Psychiatry. 2018;72(6):437–41. [DOI] [PubMed] [Google Scholar]
- 5.Badu E, O’brien AP, Mitchell R. An integrative review of recovery services to improve the lives of adults living with severe mental illness. Int J Environ Res Public Health. 2021;18(16). 10.3390/ijerph18168873. [DOI] [PMC free article] [PubMed]
- 6.Bagby RM, Parker JDA, Taylor GJ. Twenty-five years with the 20-item Toronto Alexithymia Scale. J Psychosomatic Res. 2020;131. 10.1016/J.JPSYCHORES.2020.109940. [DOI] [PubMed]
- 7.Bagby RM, Taylor GJ, Parker JDA. The twenty-item Toronto Alexithymia scale-II. Convergent, discriminant, and concurrent validity. J Psychosomatic Res. 1994;38(1):33–40. 10.1016/0022-3999(94)90006-X. [DOI] [PubMed]
- 8.Bandura A. Human Agency in Social Cognitive Theory. Am Psychol. 1989:1175–84. https://www.uky.edu/~eushe2/Bandura/Bandura1989AP.pdf. [DOI] [PubMed]
- 9.Bandura A. On the Functional Properties of Perceived Self-Efficacy Revisited. 2012;9–44. 10.1177/0149206311410606.
- 10.Belvederi Murri M, Folesani F, Costa S, Biancosino B, Colla C, Zerbinati L, Caruso R, Nanni MG, Purdon SE, Grassi L. Screening for cognitive impairment in non-affective psychoses: A comparison between the SCIP and the MoCA. Schizophr Res. 2020;218:188–94. 10.1016/J.SCHRES.2020.01.005. [DOI] [PubMed] [Google Scholar]
- 11.Bjørkedal STB, Bejerholm U, Hjorthøj C, Møller T, Eplov LF. Meaningful Activities and Recovery (MA&R): a co-led peer occupational therapy intervention for people with psychiatric disabilities. Results from a randomized controlled trial. BMC Psychiatr. 2023;23(1):1–15. 10.1186/s12888-023-04875-w. [DOI] [PMC free article] [PubMed]
- 12.Björkman, T., & Svensson, B. Quality of life in people with severe mental illness. Reliability and validity of the Manchester Short Assessment of Quality of Life (MANSA). Nordic J Psychiatr. 2005;59(4), 302–306. 10.1080/08039480500213733 [DOI] [PubMed]
- 13.Bliksted V, Fagerlund B, Weed E, Frith C, Videbech P. Social cognition and neurocognitive deficits in first-episode schizophrenia. Schizophr Res. 2014;153(1–3):9–17. 10.1016/j.schres.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 14.Bone TA. Art and Mental Health Recovery: Evaluating the Impact of a Community-Based Participatory Arts Program Through Artist Voices. Community Ment Health J. 2018;54(8):1180–8. 10.1007/s10597-018-0332-y. [DOI] [PubMed] [Google Scholar]
- 15.Boutron I, Altman DG, Moher D, Schulz KF, Ravaud P. CONSORT Statement for randomized Trials of nonpharmacologic treatments: A 2017 update and a CONSORT extension for nonpharmacologic Trial Abstracts. Ann Intern Med. 2017;167(1):40–7. 10.7326/M17-0046. [DOI] [PubMed] [Google Scholar]
- 16.Bundesen B, Aymo-Boot M, Djørup A, Fritzsche L, Gejl T, Levin K, Llambías P, Printzlau GA, Serup MG, Rosenbaum B. REWRITALIZE: Participatory creative writing groups led by authors in collaboration with mental health care professionals for people experiencing severe mental illness. Nordic J Arts Cult Wellbeing. 2020;2(2):140–47. 10.18261/ISSN.2535-7913-2020-02-05.
- 17.Chan A, Tetzlaff JM, Altman DG. 2013 Statement : Defining Standard Protocol Items for Clinical Trials. Ann Intern Med. 2016;158(3):200–7. 10.7326/0003-4819-158-3-201302050-00583.Requests. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chiang M, Reid-Varley WB, Fan X. Creative art therapy for mental illness. Psychiatry Res. 2019;275:129–36. 10.1016/J.PSYCHRES.2019.03.025. [DOI] [PubMed] [Google Scholar]
- 19.Cohen J. Statistical Power Analysis for the Behavioral Sciences Second Edition (2nd ed.). Lawrence Erlbaum Associates. 1988.
- 20.Correll, C. U., Galling, B., Pawar, A., Krivko, A., Bonetto, C., Ruggeri, M., Craig, T. J., Nordentoft, M., Srihari, V. H., Guloksuz, S., Hui, C. L. M., Chen, E. Y. H., Valencia, M., Juarez, F., Robinson, D. G., Schooler, N. R., Brunette, M. F., Mueser, K. T., Rosenheck, R. A., … Kane, J. M. Comparison of Early Intervention Services vs Treatment as Usual for Early-Phase Psychosis: A Systematic Review, Meta-analysis, and Meta-regression. JAMA Psychiatr. 2018;75(6), 555–565. [DOI] [PMC free article] [PubMed]
- 21.Corrigan PW, Larson JE, Rüsch N. Self-stigma and the “why try” effect: impact on life goals and evidence-based practices. World Psychiatry. 2009;8(2):75. 10.1002/J.2051-5545.2009.TB00218.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Crawford MJ, Killaspy H, Barnes TRE, Barrett B, Byford S, Clayton K, Dinsmore J, Floyd S, Hoadley A, Johnson T, Kalaitzaki E, King M, Leurent B, Maratos A, O’Neill FA, Osborn DP, Patterson S, Soteriou T, Tyrer P, Waller D. Group art therapy as an adjunctive treatment for people with schizophrenia: Multicentre pragmatic randomised trial. BMJ (Online). 2012;344(7847):1–9. 10.1136/bmj.e846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dalum HS, Waldemar AK, Korsbek L, Hjorthoj C, Mikkelsen JH, Thomsen K, Kistrup K, Olander M, Lindschou J, Nordentoft M, Eplov LF. Illness management and recovery: Clinical outcomes of a randomized clinical trial in community mental health centers. PLoS ONE. 2018;13(4):1–15. 10.1371/journal.pone.0194027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davidson L. Recovering a sense of self in schizophrenia. J Pers. 2020;88(1):122–32. 10.1111/jopy.12471. [DOI] [PubMed] [Google Scholar]
- 25.Davidson L, Drake RE, Schmutte T, Dinzeo T, Andres-Hyman R. Oil and water or oil and vinegar? Evidence-based medicine meets recovery. Community Ment Health J. 2009;45(5):323–32. 10.1007/S10597-009-9228-1. [DOI] [PubMed] [Google Scholar]
- 26.Davidson L, Lawless MS, Leary F. Concepts of recovery: Competing or complementary? Curr Opin Psychiatry. 2005;18(6):664–7. 10.1097/01.yco.0000184418.29082.0e. [DOI] [PubMed] [Google Scholar]
- 27.Dell, N. A., Long, C., & Mancini, M. A. Models of mental health recovery: An overview of systematic reviews and qualitative meta-syntheses. In Psychiatri Rehabil J. 2021;44(3):238–253. Educ Publishing Foundation. 10.1037/prj0000444 [DOI] [PubMed]
- 28.Dimaggio, G., & Lysaker, P. H. (2010). Metacognition and severe adult mental disorders : from research to treatment. Routledge. https://www.routledge.com/Metacognition-and-Severe-Adult-Mental-Disorders-From-Research-to-Treatment/Dimaggio-Lysaker/p/book/9781138884472
- 29.Dimitrijević A, Hanak N, Altaras Dimitrijević A, Jolić Marjanović Z. The Mentalization Scale (MentS): A Self-Report Measure for the Assessment of Mentalizing Capacity. J Pers Assess. 2018;100(3):268–80. 10.1080/00223891.2017.1310730. [DOI] [PubMed] [Google Scholar]
- 30.Dimopoulou T, Tarazi FI, Tsapakis EM. Clinical and therapeutic role of mentalization in schizophrenia-a review. CNS Spectr. 2017;22(6):450–62. 10.1017/S1092852916000687. [DOI] [PubMed] [Google Scholar]
- 31.Dixon LB, Dickerson F, Bellack AS, Bennett M, Dickinson D, Goldberg RW, Lehman A, Tenhula WN, Calmes C, Pasillas RM, Peer J, Kreyenbuhl J. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophr Bull. 2010;36(1):48–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Djikic M, Oatley K. The Art in Fiction: From Indirect Communication to Changes of the Self. Psychol Aesthet Creat Arts. 2014;8(4):498–505. [Google Scholar]
- 33.Dodell-Feder D, Tamir DI. Fiction Reading Has a Small Positive Impact on Social Cognition: A Meta-Analysis. J Exp Psychol. 2018;147(11):1713–27. [DOI] [PubMed] [Google Scholar]
- 34.Eglit GML, Palmer BW, Martin AS, Tu X, Jeste DV. Loneliness in schizophrenia: Construct clarification, measurement, and clinical relevance. PLoS ONE. 2018;13(3). [DOI] [PMC free article] [PubMed]
- 35.Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, Lancaster GA, PAFS consensus group,. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ (Clinical research ed). 2016;355: i5239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fancourt D, Finn S. Factsheet: What is the evidence on the role of the arts in improving health and well-being? A scoping review - WHO Regional Office for Europe. World Health Organization; 2019. https://www.euro.who.int/en/health-topics/health-determinants/behavioural-and-cultural-insights-for-health/publications/2019/fact-sheet-what-is-the-evidence-on-the-role-of-the-arts-in-improving-health-and-well-being-in-the-who-european-region2019%0Ahttps. [PubMed]
- 37.Farmasi L, Kiss A, Szendi I. The Narrative Facilitation of Recovery. The Application of Narrative Theories in a Group Therapy for Patients with Schizophrenia. DIEGESIS. 2018;7(1). https://www.diegesis.uni-wuppertal.de/index.php/diegesis/article/view/297.
- 38.Gallagher S, Cole J. Dissociation in self-narrative. Conscious Cogn. 2011;20(1):149–55. 10.1016/j.concog.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 39.Hallensleben N, Glaesmer H, Forkmann T, Rath D, Strauss M, Kersting A, Spangenberg L. How Is the Presence of Company Related to Thwarted Belongingness in Real Time? Taking a Closer Look at the Conceptualization of the Construct of the Interpersonal Theory of Suicide. Int J Environ Res Public Health. 2020;17(13):1–14. 10.3390/IJERPH17134873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hansen HG, Starzer M, Nilsson SF, Hjorthøj C, Albert N, Nordentoft M. Clinical Recovery and Long-Term Association of Specialized Early Intervention Services vs Treatment as Usual Among Individuals With First-Episode Schizophrenia Spectrum Disorder: 20-Year Follow-up of the OPUS Trial. JAMA Psych. 2023;80(4):371–9. 10.1001/jamapsychiatry.2022.5164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95. 10.1016/J.JBI.2019.103208. [DOI] [PMC free article] [PubMed]
- 42.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hasson-Ohayon I, Gumley A, McLeod H, Lysaker PH. Metacognition and Intersubjectivity: Reconsidering Their Relationship Following Advances From the Study of Persons With Psychosis. Front Psychol. 2020;11. 10.3389/FPSYG.2020.00567. [DOI] [PMC free article] [PubMed]
- 44.Honan CA, McDonald S, Sufani C, Hine DW, Kumfor F. The awareness of social inference test: Development of a shortened version for use in adults with acquired brain injury. Clinical Neuropsychologist. 2016;30(2):243–64. 10.1080/13854046.2015.1136691. [DOI] [PubMed] [Google Scholar]
- 45.Hu J, Zhang J, Hu L, Yu H, Xu J, King JL. Art Therapy: A Complementary Treatment for Mental Disorders. Front Psychol. 2021;12(August):1–9. 10.3389/fpsyg.2021.686005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Inchausti F, García-Poveda NV, Prado-Abril J, Ortuño-Sierra J, Gaínza-Tejedor I. Metacognition-oriented social skills training (Mosst): Theoretical framework, working methodology and treatment description for patients with schizophrenia. Papeles Del Psicologo. 2017;38(3):204–15. 10.23923/pap.psicol2017.2840.
- 47.Jørgensen MM, Zachariae R, Skytthe A, Kyvik K. Genetic and environmental factors in alexithymia: A population-based study of 8,785 Danish twin pairs. Psychother Psychosom. 2007;76(6):369–75. 10.1159/000107565. [DOI] [PubMed] [Google Scholar]
- 48.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–76. 10.1093/SCHBUL/13.2.261. [DOI] [PubMed] [Google Scholar]
- 49.Kidd DC, Castano E. Reading literary fiction improves theory of mind. Science. 2013;342(6156):377–80. [DOI] [PubMed] [Google Scholar]
- 50.Kidd DC, Castano E. Reading literary fiction can improve theory of mind. Nat Hum Behav. 2018;2(9):604–604. [DOI] [PubMed] [Google Scholar]
- 51.King R, Neilsen P, White E. Creative writing in recovery from severe mental illness. Int J Ment Health Nurs. 2013;22(5):444–52. 10.1111/j.1447-0349.2012.00891.x. [DOI] [PubMed] [Google Scholar]
- 52.Kronbichler L, Stelzig-Schöler R, Pearce BG, Tschernegg M, Said-Yürekli S, Crone JS, Uscatescu LC, Reich LA, Weber S, Aichhorn W, Perner J, Kronbichler M. Reduced spontaneous perspective taking in schizophrenia. Psychiatry Research - Neuroimaging. 2019;292(March):5–12. 10.1016/j.pscychresns.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 53.Law H, Neil ST, Dunn G, Morrison AP. Psychometric properties of the Questionnaire about the Process of Recovery (QPR). Schizophr Res. 2014;156(2–3):184–9. 10.1016/j.schres.2014.04.011. [DOI] [PubMed] [Google Scholar]
- 54.Leamy M, Bird V, Le Boutillier C, Williams J, Slade M. Conceptual framework for personal recovery in mental health: Systematic review and narrative synthesis. Br J Psychiatry. 2011;199(6):445–52. 10.1192/bjp.bp.110.083733. [DOI] [PubMed] [Google Scholar]
- 55.Lloyd C, Wong SR, Petchkovsky L. Art and Recovery in Mental Health: A Qualitative Investigation. 2007;70(5):207–14. 10.1177/030802260707000505.
- 56.Lorien L, Blunden S, Madsen W. Implementation of recovery-oriented practice in hospital-based mental health services: A systematic review. Int J Ment Health Nurs. 2020;29(6):1035–48. 10.1111/INM.12794. [DOI] [PubMed] [Google Scholar]
- 57.Lynch S, Holttum S, Huet V. The experience of art therapy for individuals following a first diagnosis of a psychotic disorder : a grounded theory study psychotic disorder : a grounded theory study. Int J Art Therapy. 2019;24(1):1–114832. 10.1080/17454832.2018.1475498. [Google Scholar]
- 58.Lysaker PH, Hamm JA, Hasson-Ohayon I, Pattison ML, Leonhardt BL. Promoting recovery from severe mental illness: Implications from research on metacognition and metacognitive reflection and insight therapy. World Journal of Psychiatry. 2018;8(1):1–11. 10.5498/WJP.V8.I1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lysaker PH, Keane JE, Culleton SP, Lundin NB. Schizophrenia, recovery and the self: An introduction to the special issue on metacognition. Schizophr Res. 2019;19. 10.1016/J.SCOG.2019.100167. [DOI] [PMC free article] [PubMed]
- 60.Ma J, Batterham PJ, Calear AL, Sunderland M. The Development and Validation of the Thwarted Belongingness Scale (TBS) for Interpersonal Suicide Risk. J Psychopathol Behav Assess. 2019;41(3):456–69. 10.1007/s10862-019-09721-6. [Google Scholar]
- 61.Mar RA, Oatley K, Hirsh J, dela Paz, J., & Peterson, J. B. Bookworms versus nerds: Exposure to fiction versus nonfiction, divergent associations with social ability, and the simulation of fictional social worlds. J Res Pers. 2006;40(5):694–712. [Google Scholar]
- 62.McDonagh MS, Dana T, Kopelovich SL, Monroe-DeVita M, Blazina I, Bougatsos C, Grusing S, Selph SS. Psychosocial Interventions for Adults With Schizophrenia: An Overview and Update of Systematic Reviews. Psychiatr Serv (Washington, D.C.). 2022;73(3):299–312. [DOI] [PubMed]
- 63.McDonald S, Bornhofen C, Shum D, Long E, Saunders C, Neulinger K. Reliability and validity of The Awareness of Social Inference Test (TASIT): A clinical test of social perception. Disabil Rehabil. 2006;28(24):1529–42. 10.1080/09638280600646185. [DOI] [PubMed] [Google Scholar]
- 64.Montag C, Haase L, Seidel D, Bayerl M, Gallinat J, Herrmann U, Dannecker K. A pilot RCT of psychodynamic group art therapy for patients in acute psychotic episodes: Feasibility, impact on symptoms and Mentalising capacity. PLoS ONE. 2014;9(11). 10.1371/journal.pone.0112348. [DOI] [PMC free article] [PubMed]
- 65.Montemagni C, Del Favero E, Riccardi C, Canta L, Toye M, Zanalda E, Rocca P. Effects of Cognitive Remediation on Cognition, Metacognition, and Social Cognition in Patients With Schizophrenia. Front Psychiatr. 2021;12. 10.3389/FPSYT.2021.649737. [DOI] [PMC free article] [PubMed]
- 66.Moriguchi Y, Maeda M, Igarashi T, Ishikawa T, Shoji M, Kubo C, Komaki G. Age and gender effect on alexithymia in large, Japanese community and clinical samples: A cross-validation study of the Toronto Alexithymia Scale (TAS-20). BioPsychoSoc Med. 2007;1. 10.1186/1751-0759-1-7. [DOI] [PMC free article] [PubMed]
- 67.Moritz S, Mahlke CI, Westermann S, Ruppelt F, Lysaker PH, Bock T, Andreou C. Embracing Psychosis: A Cognitive Insight Intervention Improves Personal Narratives and Meaning-Making in Patients With Schizophrenia. Schizophr Bull. 2018;44(2):307–16. 10.1093/SCHBUL/SBX072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mumper ML, Gerrig RJ. Leisure reading and social cognition: A meta-analysis. Psychol Aesthet Creat Arts. 2017;11(1):109–20. [Google Scholar]
- 69.Mundt JC, Marks IM, Shear MK, Greist JH. The Work and Social Adjustment Scale: A simple measure of impairment in functioning. Br J Psychiatry. 2002;180(MAY):461–4. 10.1192/bjp.180.5.461. [DOI] [PubMed] [Google Scholar]
- 70.Mundy SS, Kudahl B, Bundesen B, Hellström L, Rosenbaum B, Eplov LF. Mental health recovery and creative writing groups: A systematic review. Nordic J Arts Cult Health. 2022;4(1):1–18. 10.18261/njach.4.1.1.
- 71.National Institute for Health and Care Excellence (NICE). Bipolar disorder: assessment and management. Aust Fam Physician. 2007;36(4):240–3. [PubMed] [Google Scholar]
- 72.National Institute for Health and Care Excellence (NICE). Psychosis and schizophrenia in adults: prevention and management. Nice. 2014;4. [PubMed]
- 73.National Institute for Health and Care Excellence (NICE). Depression in adults: screening, treatment and management. Pharm J. 2023. 10.1211/pj.2023.1.175372.
- 74.Neil ST, Kilbride M, Pitt L, Nothard S, Welford M, Sellwood W, Morrison AP. The questionnaire about the process of recovery (QPR): A measurement tool developed in collaboration with service users. Psychosis. 2009;1(2):145–55. 10.1080/17522430902913450. [Google Scholar]
- 75.Nielsen CM, Hjorthøj C, Killaspy H, Nordentoft M. The effect of flexible assertive community treatment in Denmark: a quasi-experimental controlled study. The Lancet Psychiatry. 2021;8(1):27–35. 10.1016/S2215-0366(20)30424-7. [DOI] [PubMed] [Google Scholar]
- 76.Nyssen OP, Taylor SJC, Wong G, Steed E, Bourke L, Lord J, Ross CA, Hayman S, Field V, Higgins A, Greenhalgh T, Meads C. Does therapeutic writing help people with long-term conditions? Systematic review, realist synthesis and economic considerations. Health Technol Assess. 2016;20(27):1–367. 10.3310/hta20270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.O’Donnell S, Lohan M, Oliffe JL, Grant D, Galway K. The acceptability, effectiveness and gender responsiveness of participatory arts interventions in promoting mental health and Wellbeing: a systematic review. Arts Health. 2022;14(2). 10.1080/17533015.2021.1894463. [DOI] [PubMed]
- 78.Ostergaard SD, Lemming OM, Mors O, Correll CU, Bech P. PANSS-6: A brief rating scale for the measurement of severity in schizophrenia. Acta Psychiatr Scand. 2016;133(6):436–44. 10.1111/acps.12526. [DOI] [PubMed] [Google Scholar]
- 79.Ostergaard SD, Foldager L, Mors O, Bech P, Correll CU. The validity and sensitivity of PANSS-6 in the clinical antipsychotic trials of intervention effectiveness (CATIE) study. Schizophr Bull. 2018;44(2):453–62. 10.1093/schbul/sbx076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ott CV, Bjertrup AJ, Jensen JH, Ullum H, Sjalland R, Purdon SE, Vieta E, Kessing LV, Miskowiak KW. Screening for cognitive dysfunction in unipolar depression: Validation and evaluation of objective and subjective tools. J Affect Disord. 2016;190:607–15. 10.1016/J.JAD.2015.10.059. [DOI] [PubMed] [Google Scholar]
- 81.Patterson S, Crawford MJ, Ainsworth E, Waller D. Art therapy for people diagnosed with schizophrenia: Therapists’ views about what changes, how and for whom. International Journal of Art Therapy: Inscape. 2011;16(2):70–80. 10.1080/17454832.2011.604038. [Google Scholar]
- 82.Pedersen G, Hagtvet KA, Karterud S. Generalizability studies of the Global Assessment of Functioning-Split version. Compr Psychiatry. 2007;48(1):88–94. 10.1016/J.COMPPSYCH.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 83.Pennebaker JW. Expressive Writing in Psychological Science. Perspectives on Psychological Science : A Journal of the Association for Psychological Science. 2018;13(2):226–9. 10.1177/1745691617707315. [DOI] [PubMed] [Google Scholar]
- 84.Petkari E, Giacco D, Priebe S. Factorial structure of the Manchester Short Assessment of Quality of Life in patients with schizophrenia-spectrum disorders. Qual Life Res. 2020;29(3):833–41. 10.1007/s11136-019-02356-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Piat M, Wainwright M, Sofouli E, Vachon B, Deslauriers T, Préfontaine C, Frati F. Factors influencing the implementation of mental health recovery into services: a systematic mixed studies review. Syst Rev. 2021;10(1). 10.1186/S13643-021-01646-0. [DOI] [PMC free article] [PubMed]
- 86.Piersma HL, Boes JL. The GAF and psychiatric outcome: a descriptive report. Community Ment Health J. 1997;33(1):35–41. 10.1023/A:1022413110345. [DOI] [PubMed] [Google Scholar]
- 87.Present State Examination, Short Version for Clinical Use, developed by SCAN Advisory Committee on the basis of The SCAN (Schedules for Clinical Assessment in Neuropsychiatry), Version 2, American Psychiatric Press, Inc. 1994.
- 88.Priebe S, Huxley P, Knight S, Evans S. Application and results of the Manchester Short Assessment of Quality of Life (MANSA). Int J Soc Psychiatry. 1999;45(1):7–12. 10.1177/002076409904500102. [DOI] [PubMed] [Google Scholar]
- 89.Purdon, S. (2005). SCIP Manual. January 2005.
- 90.Qian J, Zhou X, Sun X, Wu M, Sun S, Yu X. Effects of expressive writing intervention for women’s PTSD, depression, anxiety and stress related to pregnancy: A meta-analysis of randomized controlled trials. Psych. Res. 2020;288. 10.1016/J.PSYCHRES.2020.112933. [DOI] [PubMed]
- 91.Ridenour JM, Knauss D, Neal DW. Promoting an integrating recovery style: A mentalization-informed approach. J Clin Pscyhol. 2021;77(8):1786–97. 10.1002/jclp.23220. [DOI] [PubMed] [Google Scholar]
- 92.Roe D, Hasson-Ohayon I, Mashiach-Eizenberg M, Derhy O, Lysaker PH, Yanos PT. Narrative Enhancement and Cognitive Therapy (NECT) Effectiveness: A Quasi-Experimental Study. J Clin Psychol. 2014;70(4):303. 10.1002/JCLP.22050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rojo E, Pino O, Guilera G, Gómez-Benito J, Purdon SE, Crespo-Facorro B, Cuesta MJ, Franco M, Martínez-Arán A, Segarra N, Tabarés-Seisdedos R, Vieta E, Bernardo M, Mesa F, Rejas J. Neurocognitive diagnosis and cut-off scores of the Screen for Cognitive Impairment in Psychiatry (SCIP-S). Schizophr Res. 2010;116(2–3):243–51. 10.1016/J.SCHRES.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 94.Romm KL, Synnes O, Bondevik H. Creative writing as a means to recover from early psychosis– Experiences from a group intervention. Arts and Health. 2023;15(3):292–305. 10.1080/17533015.2022.2130379. [DOI] [PubMed] [Google Scholar]
- 95.Samson D, Apperly IA, Braithwaite JJ, Andrews BJ, Bodley Scott SE. Seeing it their Way: Evidence for rapid and involuntary computation of what other people see. J Exp Psychol Hum Percept Perform. 2010;36(5):1255–66. 10.1037/a0018729. [DOI] [PubMed] [Google Scholar]
- 96.Schechner R. (1973): Drama, Script, Theatre, and Performance, in Richard Schechner, Performance Theory. London og New York: Routledge; 1988. [Google Scholar]
- 97.Schmid P, Czekaj A, Frick J, Steinert T, Purdon SE, Uhlmann C. The screen for cognitive impairment in psychiatry (SCIP) as a routinely applied screening tool: pathology of acute psychiatric inpatients and cluster analysis. BMC Psychiatry. 2021;21(1):1–10. 10.1186/s12888-021-03508-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Schnakenberg Martin AM, Lysaker PH. Metacognition, Adaptation, and Mental Health. Biol Psychiat. 2022;91(8):e31–2. 10.1016/J.BIOPSYCH.2021.09.028. [DOI] [PubMed] [Google Scholar]
- 99.Shanks V, Williams J, Leamy M, Bird VJ, Le Boutillier C, Slade M. Measures of personal recovery: A systematic review. Psychiatr Serv. 2013;64(10):974–80. 10.1176/appi.ps.005012012. [DOI] [PubMed] [Google Scholar]
- 100.Simonsen A, Mahnkeke MI, Fusaroli R, Wolf T, Roepstorff A, Michael J, Frith CD, Bliksted V. Distinguishing Oneself From Others: Spontaneous Perspective-Taking in First-Episode Schizophrenia and its relation to Mentalizing and Psychotic Symptoms. Schizophr Bull Open. 2020;1(1). 10.1093/schizbullopen/sgaa053.
- 101.Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, Boyd KA, Craig N, French DP, McIntosh E, Petticrew M, Rycroft-Malone J, White M, Moore L. A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. The BMJ. 2021;374(2018):1–11. 10.1136/bmj.n2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, Boyd KA, Craig N, French DP, McIntosh E, Petticrew M, Rycroft-Malone J, White M, Moore L. Framework for the development and evaluation of complex interventions: Gap analysis, workshop and consultation-informed update. Health Technol Assess. 2021;25(57):i–132. 10.3310/HTA25570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Slade M. Measuring recovery in mental health services. Isr J Psychiatry Relat Sci. 2010;47(3):206–12. [PubMed] [Google Scholar]
- 104.Slade M, Bird V, Clarke E, Le Boutillier C, McCrone P, Macpherson R, Pesola F, Wallace G, Williams J, Leamy M. Supporting recovery in patients with psychosis through care by community-based adult mental health teams (REFOCUS): A multisite, cluster, randomised, controlled trial. The Lancet Psychiatry. 2015;2(6):503–14. 10.1016/S2215-0366(15)00086-3. [DOI] [PubMed] [Google Scholar]
- 105.Stickley T, Wright N, Slade M. The art of recovery: outcomes from participatory arts activities for people using mental health services. J Ment Health. 2018;27(4):367–73. 10.1080/09638237.2018.1437609. [DOI] [PubMed] [Google Scholar]
- 106.Sundhedsstyrelsen. (2022). Bedre mental sundhed og en styrket indsats til mennesker med psykiske lidelser. In Sundhedsstyrelsen (Vol. 1). https://www.sst.dk/-/media/Udgivelser/2022/psykiatriplan/10AARS_PSYK-PLAN.ashx?la=da&hash=CD317811318C4499D2453F25DCEC92B9DF41DE08
- 107.Synnes O, Romm KL, Bondevik H. The poetics of vulnerability: creative writing among young adults in treatment for psychosis in light of Ricoeur’s and Kristeva’s philosophy of language and subjectivity. Med Health Care Philos. 2021;24(2):173–87. 10.1007/s11019-020-09998-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Taylor, G. J., Bagby, R. M., & Parker, J. D. A. The 20-Item Toronto Alexithymia Scale: IV. Reliability and factorial validity in different languages and cultures. J Psychosomatic Res. 2003;55(3), 277–283. 10.1016/S0022-3999(02)00601-3 [DOI] [PubMed]
- 109.Thorup A, Petersen L, Jeppesen P, Øhlenschlæger J, Christensen T, Krarup G, Jørgensen P, Nordentoft M. Integrated treatment ameliorates negative symptoms in first episode psychosis-results from the Danish OPUS trial. Schizophr Res. 2005;79(1):95–105. 10.1016/j.schres.2004.12.020. [DOI] [PubMed] [Google Scholar]
- 110.Van Lith T, Schofield MJ, Fenner P, Lith TV, Schofield MJ, Fenner P. Identifying the evidence-base for art-based practices and their potential benefit for mental health recovery: A critical review. Disabil Rehabil. 2013;35(16):1309–23. 10.3109/09638288.2012.732188. [DOI] [PubMed] [Google Scholar]
- 111.Vauth R, Kleim B, Wirtz M, Corrigan PW. Self-efficacy and empowerment as outcomes of self-stigmatizing and coping in schizophrenia. Psychiatry Res. 2007;150(1):71–80. 10.1016/j.psychres.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 112.Villagonzalo KA, Leitan N, Farhall J, Foley F, McLeod B, Thomas N. Development and validation of a scale for self-efficacy for personal recovery in persisting mental illness. Psychiatry Res. 2018;269(July):354–60. 10.1016/j.psychres.2018.08.093. [DOI] [PubMed] [Google Scholar]
- 113.Williams E, Dingle GA, Jetten J, Rowan C. Identification with arts-based groups improves mental wellbeing in adults with chronic mental health conditions. J Appl Soc Psychol. 2019;49(1):15–26. 10.1111/JASP.12561. [Google Scholar]
- 114.Williams J, Leamy M, Pesola F, Bird V, Le Boutillier C, Slade M. Psychometric evaluation of the Questionnaire about the Process of Recovery (QPR). Br J Psychiatry. 2015;207(6):551–5. 10.1192/bjp.bp.114.161695. [DOI] [PubMed] [Google Scholar]
- 115.Wing, J. K., Babor, T., Brugha, T., Burke, J., Cooper, J. E., Giel, R., Jablenski, A., Regier, D., & Sartorius, N. SCAN. Schedules for Clinical Assessment in Neuropsychiatry. Arch Gen Psychiatr. 1990;47(6), 589–593. 10.1001/archpsyc.1990.01810180089012 [DOI] [PubMed]
- 116.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4. 10.1001/JAMA.2013.281053. [DOI] [PubMed] [Google Scholar]
- 117.Yanos PT, DeLuca JS, Roe D, Lysaker PH. The impact of illness identity on recovery from severe mental illness: A review of the evidence. Psychiatry Res. 2020;288(April): 112950. 10.1016/j.psychres.2020.112950. [DOI] [PubMed] [Google Scholar]
- 118.Yanos PT, Lysaker PH, Roe D. Internalized stigma as a barrier to improvement in vocational functioning among people with schizophrenia-spectrum disorders. Psychiatry Res. 2010;178(1):211–3. 10.1016/J.PSYCHRES.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Yanos PT, Roe D, Markus K, Lysaker PH. Pathways Between Internalized Stigma and Outcomes Related to Recovery in Schizophrenia Spectrum Disorders. Psychiatr Serv. 2008;59(12):1437–42. 10.1176/appi.ps.59.12.1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.