Abstract
Introduction
Intestinal tuberculosis (ITB), a rare yet severe manifestation of Mycobacterium tuberculosis infection, poses significant diagnostic and therapeutic challenges due to its nonspecific clinical presentation. Perforation, a life-threatening complication, necessitates prompt surgical intervention and effective antituberculous therapy.
Case presentation
This case study highlights a 41-year-old immunocompetent male who presented with fever, abdominal pain, vomiting, and significant weight loss. A computed tomography scan revealed minimal pneumoperitoneum, intestinal wall thickening, mesenteric fat stranding, lymphadenopathy, and an intra-abdominal abscess. Exploratory laparotomy identified a perforation at the terminal ileum, leading to ileocaecal resection and stoma formation. Histopathological examination confirmed ITB, and a nine-month regimen of antituberculous medication was initiated.
Discussion
ITB, more common in immunocompromised individuals, can also affect immunocompetent patients, often mimicking other gastrointestinal conditions and delaying diagnosis. This case underscores the importance of considering ITB in differential diagnoses for patients with vague gastrointestinal symptoms. Diagnostic confirmation typically requires a combination of clinical, radiological, and microbiological assessments, with histopathology playing a crucial role. Factors such as age and comorbidities can increase the risk of severe complications like perforation. Surgical resection with anastomosis tends to yield better outcomes than direct closure, and comprehensive antituberculous therapy is essential for successful treatment.
Conclusion
The complexity of diagnosing and managing ITB, compounded by its severe complications, necessitates heightened awareness among healthcare providers. Accurate diagnosis, timely surgical intervention, and rigorous antituberculous therapy are vital for improving patient outcomes, especially in high-risk populations or regions with prevalent TB.
Keywords: Intestinal tuberculosis, Mycobacterium tuberculosis, Perforation, Abdominal tuberculosis
Highlights
-
•
Diagnosis of intestinal tuberculosis is challenging due to nonspecific symptoms.
-
•
Intestinal tuberculosis can mimic inflammation, infection, or malignancies.
-
•
Bowel perforation due to intestinal tuberculosis is associated with high mortality.
-
•
A combined approach of surgery and tuberculostatic therapy led to a complete cure.
1. Introduction
Intestinal tuberculosis (ITB) is a rare but serious presentation of Mycobacterium tuberculosis infection, predominantly affecting the ileocaecal region of the gastrointestinal tract [1]. Despite the decline in global tuberculosis rates, extrapulmonary forms, including intestinal tuberculosis, continue to pose significant challenges due to their nonspecific clinical presentation.
While ITB is more common in immunocompromised individuals, such as those with HIV or on immunosuppressive therapy, it can also occur in immunocompetent patients, though less frequently. Early diagnosis and prompt treatment are critical in preventing severe complications, such as bowel obstruction, strictures, and perforation. Perforation, in particular, is a life-threatening complication that requires early recognition and prompt surgical intervention [2]. It arises from the transmural involvement of the bowel wall by caseating granulomas, which can lead to peritonitis and sepsis if not addressed promptly. Contrast-enhanced computed tomography is crucial for diagnosis [3].
The management of ITB involves a combination of surgical intervention for complications like perforation and long-term antituberculous therapy. Surgical resection of the affected bowel segment [4], followed by the administration of a standard antituberculous drug regimen, is essential for preventing recurrence and ensuring patient recovery [5]. However, there are no standardized guidelines for the surgical management of ITB, and the choice of procedure often depends on the severity of the disease and the surgeon's experience.
In this report, we present a unique case of intestinal tuberculosis complicated by perforation in an immunocompetent patient. This case highlights the challenges in diagnosing ITB in the absence of immunosuppression and underscores the need for increased clinical suspicion and timely intervention to avoid catastrophic outcomes. By sharing this case, we aim to contribute to the limited literature on ITB in immunocompetent patients and emphasize the importance of considering this diagnosis in patients with unexplained gastrointestinal symptoms.
2. Case presentation
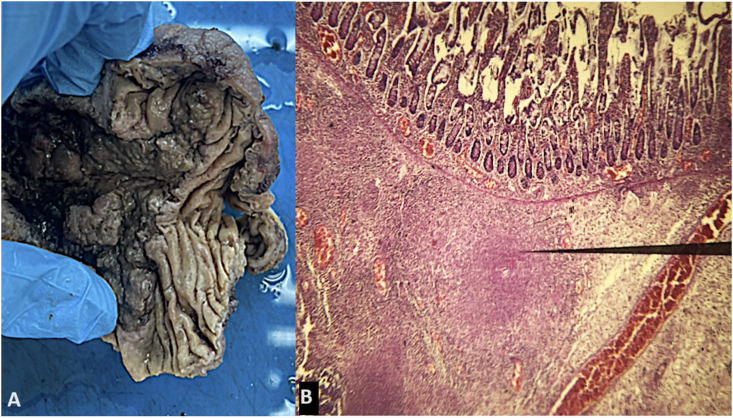
A 41-year-old immunocompetent male presented with a two-month history of generalized abdominal pain, vomiting, fever (39 °C), and a 5-kg weight loss. On physical examination, the patient exhibited diffuse abdominal tenderness and guarding. Initial laboratory workup revealed elevated inflammatory markers and a computed tomography (CT) scan of the abdomen showed minimal pneumoperitoneum, thickening of the intestinal wall, mesenteric fat stranding, multiple lymphadenopathies, and a 26 × 21 mm intra-abdominal abscess (Fig. 1). Based on these findings, the decision was made to perform an exploratory laparotomy. Intraoperative findings included the presence of approximately 100 cc of purulent fluid in the pelvic cavity and a 5 mm perforation at the terminal ileum. An ileocaecal resection was performed with the creation of a double-barrel stoma (ileostomy and colostomy). Histopathological analysis of the resected bowel revealed caseating granulomas with Langhans giant cells and epithelioid cells, confirming a diagnosis of intestinal tuberculosis (Fig. 2). Mycobacterial culture from the biopsy also tested positive for Mycobacterium tuberculosis. The patient tested negative for HIV antibodies, ruling out immunosuppression as a contributing factor. The patient was started on a nine-month course of antituberculous medication comprising ethambutol, pyrazinamide, rifampicin, and isoniazid. Postoperative recovery was uneventful, and the patient was discharged with regular follow-up planned for monitoring both stoma function and response to antituberculous therapy.
Fig. 1.
Computed tomography scan demonstrating small bowel wall thickening (white arrow) with increased stranding of mesenteric fat and abdominal lymph nodes.
Fig. 2.
Resected specimen (A), Intestinal mucosa with numerous tuberculoid, epithelioid and giganto-cellular granulomas with caseous necrosis in the submucosa (B).
3. Discussion
Diagnosis: Intestinal tuberculosis is a rare form of extrapulmonary tuberculosis that primarily affects the gastrointestinal tract. While ITB is more commonly seen in immunocompromised individuals, such as those with HIV/AIDS or on immunosuppressive therapy, it can also occur in immunocompetent patients [3]. ITB commonly affects the isolated ileocaecal region and distal ileum without significant caecum or ascending colon involvement [6]. It is often overlooked due to its nonspecific symptoms, such as abdominal pain, fever, and weight loss, which can mimic other gastrointestinal disorders, including Crohn's disease and malignancy. Patients may also experience changes in bowel habits. Roberto de Jesús Martínez Camacho et al. [7] and Laklaai Z et al. [8] demonstrated unusual manifestations of tuberculosis, with one presenting as chronic diarrhea and abdominal pain in an HIV patient leading to perforation, and the other showcasing multifocal tuberculosis in an immunocompetent individual with diverse organ involvement. In this case, the patient's vague symptoms delayed diagnosis, highlighting the need for clinicians to maintain a high index of suspicion in patients presenting with unexplained abdominal complaints, even when immunosuppression is absent.
A combination of clinical, radiological, and microbiological findings is often required for an accurate diagnosis. Imaging, such as contrast-enhanced computed tomography played a crucial role by revealing suggestive features like bowel wall thickening and mesenteric lymphadenopathy, though these findings are not pathognomonic for ITB [9]. Microbiological confirmation of intestinal TB is challenging, as the yield of acid-fast bacilli (AFB) smear and culture is often low. Endoscopic examinations, including colonoscopy and upper gastrointestinal endoscopy, can aid in obtaining biopsy samples for histopathological examination. The latter confirm the diagnosis through the identification of caseating granulomas with or without AFB on staining. Polymerase chain reaction (PCR) assays targeting Mycobacterium tuberculosis DNA can also be used to enhance diagnostic accuracy [10]. Recent studies suggest that fecal or stool samples can be effective in diagnosing abdominal tuberculosis, including ITB. In particular, Gaur et al. [11] demonstrated that stool-based diagnostics, such as nucleic acid amplification tests (NAAT), can improve the detection of Mycobacterium tuberculosis in patients with abdominal TB. This non-invasive approach is especially valuable when access to biopsy samples is limited or when endoscopic procedures are not feasible. Incorporating such diagnostic methods into clinical practice could enhance the early identification of ITB, facilitating timely treatment and reducing complications. This case underscores the importance of combining clinical, radiological, microbiological, and histopathological data to accurately diagnose ITB.
Complications: Perforation is a serious, life-threatening complication of ITB, occurring due to the transmural spread of caseating granulomas. It leads to peritonitis and sepsis if not treated promptly. Although more common in immunocompromised individuals, perforation can occur in immunocompetent patients, as seen in this case. Delayed diagnosis of ITB, advanced disease, and older age have been associated with an increased risk of perforation [12]. In this patient, a lack of early recognition likely contributed to the development of this severe complication.
Therapy: There are no standardized guidelines for the surgical treatment of intestinal tuberculosis perforations. Surgical options include resection of the affected bowel segment, strictureplasty, and drainage of abscesses, but resection and anastomosis appear to be better than simple suture repair due to lower mortality rates [13]. Di Buono et al. [14] demonstrated the feasibility of using a totally laparoscopic approach to treat complicated cases of intestinal tuberculosis, even in the emergency setting of bowel perforation. Pharmacological anti-tubercular therapy is the essential component of treatment, regardless of the surgical approach. The standard anti-tubercular therapy ATT regimen consists of a combination of isoniazid, rifampicin, pyrazinamide, and ethambutol. The duration of treatment varies but is typically extended to 9–12 months to ensure complete eradication of the infection and prevent recurrence [2].
Results: The patient responded well to surgery and antituberculous therapy, with no immediate postoperative complications. Regular follow-up is crucial to ensure stoma function, assess for potential recurrence, and monitor for drug toxicity. The early initiation of appropriate therapy, including both surgical and medical management, contributed to the favorable outcome.
Limitations of the Present Case: One limitation of this case is the delayed diagnosis, which likely contributed to the perforation. Earlier consideration of ITB, particularly in patients with unexplained abdominal symptoms in regions where tuberculosis is prevalent, could have potentially prevented the complication. Additionally, the decision to create a double-barrel stoma rather than primary anastomosis may require further discussion regarding its appropriateness, especially given the absence of other complicating factors such as immunosuppression or hemodynamic instability.
4. Conclusion
This case highlights the diagnostic challenges of intestinal tuberculosis in immunocompetent patients and underscores the need for timely intervention to prevent severe complications like perforation. Surgical resection combined with antituberculous therapy remains crucial for effective treatment. The rarity of this case emphasizes the importance of raising clinical awareness, particularly in regions where tuberculosis is prevalent.
CRediT authorship contribution statement
Imen Ben Ismail: Writing – original draft, Investigation, Data curation, Conceptualization. Saber Rebii: Investigation, Formal analysis. Mlika Mouna: Investigation, Conceptualization. Marwen Sghaier: Investigation, Data curation. Khadija Yaich: Investigation. Ayoub Zoghlami: Supervision.
Ethics statement
Ethical review and approval were not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
N/A.
References
- 1.Maulahela H., Simadibrata M., Nelwan E.J., Rahadiani N., Renesteen E., Suwarti S.W.T., et al. Recent advances in the diagnosis of intestinal tuberculosis. BMC Gastroenterol. 2022;22:89. doi: 10.1186/s12876-022-02171-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Angie E., Vargas Rodríguez, Ansony R., Godinez Vidal, Raymundo Alcántara, Gordillo, Cristobal S., Duarte Regalado, Jesús O., Soto Llanes. A case report and literature review of intestinal perforation due to. Tuberculosis. Cureus. 2023;15(8) doi: 10.7759/cureus.43241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheong J.Y., Faraj S. Rare case of colonic perforation from disseminated fungal infection in immunocompetent patient. Int. Surg. 2023;107:12–14. [Google Scholar]
- 4.Coccolini F. Tubercular bowel perforation: what to do? Ulusal Travma Ve Acil Cerrahi Dergisi. 2011;17:66–74. doi: 10.5505/tjtes.2011.39145. [DOI] [PubMed] [Google Scholar]
- 5.Wu Y.-F., Ho C.-M., Yuan C.-T., Chen C.-N. Intestinal tuberculosis previously mistreated as Crohn's disease and complicated with perforation: a case report and literature review. SpringerPlus. 2015;4 doi: 10.1186/s40064-015-1129-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ben Ismail I., Zenaidi H., Rebii S., Zoghlami A. A pitfall in the diagnosis of ileocaecal tuberculosis. Int. J. Infect. Dis. 2020;96:671–672. doi: 10.1016/j.ijid.2020.05.084. [DOI] [PubMed] [Google Scholar]
- 7.De Jesús Martínez Camacho R., Correa S.S., Sierra H.L., Gómez M.F.R., Paredes E.N., Orozco F.A.G., et al. Intestinal tuberculosis with small bowel perforation in a patient with AIDS: a case report. International Journal of Medical Science and Clinical Research Studies. 2024;4 [Google Scholar]
- 8.Laklaai Z., Channoune K., Zaghba N., Benjelloune H., Yassine N. Multifocal tuberculosis in the immunocompetent patient. Eur. Respir. J. 2022;60:4214. [Google Scholar]
- 9.Chan D.K.-H., Lee K.-C. Perforated intestinal tuberculosis in a non-AIDS immunocompromised patient. The American Journal of Case Reports. 2015;16:719–722. doi: 10.12659/AJCR.894723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mekaiel A., Al-Tkrit A., Aneeb M., et al. Tuberculosis in an immunocompetent immigrant patient. Cureus. 2020;12(9) doi: 10.7759/cureus.10225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gaur M., Singh A., Sharma V., Tandon G., Bothra A., Vasudeva A., et al. Diagnostic performance of non-invasive, stool-based molecular assays in patients with paucibacillary tuberculosis. Sci. Rep. 2020;10:7102. doi: 10.1038/s41598-020-63901-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holmes K.K., Bertozzi S., Bloom B.R., Jha P., Gelband H., DeMaria L.M., et al. Third Edition; The World Bank eBooks: 2017. Major Infectious Diseases: Key Messages from Disease Control Priorities; pp. 1–27. [PubMed] [Google Scholar]
- 13.Sasse D., Spinner C.D., Rothe K., Schneider J., Gaa J., Würstle S. Treatment of intestinal tuberculosis with small bowel perforation: a case report. J. Med. Case Rep. 2021;15 doi: 10.1186/s13256-021-02752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Di Buono G., Vella R., Amato G., Romano G., Rodolico V., Saverino M., et al. Totally laparoscopic treatment of intestinal tuberculosis complicated with bowel perforation: the first case report in worldwide literature with a brief review. Frontiers in Surgery. 2022;9 doi: 10.3389/fsurg.2022.956124. [DOI] [PMC free article] [PubMed] [Google Scholar]