Abstract
Objective: The aim of this paper was to assess the differences in clinicopathological characteristics, efficacy and prognosis of neoadjuvant chemotherapy (NAC) in human epidermal growth factor receptor2(HER2)-zero and HER2-low hormone receptor (HR)-negative breast cancer (BC) patients, and the impact of HER2-evolution on prognosis before and after NAC.
Methods: 319 triple negative breast cancer (TNBC) patients who completed NAC and surgery from August 2014 to August 2018 at Tianjin Medical University Cancer Institute and Hospital were included. Clinicopathological features, efficacy of NAC and assessment of prognosis were retrospectively analysed. The evolution of HER2-zero to HER2-low after NAC is defined as HER2-gain, the evolution of HER2-low to HER2-zero after NAC is defined as HER2-loss, and HER2 unchanged after NAC is defined as HER2-stable.
Results: In HR-negative BC, the pathological complete response (pCR) rate was significantly higher in HER2-zero compared with HER2-low patients, and the difference was statistically significant (38.9% vs 23.2%, p = 0.004), but there was no significant difference in the prognosis between the two groups. The overall rate of HER2-evolution after NAC was 19.7%, and there was a significant correlation between HER2-loss and histological grading, whereas HER2-gain was significantly associated with Ki-67 expression. In terms of prognosis, HER2-gain was better compared to the other two groups.
Conclusion: In this study, we found that HER2-low HR-negative BC showed different clinicopathological features and response to NAC compared with HER2-zero, as well as HER2-evolution before and after NAC had a significant impact on prognosis.
Keywords: HER2-low, NAC, PCR, prognosis, HER2 evolution
1 Introduction
According to 2020 global data, BC has become the most common malignant tumour worldwide, accounting for 11.7% of all new cancer cases globally, and has also become the leading cause of cancer death in women (Slamon et al., 1989).
HER2 is a proto-oncogene that is overexpressed in 10%–30% of invasive BC (Sung et al., 2021). For more than 20 years, HER2 has been dichotomised into negative and positive (Dent et al., 2007). The concept of HER2-low was proposed by Paolo Tarantino et al., in 2020:HER2-low includes immunohistochemistry (IHC) 1+ and IHC 2+/In situ hybridization (ISH) (−) (Tarantino et al., 2020), which was also detailed in the 2022 Chinese Society of Clinical Oncology guidelines for the diagnosis and management of BC (Li and Jiang, 2022), and in 2023, the ESMO expert statement supported the consensus on the definition, diagnosis and management of HER2-low BC (Mathey-Andrews, 2024; Tarantino et al., 2023). Previous clinical trials have found that the addition of trastuzumab and pertuzumab Carsten et al. to adjuvant chemotherapy does not result in a prognostic benefit for patients with HER2-low BC (Fehrenbacher et al., 2020; Schneeweiss et al., 2018). The recently developed aIHCntibody-drug conjugate (ADC) drug, T-DXd, has been approved for the treatment of patients with metastatic HER2-positive BC (Nakada et al., 2019) and it effectively targets HER2-low tumour cells and delivers its potent cytotoxic payload to neighbouring tumour cells via a bystander effect (Ogitani et al., 2016a; Ogitani et al., 2016b). And the results of this trial, DESTINY-Breast04 (NCT03734029), not only revealed the effect of T-DXd on HER2-low BC, but also broke the HER2 dichotomy method (Modi et al., 2022).
The proportion of HER2-low in triple negative breast cancer (TNBC) patients is significant, and the effect of changes in HER2 expression before and after NAC on the prognosis of TNBC is not yet known; therefore, the aim of this study was to evaluate the differences in clinicopathological characteristics, efficacy of NAC and prognosis in patients with HER2-zero and HER2-low HR-negative BC, as well as the effect of HER2-evolution on the prognosis of HER2 before and after NAC.
2 Materials and methods
2.1 Patients
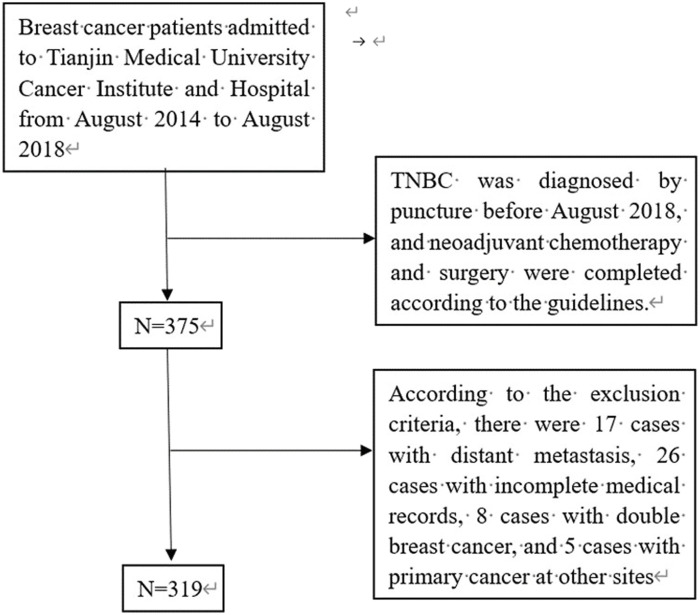
Patients with pathological tissue confirmed as TNBC obtained by crude needle aspiration biopsy at Tianjin Medical University Cancer Institute and Hospital from August 2014 to August 2018 and completed NAC and surgery according to the guidelines were included, and those with incomplete treatment data or follow-up data were excluded (Figure 1).
FIGURE 1.
Data screening process.
Clinical stage was determined by the 8th edition of the American Joint Committee on Cancer (AJCC) tumour-lymph node metastasis (TNM) stage system. Estrogen receptor (ER) and progesterone receptor (PR) were detected by IHC with a cut-off value set at <1%, and HR-negative was defined as negative for both ER and pR. HER2 status was determined by the American Society of Clinical Oncology/College of American Pathologists (ASCO/CAP) Guidelines for HER2 testing, and consisted of IHC 0, IHC 1+, or IHC 2+/FISH (−). HER2-zero was defined as IHC 0, and HER2-low was defined as IHC 1+ or IHC 2+/FISH (−). Evolution of HER2-zero to HER2-low by NAC was defined as HER2-gain, evolution of HER2-low to HER2-zero by NAC was defined as HER2-loss, and HER2 unchanged by NAC was defined as HER2-stable.
2.2 NAC and efficacy evaluation
All patients in this study were treated with NAC. NAC regimens included anthracycline and paclitaxel-based regimens, paclitaxel combined with platinum-based regimens, and other regimens based on guideline recommendations. During the course of treatment, all patients underwent imaging every two cycles to assess clinical efficacy, including ultrasound and MRI. The vast majority of patients underwent surgery after completing all cycles of NAC. The pathological evaluation criterion pCR was defined (Mazouni et al., 2007) as the absence of invasive carcinoma component in the resected breast lesion and in all lymph nodes ipsilateral to the resected breast after completion of NAC, but residual ductal carcinoma-in-situ component may be present in the breast lesion; or the cancerous cells are necrotic or disappeared, and are replaced by granulation or fibrous tissue (i.e.,ypT0/isypN0).
2.3 Statistical analysis
Follow-up by telephone or outpatient review information, with a cut-off date of 31 December 2023, recording the results of the patient’s most recent review, and in case of recurrence/metastasis, recording the time of recurrence/metastasis, i.e., the site of metastasis, etc.,. Disease free survival (DFS) was defined as the time from the end of surgery to the recurrence/metastasis of the disease; Overall survival (OS) was defined as the time from the end of surgery to death or the cut-off of follow-up. Categorical variables described their component ratios, and comparisons between subgroups with different clinicopathological characteristics were performed using the chi-square test. The chi-square test was used for univariate analysis of the relevant factors affecting pCR, followed by multivariate analysis of the relevant factors affecting pCR using logistic regression model, the Kaplan-Meier method was applied to calculate the survival rate and plot the survival curves, and the log-rank test was used to compare the differences in survival between the groups, the above analyses were adjusted for relevant confounding factors such as age, stage, grade, and treatment. And all the data were analysed and processed using SPSS 26.0 statistical software. p < 0.05 was considered statistically significant.
3 Results
3.1 Clinicopathological characteristics
A total of 319 TNBC patients were included in this study. The clinicopathological differences between HER2-zero and HER2-low patients are summarised in Table 1. There were statistically significant differences between the HER2-zero and HER2-low groups in terms of age at diagnosis, clinical N stage, histological grading and Ki67(p < 0.05). That is, compared with patients in the HER2-zero group, patients in the HER2-low group had a greater age at diagnosis (p = 0.035), a greater proportion of patients with clinical N1 and N2-3 stages at the time of the initial diagnosis (p = 0.001), and a significantly higher expression of Ki67(p = 0.012), however, the proportion of patients with histological grade III was lower (p < 0.001). (Table 1).
TABLE 1.
Comparison of clinicopathological features between HER2-zero and HER2-low HR-negative BC patients.
| Clinicopathological features | n | HER2-zero n (%) | HER2-low n (%) | χ2 | p |
|---|---|---|---|---|---|
| Age at diagnosis | 4.455 | 0.035 | |||
| <50 | 151 | 62 (55.4) | 89 (43.0) | ||
| ≥50 | 168 | 50 (44.6) | 118 (57.0) | ||
| Menopausal status at diagnosis | 0.537 | 0.464 | |||
| Premenopausal | 162 | 60 (53.6) | 102 (49.3) | ||
| Postmenopausal | 157 | 52 (46.4) | 105 (50.7) | ||
| Family history | 0.041 | 0.840 | |||
| No | 292 | 103 (92.0) | 189 (91.3) | ||
| Yes | 27 | 9 (8.0) | 18 (8.7) | ||
| Clinical T stage | 0.975 | 0.614 | |||
| cT0-1 | 66 | 23 (20.5) | 42 (20.3) | ||
| cT2 | 158 | 59 (52.7) | 99 (47.8) | ||
| cT3-4 | 95 | 30 (26.8) | 66 (31.9) | ||
| Clinical N stage | 13.194 | 0.001 | |||
| cN0 | 110 | 53 (47.3) | 57 (27.5) | ||
| cN1 | 167 | 45 (40.2) | 122 (58.9) | ||
| cN2-3 | 42 | 14 (12.5) | 28 (13.5) | ||
| Pathological pattern | 1.523 | 0.217 | |||
| Invasive ductal carcinoma | 293 | 103 (92.0) | 181 (87.4) | ||
| Other | 9 | 9 (8.0) | 26 (12.6) | ||
| Histological grading | 55.196 | <0.001 | |||
| Ⅰ-Ⅱ | 166 | 27 (24.1) | 139 (67.1) | ||
| Ⅲ | 153 | 85 (75.9) | 68 (32.9) | ||
| Lymphovascular Invasion | 0.528 | 0.467 | |||
| No | 252 | 91 (81.3) | 161 (77.8) | ||
| Yes | 67 | 21 (18.7) | 46 (22.2) | ||
| TIL (%) | 0.239 | 0.625 | |||
| <10 | 278 | 99 (88.4) | 179 (86.5) | ||
| ≥10 | 41 | 13 (11.6) | 28 (13.5) | ||
| Ki67(%) | 6.242 | 0.012 | |||
| ≤14 | 64 | 31 (27.7) | 33 (15.9) | ||
| >14 | 255 | 81 (72.3) | 174 (84.1) | ||
| p53 (%) | 0.643 | 0.423 | |||
| ≤10 | 102 | 39 (34.8) | 63 (30.4) | ||
| >10 | 217 | 73 (65.2) | 144 (69.6) | ||
| CK5/6 | 0.215 | 0.643 | |||
| Negative | 134 | 49 (43.8) | 85 (41.1) | ||
| Positive | 185 | 63 (56.2) | 122 (58.9) | ||
| EGFR | 0.084 | 0.772 | |||
| Negative | 88 | 32 (28.6) | 56 (27.1) | ||
| Positive | 231 | 80 (71.4) | 151 (72.9) |
3.2 HER2 and efficacy of NAC
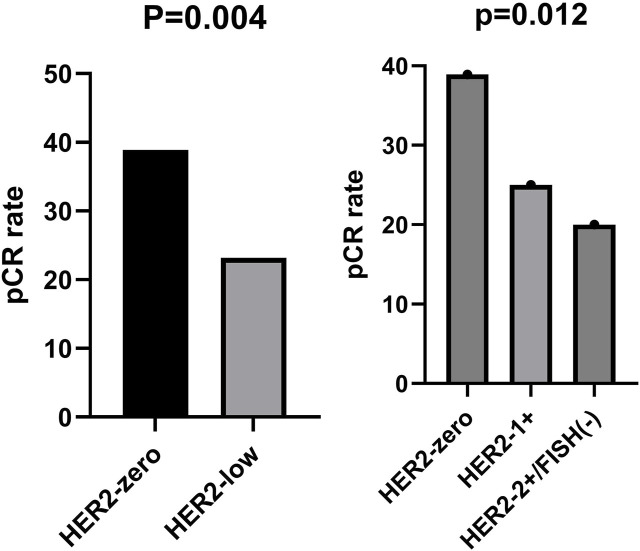
The pCR rate was lower and statistically significant for HER2-low compared to HER2-zero (23.2% vs 38.9%, p = 0.004). pCR rates were decreasing between HER2-zero, HER2-1+, and HER2-2+/FISH(−), possessing a statistically significant difference (38.9%vs25% vs 20%,p = 0.012). (Figure 2).
FIGURE 2.
Comparison of pCR rates for different HER2 expression states.
In the HER2-low subgroup, the pCR rate was 42.9% in patients with clinical stage T0-1, 22.2% in clinical stage T2, and 12.1% in clinical stage T3-4, with a statistically significant difference (p = 0.001). The pCR rate was 25.4% for patients with the pathological type of invasive ductal carcinoma and 7.7% for patients with other pathological types, and the difference was statistically significant (p = 0.045). After multifactorial analysis, it was shown that clinical T-stage was an independent influencing factor affecting the pCR rate of NAC in HER2-low HR-negative patients, and the higher the clinical T-stage, the less likely it was to achieve pathological complete remission (Table 2).
TABLE 2.
Analysis of factors affecting the pCR rate of NAC for HER2-low HR-negative BC.
| Factors | n | pCR (%) | χ2 | p | OR (95%CI) | p |
|---|---|---|---|---|---|---|
| Age at diagnosis | 0.015 | 0.904 | ||||
| <50 | 89 | 21 (23.6) | ||||
| ≥50 | 118 | 27 (229) | ||||
| Menopausal status at diagnosis | 0.197 | 0.657 | ||||
| Premenopausal | 102 | 25 (24.5) | ||||
| Postmenopausal | 105 | 23 (21.9) | ||||
| Family history | 0.471 | 0.493 | ||||
| No | 189 | 45 (23.8) | ||||
| Yes | 18 | 3 (16.7) | ||||
| Clinical T stage | 13.713 | 0.001 | ||||
| cT0-1 | 42 | 18 (42.9) | 1 | |||
| cT2 | 99 | 22 (22.2) | 0.399 (0.182–0.875) | 0.022 | ||
| cT3-4 | 66 | 8 (12.1) | 0.178 (0.068–0.468) | <0.001 | ||
| Clinical N stage | 5.116 | 0.077 | ||||
| cN0 | 57 | 15 (26.3) | ||||
| cN1 | 122 | 31 (25.4) | ||||
| cN2-3 | 28 | 2 (7.1) | ||||
| Pathological pattern | 4.009 | 0.045 | ||||
| Invasive ductal carcinoma | 181 | 46 (25.4) | 1 | |||
| Other | 26 | 2 (7.7) | 0.231 (0.051–1.037) | 0.056 | ||
| HER2 expression | 0.671 | 0.413 | ||||
| 1+ | 132 | 33 (25.0) | ||||
| 2+/FISH(−) | 75 | 15 (20.0) | ||||
| Ki67(%) | 0.050 | 0.823 | ||||
| ≤14 | 24 | 6 (25.0) | ||||
| >14 | 183 | 42 (23.0) | ||||
| p53 (%) | 0.001 | 0.979 | ||||
| ≤10 | 65 | 15 (23.1) | ||||
| >10 | 142 | 33 (23.2) |
3.3 HER2 and prognosis
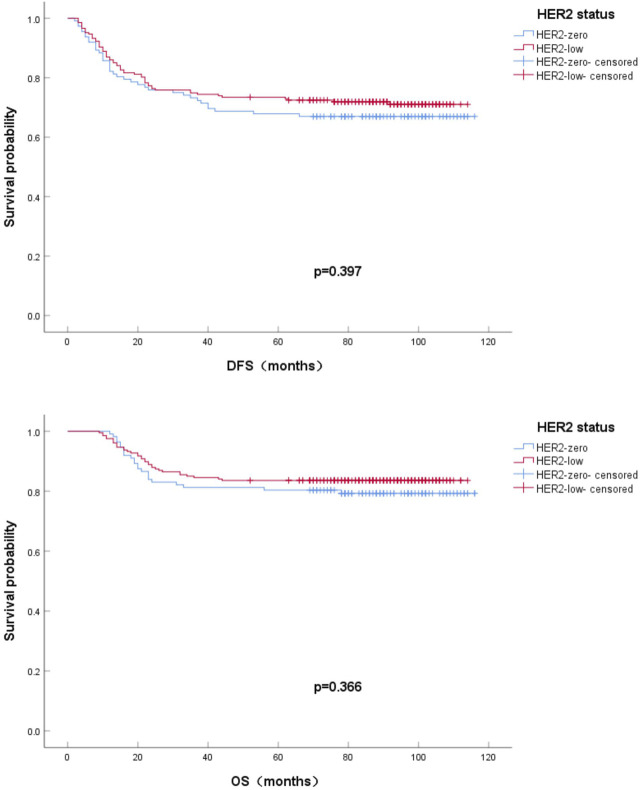
Among 319 HR-negative/HER2-negative BC patients, 96 cases (30.1%) experienced recurrence or metastasis, of which distant metastasis included, 31 bone metastasis, 16 lung metastasis, 15 liver metastasis, and 8 brain metastasis. The 5-year DFS rates of HER2-zero and HER2-low patients were 67.0% and 72.9%, respectively. By the end of observation, the overall number of deaths was 57 or 17.9%, and the HER2-zero and HER2-low OS rates were 79.5% and 83.6%, respectively. The effects of HER2-low and HER2-zero on survival and prognosis were compared by Kaplan-Meier method of univariate analysis and plotting of survival curves. As seen from the survival curves,the differences in DFS and OS between the two groups were not statistically significant (p = 0.397; p = 0.366). (Figure 3).
FIGURE 3.
Kaplan-Meier survival curves for DFS (A) and OS (B) in HER2-zero vs HER2-low HR-negative BC patients.
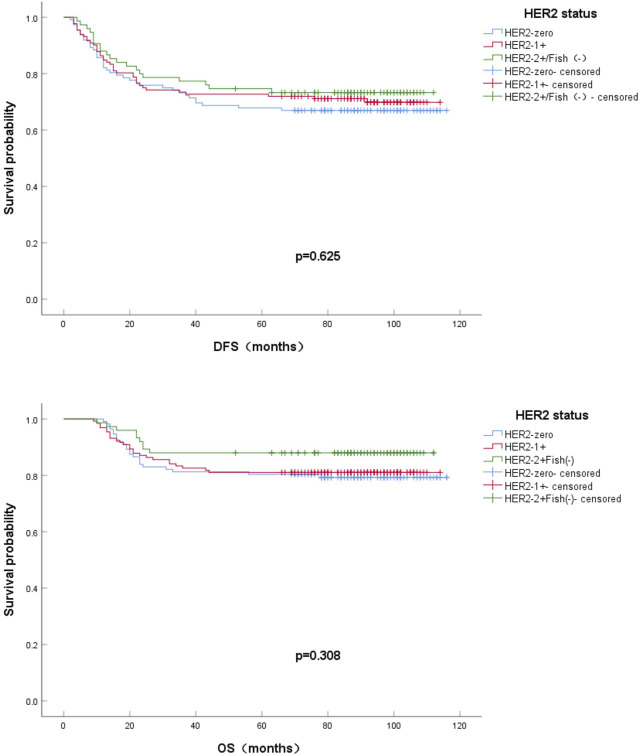
According to HER2 IHC and FISH regrouping, the 5-year DFS rates were 67.0%, 72.7%, and 73.3% for HER2-zero, HER2-1+ and HER2-2+/FISH(−), respectively. By the end of observation, the OS rates were 79.5%,81.1%, and 88.0% for HER2-zero, HER2-1+ and HER2-2+/FISH(−), respectively.The effects of HER2-zero, HER2-1+ and HER2-2+/FISH(−) on survival and prognosis were compared by Kaplan-Meier method of univariate analysis and plotting survival curves. As seen from the survival curves, the differences in DFS and OS between the two groups were not statistically significant (p = 0.625; p = 0.308). (Figure 4).
FIGURE 4.
Kaplan-Meier survival curves for DFS (A) and OS (B) in HER2-zero vs HER2-1+ vs HER2 2+/Fish(-) HR-negative BC patients.
3.4 Clinicopathological characteristics of HER2-evolution
Of the 319 patients included, the overall rate of HER2-evolution after NAC was 19.7%, with 51 HER2-loss and 12 HER2-gain cases. The relationship between HER2-evolution and clinicopathological features was further analysed, and compared with HER2-stable and HER2-gain cases, a histological classification grade III was higher (43.0% vs. 25.0% vs. 78.4%, p < 0.001). Meanwhile, the proportion of Ki-67 > 14% was higher in HER2-gain cases than in HER2-stable and HER2-loss cases (91.7% vs. 82.0% vs. 66.7%, p = 0.026). (Table 3).
TABLE 3.
Clinicopathological features of HER2-evolution in HR-negative BC after NAC.
| Clinicopathological features | HER2-stable n = 256 | HER2-loss n = 51 | HER2-gain n = 12 | χ2 | p |
|---|---|---|---|---|---|
| Age at diagnosis | 1.479 | 0.477 | |||
| <50 | 117 | 28 | 6 | ||
| ≥50 | 139 | 23 | 6 | ||
| Menopausal status at diagnosis | 0.004 | 0.998 | |||
| Premenopausal | 130 | 26 | 6 | ||
| Postmenopausal | 126 | 25 | 6 | ||
| Family history | 0.141 | 0.932 | |||
| No | 135 | 46 | 11 | ||
| Yes | 21 | 5 | 1 | ||
| Clinical T stage | 3.464 | 0.483 | |||
| cT0-1 | 53 | 9 | 2 | ||
| cT2 | 131 | 24 | 4 | ||
| cT3-4 | 72 | 18 | 6 | ||
| Clinical N stage | 7.297 | 0.121 | |||
| cN0 | 87 | 21 | 2 | ||
| cN1 | 131 | 26 | 10 | ||
| cN2-3 | 38 | 4 | 0 | ||
| Pathological pattern | 1.777 | 0.411 | |||
| Invasive ductal carcinoma | 225 | 48 | 11 | ||
| Other | 31 | 3 | 1 | ||
| Histological grading | 24.063 | <0.001 | |||
| Ⅰ-Ⅱ | 146 | 11 | 9 | ||
| Ⅲ | 110 | 40 | 3 | ||
| Lymphovascular Invasion | 1.173 | 0.556 | |||
| No | 203 | 41 | 8 | ||
| Yes | 53 | 10 | 4 | ||
| TIL (%) | 1.696 | 0.428 | |||
| <10 | 220 | 47 | 11 | ||
| ≥10 | 36 | 4 | 1 | ||
| Ki67(%) | 7.330 | 0.026 | |||
| ≤14 | 46 | 17 | 1 | ||
| >14 | 210 | 34 | 11 | ||
| p53 (%) | 2.842 | 0.241 | |||
| ≤10 | 76 | 21 | 3 | ||
| >10 | 180 | 30 | 9 | ||
| CK5/6 | 0.575 | 0.750 | |||
| Negative | 107 | 23 | 4 | ||
| Positive | 149 | 28 | 8 | ||
| EGFR | 0.458 | 0.796 | |||
| Negative | 69 | 16 | 3 | ||
| Positive | 187 | 35 | 9 |
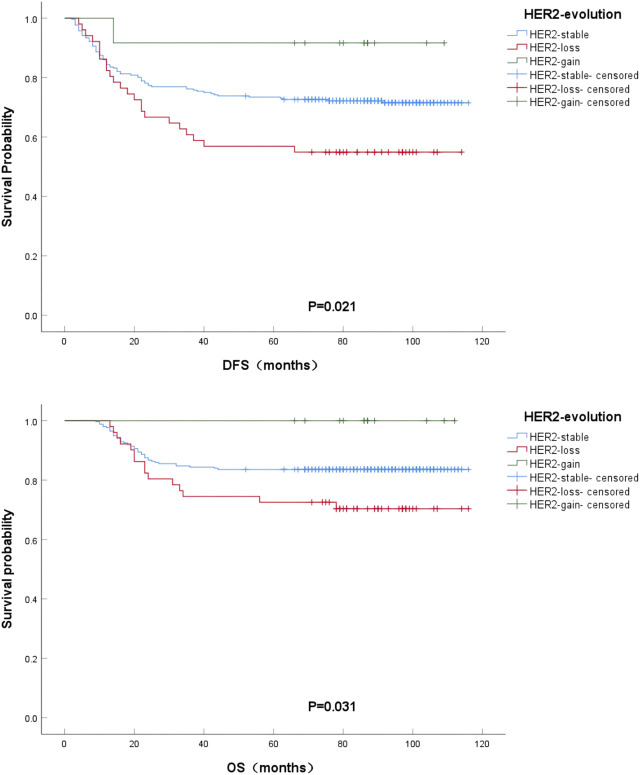
3.5 HER2-evolution and prognosis
The prognostic impact of HER2-evolution after HER2-negative BC NAC was compared by Kaplan-Meier method of univariate analysis and plotting of survival curves. From the survival curves, it can be seen that DFS and OS were significantly better in HER2-gain patients compared to HER2-stable patients, but HER2-loss patients had the worst DFS and OS compared to HER2-stable patients, and the difference was statistically significant (p = 0.021; p = 0.031). (Figure 5).
FIGURE 5.
Kaplan-Meier survival curves for DFS (A) and OS (B) in HER2-stable, HER2-gain, and HER2-loss patients in HR-negative BC.
4 Discussion
BC is a heterogeneous disease with significant heterogeneity of cancer cells and tumour microenvironment during its development, so it has different biological features, molecular characteristics and therapeutic features (Zardavas et al., 2015). TNBC is a common type of BC, accounting for about 15%–20% of BC occurrence. This type of BC is a heterogeneous BC lacking expression of ER, PR, and HER2 amplification, and compared with other types of BC that have a higher risk of both local and distant recurrence (Dent et al., 2007; Lejeune et al., 2023). Also due to the lack of relevant receptor markers, patients with TNBC cannot benefit from established endocrine- or HER2-targeted drugs, and therefore the search for new targets and the development of new therapeutic regimens is an urgent issue in this field.
In this study, 64.9% of the patients exhibited HER2-low, and we compared the clinical case characteristics of HER2-low and HER2-zero HR-negative BC patients, which suggested that compared to HER2-zero patients, HER2-low patients were older (p = 0.035), had a later clinical N-stage (p = 0.001), and had higher Ki67 expression (p = 0.012), but histological grading was more (p < 0.001). Studies by scholars such as Ximena Baez-Navarro and William Jacot have also validated our results, where among HR-negative patients, HER2-low patients were older and less likely to have grade III histological grading (Jacot et al., 2021; Baez-Navarro et al., 2023). In contrast to our study, some studies have also reported a lower frequency of HER2-low BC Ki67 ≥ 14% or 20% in HR-negative BC compared to HER2-zero tumours (Ma et al., 2024). This may be related to, for example, ethnic differences.
NAC is a frequently chosen treatment option for TNBC and has a high survival rate in patients who achieve pCR (Glück et al., 2012; Liedtke et al., 2023). In our study, we found that among HR-negative BC patients, the pCR rate of HER2-low patients was significantly lower than that of HER2-zero patients (23.2% vs 38.9%, p = 0.004), and the results of the unifactorial and multifactorial analyses of the influence of NAC on the pCR rate of HER2-low HR-negative BC suggested that the clinical T-stage was an independent influencing factor. Existing studies are conflicting on this point of view, and although the pCR rates of the two groups are numerically different, fewer are statistically different (Liedtke et al., 2023; Shao et al., 2022). Xu et al. based their study on a multicentre study in China, for HR-negative BC patients, the tpCR [total (both breast and axillary lymph nodes) pathologic complete response] rate, bpCR (breast pathologic complete response) rate, and MP4-5 [The score of Miller-Payne (MP) grade, MP assessment was evaluated based on reduced tumor cellularity of resection samples and comparison with core needle biopsy samples. Grades 4–5 are categorized as good pathological response.] rate of HER2-low patients were significantly lower than those of HER2-zero patients (Xu et al., 2023). Shao et al. similarly explored the effect of the effect of HER2-low on NAC efficacy in different states of HR, and they made adjustments to the definition of pCR, and their results indicated that HER2-low might be related to the pCR of BC patients treated with NAC, but different HR statuses and criteria for the definition of pCR need to be taken into account at the same time (Schettini et al., 2021).
Since HER2-low BC began to receive attention, relevant studies have investigated the differences between HER2-low and HER2-zero. Most of the results showed no significant difference in prognosis between the two when HR expression was not considered (Jacot et al., 2021; Schettini et al., 2021; Horisawa et al., 2022; Agostinetto et al., 2021; de Moura Leite et al., 2021; Gampenrieder et al., 2021; Wu et al., 2023). In the present study, we found that among HR-negative BC patients, the DFS and OS rates were not statistically significant, although HER2-low patients had slightly better DFS and OS rates than those of HER2-zero patients, which was consistent with the results of most of the studies mentioned above; moreover, we did not find any differences in DFS and OS among the HER2-zero, HER2-1+ and HER2-2+/Fish (−) groups. Studies by scholars such as Gampenrieder and William Jacot revealed similar findings in patients with metastatic TNBC and non-metastatic TNBC (Schettini et al., 2021; Gampenrieder et al., 2023). Denkert et al. also reported the prognosis of HER2-low and HER2-zero BC, and according to their study, the prognosis of HER2-low BC was statistically significantly superior to HER2-zero BC, especially in HR-negative patients (Denkert et al., 2021). The difference in outcomes may be related to differences in the number of cases and diagnosis of HER2-low between studies.
In the present study, we found HER2-evolution after receiving NAC, and it has been reported that discordance in HR and/or HER2 status between primary and residual tumours after NAC is a relatively common phenomenon (Miglietta et al., 2022). In this study, we assessed the evolution of HER2 expression from puncture biopsy to residual disease after NAC, and the overall rate of HER2-evolution after NAC was 19.7%, which resulted in a lower figure than in other studies because only BC patients who were HER2-negative both before and after NAC were included in this study. Exploratory analyses of clinicopathological features and HER2-evolution showed that patients with histological grade III were more likely to develop HER2-loss, and those with Ki-67 > 14% were more likely to develop HER2-gain This may be related to the higher tumour heterogeneity in these patients. Unlike the present study, a study exploring the relationship between HER2-evolution and clinicopathological features in TNBC patients with non-pCR after NAC showed that HER2-evolution were more related to clinical T-stage (Shao et al., 2024). Although the results of the two studies were different, they were able to show that HER2-evolution may be associated with higher tumour heterogeneity. To address the impact of HER2-evolution on prognosis, we found that DSF and OS were prolonged in HER2-gain patients compared to HER2-stable, which was more favourable than that of HER2-loss patients. A study by Shao et al. also found that DFS and OS trended more favourably in HER2-gain patients compared to HER2-stable in patients with TNBC, but again, there was no statistically significance (Shao et al., 2024). The impact of HER2-evolution on BC prognosis is unclear in the available studies, and the inclusion and exclusion criteria likewise vary between studies, but focused monitoring of patients with HER2-evolution after NAC is necessary.
Currently, the concept of HER2-ultralow arose as a result of a more nuanced categorization of HER2 expression status, i.e., scoring 0 with incomplete and faint staining in ≤10% of tumor cells (Hayes, 2019). And in Destiny Breast-06, T-DXd was evaluated in patients with HER-low or HER2-ultralow (IHC 0, membrane staining), HR + mBC who had disease progression (PD) after endocrine-based therapy and had not received prior CT for mBC, and it was found that in HER2-low mBC, T-DXd compared to TPC (CT) showed a statistically significant and clinically meaningful PFS benefit and that HER2-ultra-low was consistent with HER2-low results (Franchina et al., 2023). This may suggest a new molecular typing of breast cancer and a new therapeutic strategy for breast cancer patients who were once “drug-free”.
In TNBC patients, although no survival differences in DFS and OS were found, patients with HER 2-low BC had a lower pCR rate than patients with HER2-zero BC. The DESTINY-Breast04 clinical trial demonstrated that in patients with HER 2-low metastatic B, T-DXd resulted in a progression-free survival and OS that was significantly longer than that achieved with the physician’s chosen (Fehrenbacher et al., 2020). Therefore, clinical trials that incorporate HER2-low BC into systemic treatment decisions for non-metastatic breast cancer should be explored.
In conclusion, there is no uniformity in the clinicopathological features and prognosis for patients with HER2-low HR-negative BC. However, as with the results of other studies, the results of this retrospective analysis showed that the clinical case characteristics and efficacy of NAC in HER2-low differ from those in HER2-zero patients, and it is not possible to clarify the clinicopathological and prognostic characteristics of patients with HER2-low HR-negative BC with this study alone. Our study has the advantage of excluding the interference of HR status, but it also has some limitations, including a relatively small sample size and retrospective single-centre study, which may lead to selectivity bias. And different guidelines for HER2 detection and interpretation were used during this period, and lack of pathology focused on correcting HER2 expression. And all the study subjects were Chinese, which should be cautious in interpreting these results because of the possible differences in cancer biology among different races. Our study is also a retrospective study conducted on HER2-low HR-negative BC patients, which we hope will provide a reference for later prospective studies as well as more attention to this population in future clinical work.
5 Conclusion
In conclusion, this study found that HER2-low HR-negative BC disorders exhibit different clinicopathological features, response to NAC, and prognosis after treatment, as well as the prognostic impact of HER2-evolution after NAC.
Acknowledgments
We thank all patients who participated in our study.
Funding Statement
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by research funding from the Youth Science Foundation of National Natural Science Foundation of China (No. 82203407).
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
J-JL: Conceptualization, Methodology, Writing–original draft, Writing–review and editing. YZ: Conceptualization, Methodology, Writing–original draft, Writing–review and editing, Data curation, Formal Analysis, Funding acquisition, Investigation, Project administration, Resources, Software, Supervision, Validation, Visualization. S-CZ: Data curation, Formal Analysis, Investigation, Project administration, Writing–original draft. XL: Data curation, Investigation, Methodology, Project administration, Writing–original draft. S-NW: Data curation, Investigation, Methodology, Project administration, Writing–original draft. X-YL: Data curation, Investigation, Methodology, Project administration, Writing–original draft. JZ: Conceptualization, Formal Analysis, Funding acquisition, Methodology, Resources, Writing–review and editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Agostinetto E., Rediti M., Fimereli D., Debien V., Piccart M., Aftimos P., et al. (2021). HER2-Low breast cancer: molecular characteristics and prognosis. Cancers (Basel) 13 (11), 2824. 10.3390/cancers13112824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baez-Navarro X., van Bockstal M. R., Andrinopoulou E. R., van Deurzen C. H. M. (2023). HER2-Low breast cancer: incidence, clinicopathologic features, and survival outcomes from real-world data of a large nationwide cohort. Mod. Pathol. 36 (4), 100087. 10.1016/j.modpat.2022.100087 [DOI] [PubMed] [Google Scholar]
- de Moura Leite L., Cesca M. G., Tavares M. C., Santana D. M., Saldanha E. F., Guimarães P. T., et al. (2021). HER2-low status and response to neoadjuvant chemotherapy in HER2 negative early breast cancer. Breast Cancer Res. Treat. 190 (1), 155–163. 10.1007/s10549-021-06365-7 [DOI] [PubMed] [Google Scholar]
- Denkert C., Seither F., Schneeweiss A., Link T., Blohmer J. U., Just M., et al. (2021). Clinical and molecular characteristics of HER2-low-positive breast cancer: pooled analysis of individual patient data from four prospective, neoadjuvant clinical trials. Lancet Oncol. 22 (8), 1151–1161. 10.1016/s1470-2045(21)00301-6 [DOI] [PubMed] [Google Scholar]
- Dent R., Trudeau M., Pritchard K. I., Hanna W. M., Kahn H. K., Sawka C. A., et al. (2007). Triple-negative breast cancer: clinical features and patterns of recurrence. Clin. Cancer Res. 13 (15 Pt 1), 4429–4434. 10.1158/1078-0432.Ccr-06-3045 [DOI] [PubMed] [Google Scholar]
- Fehrenbacher L., Cecchini R. S., Geyer C. E., Jr., Rastogi P., Costantino J. P., Atkins J. N., et al. (2020). NSABP B-47/NRG Oncology phase III randomized trial comparing adjuvant chemotherapy with or without trastuzumab in high-risk invasive breast cancer negative for HER2 by FISH and with IHC 1+ or 2. J. Clin. Oncol. 38 (5), 444–453. 10.1200/jco.19.01455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franchina M., Pizzimenti C., Fiorentino V., Martini M., Ricciardi R., Silvestris N., et al. (2023). Low and ultra-low HER2 in human breast cancer: an effort to define new neoplastic subtypes. Int. J. Mol. Sci24 (16), 12795. 10.3390/ijms241612795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gampenrieder S. P., Dezentjé V., Lambertini M., de Nonneville A., Marhold M., Le Du F., et al. (2023). Influence of HER2 expression on prognosis in metastatic triple-negative breast cancer-results from an international, multicenter analysis coordinated by the AGMT Study Group. ESMO Open 8 (1), 100747. 10.1016/j.esmoop.2022.100747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gampenrieder S. P., Rinnerthaler G., Tinchon C., Petzer A., Balic M., Heibl S., et al. (2021). Landscape of HER2-low metastatic breast cancer (MBC): results from the Austrian AGMT_MBC-Registry. Breast Cancer Res. 23 (1), 112. 10.1186/s13058-021-01492-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glück S., Ross J. S., Royce M., McKenna E. F., Jr., Perou C. M., Avisar E., et al. (2012). TP53 genomics predict higher clinical and pathologic tumor response in operable early-stage breast cancer treated with docetaxel-capecitabine ± trastuzumab. Breast Cancer Res. Treat. 132 (3), 781–791. 10.1007/s10549-011-1412-7 [DOI] [PubMed] [Google Scholar]
- Hayes F. (2019). HER2 and breast cancer - a phenomenal success story. N. Engl. J. Med. 381 (13), 1284–1286. 10.1056/NEJMcibr1909386 [DOI] [PubMed] [Google Scholar]
- Horisawa N., Adachi Y., Takatsuka D., Nozawa K., Endo Y., Ozaki Y., et al. (2022). The frequency of low HER2 expression in breast cancer and a comparison of prognosis between patients with HER2-low and HER2-negative breast cancer by HR status. Breast Cancer 29 (2), 234–241. 10.1007/s12282-021-01303-3 [DOI] [PubMed] [Google Scholar]
- Jacot W., Maran-Gonzalez A., Massol O., Sorbs C., Mollevi C., Guiu S., et al. (2021). Prognostic value of HER2-low expression in non-metastatic triple-negative breast cancer and correlation with other biomarkers. Cancers (Basel) 13 (23), 6059. 10.3390/cancers13236059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejeune M., Reverté L., Sauras E., Gallardo N., Bosch R., Roso A., et al. (2023). Prognostic implications of the residual tumor microenvironment after neoadjuvant chemotherapy in triple-negative breast cancer patients without pathological complete response. Cancers (Basel) 15 (3), 597. 10.3390/cancers15030597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li J., Jiang Z. (2022). Chinese society of clinical Oncology breast cancer (CSCO BC) guidelines in 2022: stratification and classification. Cancer Biol. Med. 19 (6), 769–773. 10.20892/j.issn.2095-3941.2022.0277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liedtke C., Mazouni C., Hess K. R., André F., Tordai A., Mejia J. A., et al. (2023). Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J. Clin. Oncol. 41 (10), 1809–1815. 10.1200/jco.22.02572 [DOI] [PubMed] [Google Scholar]
- Ma Y., Jiao D., Zhang J., Lv M., Chen X., Liu Z. (2024). HER2-Low status was associated with better breast cancer-specific survival in early-stage triple-negative breast cancer. Oncologist 29 (3), e309–e318. 10.1093/oncolo/oyad275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathey-Andrews N. (2024). Prime editing GEMMs to model cancer mutations. Nat. Rev. Cancer 24 (1), 2. 10.1038/s41568-023-00627-w [DOI] [PubMed] [Google Scholar]
- Mazouni C., Peintinger F., Wan-Kau S., Andre F., Gonzalez-Angulo A. M., Symmans W. F., et al. (2007). Residual ductal carcinoma in situ in patients with complete eradication of invasive breast cancer after neoadjuvant chemotherapy does not adversely affect patient outcome. J. Clin. Oncol. 25 (19), 2650–2655. 10.1200/jco.2006.08.2271 [DOI] [PubMed] [Google Scholar]
- Miglietta F., Griguolo G., Bottosso M., Giarratano T., Lo Mele M., Fassan M., et al. (2022). HER2-low-positive breast cancer: evolution from primary tumor to residual disease after neoadjuvant treatment. NPJ Breast Cancer 8 (1), 66. 10.1038/s41523-022-00434-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modi S., Jacot W., Yamashita T., Sohn J., Vidal M., Tokunaga E., et al. (2022). Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N. Engl. J. Med. 387 (1), 9–20. 10.1056/NEJMoa2203690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakada T., Sugihara K., Jikoh T., Abe Y., Agatsuma T. (2019). The latest research and development into the antibody-drug conjugate, [fam-] trastuzumab deruxtecan (DS-8201a), for HER2 cancer therapy. Chem. Pharm. Bull. (Tokyo) 67 (3), 173–185. 10.1248/cpb.c18-00744 [DOI] [PubMed] [Google Scholar]
- Ogitani Y., Aida T., Hagihara K., Yamaguchi J., Ishii C., Harada N., et al. (2016a). DS-8201a, A novel HER2-targeting ADC with a novel dna topoisomerase I inhibitor, demonstrates a promising antitumor efficacy with differentiation from T-DM1. Clin. Cancer Res. 22 (20), 5097–5108. 10.1158/1078-0432.Ccr-15-2822 [DOI] [PubMed] [Google Scholar]
- Ogitani Y., Hagihara K., Oitate M., Naito H., Agatsuma T. (2016b). Bystander killing effect of DS-8201a, a novel anti-human epidermal growth factor receptor 2 antibody-drug conjugate, in tumors with human epidermal growth factor receptor 2 heterogeneity. Cancer Sci. 107 (7), 1039–1046. 10.1111/cas.12966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schettini F., Chic N., Brasó-Maristany F., Paré L., Pascual T., Conte B., et al. (2021). Clinical, pathological, and PAM50 gene expression features of HER2-low breast cancer. NPJ Breast Cancer 7 (1), 1. 10.1038/s41523-020-00208-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneeweiss A., Park-Simon T. W., Albanell J., Lassen U., Cortés J., Dieras V., et al. (2018). Phase Ib study evaluating safety and clinical activity of the anti-HER3 antibody lumretuzumab combined with the anti-HER2 antibody pertuzumab and paclitaxel in HER3-positive, HER2-low metastatic breast cancer. Invest. New Drugs 36 (5), 848–859. 10.1007/s10637-018-0562-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao Y., Guan H., Luo Z., Yu Y., He Y., Chen Q., et al. (2024). Clinicopathological characteristics and value of HER2-low expression evolution in breast cancer receiving neoadjuvant chemotherapy. Breast 73, 103666. 10.1016/j.breast.2023.103666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao Y., Yu Y., Luo Z., Guan H., Zhu F., He Y., et al. (2022). Clinical, pathological complete response, and prognosis characteristics of HER2-low breast cancer in the neoadjuvant chemotherapy setting: a retrospective analysis. Ann. Surg. Oncol. 29 (13), 8026–8034. 10.1245/s10434-022-12369-4 [DOI] [PubMed] [Google Scholar]
- Slamon D. J., Godolphin W., Jones L. A., Holt J. A., Wong S. G., Keith D. E., et al. (1989). Studies of the HER-2/neu proto-oncogene in human breast and ovarian cancer. Science 244 (4905), 707–712. 10.1126/science.2470152 [DOI] [PubMed] [Google Scholar]
- Sung H., Ferlay J., Siegel R. L., Laversanne M., Soerjomataram I., Jemal A., et al. (2021). Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71 (3), 209–249. 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- Tarantino P., Hamilton E., Tolaney S. M., Cortes J., Morganti S., Ferraro E., et al. (2020). HER2-Low breast cancer: pathological and clinical landscape. J. Clin. Oncol. 38 (17), 1951–1962. 10.1200/jco.19.02488 [DOI] [PubMed] [Google Scholar]
- Tarantino P., Viale G., Press M. F., Hu X., Penault-Llorca F., Bardia A., et al. (2023). ESMO expert consensus statements (ECS) on the definition, diagnosis, and management of HER2-low breast cancer. Ann. Oncol. 34 (8), 645–659. 10.1016/j.annonc.2023.05.008 [DOI] [PubMed] [Google Scholar]
- Wu Q., Yang F., Liu Y., Zhang H., Zhang S., Xin L., et al. (2023). Analysis of clinicopathological characteristics and prognostic factors of early-stage human epidermal growth factor receptor 2 (HER2)-low breast cancer: compared with HER2-0 breast cancer. Cancer Med. 12 (19), 19560–19575. 10.1002/cam4.6571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu W., Jiang Y., Xu L., Li C., Wang J., Liu Z., et al. (2023). HER2-low status may predict poor neoadjuvant chemotherapy response in HR-negative breast cancer: a real-world multicenter study. Jpn. J. Clin. Oncol53 53 (6), 463–471. 10.1093/jjco/hyad009 [DOI] [PubMed] [Google Scholar]
- Zardavas D., Irrthum A., Swanton C., Piccart M. (2015). Clinical management of breast cancer heterogeneity. Nat. Rev. Clin. Oncol. 12 (7), 381–394. 10.1038/nrclinonc.2015.73 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.