Abstract
Retinal vascular occlusions are rare in young people, and any occlusion warrants an extensive clinical evaluation to establish the etiology. Cardiac malformations are a source of embolism. We present a case of atrial septal defect (ASD) in a patient with type II Mayer-Rokitansky-Küster-Hauser syndrome, leading to unilateral branch retinal arterial occlusion (BRAO) in a young woman. A 21-year-old woman presented with sudden, painless, blurring of vision, and a superior visual field defect in her right eye. A fundus examination confirmed the BRAO diagnosis. Ocular and systemic evaluation revealed primary amenorrhea, ASD, ectopic kidneys, and pelvic cyst. Any vascular occlusion in a young patient must be thoroughly evaluated, including a detailed systemic history.
Keywords: Atrial septal defect, branch retinal arterial occlusion, Mayer-Rokitansky-Küster-Hauser syndrome, primary amenorrhea, retinal vascular occlusion
Introduction
Branch retinal arterial occlusion (BRAO) represents nearly one-third of all acute retinal artery obstructions.[1,2] Arterial hypertension, carotid artery diseases, diabetes mellitus, hyperlipidemia, hyperuricemia, and chronic smoking are the most frequent age-adjusted risk factors for retinal arterial occlusions (RAOs), including BRAO.[2] BRAO is seen mostly in the elderly and is rare in young adults.[2] The embolic episodes are the most common association of BRAO in the elderly.[3] Hypercoagulability is the most prevalent underlying condition in young adults, followed by cardiac valvular diseases.[4,5] However, there are some geographic or ethnic differences. Raised homocysteine levels accounted for the majority of RAO in an Indian patients, while hypercoagulable conditions were more prevalent among Western individuals.[4,5] Hence, a comprehensive systemic evaluation is needed for a young patient with retinal vein occlusion (RVO) to pinpoint the underlying cause. We report a case of BRAO in an apparently asymptomatic young female patient with a history of primary amenorrhea, in which a comprehensive approach led to the detection of type II Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome and atrial septal defect (ASD).
Case Report
A 21-year-old girl presented to the ophthalmology department with the complaint of sudden, painless blurring of vision in her right eye with loss of superior half of her visual field of 1-day duration. She had no history of ocular trauma, flashes, floaters, or other ocular symptoms. There was no history of breathlessness, fatigue, palpitations, and recurrent respiratory infections. Obstetric history was significant for primary amenorrhea.
Her visual acuity at the presentation was 6/9 in the right eye and 6/6 in the left eye, which improved to 6/6 in the right eye but the upper half of the alphabets on Snellen’s chart was missing. A relative afferent pupillary defect was observed in the right eye and the rest of the anterior segment examination was within normal in both eyes. Intraocular pressure (IOP) was 15 mmHg bilaterally. On fundus examination, the right eye showed a pale area in the inferotemporal retina around the macular region suggestive of BRAO, and the left eye fundus was unremarkable. Immediate ocular massage, oral acetazolamide to reduce IOP, and carbon dioxide inhalation did not improve the condition. The fundus image depicted a wedge-shaped pale retina along the inferotemporal arcade sparing the fovea and extending medially till the optic nerve, more appreciable on a red-free image [Figure 1a]. Optical coherence tomography through the pale retina depicted hyperreflectivity and thickening of the inner retinal layers [Figure 1b] in comparison to the corresponding superior arcuate area of contra-lateral eye shows clearly demarcated inner retinal layers [Figure 1c].
Figure 1.
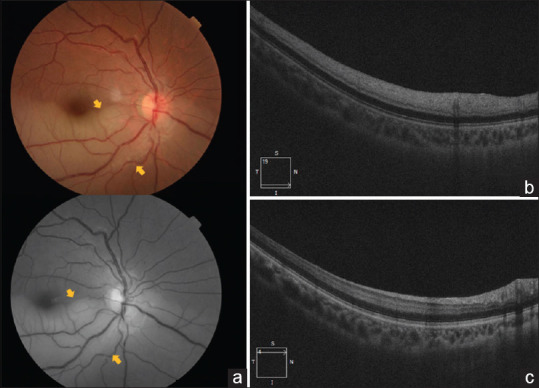
(a) Color and red-free fundus photo showing inferotemporal pale retina due to BRAO in the right eye (yellow arrows). (b) Optical coherence tomography (OCT) scan of the right eye showing hyperreflective band in the inner plexiform and inner nuclear layer and thickening of the retinal layer. (c) OCT scan of the corresponding superior arcuate area shows normal thickness and reflectivity of inner retinal layers
A gynecological and cardiology work-up was sought to establish the etiology. The secondary sexual characters, axillary and pubic hairs (Tanner Stage IV), and breasts (Tanner Stage III) were well developed for her age. On auscultation, cardiac S2 sound was loud with normal S1 sound, and a pansystolic murmur at the pulmonary area was appreciated. On two-dimensional echocardiography ASD (secundum type with left to right shunt) with a diameter of 25 mm was revealed with severe pulmonary stenosis. Pelvic imaging with transabdominal ultrasonography revealed single ectopic kidney and a pelvic cyst. Magnetic resonance imaging divulged uterovaginal aplasia [Figure 2a and b], absent right kidney and left ectopic kidney [Figure 2c]. Blood investigations revealed hemoglobin level of 16.4 g/dL with neutrophilia, borderline raised erythrocyte sedimentation rate (22 mm/1st h), normal homocysteine level (14 mg/dL), normal luteinizing hormone (3.54 mIU/mL), mildly raised follicle-stimulating hormone (11 mIU/mL), and a raised prolactin (36.07 μg/L) level. Based on clinical and imaging findings diagnosis of type II MRKH syndrome with ASD and right eye BRAO was made. In consultation with cardiology, the patient was initiated on antiplatelet and anticoagulant therapy and was advised to follow with cardiosurgery, gynecology, and general surgery for surgical management of ASD and pelvic abnormalities.
Figure 2.
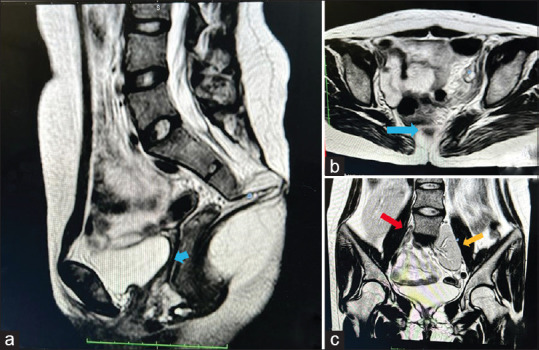
(a) Magnetic resonance imaging shows aplasia of the uterus (blue arrow) and (b) upper vagina (blue arrow), (c) absence of right kidney (red arrow) and left ectopic kidney (yellow arrow)
Discussion
This is perhaps the first case report of BRAO associated with ASD in patients with type II MRKH syndrome. MRKH syndrome is a rare disorder that affects the female reproductive system and is characterized by congenital aplasia of the uterus and the upper part (2/3) of the vagina in women showing normal development of secondary sexual characteristics, a normal 46, XX karyotype, and primary amenorrhea.[6] Isolated uterovaginal aplasia is referred to as type I (isolated) MRKH syndrome or as Rokitansky sequence, whereas incomplete aplasia associated with other malformations is generally referred to as type II MRKH syndrome or as MURCS association, and sometimes genital renal ear syndrome.[6] Type II MRKH syndrome is frequently associated with unilateral renal agenesis, hypoplasia, ectopia, spinal and vertebral abnormalities, and malformation of the facial, middle ear, and external ear structures.[6] The association of MRKH syndrome is less common with limb and heart abnormalities. Cardiac abnormalities reported with MURCS include aortopulmonary window, ASD, pulmonary valvular stenosis, and Tetralogy of Fallot.[7,8,9,10] ASD is an uncommon association of type II MRKH syndrome.[7] Retinal vascular occlusion is very rare in ASD, especially in young patients.[11] ASD is associated with paradoxical embolism and occlusive vascular events.[12] Nearly 14% of cases of ASD are complicated with paradoxical embolism, and patients with paradoxical embolism in ASD tend to be younger and have smaller defects than those with ASDs without paradoxical embolism.[12] An undiagnosed ASD may lead to vascular occlusion of vital circulations, as in our case.
A small cardiac defect (<5 mm) is usually asymptomatic, whereas defects larger than 10 mm present sooner in the third decade of life. However, our patient was asymptomatic even with a large ASD. This could be due to two reasons. One, our patient is still young to be symptomatic, and second due to the presence of severe pulmonary stenosis. When ASD coexists with pulmonary stenosis, a significant left-to-right shunting is prevented by the outflow obstruction, providing pulmonary vascular protection until adulthood.[13] Further, Bannan et al. hypothesized that right-to-left shunting through a smaller defect is facilitated by the low systemic vascular resistance in youth but as the systemic vascular resistance rises with age, the flow is curtailed, making embolism less likely in olds.[12] The embolic event may be accentuated by Valsalva maneuver though the cause of initial thrombosis remains unknown in these patients.[14] However, in our case, we could not identify any precipitating event leading to embolism.
There are no established treatments for RAO and role of ocular massage, anterior chamber paracentesis, and hyperbaric oxygen therapy remain inconclusive.[15] Our patient presented after 24 h, and these interventions were not helpful in restoring the circulation. However, proactive cardiovascular evaluation was rewarding in establishing the source of the embolism. We counseled our patient for further management to prevent any life-threatening event in the future and to deal with gynecological problems. It has been suggested that ASDs, regardless of shunt size, should either be closed or prompt antiplatelet or anticoagulant therapy should be initiated.[12] Hence, a temporal association between BRVO and type II MRKH syndrome suggests that any vascular occlusion in a young patient must be thoroughly evaluated, including a detailed systemic history.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal her identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Mason JO, 3rd, Shah AA, Vail RS, Nixon PA, Ready EL, Kimble JA. Branch retinal artery occlusion: Visual prognosis. Am J Ophthalmol. 2008;146:455–7. doi: 10.1016/j.ajo.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 2.Schmidt D, Hetzel A, Geibel-Zehender A, Schulte-Mönting J. Systemic diseases in non-inflammatory branch and central retinal artery occlusion –An overview of 416 patients. Eur J Med Res. 2007;12:595–603. [PubMed] [Google Scholar]
- 3.Ward M, Etzel J, Sauerzopf S, Crabtree G. Retinal artery occlusions and risk factors in the young. Invest Ophthalmol Vis Sci. 2021;62:3200. [Google Scholar]
- 4.Ratra D, Dhupper M. Retinal arterial occlusions in the young: Systemic associations in Indian population. Indian J Ophthalmol. 2012;60:95–100. doi: 10.4103/0301-4738.94049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greven CM, Slusher MM, Weaver RG. Retinal arterial occlusions in young adults. Am J Ophthalmol. 1995;120:776–83. doi: 10.1016/s0002-9394(14)72731-x. [DOI] [PubMed] [Google Scholar]
- 6.Morcel K, Camborieux L, Programme de Recherches Sur Les Aplasies Müllériennes. Guerrier D. Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome. Orphanet J Rare Dis. 2007;2:13. doi: 10.1186/1750-1172-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fakih MH, Williamson HO, Seymour EQ, Pai S. Concurrence of the Holt-Oram syndrome and the Rokitansky-Kuster-Hauser syndrome. A case report. J Reprod Med. 1987;32:549–50. [PubMed] [Google Scholar]
- 8.Ulrich U, Schrickel J, Dorn C, Richter O, Lewalter T, Lüderitz B, et al. Mayer-von Rokitansky-Küster-Hauser syndrome in association with a hitherto undescribed variant of the Holt-Oram syndrome with an aorto-pulmonary window. Hum Reprod. 2004;19:1201–3. doi: 10.1093/humrep/deh198. [DOI] [PubMed] [Google Scholar]
- 9.Kula S, Saygili A, Tunaoğlu FS, Olguntürk R. Mayer-Rokitansky-Küster-Hauser syndrome associated with pulmonary stenosis. Acta Paediatr. 2004;93:570–2. doi: 10.1080/08035250310023773. [DOI] [PubMed] [Google Scholar]
- 10.Gilliam ML, Shulman LP. Tetralogy of fallot, imperforate anus, and Müllerian, renal, and cervical spine (MURCS) anomalies in a 15-year-old girl. J Pediatr Adolesc Gynecol. 2002;15:231–3. doi: 10.1016/s1083-3188(02)00161-4. [DOI] [PubMed] [Google Scholar]
- 11.Lyons LJ, Yarrabolu T, Kuffel RR, Jr, Bishop JE. Juvenile central retinal artery occlusion associated with atrial septal defect. J Pediatr Ophthalmol Strabismus. 2019;56:e73–5.. doi: 10.3928/01913913-20191016-01. [DOI] [PubMed] [Google Scholar]
- 12.Bannan A, Shen R, Silvestry FE, Herrmann HC. Characteristics of adult patients with atrial septal defects presenting with paradoxical embolism. Catheter Cardiovasc Interv. 2009;74:1066–9. doi: 10.1002/ccd.22170. [DOI] [PubMed] [Google Scholar]
- 13.Medina A, de Lezo JS, Delgado A, Caballero E, Segura J, Romero M. Combined percutaneous atrial septal defect occlusion and pulmonary balloon valvuloplasty in adult patients. Tex Heart Inst J. 2000;27:216–7. [PMC free article] [PubMed] [Google Scholar]
- 14.Shoeibi N, Poorzand H, Abrishami M. Branch retinal artery occlusion in a patient with patent foramen ovale. J Ophthalmic Vis Res. 2013;8:58–61. [PMC free article] [PubMed] [Google Scholar]
- 15.Terao R, Fujino R, Ahmed T. Risk factors and treatment strategy for retinal vascular occlusive diseases. J Clin Med. 2022;11:6340. doi: 10.3390/jcm11216340. [DOI] [PMC free article] [PubMed] [Google Scholar]


