Abstract
Introduction
Dermoscopy is an important noninvasive tool that helps to determine the stability and activity of vitiligo. Various dermoscopic findings help classify the disease as stable or unstable. This is important for the management of the disease, as surgical management requires disease stability.
Objectives
We aimed to describe the dermoscopic findings in vitiligo and to assess the frequency of various dermoscopic findings in stable and unstable vitiligo.
Methods
This was a hospital-based cross-sectional descriptive study of 100 vitiligo patients and various dermoscopic findings. Results are expressed as percentages.
Results
The most common dermoscopic findings in stable vitiligo patches were sharp border, marginal and perifollicular pigmentation, and reticulate pigment network. Findings such as polka dot appearance, starburst appearance, comet tail, and satellite lesions were seen in unstable vitiligo patches.
Conclusions
Dermoscopy is extremely helpful in determining the stability of vitiligo patches.
Keywords: Dermoscopy, Vitiligo, Stability of vitiligo, Activity of vitiligo
Introduction
Vitiligo is an autoimmune disorder which is clinically characterized by depigmented macules. Though the disease is considered to be asymptomatic, it has adverse cosmetic and psychological effects on patients. There are multiple management options, including medical and surgical therapy, depending on the disease activity and stability. Assessing the activity of the disease is of paramount value because the stability of the disease is important for surgical management. Dermoscopy is a noninvasive tool that allows the identification of subtle features in stable and unstable vitiligo that are otherwise invisible to the naked eye. Thus, dermoscopy aids in evaluating disease activity and guides in the management.
Objectives
The study aimed to describe various dermoscopic findings in stable and unstable vitiligo, including patients who are undergoing treatment, and to assess the frequency of various dermoscopic findings in stable and unstable vitiligo
Methods
This hospital-based cross-sectional descriptive study was carried out over a period of six months in the Department of Dermatology at Andhra Medical College. The study subjects were 100 clinically diagnosed patients of vitiligo who were attending the Dermatology Department of our Institute. All vitiligo patients, including patients who were on treatment, were included in the study. Patients with other causes of hypopigmentation and depigmentation were excluded. Approval from the institutional ethics committee was taken prior to the study. A written informed consent was taken from all study participants. A pre-structured proforma was used to collect the baseline data. Based on the patient’s history, the disease was classified as stable or unstable vitiligo.
The criteria for stability included absence of any new lesions, no progression of existing lesions, and absence of Koebner phenomena for the past one year [1]. In addition, repigmentation of depigmented area by medical treatment was also taken as a criteria for stability [2].
After detailed history taking and clinical examination, dermoscopic examination was performed with a DermLite DL4 handheld dermatoscope under polarized light. Photographs were taken, and findings were documented. The frequency of each finding was calculated separately for stable and unstable vitiligo patches. Data analysis was done using Microsoft Office 2021, and results are expressed as percentages.
Results
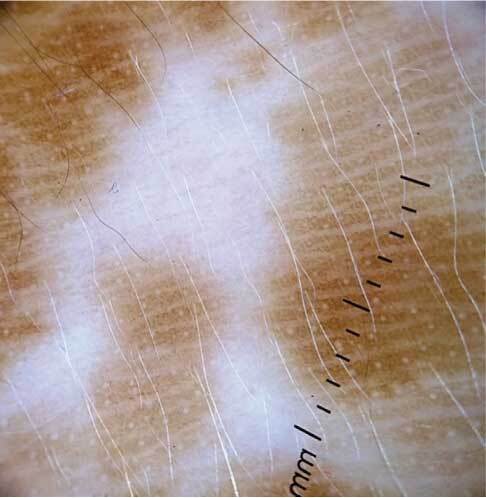
This study comprised 62 male patients and 38 female patients. The most common age group involved was between 3–40 years. Among the study participants, 56 (56%) patients had clinically stable vitiligo, and 44 patients had unstable vitiligo. Dermoscopic examination revealed three patterns of borders in vitiligo patches: sharp border, irregular border and trichrome pattern (Figure 1A–C). Among the 56 stable vitiligo patients, the most commonly observed pattern was sharp border (n=44, 78.6%), followed by irregular border (n=10, 17.9%). Trichrome pattern was seen only in two patients with stable vitiligo (3.6%). In patients with unstable vitiligo, irregular border (n=22, 50%), followed by trichrome pattern (n=20, 45.5%) were commonly observed (Table 1). Four types of pigment network patterns were observed in vitiligo patches: reticular pigment pattern, reduced pigment network, absent pigment network, and reverse pigment network (Figure 2A–D). Among these, reticular pigment network was most commonly seen in stable vitiligo patches (n=32, 57.1%), whereas in unstable vitiligo, absent pigment network was most frequent (n=22, 50%) (Table 2). The other dermoscopic findings that were noted in most of the stable vitiligo patches were marginal hyperpigmentation (n=44, 78.6%) and perifollicular hyperpigmentation (n=40, 71.4%). Marginal pigmentation was seenonly in patients with unstable vitiligo (Table 3). Leukotrichia was noted in 28 patients with stable vitiligo and 18 patients with unstable vitiligo (Figure 3; Table 4). Few findings were seen only in unstable vitiligo patches, including polka dot appearance (n=18, 40.9%), starburst appearance (n=10, 22.7%), comet tail appearance (n= 8, 18.2%), and satellite lesions (n=18, 40.9%) (Figure 4A–D). Patients who were on treatment with either steroids or NBUVB had erythema and telangiectasia in addition to the above-mentioned findings (Table 5; Figure 5A–B).
Figure 1.
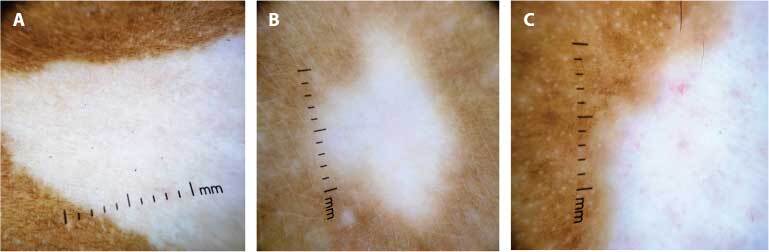
Dermoscopic examination with polarized light showing borders of vitiligo patches: (A) sharp border, (B) irregular border, (C) trichrome pattern.
Table 1.
Frequency of Distribution of Various Dermoscopic Patterns Vitiligo Border Patches in Stable and Unstable Vitiligo.
| Sharp Border | Irregular | Trichrome | |
|---|---|---|---|
| Stable | 44(78.6%) | 10(17.9%) | 2(3.6%) |
| Unstable | 2(4.5%) | 22(50%) | 20(45.5%) |
| On treatment | 10(33.3%) | 14(46.7%) | 6(20%) |
Figure 2.

Dermoscopic examination of pigmentary network in vitiligo patches with polarized light: (A) reticular pigment network, (B) reduced pigment network, (C) absent pigment network, (D) reverse pigment network.
Table 2.
Frequency of Distribution of Pigmentary Network Pattern on Dermoscopy Among Stable and Unstable Vitiligo Patches.
| Stable | Unstable | On treatment | |
|---|---|---|---|
| Absent pigment network | 14(25%) | 22(50%) | 10(33.3%) |
| Reticular pigment network | 32(57.1%) | 2(4.5%) | 8(26.7%) |
| Reduced pigment network | 10(17.9%) | 8(18.2%) | 8(26.7%) |
| Reverse pigment network | 0 | 12(27.3%) | 4(13.3%) |
Table 3.
Frequency of Distribution of Marginal and Perifollicular Pigmentation Among Stable and Unstable Vitiligo Patches.
| Marginal Hyperpigmentation | Perifollicular Hyperpigmentation | |
|---|---|---|
| Stable | 44(78.6%) | 40(71.4%) |
| Unstable | 4(9.1%) | 6(13.63%) |
| On treatment | 16(53.33%) | 12(40%) |
Figure 3.
Dermoscopic examination with polarized light showing leukotrichia within the vitiligo patch.
Table 4.
Frequency of Distribution ofLeukotrichia Among Stable and Unstable Vitiligo Patches.
| Number of Patients | |
|---|---|
| Stable | 28(50%) |
| Unstable | 18(40.9%) |
| On treatment | 10(33.3%) |
Figure 4.
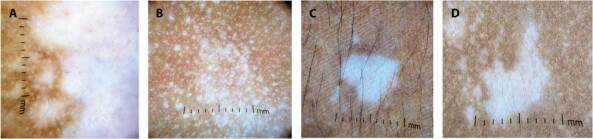
Dermoscopic examination with polarized light showing:(A) polka dot appearance, (B) starburst appearance, (C) comet tail appearance, (D) satellite lesions.
Table 5.
Frequency of Distribution of Erythema and Telangiectasia Among Stable and Unstable Vitiligo Patches On Treatment.
| Erythema | Telangiectasia | |
|---|---|---|
| Stable | 2(3.57%) | 0 |
| Unstable | 8(18.2%) | 8(18.2%) |
| On treatment | 10(33.3%) | 8(26.6%) |
Figure 5.
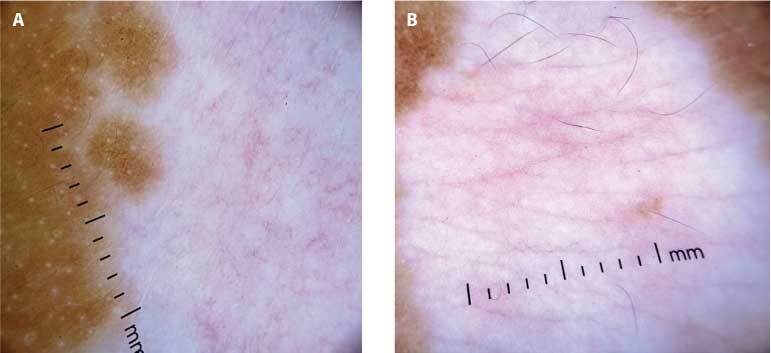
Dermoscopic examination with polarized light in vitiligo patients who are on treatment showing (A) erythema and (B) telangiectasia.
Discussion
Out of 56 clinically diagnosed stable vitiligo patients, the most common dermoscopic findings observed were sharp border in 44 (78.6%), marginal hyperpigmentation in 44 (78.6%), perifollicular hyperpigmentation in 40 (71.4%), and reticular pigment network in 16 (57.14%). Among the 44 unstable vitiligo cases, frequent findings were irregular border in 22 (50%), trichrome pattern in 20 (45.4%), polka dot appearance in 18 (40.9%), and satellite lesions in 18 (40.9%). Erythema and telangiectasia were noted only in patients who were on treatment (33.3% and 26.6%, respectively).
A study done by Purnima et al. noticed marginal hyperpigmentation in 100% of stable vitiligo patients [2]. In our study, 78.6% of patients with stable vitiligo showed marginal hyperpigmentation. Nirmal et al. proposed that absence of satellite lesions and absence of micro-Koebner phenomena (comet tail) were the most sensitive markers of stable vitiligo [3]. Similarly, in our study, none of the patients with stable vitiligo had satellite lesions or comet tail appearance. In another study, Nirmal mentioned the utility of blue light in dermoscopy to diagnose stable lesions in vitiligo, as the blue light increases the contrast between areas with preserved melanin and those with melanin loss [4].
Awar et al. concluded that presence of erythema and telangiectasia indicated treatment response [1]. In our study, only patients who were undergoing treatment had erythema or telangiectasia on dermoscopy. A study by Thatte et al. found that 90% of the evolving vitiligo patches had white glow in dermoscopic examination [5]. In our study, we did not mention diffuse white glow, as most of the lesions were depigmented. Aljasser mentioned the use of dermoscopy in detecting leukotrichia in facialpatches that are otherwise invisible to the naked eye [6]. In our study also, we found that dermoscopyhelped to detect subtle leukotrichia, which are not seen on the normal clinical examination. Abhijeet et al. described post-graft trichrome and Manchurian gravy signs on dermoscopy as a predictor of disease activity after skin grafting [7]. In our study, none of the patients underwent any surgical procedures.
Limitations
The patient history may not be reliable in some cases to assess the activity of vitiligo to correlate clinically. Histopathologyor any other confirmatory investigations were not done for any of the cases.
Conclusions
Dermoscopic findings like sharp border, perifollicular and marginal hyperpigmentation, and reticular pigment network suggest stability. Irregular border and trichrome pattern were the most common dermoscopic findings noted in unstable vitiligo patches. Patterns like polka dots, satellite lesions, reverse pigment network, and starburst appearance were seen only in unstable vitiligo patches. Patients who were on treatment showed erythema and telangiectasia in addition. Thus, dermoscopy is useful in assessing the activity of vitiligo and response to treatment. Since stability of vitiligo is necessary for surgical management, dermoscopic examination helps to guide the management of the disease by assessing the activity and stability.
Footnotes
Funding: None.
Competing Interests: None.
Authorship: All authors have contributed significantly to this publication.
References
- 1.Awal G, Kaur J, Kaur K. Dermoscopy in Vitiligo: An emerging armamentarium in diagnosis and activity assessment. Pigment International. 2022 Jan 1;9(1) doi: 10.4103/pigmentinternational.pigmentinternational_143_21. [DOI] [Google Scholar]
- 2.Purnima G, Tejaswitha Gudivada NA, Narasimharao TV. Dermoscopy— a tool to assess stability in vitiligo. Int J Contemp Med Res. 2017;4(10):2066–8. [Google Scholar]
- 3.Nirmal B, Antonisamy B, Peter CD, George L, George AA, Dinesh GM. Cross-sectional study of dermatoscopic findings in relation to activity in vitiligo: BPLeFoSK criteria for stability. Journal of Cutaneous and Aesthetic Surgery. 2019 Jan;12(1):36. doi: 10.4103/JCAS.JCAS_147_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nirmal B. Utility of blue light in dermoscopy for diagnosing stable lesions in vitiligo. Dermatology Practical & Conceptual. 2021 Jan 29;:e2021141. doi: 10.5826/dpc.11041a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thatte SS, Khopkar US. The utility of dermoscopy in the diagnosis of evolving lesions of vitiligo. Indian Journal of Dermatology, Venereology and Leprology. 2014 Nov 1;80:505. doi: 10.4103/0378-6323.142074. [DOI] [PubMed] [Google Scholar]
- 6.AlJasser MI. Dermoscopy for facial leukotrichia in vitiligo: An important step for a better treatment decision. Dermatol Pract Concept. 2022 Jul;12(3) doi: 10.5826/dpc.1203a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jha AK, Sonthalia S, Lallas A, Chaudhary RK. Post-graft trichrome and Manchurian gravy signs on dermoscopy can predict disease activity in vitiligo lesions post-skin grafting. Int J Dermatol. 2018 Aug 3;57(11):e144–5. doi: 10.1111/ijd.14141. [DOI] [PubMed] [Google Scholar]


