Abstract
Aims: Skin perfusion pressure (SPP) and ankle-brachial index (ABI) are useful in screening for peripheral arterial disease in patients undergoing hemodialysis (HD). We compared the prognostic abilities of the SPP and ABI in predicting the composite outcomes of mortality and atherosclerotic vascular events.
Methods: This single-center prospective cohort study enrolled 258 patients undergoing HD. The patients with SPP and ABI measurements were divided into tertiles. Log-rank tests, Cox regression analyses, and discrimination parameters were used for comparisons.
Results: Over a median follow-up period of 3.7 (1.4-5.0) years, 119 composite events were recorded. The incidence rates of composite events were 27.5, 13.3, and 9.1 per 100 person years, respectively, across the SPP tertiles (log-rank:p<0.001), and 23.2, 13.2, and 11.6 per 100 person years across the ABI tertiles (p=0.003). With the 3rd tertiles as references, the 1st tertiles of the SPP and ABI were significantly associated with the composite outcome (adjusted hazard ratio [aHR]: 2.58, 95% confidence interval [CI]: 1.57–4.23 and aHR: 1.70, 95% CI: 1.06–2.73, respectively). Adding the tertiles of the SPP to a predictive model with established risk factors significantly improved the model performance. This improvement was larger than that of the ABI in terms of net reclassification (0.330 vs. 0.275) and integrated discrimination (0.045 vs. 0.012). Furthermore, in patients with a normal ABI, the 1st SPP tertile (<71 mmHg) was significantly associated with the outcome (aHR, 1.97; 95% CI, 1.13–3.41) when compared to the 3rd tertile.
Conclusions: Even patients with a normal ABI have a poor prognosis if their SPP levels are low. SPP outperformed ABI in predicting mortality and cardiovascular outcomes in HD patients.
Keywords: Ankle-brachial index, Cardiovascular event, Hemodialysis, Mortality, Skin perfusion pressure
Introduction
Peripheral artery disease (PAD) is common in patients with end-stage renal disease (ESRD). Arterial occlusive disease is a manifestation of systemic atherosclerosis. Therefore, patients with PAD are more likely to develop cardiovascular events such as coronary artery disease (CAD) and stroke 1 - 3) . As PAD leads to a poor prognosis and quality of life, noninvasive screening methods involving the ankle-brachial index (ABI) and skin perfusion pressure (SPP) are strongly recommended for hemodialysis (HD) patients. Major cardiovascular disease societies recommend the ABI as the primary screening method for early detection and as an indication for therapeutic intervention 4 , 5) . Since blood pressure is usually higher at the ankle than at the arm, an ABI <0.9 suggests the presence of an obstructive disorder, whereas an ABI >1.4 indicates the presence of non-compressible calcified vessels 6) . In addition, several studies have reported that an abnormal ABI is a reliable marker not only for detecting PAD, but also for predicting death and cardiovascular events, independent of conventional risk factors 7 - 10) . However, ABI has some limitations as it may produce false negatives in patients with calcified arteries, especially in the HD population 11 , 12) . Thus, the prevalence of PAD is frequently underestimated when assessed using the ABI alone.
The SPP is suitable for the functional assessment of local peripheral blood flow. It is a useful alternative to the ABI in HD patients because the SPP can be assessed even in patients with severe arterial stiffness. Okamoto et al. reported that an SPP value of 50 mmHg is the cutoff value for detecting PAD, with 84.9% sensitivity and 76.9% specificity 13) . Moreover, we previously reported that low SPP is an independent risk factor for atherosclerotic vascular events (AVEs), and that an SPP of <70 mmHg is associated with high mortality and an increased risk of AVEs 14 , 15) . Few studies have directly compared the long-term prognostic abilities of SPP and ABI 16 , 17) .
Aim
This study aimed to determine whether a low SPP predicts systemic vascular events such as mortality and AVEs more accurately than ABI in HD patients.
Methods
Study Design and Population
This prospective cohort study was performed at a single outpatient dialysis center affiliated with Kariya Toyota General Hospital (Kariya, Aichi Prefecture, Japan). The study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the hospital’s institutional review board (approval number: 770). The need for informed consent was waived because of the observational nature of the study.
In total, 461 patients underwent maintenance HD at our facility between May 2013 and April 2021. Among them, 286 patients underwent measurement of both ABI and SPP within one year. Moreover, 28 patients diagnosed with PAD and those receiving therapeutic interventions were excluded (amputation, n=6; gangrene, n=10; and revascularization of the lower extremities, n=12). In total, 258 patients were included in the analysis. In addition, we performed a subgroup analysis of patients whose ABI (n=215) and SPP (n=230) values were within the normal range to determine whether low SPP or ABI was a risk factor, even in patients with normal levels.
Measurements and Classification
The SPP was measured at the soles of the feet 1 h after initiating HD treatment when the patients were in a stable and supine position. The measurements were performed using a laser Doppler probe device and a SensiLase PAD4000 Doppler Waveform Analyzer (Kaneka Medix Corp., Osaka, Japan). The lowest value for the two feet was included in the analysis of the ischemic status. The measurements were conducted by well-trained operators and were repeated in healthy volunteers. The intra-observer variance was 4.21%, the inter-observer variance was 3.55%, and the average value was 78.2±9.2 mmHg 15) . In contrast, the ABI was measured before HD treatment in the supine position, with the limbs at the level of the heart. The ABI was calculated by dividing the lowest systolic blood pressure in both ankles by the systolic blood pressure in the arm without vascular access. SPP and ABI values were measured on different days, but within one year, since our preliminary study confirmed that SPP values were stable for at least one year.
We stratified the patients according to the tertiles or quintiles of the SPP or ABI values, and compared their prognoses. Abnormal SPP and ABI were defined as <50 mmHg and <0.9 or >1.4, respectively, based on previous guidelines 5 , 13) .
Outcomes
The primary outcome was the time to the first composite endpoint event with all-cause mortality and any hospitalization for an AVE (including CAD, stroke, or PAD). The secondary outcome was time to death or an AVE. Cardiologists diagnosed CAD including acute coronary syndrome, myocardial infarction, percutaneous coronary intervention, and coronary artery bypass graft surgery. Neurologists diagnosed stroke, including atherosclerotic ischemic stroke or intracerebral hemorrhage. Cardiologists also diagnosed PAD, including vascular interventions due to lower limb ischemia (e.g., endovascular treatment, or amputation) and symptoms of critical limb ischemia (e.g., pain at rest, intractable ulcers, or gangrene). The incidence of all events was determined based on electronic medical records from May 2013 to April 2021, with a maximum follow-up period of five years.
Statistical Methods
The baseline characteristics of the study population are presented as the mean±standard deviation for normally distributed variables and the median (interquartile range) for non-normally distributed variables. The relationship between SPP and ABI was explored using a scatter plot and Pearson’s correlation coefficient. Kaplan–Meier failure curves were used to estimate the cumulative incidence of each outcome. The log-rank test was used to evaluate the differences in survival curves over the 5-year follow-up period. Based on previous studies, we collected data for 20 confounding factors that are known to be associated with the atherosclerotic risk in the HD population, 8 of which were selected as adjustment factors in the main analysis (i.e., sex, age, systolic blood pressure, prior history of AVE, diabetes, albumin, C-reactive protein, and hemoglobin) 18 , 19) . All missing values were imputed using multiple imputations with a chained equation, and 20 imputed datasets were created. Univariate and multivariate Cox proportional hazards analyses were used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs). Schoenfeld residuals were used to test the assumption of proportional hazards. Furthermore, we compared model performances by calculating Harrel’s C-index, net reclassification improvement (NRI), and integrated discrimination improvement (IDI). This assessed whether adding SPP or ABI tertiles to a base model with 8 established risk factors improved predictability. The incidence rates of composite events across SPP and ABI levels in patients with normal ABI (215 patients) and SPP (230 patients) were estimated using Poisson regression models with restricted cubic splines. P values of <0.05 were considered to indicate statistical significance. All statistical analyses were performed using Stata SE/16.1 (Stata Corp., College Station, TX, USA).
Results
Predictive Values of SPP and ABI in the Entire Cohort
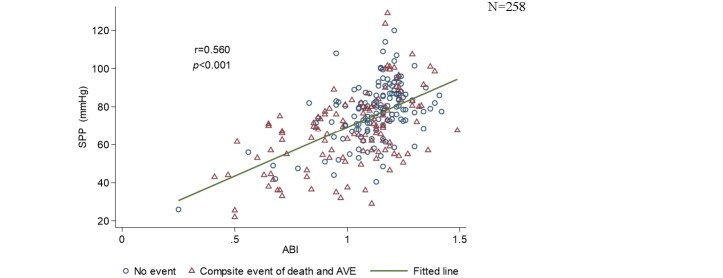
The baseline characteristics of the study population are presented in Table 1 . Of the 258 participants, 165 (64.0%) were men, with a median age of 70.8 years (62.3–76.0) and a median HD duration of 1.8 years (0.1–5.7). One hundred sixty-one (62.4%) patients underwent SPP and ABI evaluations within 3 months, and the median absolute day gap between these measurements was 63 (19-166) days. The mean SPP and median ABI were 72.9±18.2 mmHg and 1.13 (0.99–1.20), respectively. The cutoff values of the tertiles were 67 and 81 mmHg for SPP and 1.06 and 1.18 for ABI. A scatterplot showing the relationship between the SPP and ABI values is presented in Supplemental Fig.1 with a Pearson’s correlation coefficient of 0.56 (p<0.001).
Table 1. Baseline characteristics of the study population.
| Characteristics | Overall | SPP | ABI | ||||
|---|---|---|---|---|---|---|---|
| N= 258 |
T1 n= 86 |
T2 n= 89 |
T3 n= 83 |
T1 n= 87 |
T2 n= 89 |
T3 n= 82 |
|
| SPP, mmHg | 72.9 (18.2) | 52.8 (11.2) | 74.7 (4.1) | 91.9 (10.0) | 61.5 (17.0) | 74.6 (15.7) | 83.2 (15.1) |
| ABI | 1.13 (0.99, 1.20) | 1.00 (0.73, 1.12) | 1.12 (1.04, 1.18) | 1.19 (1.13, 1.23) | 0.90 (0.71, 0.99) | 1.13 (1.09, 1.16) | 1.23 (1.20, 1.29) |
| Age, years | 70.8 (62.3, 76.0) | 73.4 (63.3, 77.9) | 68.8 (63.1, 73.7) | 68.2 (59.9, 75.8) | 71.6 (63.5, 77.8) | 71.2 (59.6, 75.8) | 68.1 (61.3, 73.7) |
| Male sex, n (%) | 165 (64.0%) | 55 (64.0%) | 58 (65.2%) | 52 (62.7%) | 59 (67.8%) | 49 (55.1%) | 57 (69.5%) |
| Duration of dialysis, years | 1.8 (0.1, 5.7) | 2.7 (0.2, 6.8) | 1.9 (0.2, 5.6) | 0.8 (0.1, 4.6) | 2.6 (0.1, 7.9) | 1.5 (0.1, 5.3) | 1.7 (0.1, 4.1) |
| Body mass index, kg/m2 | 21.9 (19.9, 24.5) | 21.4 (19.6, 24.0) | 22.6 (20.8, 25.9) | 21.7 (19.6, 24.1) | 21.7 (20.1, 24.8) | 21.9 (19.7, 24.3) | 22.2 (19.9, 24.9) |
| Systolic blood pressure, mmHg | 158 (25) | 152 (28) | 160 (26) | 161 (20) | 158 (28) | 156 (21) | 158 (27) |
| Current smoking, n (%) | 34 (13.2%) | 13 (15.1%) | 7 ( 7.9%) | 14 (16.9%) | 8 ( 9.2%) | 13 (14.6%) | 13 (15.9%) |
| Prior history of | |||||||
| Any AVE, n (%) | 80 (31.0%) | 35 (40.7%) | 27 (30.3%) | 18 (21.7%) | 36 (41.4%) | 26 (29.2%) | 18 (22.0%) |
| CAD, n (%) | 35 (13.6%) | 19 (22.1%) | 10 (11.2%) | 6 ( 7.2%) | 20 (23.0%) | 什(12.4%) | 4 ( 4.9%) |
| Stroke, n (%) | 51 (19.8%) | 17 (19.8%) | 20 (22.5%) | 14 (16.9%) | 18 (20.7%) | 19 (21.3%) | 14 (17.1%) |
| Comorbidities | |||||||
| Diabetes mellitus, n (%) | 121 (46.9%) | 45 (52.3%) | 43 (48.3%) | 33 (39.8%) | 52 (59.8%) | 35 (39.3%) | 34 (41.5%) |
| Hypertension, n (%) | 167 (64.7%) | 44 (51.2%) | 60 (67.4%) | 63 (75.9%) | 57 (65.5%) | 57 (64.0%) | 53 (64.6%) |
| Laboratory data | |||||||
| Urea nitrogen, mg/dl | 59.8 (13.7) | 58.9 (13.2) | 57.9 (13.4) | 62.9 (14.1) | 59.3 (13.3) | 58.9 (13.8) | 61.5 (13.9) |
| Creatinine, mg/dl | 9.7 (2.7) | 9.3 (2.6) | 9.9 (2.5) | 9.8 (2.9) | 9.7 (2.6) | 9.6 (2.6) | 9.9 (2.8) |
| Albumin, g/dl | 3.7 (3.4, 4.0) | 3.7 (3.4, 3.9) | 3.7 (3.5, 4.0) | 3.7 (3.4, 3.9) | 3.6 (3.3, 4.0) | 3.7 (3.5, 4.0) | 3.7 (3.5, 3.9) |
| C-reactive protein, mg/dl | 0.13 (0.05, 0.47) | 0.19 (0.07, 0.63) | 0.13 (0.05, 0.41) | 0.07 (0.04, 0.35) | 0.18 (0.07 , 0.57) | 0.13 (0.06, 0.54) | 0.08 (0.04, 0.21) |
| Albumin-adjusted Ca, mg/dl | 9.0 (0.6) | 9.0 (0.7) | 9.0 (0.6) | 8.9 (0.6) | 9.0 (0.7) | 9.0 (0.6) | 8.9 (0.6) |
| Phosphate, mg/dl | 5.1 (1.3) | 4.9 (1.3) | 5.1 (1.2) | 5.2 (1.4) | 5.1 (1.3) | 4.9 (1.3) | 5.3 (1.3) |
| Intact PTH, pg/ml | 206 (132, 289) | 222 (135, 284) | 199 (132, 258) | 198 (130, 316) | 199 (129, 250) | 198 (132, 289) | 231 (133, 318) |
| Hemoglobin, g/dl | 10.4 (0.8) | 10.3 (0.8) | 10.5 (0.8) | 10.4 (0.9) | 10.4 (0.8) | 10.5 (0.8) | 10.3 (0.8) |
| Total cholesterol, mg/dl | 156 (135, 178) | 146 (129, 169) | 161 (139, 181) | 159 (140, 190) | 151 (126, 174) | 156 (133, 176) | 159 (145, 190) |
| HDL cholesterol, mg/dl | 50 (40, 60) | 48 (40, 58) | 48 (38, 59) | 56 (42, 65) | 46 (38, 58) | 50 (40, 60) | 50 (40, 63) |
Values for continuous data are given as mean±standard deviation or median (25-75th interquartile range) and those for categorical data, as count (percentage). The cut-off points for tertile divisions were 67 mmHg and 81 mmHg for SPP and 1.06 and 1.18 for ABI.
SPP, skin perfussion pressure; ABI, ankle-brachial index; Tl, 1st tertile; T2, 2nd tertile; T3, 3rd tertile; N, number of all patients; n, number of patients in each specific group; AVE, atherosclerotic vascular event; CAD, coronary artery disease; Ca, calcium; PTH, parathyroid hormone; HDL, high-density lipoprotein.
Supplemental Fig.1. Correlation between SPP and ABI values.
The scatterplot shows the relationship between SPP and ABI values. Pearson's correlation coefficient was calculated to be 0.56 (p<0.001). Blue circles represent patients who did not experience any composite event of death and AVE, whereas red triangles represent those who did. We found that the blue circles were concentrated where both SPP and ABI were high.
SPP, skin perfusion pressure; ABI, ankle-brachial index; AVE, atherosclerotic vascular event.
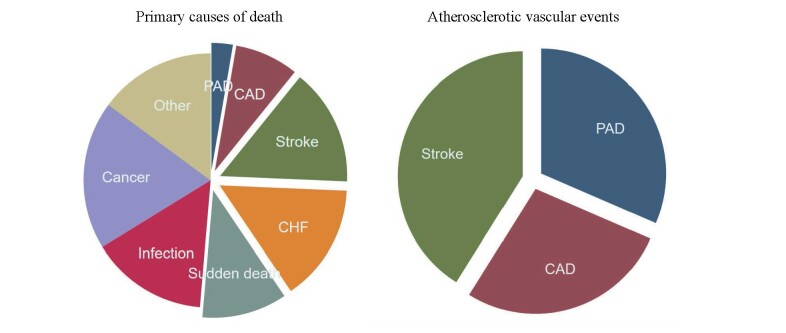
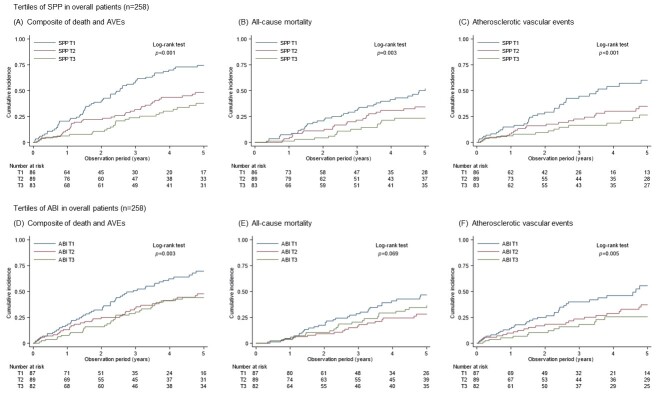
During the follow-up period [median, 3.7 years (1.4–5.0) years], 119 composite events occurred, 74 patients died, and 73 AVEs occurred ( Supplemental Table 1 ) . Across the tertiles of SPP, the incidence rates of composite events during the 5 years were 27.5, 13.3, and 9.1 per 100 person-years (PY), respectively, (log-rank: p<0.001); those of mortality were 13.4, 8.1, and 5.1 per 100 PY (p=0.003); and those of AVEs were 18.3, 8.8, and 6.0 per 100 PY (p<0.001) [ Fig.1 (A), (B), and (C) ] . In the ABI group, the rates of composite events during the 5 years were 23.2, 13.2, and 11.6 per 100 PY (p=0.003), respectively, those of mortality were 11.9, 6.3, and 8.5 per 100 PY (p=0.069), and those of AVE were 16.0, 9.3, and 6.2 per 100 PY (p=0.005) [ Fig.1 (D), (E), and (F) ] . The low tertiles of SPP and ABI were associated with a significantly higher incidence of events.
Supplemental Table 1. Description of the primary causes of death and the occurrence of AVEs.
| Primary causes of death | Number of patients (%) | Atherosclerotic vascular events | Number of patients (%) | ||
|---|---|---|---|---|---|
| Peripheral artery disease | 2 | (2.7) | Peripheral artery disease | 23 | (31.5) |
| Coronary artery disease | 6 | (8.1) | Coronary artery disease | 20 | (27.4) |
| Stroke | 11 | (14.9) | Stroke | 30 | (41.1) |
| Congestive heart failure | 11 | (14.9) | |||
| Sudden unexpected death | 8 | (10.8) | |||
| Infection | 11 | (14.9) | |||
| Cancer | 14 | (18.9) | |||
| Other | 11 | (14.9) | |||
| total | 74 | (100) | total | 73 | (100) |
We presented findings on the primary causes of death and the occurrence of AVEs. Cardiovascular events accounted for more than half of all cases of mortality. Additionally, the most prevalent AVE was stroke.
AVE, atherosclerotic vascular event; PAD, peripheral artery disease; CAD, coronary artery disease; CHF, congestive heart failure.
Fig.1. Cumulative incidence of outcomes stratified by SPP and ABI tertiles in all patients.
Kaplan–Meier failure curves show the cumulative incidence of outcomes. In terms of the composite event at the 5-year time point, the tertiles were 0.74, 0.48, and 0.38 for SPP T1, T2, and T3, respectively (p<0.001) (A), and 0.70, 0.48, and 0.44 for ABI T1, T2, and T3 (p=0.003) (D). For all-cause death, the tertiles were 0.52, 0.34, and 0.23, respectively for SPP (p=0.003) (B), and 0.47, 0.28, and 0.36 for ABI (p=0.069) (E). For AVEs, the tertiles were 0.60, 0.35, and 0.27, respectively, for SPP (p<0.001) (C) and 0.56, 0.37, and 0.26 for ABI (p=0.005) (F).
SPP, skin perfusion pressure; ABI, ankle-brachial index; AVEs, atherosclerotic vascular events; T1, 1st tertile; T2, 2nd tertile; T3, 3rd tertile.
Table 2 presents the results of the Cox proportional hazards models for each endpoint in the univariate and multivariate analyses of the 258 patients. As a result of the composite event, with the 3rd tertile (T3) of SPP as the reference value, the adjusted HR (aHR) was 2.58 (95% CI: 1.57–4.23) for the 1st tertile (T1) and 1.50 (95% CI: 0.89–2.53) for the 2nd tertile (T2). Regarding the ABI, the aHR was 1.70 (95% CI: 1.06–2.73) for T1 and 1.36 (95% CI: 0.82–2.25) for T2. Adjustment for 20 literature-based covariates did not substantially alter the results ( Supplemental Table 2 ) . Similarly, the HRs for mortality and AVEs are shown; the effect sizes for SPP were larger than those for ABI. Moreover, we determined the aHR of composite outcomes across quintiles using multivariate analyses, as shown in Fig.2 . With the 4th quintile (Q4) as the reference value, the aHR for SPP increased stepwise up to the 1st quintile (Q1), whereas that for ABI was not significantly different from the 2nd through 5th quintiles (Q2–Q5).
Table 2. Hazard ratios by SPP and ABI tertiles in all patients.
| Outcomes | Tertile | Overall patients (N = 258) | ||||||
|---|---|---|---|---|---|---|---|---|
| SPP | ABI | |||||||
| HRs | 95% CI | p value | HRs | 95% CI | p value | |||
| Composite event | Non-adjusted | T1 | 3.05 | (1.90, 4.89) | <0.001 | 1.99 | (1.28, 3.11) | 0.002 |
| T2 | 1.46 | (0.88, 2.43) | 0.141 | 1.14 | (0.70, 1.85) | 0.595 | ||
| T3 | ref. | ref. | ||||||
| Adjusted | T1 | 2.58 | (1.57, 4.23) | <0.001 | 1.70 | (1.06, 2.73) | 0.028 | |
| T2 | 1.50 | (0.89, 2.53) | 0.129 | 1.36 | (0.82, 2.25) | 0.240 | ||
| T3 | ref. | ref. | ||||||
| All-cause mortality | Non-adjusted | T1 | 2.70 | (1.45, 5.00) | 0.002 | 1.40 | (0.82, 2.41) | 0.218 |
| T2 | 1.62 | (0.84, 3.14) | 0.149 | 0.74 | (0.40, 1.36) | 0.326 | ||
| T3 | ref. | ref. | ||||||
| Adjusted | T1 | 1.79 | (0.93, 3.45) | 0.084 | 1.07 | (0.59, 1.93) | 0.822 | |
| T2 | 1.52 | (0.77, 3.03) | 0.230 | 0.74 | (0.39, 1.42) | 0.364 | ||
| T3 | ref. | ref. | ||||||
| Atherosclerotic vascular events | Non-adjusted | T1 | 3.00 | (1.63, 5.51) | <0.001 | 2.59 | (1.39, 4.81) | 0.003 |
| T2 | 1.45 | (0.76, 2.78) | 0.262 | 1.5 | (0.78, 2.91) | 0.226 | ||
| T3 | ref. | ref. | ||||||
| Adjusted | T1 | 2.82 | (1.49, 5.33) | 0.001 | 2.38 | (1.24, 4.56) | 0.009 | |
| T2 | 1.44 | (0.74, 2.83) | 0.287 | 1.79 | (0.90, 3.58) | 0.097 | ||
| T3 | ref. | ref. | ||||||
Cox proportional hazard models were adjusted for eight covariates: sex, age, systolic blood pressure, prior history of AVE and diabetes, albumin, C-reactive protein, and hemoglobin levels. The HRs are presented in the 3rd tertile as a reference. The effect sizes for SPP are larger than those for ABI.
SPP, skin perfusion pressure; ABI, ankle-brachial index; HR, hazard ratio; CI, confidence interval; T1, 1st tertile; T2, 2nd tertile; T3, 3rd tertile; ref, reference; BP, blood pressure; AVE, atherosclerotic vascular event.
Supplemental Table 2. Hazard ratios for composite events by SPP and ABI tertiles in all patients.
| Tertile | SPP | ABI | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adjusted for 8 factors | Adjusted for 20 factors | Adjusted for 8 factors | Adjusted for 20 factors | |||||||||
| HR | 95% CI | p value | HR | 95% CI | p value | HR | 95% CI | p value | HR | 95% CI | p value | |
| T1 | 2.58 | (1.57, 4.23) | <0.001 | 2.82 | (1.62, 4.92) | <0.001 | 1.70 | (1.06, 2.74) | 0.028 | 1.65 | (1.00, 2.74) | 0.052 |
| T2 | 1.50 | (0.89, 2.54) | 0.129 | 1.56 | (0.89, 2.73) | 0.122 | 1.36 | (0.82, 2.25) | 0.240 | 1.36 | (0.80, 2.31) | 0.253 |
| T3 | ref. | ref. | ref. | ref. | ||||||||
| Age | 1.03 | (1.01, 1.04) | 0.003 | 1.02 | (1.00, 1.04) | 0.069 | 1.03 | (1.01, 1.05) | 0.003 | 1.02 | (1.00, 1.04) | 0.059 |
| Male sex | 1.26 | (0.82, 1.92) | 0.289 | 1.40 | (0.76, 2.57) | 0.281 | 1.32 | (0.85, 2.04) | 0.217 | 1.53 | (0.82, 2.85) | 0.180 |
| Body mass index | 0.96 | (0.89, 1.03) | 0.212 | 0.97 | (0.91, 1.04) | 0.428 | ||||||
| Activities of Daily Living | 1.08 | (0.74, 1.58) | 0.707 | 1.18 | (0.81, 1.73) | 0.389 | ||||||
| Current smoking | 1.03 | (0.55, 1.94) | 0.932 | 1.23 | (0.67, 2.27) | 0.505 | ||||||
| Systolic blood pressure | 1.00 | (1.00, 1.01) | 0.436 | 1.00 | (0.99, 1.01) | 0.736 | 1.00 | (0.99, 1.01) | 0.776 | 1.00 | (0.99, 1.01) | 0.854 |
| Prior history of AVE | 1.16 | (0.79, 1.72) | 0.443 | 1.08 | (0.71, 1.67) | 0.715 | 1.20 | (0.81, 1.78) | 0.367 | 1.10 | (0.72, 1.70) | 0.653 |
| Diabetes mellitus | 1.20 | (0.81, 1.77) | 0.36 | 1.30 | (0.82, 2.06) | 0.266 | 1.14 | (0.77, 1.69) | 0.506 | 1.27 | (0.82, 1.99) | 0.287 |
| Albumin | 0.41 | (0.25, 0.66) | <0.001 | 0.41 | (0.24, 0.70) | 0.001 | 0.43 | (0.27, 0.70) | 0.001 | 0.44 | (0.26, 0.74) | 0.002 |
| C-reactive protein | 1.09 | (0.96, 1.24) | 0.169 | 1.15 | (0.99, 1.33) | 0.077 | 1.12 | (0.99, 1.26) | 0.064 | 1.13 | (0.97, 1.31) | 0.123 |
| Hemoglobin | 0.78 | (0.62, 0.99) | 0.044 | 0.72 | (0.54, 0.95) | 0.020 | 0.76 | (0.60, 0.96) | 0.022 | 0.72 | (0.55, 0.95) | 0.019 |
| Erythropoietin resistance index | 0.99 | (0.97, 1.02) | 0.671 | 1.00 | (0.97, 1.03) | 0.886 | ||||||
| Calcium-phosphate product | 1.01 | (0.99, 1.03) | 0.222 | 1.00 | (0.99, 1.02) | 0.702 | ||||||
| Intact parathyroid hormone | 1.00 | (1.00, 1.00) | 0.850 | 1.00 | (1.00, 1.00) | 0.936 | ||||||
| Antihypertensive drugs | 1.06 | (0.66, 1.70) | 0.814 | 0.90 | (0.57, 1.43) | 0.651 | ||||||
| Antilipemic drugs | 1.11 | (0.65, 1.89) | 0.708 | 1.11 | (0.64, 1.91) | 0.714 | ||||||
| Calcium-containing phosphate binders | 0.9 | (0.49, 1.63) | 0.721 | 0.87 | (0.50, 1.51) | 0.618 | ||||||
| Dialysis time per session | 1.00 | (0.98, 1.01) | 0.699 | 1.00 | (0.98, 1.02) | 0.716 | ||||||
| Quantity of blood flow in treatment | 1.00 | (0.99, 1.02) | 0.643 | 1.00 | (0.99, 1.02) | 0.669 | ||||||
| Single pool Kt/V urea nitrogen | 1.40 | (0.30, 6.56) | 0.666 | 1.62 | (0.37, 6.99) | 0.520 | ||||||
Cox proportional hazard models were adjusted for 20 literature-based covariates: age, sex, body mass index, activities of daily living, current smoking, systolic blood pressure, prior history of AVE and diabetes, laboratory data of albumin, C-reactive protein, hemoglobin, calcium-phosphate product, intact parathyroid hormone, erythropoietin resistance index, single-pool Kt/V urea nitrogen, medication status of antihypertensive drugs, antilipemic drugs, calcium-containing phosphate binders, dialysis prescription of therapy time per session, and quantity of blood flow per minute. Of these 20 factors, we selected eight confounders for assessing model performance (Table 3) or other statistical analyses. We confirmed that the HRs were consistent across models, adjusting for 8 or all 20 variables.
SPP, skin perfusion pressure; ABI, ankle-brachial index; HR, hazard ratio; CI, confidence interval; T1, 1st tertile; T2, 2nd tertile; T3, 3rd tertile; AVE, atherosclerotic vascular event.
Fig.2. Hazard ratios for composite events across the SPP and ABI quintiles in all patients.
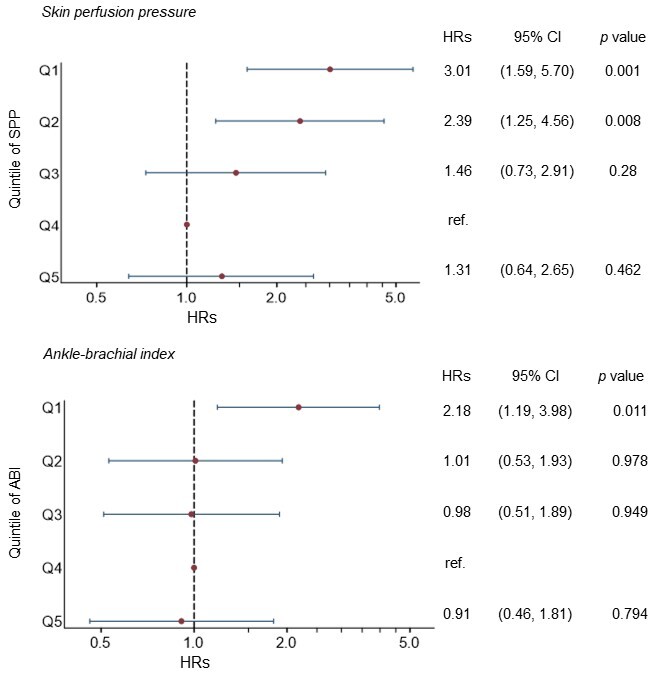
Forest plots show the HRs and 95% CIs for each quintile group. The HRs are presented in the 4th quintile as a reference. The Cox proportional hazard models were adjusted for eight covariates: sex, age, systolic blood pressure, history of AVEs and diabetes, albumin, C-reactive protein, and hemoglobin.
SPP, skin perfusion pressure; ABI, ankle-brachial index; HR, hazard ratio; CI, confidence interval; ref, reference; Q1, 1st quintile; Q2, 2nd quintile; Q3, 3rd quintile; Q4, 4th quintile; Q5, 5th quintile; AVE, atherosclerotic vascular event.
Table 3 presents the discrimination parameters of the prediction models for the composite endpoints. The addition of SPP or ABI tertiles to the basic model with established risk factors (SPP or ABI model) improved the model performance. Notably, the SPP model showed greater improvement than the ABI model in terms of Harrell’s C-index (0.721 vs. 0.703), NRI (0.330 vs. 0.275), and IDI (0.045 vs. 0.012). Furthermore, the addition of the SPP to the ABI model significantly improved the NRI (0.359, p=0.004) and IDI (0.033, p=0.003), whereas the addition of the ABI to the SPP model did not improve them (NRI: 0.109, p=0.382, and IDI: 0.001, p=0.712). These model performance comparisons clarified that the SPP outperformed the ABI in predicting mortality and cardiovascular outcomes in the HD population.
Table 3. Discrimination parameters of four models for predicting the composite outcome.
| Harrell ’s C | 95%CI | NRI | p value | IDI | p value | |||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Established risk factors | 0.700 | (0.656, 0.744) | Model 1 | ref. | ref. | ref. | ref. |
| Model 2 | Model 1 + ABI | 0.703 | (0.658, 0.749) | Model 2 vs. Model 1 | 0.275 | 0.028 | 0.012 | 0.073 |
| Model 3 | Model 1 + SPP | 0.721 | (0.677, 0.764) | Model 3 vs. Model 1 | 0.330 | 0.008 | 0.045 | <0.001 |
| Model 4 | Model 1 + ABI + SPP | 0.721 | (0.677, 0.765) | Model 4 vs. Model 2 | 0.359 | 0.004 | 0.033 | 0.003 |
| Model 4 vs. Model 3 | 0.109 | 0.382 | 0.001 | 0.712 | ||||
We established risk prediction models for the composite event of death and AVEs. Model 1 includes the eight risk factors identified as in Table 2. In Models 2--4, the factors of SPP and/or ABI tertiles are added to Model 1.
Harrell ’s C, Harrell ’s C-statistic; NRI, net reclassification improvement; IDI, integrated discrimination improvement; CI, confidence interval; ref., reference; ABI, ankle-brachial index; SPP, skin perfusion pressure; AVEs, atherosclerotic vascular events.
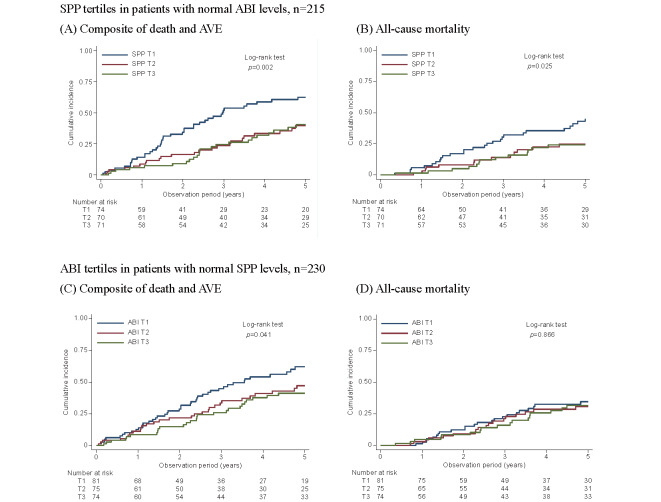
Subgroup Analysis of Patients with Normal ABI and SPP Levels
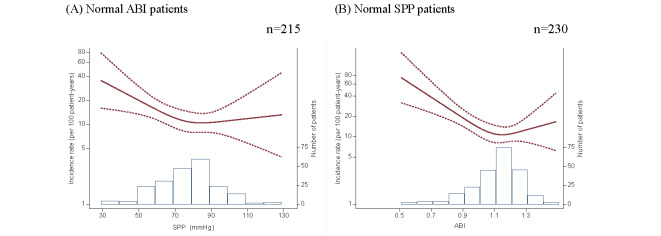
We performed subgroup analyses of patients with normal ABI values (n=215) and normal SPP values (n=230), and divided them into tertiles. The cutoff values of the SPP were 71 and 83 mmHg in a normal ABI group, while those of the ABI were 1.06 and 1.18 in a normal SPP group. Supplemental Table 3 shows the characteristics of the patient backgrounds of the normal ABI group, comparing SPP T1 to SPP T2+T3. Significant differences were observed in old age, low systolic blood pressure, prevalence of CAD and diabetes, and low cholesterol. Across the SPP tertiles, the incidence rates of composite events were 20.3, 9.9, and 9.8 per 100 PY (log-rank: p=0.002), and those of mortality were 11.2, 5.5, and 5.4 per 100 PY (p=0.025). Across the ABI tertiles, the incidence rates of composite events were 19.0, 12.7, and 10.5 per 100 PY (log-rank: p=0.041), and those of mortality were 8.4, 7.2, and 7.2, respectively, per 100 PY (p=0.866) ( Supplemental Fig.2 ) . These findings show that the event rate was significantly higher in patients with SPP T1, even if their ABI was within the normal range. Similarly, in the normal SPP group, ABI T1 was associated with a higher incidence of composite events; however, this was not the case for all-cause mortality. Cox proportional hazards models of composite events showed an aHR of 1.97 (95% CI: 1.13–3.41) for SPP T1 relative to T3 and 1.69 (95% CI: .02–2.81) for ABI T1 relative to T3 ( Supplemental Table 4 ) . Again, the effect size of SPP T1 was larger than that of ABI T1. Supplemental Fig.3 shows that patients with SPP <70 mmHg had a higher risk of composite events among normal ABI patients, and that patients with ABI <1.0 were also at a higher risk among normal SPP patients. These results indicate that additional SPP and ABI measurements are useful tools for further risk stratification, even in patients with normal ABI and SPP levels.
Supplemental Table 3. Baseline characteristics of patients with normal ABIs in a subgroup analysis.
| Characteristics | Overall N = 215 | SPP T1 n =74 | SPP T2 + T3 n =141 | p value |
|---|---|---|---|---|
| SPP, mmHg | 76.4 (16.5) | 58.9 (9.8) | 85.6 (10.9) | <0.001* |
| Age, years | 70.1 (60.8, 76.0) | 73.6 (61.6, 79.2) | 67.6 (60.6, 73.2) | 0.004* |
| Male sex, n (%) | 138 (64.2%) | 51 (68.9%) | 87 (61.7%) | 0.290 |
| Duration of dialysis, years | 1.6 (0.1, 5.4) | 1.9 (0.2, 5.7) | 1.2 (0.1, 5.0) | 0.250 |
| Body mass index, kg/m² | 21.9 (19.7, 24.6) | 21.6 (19.4, 25.0) | 22.1 (20.0, 24.4) | 0.690 |
| Systolic blood pressure, mmHg | 157 (24) | 152 (26) | 160 (22) | 0.028* |
| Current smoking, n (%) | 29 (13.5%) | 10 (13.5%) | 19 (13.5%) | 0.990 |
| Prior history of | ||||
| Any AVE, n (%) | 59 (27.4%) | 28 (37.8%) | 31 (22.0%) | 0.013* |
| CAD, n (%) | 22 (10.2%) | 13 (17.6%) | 9 (6.4%) | 0.010* |
| Stroke, n (%) | 42 (19.5%) | 17 (23.0%) | 25 (17.7%) | 0.360 |
| Comorbidities | ||||
| Diabetes mellitus, n (%) | 96 (44.7%) | 40 (54.1%) | 56 (39.7%) | 0.045* |
| Hypertension, n (%) | 145 (67.4%) | 44 (59.5%) | 101 (71.6%) | 0.070 |
| Laboratory data | ||||
| Urea nitrogen, mg/dL | 59.9 (13.9) | 58.9 (13.5) | 60.4 (14.1) | 0.450 |
| Creatinine, mg/dL | 9.7 (2.7) | 9.6 (2.5) | 9.8 (2.8) | 0.590 |
| Albumin, g/dL | 3.7 (3.4, 4.0) | 3.7 (3.4, 4.0) | 3.7 (3.5, 3.9) | 0.900 |
| C-reactive protein | 0.12 (0.05, 0.41) | 0.13 (0.07, 0.43) | 0.08 (0.04, 0.40) | 0.066 |
| Albumin-adjusted Ca, mg/dL | 9.0 (0.6) | 9.0 (0.7) | 8.9 (0.6) | 0.450 |
| Phosphate, mg/dL | 5.0 (1.3) | 4.9 (1.3) | 5.1 (1.3) | 0.370 |
| Intact PTH, pg/mL | 206 (129, 296) | 207 (118, 274) | 206 (132, 300) | 0.530 |
| Hemoglobin, g/dL | 10.5 (0.8) | 10.4 (0.8) | 10.5 (0.8) | 0.430 |
| Total cholesterol, mg/dL | 156 (135, 179) | 144 (130, 161) | 163 (144, 190) | <0.001* |
| HDL cholesterol, mg/dL | 49 (40, 61) | 44 (39, 56) | 53 (40, 65) | 0.020* |
In patients with normal ABI levels, the cut-off points of SPP tertiles were 71 and 83 mmHg. Because those with SPP T1 had a significantly higher event rate, the patients’ background characteristics were compared with those of SPP T1 with T2+T3. Differences were assessed using the unpaired Student’s t-test, Mann–Whitney test, or chi-square test, as needed. *denotes a significance level of p<0.05.
ABI, ankle-brachial index; T1, 1st tertile; T2, 2nd tertile; T3, 3rd tertile; N, number of all patients; n, number of patients in a specific group; SPP, skin perfusion pressure; AVE, atherosclerotic vascular event; CAD, coronary artery disease; Ca, calcium; PTH, parathyroid hormone; HDL, high- density lipoprotein.
Supplemental Fig.2. Cumulative incidence of the composite event and mortality stratified by SPP and ABI tertiles in patients with normal ABI and SPP.
The cut-off points are 71 and 83 mmHg for SPP and 1.06 and 1.18 for ABI. In 215 patients with normal ABI levels, the cumulative incidences for the composite events during 5 years were 0.63, 0.40, and 0.41 with p=0.002 (A), and those for death were 0.45, 0.25, and 0.24 with p=0.025 for SPP T1, T2, and T3, respectively (B). In 230 patients with normal SPP levels, those for composite events were 0.62, 0.47, and 0.41 with p=0.041 (C), and those for death were 0.35, 0.31, and 0.32 with p=0.866 for ABI T1, T2, and T3, respectively (D).
SPP, skin perfusion pressure; ABI, ankle-brachial index; AVEs, atherosclerotic vascular events; T1, 1st tertile; T2, 2nd tertile; T3, 3rd tertile.
Supplemental Table 4. Hazard ratios for the composite event and mortality by SPP and ABI tertiles in subgroup analyses of normal ABI and SPP levels.
| Outcome | Tertile | (A) Normal ABI patients | (B) Normal SPP patients | |||||
|---|---|---|---|---|---|---|---|---|
| SPP HR | 95% CI | p value | ABI HR | 95% CI | p value | |||
| Composite event | Non-adjusted | T1 | 2.11 | (1.26, 3.52) | 0.004 | 1.80 | (1.10, 2.94) | 0.018 |
| T2 | 1.02 | (0.57, 1.81) | 0.955 | 1.20 | (0.71, 2.05) | 0.484 | ||
| T3 | ref. | ref. | ||||||
| Adjusted | T1 | 1.97 | (1.13, 3.41) | 0.016 | 1.69 | (1.02, 2.81) | 0.043 | |
| T2 | 1.08 | (0.59, 1.96) | 0.791 | 1.39 | (0.79, 2.43) | 0.255 | ||
| T3 | ref. | ref. | ||||||
| All-cause mortality | Non-adjusted | T1 | 2.12 | (1.10, 4.12) | 0.026 | 1.15 | (0.61, 2.15) | 0.663 |
| T2 | 1.05 | (0.49, 2.26) | 0.905 | 0.99 | (0.51, 1.79) | 0.980 | ||
| T3 | ref. | ref. | ||||||
| Adjusted | T1 | 1.53 | (0.73, 3.21) | 0.255 | 0.92 | (0.47, 1.79) | 0.813 | |
| T2 | 1.16 | (0.52, 2.57) | 0.723 | 0.97 | (0.47, 1.99) | 0.939 | ||
| T3 | ref | ref. | ||||||
We performed a subgroup analysis using Cox proportional hazards models to determine whether low SPP or ABI was at risk in patients with normal ABI (A) or SPP (B) levels. SPP T1 and ABI T1 were risk factors for composite outcomes, even in patients with normal ABIs and SPPs; however, the effect size of SPP T1 was higher than that of ABI T1.
SPP, skin perfusion pressure; ABI, ankle-brachial index; aHR, adjusted hazard ratio; CI, confidence interval; T1, 1st tertile; T2, 2nd tertile; T3, 3rd tertile; ref, reference
Supplemental Fig.3. The incidence rate of the composite event against SPP and ABI levels in patients with normal ABI and SPP.
Incidence rates were analyzed via Poisson regression adjusted for eight risk factors, as shown in Table 2, and presented using a restricted cubic spline model. The dashed lines show 95% CIs. The number of patients in the histogram is presented in the second axis. These rates were explored across SPP values in patients with a normal ABI (A) and across ABI values in patients with a normal SPP (B). Lower SPP and ABI levels were associated with a higher risk, even if ABI or SPP was within the normal range.
SPP, skin perfusion pressure; ABI, ankle-brachial index; CI, confidence interval
Discussion
We investigated the long-term prognostic ability of SPP and ABI to predict mortality and AVEs in patients undergoing HD. The main findings of this study are as follows: First, low SPP and ABI values were independently associated with a high incidence of death and AVEs. This finding could improve the model performance in predicting the composite outcome beyond the established risk factors. Second, the SPP model outperformed the ABI model in terms of Harrell’s C-index, NRI, and IDI. Third, as many as 83% (215/258) of the patients had a normal ABI, and the lowest tertile of SPP (T1) was associated with a poor prognosis. For these reasons, we suggest that physicians assess the SPP as the primary screening method in clinical practice, not only for PAD but also for prognostication. The ABI should be evaluated secondarily to improve screening accuracy for patients with normal SPP values.
Worldwide, measurement of the ABI is an established screening method for the evaluation of atherosclerosis. Several investigators have reported it as an independent prognostic factor in patients with and without renal dysfunction 7 - 10) . Regarding SPP, few investigators have described the relationship between atherosclerosis and mortality only over a limited observation period in patients with ESRD. Hatakeyama et al. reported the 2-year prognosis 16) , whereas our follow-up period was 5 years. Otani et al. showed associations between ABI and SPP and mortality, whereas we assessed the atherosclerotic vascular risk 17) . Furthermore, our previous studies have revealed that a low SPP is related to a poor prognosis and the incidence of AVEs, and that the cutoff value for an increased risk is approximately 70 mmHg 14 , 15) . To the best of our knowledge, this study is the first report to directly compare the ABI and SPP while describing the long-term prognosis and cardiovascular risk.
ABI measurements still have several limitations that make them less sensitive in the HD population than in the general population 20 , 21) . The most relevant finding of our study was that the SPP could compensate for these shortcomings of the ABI in a population with severe arterial calcification. It should be noted that the SPP enables a more accurate assessment of the risk of cardiovascular events in clinical practice in comparison to the ABI even when the study population includes patients with normal ABI values. A low SPP value with a normal ABI reflects older age, a reduced cardiac function, and the prevalence of diabetes ( Supplemental Table 3 ) , all of which are commonly recognized as atherosclerotic promoters in patients with ESRD. Therefore, the SPP may be more suitable than the ABI as a routine screening parameter in HD practice. In addition, the ABI should be evaluated secondarily for patients whose SPP values are normal, because ABI also provides further risk classification ( Supplemental Table 4 and Supplemental Fig.3 ) .
We considered why the assessment of the SPP was superior to that of the ABI. The SPP is the pressure required to restore microcirculatory blood flow after the carefully controlled release of occlusion. This technical feature can potentially assess the peripheral endothelial function more accurately, whereas the ABI quantifies only the blood pressure ratio between the upper and lower extremities. This principle is similar to flow-mediated dilation in terms of a blood flow-dependent vasodilatory response 22) . Therefore, the SPP might allow us to stratify the risk: SPP <30 mmHg indicates delayed wound healing 23 , 24) , SPP <50 mmHg suggests PAD 13) , and SPP <70 mmHg implies an increased risk of systemic vascular events 14 , 15) .
The present study was associated with several limitations. First, a patient selection bias may have existed during enrollment. The SPP is routinely measured in all patients, whereas the ABI is not measured regularly. It is typically measured in patients with unstable SPP values or shortly after the initiation of dialysis. The median duration of dialysis for enrolled patients was 1.8 (0.1–5.7) years ( Table 1 ) , suggesting that well-conditioned outpatients were included in the study. Second, the generalizability of the study findings is limited because the study population was limited to Japanese HD outpatients. Regional characteristics and local treatment techniques may have influenced the outcomes. Future studies with larger sample sizes of patients with different ethnicities should be conducted.
Conclusion
ABI and SPP measurements have a high clinical utility in predicting mortality and atherosclerotic outcomes in patients undergoing HD. Furthermore, the SPP enables the detection of potential risks that cannot be assessed by the ABI alone. Measurement of the SPP rather than the ABI may contribute to a better understanding of how the overall status of the HD population predicts cardiovascular outcomes.
Acknowledgement
The authors are grateful to all medical staff and patients who participated in this study.
Notice of Grant Support
This study required no specific funding.
Conflict of Interest Statement
None declared.
References
- 1).Bhatt DL, Steg PG, Ohman EM, Hirsch AT, Ikeda Y, Mas JL, Goto S, Liau CS, Richard AJ, Röther J, and Wilson PW: International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA, 2006; 295: 180-189 [DOI] [PubMed] [Google Scholar]
- 2).O’Hare AM, Feinglass J, Reiber GE, Rodriguez RA, Daley J, Khuri S, Henderson WG, and Johansen KL: Postoperative mortality after nontraumatic lower extremity amputation in patients with renal insufficiency. J Am Soc Nephrol, 2004; 15: 427-434 [DOI] [PubMed] [Google Scholar]
- 3).Rajagopalan S, Dellegrottaglie S, Furniss AL, Gillespie BW, Satayathum S, Lameire N, Saito A, Akiba T, Jadoul M, Ginsberg N, Keen M, Port FK, Mukherjee D, and Saran R: Peripheral arterial disease in patients with end-stage renal disease: observations from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Circulation, 2006; 114: 1914-1922 [DOI] [PubMed] [Google Scholar]
- 4).Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, Bell K, Caporusso J, Durand-Zaleski I, Komori K, Lammer J, Liapis C, Novo S, Razavi M, Robbs J, Schaper N, Shigematsu H, Sapoval M, White C, White J, Clement D, Creager M, Jaff M, Mohler E, 3rd, Rutherford RB, Sheehan P, Sillesen H, and Rosenfield K: Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg, 2007; 33 Suppl 1: S1-75 [DOI] [PubMed] [Google Scholar]
- 5).Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, Fleisher LA, Fowkes FG, Hamburg NM, Kinlay S, Lookstein R, Misra S, Mureebe L, Olin JW, Patel RA, Regensteiner JG, Schanzer A, Shishehbor MH, Stewart KJ, Treat-Jacobson D, and Walsh ME: 2016 AHA/ACC Guideline on the Management of Patients With Lower Extremity Peripheral Artery Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation, 2017; 135: e686-e725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6).Aboyans V, Criqui MH, Abraham P, Allison MA, Creager MA, Diehm C, Fowkes FG, Hiatt WR, Jönsson B, Lacroix P, Marin B, McDermott MM, Norgren L, Pande RL, Preux PM, Stoffers HE, and Treat-Jacobson D: Measurement and interpretation of the ankle-brachial index: a scientific statement from the American Heart Association. Circulation, 2012; 126: 2890-2909 [DOI] [PubMed] [Google Scholar]
- 7).Fowkes FG, Murray GD, Butcher I, Heald CL, Lee RJ, Chambless LE, Folsom AR, Hirsch AT, Dramaix M, deBacker G, Wautrecht JC, Kornitzer M, Newman AB, Cushman M, Sutton-Tyrrell K, Fowkes FG, Lee AJ, Price JF, d’Agostino RB, Murabito JM, Norman PE, Jamrozik K, Curb JD, Masaki KH, Rodríguez BL, Dekker JM, Bouter LM, Heine RJ, Nijpels G, Stehouwer CD, Ferrucci L, McDermott MM, Stoffers HE, Hooi JD, Knottnerus JA, Ogren M, Hedblad B, Witteman JC, Breteler MM, Hunink MG, Hofman A, Criqui MH, Langer RD, Fronek A, Hiatt WR, Hamman R, Resnick HE, Guralnik J, and McDermott MM: Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA, 2008; 300: 197-208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8).Ono K, Tsuchida A, Kawai H, Matsuo H, Wakamatsu R, Maezawa A, Yano S, Kawada T, and Nojima Y: Ankle-brachial blood pressure index predicts all-cause and cardiovascular mortality in hemodialysis patients. J Am Soc Nephrol, 2003; 14: 1591-1598 [DOI] [PubMed] [Google Scholar]
- 9).Chen HY, Wei F, Wang LH, Wang Z, Meng J, Yu HB, Zhang RN, Sun GJ, Jiang AL, and Wang L: Abnormal ankle-brachial index and risk of cardiovascular or all-cause mortality in patients with chronic kidney disease: a meta-analysis. J Nephrol, 2017; 30: 493-501 [DOI] [PubMed] [Google Scholar]
- 10).Washida N, Wakino S, Hayashi K, Kuwahara T, and Itoh H: Brachial-ankle pulse wave velocity predicts silent cerebrovascular diseases in patients with end-stage renal diseases. J Atheroscler Thromb, 2010; 17: 165-172 [DOI] [PubMed] [Google Scholar]
- 11).O’Hare A and Johansen K: Lower-extremity peripheral arterial disease among patients with end-stage renal disease. J Am Soc Nephrol, 2001; 12: 2838-2847 [DOI] [PubMed] [Google Scholar]
- 12).Takahara M, Kaneto H, Iida O, Katakami N, Matsuoka TA, Ikeda M, and Shimomura I: Association of diabetes and hemodialysis with ankle pressure and ankle-brachial index in Japanese patients with critical limb ischemia. Diabetes Care, 2012; 35: 2000-2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Okamoto K, Oka M, Maesato K, Ikee R, Mano T, Moriya H, Ohtake T, and Kobayashi S: Peripheral arterial occlusive disease is more prevalent in patients with hemodialysis: comparison with the findings of multidetector-row computed tomography. Am J Kidney Dis, 2006; 48: 269-276 [DOI] [PubMed] [Google Scholar]
- 14).Hiratsuka M, Koyama K, Yamamoto J, Narita A, Sasakawa Y, Shimogushi H, Ogawa A, Kimura T, Mizuguchi K, and Mizuno M: Skin Perfusion Pressure and the Prevalence of Atherothrombosis in Hemodialysis Patients. Ther Apher Dial, 2016; 20: 40-45 [DOI] [PubMed] [Google Scholar]
- 15).Hiratsuka M, Koyama K, Takahashi H, Kasugai T, Hagita J, Kondo A, Koike K, and Hamano T: Low plantar skin perfusion pressure predicts long-term atherosclerotic vascular events and mortality in maintenance haemodialysis patients. Atherosclerosis, 2020; 312: 66-71 [DOI] [PubMed] [Google Scholar]
- 16).Hatakeyama S, Saito M, Ishigaki K, Yamamoto H, Okamoto A, Ishibashi Y, Murasawa H, Imanishi K, Tokui N, Okamoto T, Suzuki Y, Sugiyama N, Imai A, Kudo S, Yoneyama T, Hashimoto Y, Koie T, Kaminura N, Saitoh H, Funyu T, and Ohyama C: Skin perfusion pressure is a prognostic factor in hemodialysis patients. Int J Nephrol, 2012; 2012: 385274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17).Otani Y, Otsubo S, Kimata N, Takano M, Abe T, Okajima T, Miwa N, Tsuchiya K, Nitta K, and Akiba T: Effects of the ankle-brachial blood pressure index and skin perfusion pressure on mortality in hemodialysis patients. Intern Med, 2013; 52: 2417-2421 [DOI] [PubMed] [Google Scholar]
- 18).Tsuruya K and Hirakata H: Japanese Society for Dialysis Therapy guidelines for management of cardiovascular diseases in patients on chronic hemodialysis. Ther Apher Dial, 2012; 16: 384-386 [DOI] [PubMed] [Google Scholar]
- 19).Okamura T, Tsukamoto K, Arai H, Fujioka Y, Ishigaki Y, Koba S, Ohmura H, Shoji T, Yokote K, Yoshida H, Yoshida M, Deguchi J, Dobashi K, Fujiyoshi A, Hamaguchi H, Hara M, Harada-Shiba M, Hirata T, Iida M, Ikeda Y, Ishibashi S, Kanda H, Kihara S, Kitagawa K, Kodama S, Koseki M, Maezawa Y, Masuda D, Miida T, Miyamoto Y, Nishimura R, Node K, Noguchi M, Ohishi M, Saito I, Sawada S, Sone H, Takemoto M, Wakatsuki A, and Yanai H: Japan Atherosclerosis Society (JAS) Guidelines for Prevention of Atherosclerotic Cardiovascular Diseases 2022. J Atheroscler Thromb, 2024; 31: 641-853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Adragao T, Pires A, Branco P, Castro R, Oliveira A, Nogueira C, Bordalo J, Curto JD, and Prata MM: Ankle--brachial index, vascular calcifications and mortality in dialysis patients. Nephrol Dial Transplant, 2012; 27: 318-325 [DOI] [PubMed] [Google Scholar]
- 21).Ohtake T, Oka M, Ikee R, Mochida Y, Ishioka K, Moriya H, Hidaka S, and Kobayashi S: Impact of lower limbs’ arterial calcification on the prevalence and severity of PAD in patients on hemodialysis. J Vasc Surg, 2011; 53: 676-683 [DOI] [PubMed] [Google Scholar]
- 22).Thijssen DHJ, Bruno RM, van Mil A, Holder SM, Faita F, Greyling A, Zock PL, Taddei S, Deanfield JE, Luscher T, Green DJ, and Ghiadoni L: Expert consensus and evidence-based recommendations for the assessment of flow-mediated dilation in humans. Eur Heart J, 2019; 40: 2534-2547 [DOI] [PubMed] [Google Scholar]
- 23).Castronuovo JJ, Jr., Adera HM, Smiell JM, and Price RM: Skin perfusion pressure measurement is valuable in the diagnosis of critical limb ischemia. J Vasc Surg, 1997; 26: 629-637 [DOI] [PubMed] [Google Scholar]
- 24).Pan X, You C, Chen G, Shao H, Han C, and Zhi L: Skin perfusion pressure for the prediction of wound healing in critical limb ischemia: a meta-analysis. Arch Med Sci, 2018; 14: 481-487 [DOI] [PMC free article] [PubMed] [Google Scholar]