Introduction
Although very infrequent, squamous cell carcinoma (SCC) has been described as a possible complication of hidradenitis suppurativa (HS) [1–3]. Herein, we describe three cases of SCC and one case of basal cell carcinoma (BCC) complicating HS, with the aim of raising concerns about the possibility of malignancy in these patients.
Case Presentation
All patients with HS from January 1985 to December 2023 whose lesions were biopsied or had undergone surgery at our hospital were evaluated. Patients that had developed malignancies within HS lesions were selected. Overall, 580 patients with a histologic study of HS were evaluated. Of these, four patients (0.7%) presented malignancies within lesions of HS (3 SCC; 1 BCC) (Table 1). The median age of patients was 62.5 years (range 62–73). Clinical and histological information of each patient is displayed in Table 1.
Table 1.
Clinical characteristics of patients and histologic features of the lesions.
| Patient | Sex (age in years) | Smoker | Hurly Stage | Duration of HS (years) | Previous treatments for HS | Location of Cancer | Macroscopic appearance | Histology | HPV | Surveillance | Comments |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female (73) | Yes | ? | ? | ? | Vulva | 6.2 × 6 cm tumor in the anterior region of the vulva, affecting labia mayor and minor of both sides. | Keratinizing and well-differentiated squamous cell carcinoma over foci of hidradenitis suppurativa with abscesses and scarring fibrosis. Depth of infiltration: 14 mm. | – | Free of relapse 6 months after surgical intervention | No nodal involvement or distant metastases |
| 2 | Male (60) | Yes | III | 35 | Antibiotics Metformin Surgery | Gluteal region | Multiple fistulae with fibrosus scars all over gluteal region. In the inferior pole of the right buttock there is an 8×4 cm hyperkeratotic and ulcerated nodule | Multiple epidermal fistulae with surrounding mixed inflammatory infiltrate and areas of fibrous scarring are seen. In various foci, well-differentiated squamous cell carcinoma nests can be observed arising from these fistulae. Various corneal pearls and pseudoepitheliomatous hyperplasia are seen. | – | Died due to infectious complications of the HS 3 months after surgery of the SCC | Sacral and pelvic osteomyelitis, epidural empyema, bacterial meningitis, and bacteriemia secondary to sacral and gluteal abscesses No nodal involvement or distant metastases |
| 3 | Male (63) | Yes | III | 41 | Antibiotics Retinoids Corticosteroids Metformin Secukinumab (last 10 months) CO2 laser Surgery | Gluteal region | Indurated erythematous plaque with multiple subcutaneous abscesses and fistulae affecting both buttocks and intergluteal region | Numerous cavities and fistulae with surrounding inflammation and fibrosis. Multiple foci of well differentiated squamous cell carcinoma can be seen arising from cavities and fistulae, affecting dermis and hypodermis. | – | Free of relapse 9.5 months after the surgical intervention | No nodal involvement or distant metastases |
| 4 | Female (62) | Yes | ? | ? | ? | Right inguinal region | Ulcerated greyish plaque of 9.7 × 4 cm with surrounding erythema, suppurating fistulae, and fibrous scars | Solid basal cell carcinoma | ? | Free of relapse 22.5 months after the surgical intervention |
Abbreviations: HPV: human papilloma virus; HS: hidradenitis suppurativa; SCC: squamous cell carcinoma; ?: Unknown; –: negative.
In Patients 1, 2, and 4, in whom macroscopic tumoral lesions were evident, surgery was performed as oncological treatment. In Patient 3, in whom no clinically evident malignant lesion was seen (Figure 1A), surgery was performed due to failure of medical treatments, and a SCC was detected as an incidental finding (Figure 1E). Histologically, Patients 1–3 presented a well-differentiated multifocal SCC, which grew along fibrosed fistulae (Figures 1B–D and F–H). Similarly, Patient 4 showed a solid BCC growing along these fistulae as well (Figure 2). Patients 1, 3, and 4 remain free of relapse 6, 9.5, and 22.5 months after surgery, respectively. Patient 2 died from infectious complications derived from HS.
Figure 1.
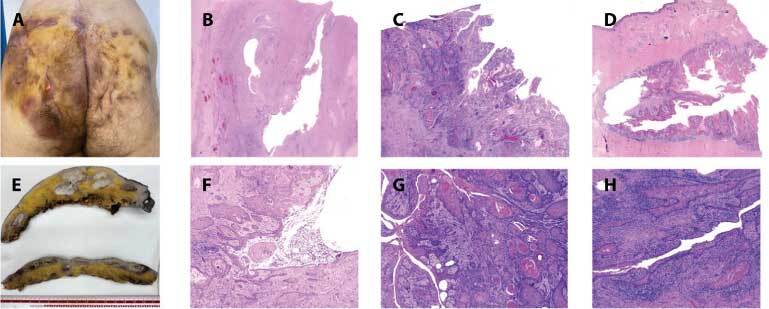
(A) Clinical appearance of Patient 3: extensive plaques of HS with multiple fistulae openings. (B–D) Microscopic appearance of squamous cell carcinoma arising within sinus of hidradenitis suppurativa lesions; Patients 1–3, respectively (H&E, ×10). (E) Macroscopic appearance of the resected surgical specimen in Patient 3: multifocal nodular infiltrating lesions. (F–H) Irregular epidermic sharp-shaped proliferation that invades the underlying dermis and grows along the sinuses (Patients 1–3, respectively). Note that some cornified pearls can be observed in F and G (H&E, 40).
Figure 2.
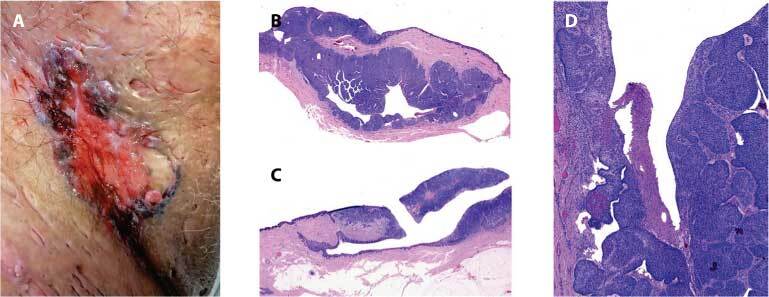
Basal cell carcinoma within hidradenitis suppurativa lesions. (A) Clinical appearance of the basal cell carcinoma in Patient 4: ulcerated plaque with irregular and pigmented borders and scarred surrounding tissue. (B, C) Areas of basal cell carcinoma nests along margins of a sinus (H&E, ×10). (D) Multiple nests composed of basaloid cells, and peripheric cleft (H&E, ×40).
Discusssion
SCC has been reported as a very rare complication of HS, related to maintained inflammation [1–3]. Most reported SCC are well-differentiated type; nonetheless, the potential spread of SCC along fistulae and sinus should be highlighted, which could easily go unnoticed if superficial biopsies were taken, only detecting areas of pseudoepitheliomatous hyperplasia [1–4]. Even though histologic appearance might seem inconspicuous, SCC arising within HS can be multifocal, and thus show an aggressive behavior [1,3,5]. In general, wide local excision is the first-line therapy [1,3]. Nevertheless, this might be challenging due to the affected anatomical locations, multifocality and extension of SCC within HS fistulae [3]. It must be highlighted that Patients 1 and 2 showed an evident nodule within HS. Nonetheless, patients are frequently discouraged and tired of recurrent activity periods of HS and might thus disregard complications of their disease. Similarly, subclinical presentation is also possible, as occurred in Patient 3. In addition, to the authors’ knowledge, the present is the first reported case of basal cell carcinoma arising within HS in a non-sun exposed area.
Conclusion
In conclusion, SCC is a potential complication of HS, which may go unnoticed and show a more aggressive behavior than expected. Although extremely rare, BCC could also show within HS. Therefore, a periodic examination of patients and a histological analysis of resected HS lesions are needed to detect malignancies within HS early.
Footnotes
Funding: None.
Competing Interests: None.
Authorship: All authors have contributed significantly to this publication.
References
- 1.Sachdeva M, Mufti A, Zaaroura H, et al. Squamous cell carcinoma arising within hidradenitis suppurativa: a literature review. Int J Dermatol. 2021;60(11) doi: 10.1111/ijd.15677. [DOI] [PubMed] [Google Scholar]
- 2.Gierek M, Niemiec P, Szyluk K, Ochala-Gierek G, Bergler-Czop B. Hidradenitis suppurativa and squamous cell carcinoma:a systemic review of the literature. Adv Dermatol Allergol. 2023;40(3):350–354. doi: 10.5114/ada.2023.126563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lavogiez C, Delaporte E, Darras-Vercambre S, et al. Clinicopathological Study of 13 Cases of Squamous Cell Carcinoma Complicating Hidradenitis Suppurativa. Dermatology. 2010;220(2):147–153. doi: 10.1159/000269836. [DOI] [PubMed] [Google Scholar]
- 4.Racanelli E, Jfri A, Gefri A, et al. Cutaneous Squamous Cell Carcinoma in Patients with Hidradenitis Suppurativa. Cancers. 2021;13(5):1153. doi: 10.3390/cancers13051153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martorell A, García-Martínez FJ, Jiménez-Gallo D, et al. An Update on Hidradenitis Suppurativa (Part I): Epidemiology, Clinical Aspects, and Definition of Disease Severity. Actas Dermosifiliogr (Engl Ed) 2015;106(9):703–715. doi: 10.1016/j.adengl.2015.09.008. [DOI] [PubMed] [Google Scholar]


