Abstract
Background
Hair transplantation (HT) has been reported to be effective for the treatment of female-pattern hair loss (FPHL). Few studies have investigated HT in FPHL.
Objective
To evaluate the clinical features of FPHL treated with HT and analyze the real-world results of HT.
Methods
We conducted a retrospective chart review of 195 FPHL patients who underwent hair transplants. The patients’ demographics, clinical features, and clinical courses of HT were recorded.
Results
The mean (±SD) age of patients was 49.1±11.9 years. Analysis of the severity of hair loss showed that 31.8%, 49.7%, and 18.5% of patients had F1, F2, and F3 types of hair loss (according to the BASP Classification); 88.2% of patients had more than 75% satisfaction with HT. The satisfaction level was significantly higher in the group that had the highest number of hairs implanted. Complications such as pain, facial edema, folliculitis, scar, paresthesia, telogen effluvium were found.
Conclusion
This study could provide substantial information of HT in FPHL. Clinicians could deliver more sufficient counsel to FPHL patients about HT.
Keywords: Alopecia, Transplantation
INTRODUCTION
Hair may not have crucial biological functions, but is important for self-esteem and social identity functions. The phobia of hair loss is nearly as great as the fear of experiencing a myocardial infarction1,2. Additionally, the fear of hair loss was significantly higher in women than in men2. Therefore, appropriate treatment of hair loss is very important for women. However, the options of medical treatment are very limited and could have unsatisfactory outcomes with regard to female-pattern hair loss (FPHL), unlike the outcomes in male-pattern baldness (MPB)1. For example, the use of finasteride, a 5α-reductase type 2 inhibitor, in FPHL remains controversial and is generally contraindicated, especially in premenopausal women, because of its teratogenic effects1,3. Therefore, due to the limited medical treatment options for FPHL, hair transplantation (HT) has been performed as an optional surgical treatment, especially in patients with severe FPHL that is refractory to medical treatment or for cosmetic purposes. The clinicopathological characteristics of FPHL and the performance and clinical course of HT differ from that of MPB and HT in MPB, respectively1,4. However, few studies have investigated HT in FPHL.
This study was conducted to obtain a better understanding of the clinical features of HT in FPHL and to identify the factors that were associated with patient satisfaction in order to decrease conflicts between surgeons and patients.
MATERIALS AND METHODS
In this study, we retrospectively enrolled 195 patients who underwent HT between 2010 and 2020 at multicenter institutions in South Korea. The study protocol was reviewed and approved by the Institutional Review Board (IRB No 2021-06-023). Only women who underwent HT for FPHL were included in the present study. Patients who underwent HT for other purposes, such as the correction of scarring alopecia or receding hairline, were excluded. We collected preoperative demographics and clinical data that included age, hair-loss period, treatment history, family history of hair loss, severity of hair loss using the BASP classification5, HT technique, implanted total hair number, and the patient’s subjective satisfaction with HT.
As the type of HT technology used was only follicular unit transplantation (FUT) at the three hospitals, surgery was performed using only FUT. In the other three hospitals, both follicular unit extraction (FUE) and FUT methods were available. Therefore, in this study, the choice of HT method was mainly determined by the preference of the doctor and patient, and partly by the characteristics of the posterior scalp. (e.g. very tight scalp, very low hair density)
To calculate the number of transplanted hairs, the collected follicular units were multiplied by 2. According to research, the distribution of 1, 2, 3 hair per follicular unit in the occipital scalp is known to be 1:2:3, with an average of 2 hairs per follicle6.
Furthermore, we collected data on postoperative clinical features, including pain, facial edema, donor-site scar, folliculitis, donor- and recipient-site paresthesia, and telogen effluvium at the operation site. Postoperative pain was evaluated using a 10-point visual analog scale (VAS). The patient’s subjective satisfaction was defined as 0 points when they were dissatisfied, and as 1, 2, 3, and 4 points for approximately 25%, 50%, 75%, and >90% of patient satisfaction, respectively. Patient satisfaction was assessed at least 1 year after surgery, at which point the transplanted hairs had grown and cosmetically acceptable results had been achieved7.
RESULTS
Patient demographics and preoperative clinical features
We analyzed the clinical features of 195 Korean women with FPHL who underwent HT, and the demographics and preoperative clinical characteristics of the study cohort are presented in Table 1. The mean (±SD) age of patients was 49.1±11.9 years; 7.7%, 15.9%, 19.0%, 37.9%, 19.0%, and 0.5% of the cohort were in their 20s, 30s, 40s, 50s, 60s, and 70s, respectively. The mean hair loss period was 121.7±92.7 months, and 80.2% of the participants had a family history of baldness (first-degree relatives). With regard to the pre-HT medical treatments that were availed, we ascertained that 18.1%, 22.8%, 2.6%, 33.2%, 14.5%, 23.3%, and 16.6% of patients had used a 5α-reductase inhibitor, topical minoxidil, herbal medication, cosmeceuticals (e.g., shampoo or hair tonic), mesotherapy, nutritional supplements (e.g., vitamins, minerals, etc.), and visited no-clinician-managed scalp care centers; 22.3% of patients did not avail any pre-HT medical treatment for FPHL. Cosmeceuticals were the most frequently used pre-HT intervention to treat hair loss. Analysis of the severity of hair loss showed that 31.8%, 49.7%, and 18.5% of patients had F1, F2, and F3 types of hair loss (according to the BASP Classification).
Table 1. Patient demographics and clinical features.
| Characteristics | Values (n=195) | |
|---|---|---|
| Age (yr) | ||
| 10–19 | 0 (0) | |
| 20–29 | 15 (7.7) | |
| 30–39 | 31 (15.9) | |
| 40–49 | 37 (19.0) | |
| 50–59 | 74 (37.9) | |
| 60–69 | 37 (19.0) | |
| 70–79 | 1 (0.5) | |
| Mean ± SD | 49.1±11.9 | |
| Past treatment history (n=193) | ||
| 5α-reductase inhibitor | 35 (18.1) | |
| Topical minoxidil | 44 (22.8) | |
| Herbal medication | 5 (2.6) | |
| Cosmeceuticals | 64 (33.2) | |
| Mesotherapy | 28 (14.5) | |
| Nutritional supplement | 45 (23.3) | |
| Hair care clinic (not hospital) | 32 (16.6) | |
| No treatment | 43 (22.3) | |
| BASP classification | ||
| F1 | 62 (31.8) | |
| F2 | 97 (49.7) | |
| F3 | 36 (18.5) | |
Values are presented as absolute numbers only, mean ± standard deviation, or percentages (%).
Post-HT clinical course
Details of the patients’ post-HT clinical course are described in Table 2. With regard to the type of HT technique used, 74.9% and 25.1% of patients received FUT or FUE, respectively. The number (not follicular unit) of hairs transplanted was in the ranges 1,000–1,999, 2,000–2,999, 3,000–3,999, and 4,000–4,999 in 6.2%, 36.9%, 51.3%, and 5.6% of patients, respectively. Although all participants received analgesics for postoperative pain control after the effect of the local anesthetic disappeared, 66.5% of patients experienced pain on the first postoperative day after HT. In the majority of the study cohort, the VAS pain score was less than 3 on the day of the operation and on the first postoperative day after HT and might be attributable to analgesic use. Only five patients had VAS scores higher than five for pain on the first day after HT. Nonetheless, 29.2% and 24.2% of patients complained of pain on day 7 and 10, respectively, after HT. In general, the pain lessened over time; however, two participants had VAS scores higher than five on the tenth day after HT.
Table 2. Clinical courses after HT.
| Characteristics | Values (n=195) | ||
|---|---|---|---|
| Implanted hair numbers | |||
| 1,000–1,999 | 12 (6.2) | ||
| 2,000–2,999 | 72 (36.9) | ||
| 3,000–3,999 | 100 (51.3) | ||
| 4,000–4,999 | 11 (5.6) | ||
| Mean ± SD | 2,930±695.3 | ||
| Satisfaction Scale | |||
| 0 (not satisfied) | 0 (0) | ||
| 1 (about 25%) | 2 (1.0) | ||
| 2 (about 50%) | 21 (10.8) | ||
| 3 (about 75%) | 92 (47.2) | ||
| 4 (more than 90%) | 80 (41.0) | ||
| Pain (n=161) | |||
| Immediately after surgery | |||
| Yes | 107 (66.5) | ||
| No | 54 (33.5) | ||
| Mean VAS score | 2.3±1.4 | ||
| 1 day after HT | |||
| Yes | 107 (66.5) | ||
| No | 54 (33.5) | ||
| Mean VAS score | 2.0±1.2 | ||
| 7 days after HT | |||
| Yes | 47 (29.2) | ||
| No | 114 (70.8) | ||
| Mean VAS score | 1.6±1.4 | ||
| 10 days after HT | |||
| Yes | 39 (24.2) | ||
| No | 122 (75.8) | ||
| Mean VAS score | 1.5±1.3 | ||
| Facial edema | |||
| Yes | 31 (15.9) | ||
| No | 164 (84.1) | ||
| Mean occurrence time (days) | 1.6 | ||
| Mean duration (days) | 2.9±1.3 | ||
| Folliculitis | |||
| Yes | 30 (15.4) | ||
| No | 165 (84.6) | ||
| Mean occurrence time (mo) | 1.5±0.7 | ||
| Donor site scar | |||
| Keloid scar | 0 (0) | ||
| Hypertrophic scar | 3 (1.5) | ||
| Flat scar | 144 (73.9) | ||
| Round dot like scar | 48 (24.6) | ||
| Donor site paresthesia | |||
| Yes | 22 (11.3) | ||
| No | 173 (88.7) | ||
| Recipient site paresthesia | |||
| Yes | 67 (34.4) | ||
| No | 128 (65.6) | ||
| Donor site telogen effluvium | |||
| Yes | 13 (6.7) | ||
| No | 182 (93.3) | ||
| Recipient site telogen effluvium | |||
| Yes | 88 (45.1) | ||
| No | 107 (54.9) | ||
Values are presented as absolute numbers only, mean ± standard deviation, or percentages (%).
HT: hair transplantation.
After HT, 15.9% of patients experienced facial edema, which occurred, on average, 1.6 days after the operation and lasted for 2.9 days. Moreover, 15.4% of patients experienced postoperative scalp folliculitis, which occurred, on average, 1.5 months after HT, and these patients also complained of pruritus (43.3%) or pain (20.0%); however, 36.7% of patients with scalp folliculitis were asymptomatic. Scalp folliculitis resolved spontaneously in most of the patients. Furthermore, almost all patients who underwent FUT or FUE had a linear or circular scar, respectively, at the donor sites. Three patients (1.5%) had hypertrophic scars. Donor-site and recipient-site paresthesia were observed in 11.3% and 34.4% of patients, but disappeared before the 6-month postoperative visit in nearly all patients (one patient had recipient-site paresthesia for >6 months). Furthermore, 6.7% and 45.1% of patients experienced telogen effluvium of surrounding hair at the donor site and of preexisting (not transplanted) hair at the recipient site, respectively.
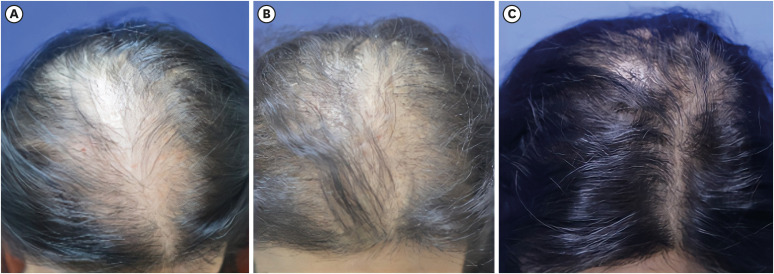
Patient satisfaction with HT was rated as 1, 2, 3, and 4 points in 1.0%, 10.8%, 47.2%, and 41.0% of patients, respectively (Fig. 1). The satisfaction level was significantly higher in the group that had the highest number of hairs implanted.
Fig. 1. Four-point satisfaction of a patient with hair transplantation. A 38-year-old female patient was of BASP classification type 3 before surgery (A). This patient received a total of 2,768 hair transplants. She experienced recipient site effluvium four months after surgery (B). Thirteen months after the operation, female pattern hair loss was maintained in a significantly improved state, and subjective satisfaction score was 4 points (C).
Comparison of FUT and FUE
In this pilot retrospective study, we compared only the representative parameters such as the implanted hair numbers, postoperative pain, donor-site paresthesia, and scalp folliculitis between the FUT and FUE groups (Table 3). In the FUT group, 6.2%, 30.8%, 56.2%, and 6.8% of patients received 1,000–1,999, 2,000–2,999, 3,000–3,999, and 4,000–4,999 hairs, respectively, during HT. Similarly, in the FUE group, 6.1%, 55.2%, 36.7%, and 2.0% of patients received 1,000–1,999, 2,000–2,999, 3,000–3,999, and 4,000–4,999 hairs, respectively, during HT. The mean implanted hair numbers were 3,034±687.7 in FUT and 2,621±628.4 in FUE, and the FUT group had a higher number of implanted hairs than the FUE group.
Table 3. Comparison of FUT and FUE.
| Variables | FUT | FUE | ||
|---|---|---|---|---|
| Implanted hair | 146 (100) | 49 (100) | ||
| 1,000–1,999 | 9 (6.2) | 3 (6.1) | ||
| 2,000–2,999 | 45 (30.8) | 27 (55.2) | ||
| 3,000–3,999 | 82 (56.2) | 18 (36.7) | ||
| 4,000–4,999 | 10 (6.8) | 1 (2.0) | ||
| Mean ± SD | 3,034±687.7 | 2,621±628.4 | ||
| Pain | 113 (100) | 48 (100) | ||
| Operative day | ||||
| Yes | 97 (85.8) | 10 (20.8) | ||
| No | 16 (14.2) | 38 (79.2) | ||
| 1 day after HT | ||||
| Yes | 100 (88.5) | 7 (14.6) | ||
| No | 13 (11.5) | 41 (85.4) | ||
| 7 days after HT | ||||
| Yes | 40 (34.5) | 7 (14.6) | ||
| No | 73 (65.5) | 41 (85.4) | ||
| 10 days after HT | ||||
| Yes | 33 (19.2) | 6 (12.5) | ||
| No | 80 (70.8) | 42 (87.5) | ||
| Donor site, paresthesia | 146 (100) | 49 (100) | ||
| Yes | 22 (15.1) | 0 (0) | ||
| No | 124 (84.9) | 49 (100) | ||
| Folliculitis | 146 (100) | 49 (100) | ||
| Yes | 28 (19.2) | 2 (4.1) | ||
| No | 118 (80.8) | 27 (95.9) | ||
Values are presented as absolute numbers only, mean ± standard deviation, or percentages (%).
FUT: follicular unit transplantation, FUE: follicular unit extraction, HT: hair transplantation.
Immediate postoperative pain and pain on the first postoperative day after HT were associated with the HT technique. Significantly more patients who received FUT complained of pain than those who received FUE. Moreover, there was a correlation between donor-site paresthesia and HT technique, because only patients who underwent FUT had donor-site paresthesia. Furthermore, a significantly higher proportion of patients (19.2%) who received FUT suffered scalp folliculitis, compared to patients who received FUE (4.1%).
DISCUSSION
Usually, in women, androgenetic alopecia presents at the vertex and mid-scalp regions, with relative preservation of the frontal scalp region1. In our study, most patients with FPHL who received HT were in their 40s and 50s. The mean age of participants in this cohort was similar to that of patients who had undergone HT for FPHL and were evaluated in a previous study8, and was slightly higher than that of hair-transplanted MPB patients in the study by Baser et al.9 This may be because female hair loss may appear later in life than male hair loss10. Furthermore, women have longer hair than men and can hide baldness through their hairstyle or may perceive their hair loss somewhat later.
The severity of hair loss in our participants was mostly F1 or F2 (F1 or F2 in the BASP classification is nearly the same as the L1 or L2 grade, respectively, in Ludwig Classification), and is similar to the severity mentioned in the report by Uebel8. As F1 or F2 in the BASP Classification means mild to moderate hair loss, hair-loss severity is similar to the severity of hair loss in MPB patients who received HT in the study by Baser et al.9
Prior to HT, our FPHL patients had selected various types of medical treatment, such as cosmeceuticals, minoxidil, mesotherapy and hair care shops. In our study, cosmeceuticals, but not minoxidil, was the most frequently used option. Although minoxidil is the only Food and Drug Administration-approved drug and is commonly used for FPHL, fewer people than expected used minoxidil before HT in our study. The reason for the relatively lower use of minoxidil is that Korean hair loss patients tend to seek advice from people around them or seek unapproved treatments from alternative medicine practitioners rather than visiting hospitals11. In addition, the present study has been conducted only in a professional hair transplant clinic and hospital that patients might visit only for HT. Furthermore, there is a possibility that clinicians were concerned about the vasodilatory effect of minoxidil, which may interfere with the HT.
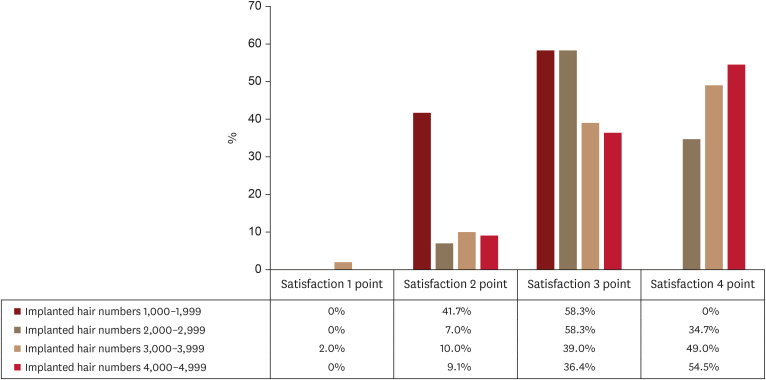
In our study, 47.2% of patients showed 75% satisfaction with the surgical results, and 41.0% of patients showed more than 90% satisfaction. The majority of people reported a high level of overall satisfaction. That was equivalent to the outcomes of HT in patients with MPB9. Considering the relative low satisfaction with medical treatment in FPHL, HT in FPHL might be a good treatment option. According to Yang Liu et al, income, education level, surgical purpose, and alopecia grade were all related to the overall satisfaction of patients with regard to HT, whereas sex, age, marriage, and family history of alopecia were not.12 In our study, the factor that correlated with satisfaction included the number of implanted hairs. The group that received a larger number of implanted hairs generally exhibited higher satisfaction points (Fig. 2).
Fig. 2. Association between implanted hair number and patient satisfaction. The group with a larger number of transplanted hairs tended to have a distribution of higher satisfaction points, while the group with a smaller number of transplanted hairs tended to have a distribution of lower satisfaction points.
Post-HT complications, such as pain, folliculitis, keloids, infection, bleeding, and facial edema, are usually manageable13,14. In the present study, postoperative pain was the most common complication. The pain VAS score indicates relatively mild pain, which might be attributable to the analgesics administered to patients after HT. In particular, immediate postoperative pain and pain on the first day after HT were associated with the HT technique. Patients who received FUT complained of pain significantly more than those who received FUE. Pain is usually one of the considerations that affect a patient’s decision about HT. Therefore, appropriate analgesia during the operation and in the postoperative period is essential, and surgeons should make every effort to reduce pain after HT.
We found that scalp folliculitis was a common complication; 15.4% of the participants experienced folliculitis of the scalp. In a study conducted by Loganathan et al.15, sterile folliculitis was found in 23.29% of patients. However, in a study conducted by Salanitri et al.13, folliculitis was only found in 1.1% of patients. Thus, studies on the incidence of folliculitis are needed. Folliculitis-related symptoms were mild and most of them improved spontaneously. More patients who received FUT experienced folliculitis than patients who received FUE. This is possible because a high implanted hair density may lead to folliculitis due to the more unregulated sebaceous glands accompanying the transplanted hairs16. Therefore, in this study, the high incidence of folliculitis in patients who underwent FUT is thought to be due to the large number of transplanted hairs rather than the characteristics of the surgery itself.
Facial edema usually occurs 4 days after the HT operation, and edema in the forehead or eyelids is a common occurrence14,15. In our study, facial edema was one of the commonest complications, and 15.9% of patients experienced post-HT facial edema. Loganathan et al. reported that 42.7% of male patients had facial edema15. In MPB, the hairs are usually implanted in the frontal and mid-scalp regions; therefore, there could be a post-HT disturbance of lymphatic flow in the frontal area, and this may cause facial edema more frequently in MPB than in FPHL.
Donor-site paresthesia was observed 11.3% of patients, but disappeared within 6 months of surgery in most patients. Only patients who received the FUT technique had donor-site paresthesia, which could have been caused by the transection of branches of the greater occipital, lesser occipital, or auriculotemporal nerves and/or aberrant neural healing12. Thus, when performing HT, it is necessary for the surgeon to cut the scalp tissue in the donor area more carefully to minimize nerve damage.
Effluvium of transplanted hair at the recipient site occurs in most patients, and effluvium of preexisting hair in the recipient area may occur after HT14. Postoperative effluvium of implanted hair typically begins 2 to 6 weeks after surgery. Recovery from recipient-site effluvium generally begins approximately 3 months after HT, when the transplanted follicles begin their new growth cycle14. In our study, 45.1% of patients suffered telogen effluvium of preexisting hair at the recipient site. Telogen effluvium of both transplanted and preexisting hair in the recipient site tends to increase the patient’s worry and anxiety about the success of HT; therefore, appropriate and substantial counseling by the clinician is essential to mitigate patient anxiety about the success of the procedure.
FUT and FUE each have pros and cons in terms of pain, scarring, and surgery time7. In this study, the FUT group had a larger number of transplanted hairs than the FUE group, leading to more satisfactory results. The FUE group had fewer postoperative complications than the FUT group, including a lower incidence of postoperative pain, donor site paresthesia, and folliculitis. However, the above results may be affected by various factors, such as the number of hairs transplanted and the patient’s overall health, as well as the hair transplant technique. Therefore, accurate comparisons between FUT and FUE are limited in this small retrospective study.
This study has limitations, including the retrospective multicenter design. First, the effect of HT was not evaluated by a physician’s global assessment, but rather by the patient’s subjective satisfaction. However, this aspect is considered a meaningful outcome because the patient’s subjective satisfaction with HT is the most important indicator of the procedure’s success. Second, only a small number of patients were included in our study. In particular, comparative analysis of FUT and FUE did not include a large number of participants. Since the 2010s, the advancement of mechanical devices has led to the increased adoption of the FUE method, accommodating varying patient preferences7. Further studies on comparative analysis are needed. Nonetheless, this study, to some extent, alleviates the paucity of studies on HT outcomes in FPHL patients. Further large-sample studies are needed to identify the clinical features of FPHL treated with HT.
In conclusion, this study could provide substantial information of HT in FPHL. Also, our study can provide the HT surgeon important information about proper initial consultation, and efficient management after HT which could lead to a good cosmetic result.
Footnotes
FUNDING SOURCE: None.
CONFLICTS OF INTEREST: The authors have nothing to disclose.
DATA SHARING STATEMENT: Research data are not shared.
References
- 1.Ramos PM, Miot HA. Female pattern hair loss: a clinical and pathophysiological review. An Bras Dermatol. 2015;90:529–543. doi: 10.1590/abd1806-4841.20153370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Penha MÁ, Santos PM, Miot HA. Dimensioning the fear of dermatologic diseases. An Bras Dermatol. 2012;87:796–799. doi: 10.1590/s0365-05962012000500027. [DOI] [PubMed] [Google Scholar]
- 3.Manabe M, Tsuboi R, Itami S, Osada SI, Amoh Y, Ito T, et al. Guidelines for the diagnosis and treatment of male-pattern and female-pattern hair loss, 2017 version. J Dermatol. 2018;45:1031–1043. doi: 10.1111/1346-8138.14470. [DOI] [PubMed] [Google Scholar]
- 4.Unger WP, Unger RH. Hair transplanting: an important but often forgotten treatment for female pattern hair loss. J Am Acad Dermatol. 2003;49:853–860. doi: 10.1016/s0190-9622(03)01568-8. [DOI] [PubMed] [Google Scholar]
- 5.Lee WS, Ro BI, Hong SP, Bak H, Sim WY, Kim DW, et al. A new classification of pattern hair loss that is universal for men and women: basic and specific (BASP) classification. J Am Acad Dermatol. 2007;57:37–46. doi: 10.1016/j.jaad.2006.12.029. [DOI] [PubMed] [Google Scholar]
- 6.Jimenez F, Ruifernández JM. Distribution of human hair in follicular units. A mathematical model for estimating the donor size in follicular unit transplantation. Dermatol Surg. 1999;25:294–298. doi: 10.1046/j.1524-4725.1999.08114.x. [DOI] [PubMed] [Google Scholar]
- 7.Collins K, Avram MR. Hair transplantation and follicular unit extraction. Dermatol Clin. 2021;39:463–478. doi: 10.1016/j.det.2021.04.003. [DOI] [PubMed] [Google Scholar]
- 8.Uebel CO, Piccinini PS, Spencer LS, da Silveira JA. Female pattern hair loss: why the follicular unit transplantation surgical technique remains a good option. Plast Reconstr Surg. 2021;147:839–849. doi: 10.1097/PRS.0000000000007760. [DOI] [PubMed] [Google Scholar]
- 9.Tan Baser N, Cigsar B, Balci Akbuga U, Terzioglu A, Aslan G. Follicular unit transplantation for male-pattern hair loss: evaluation of 120 patients. J Plast Reconstr Aesthet Surg. 2006;59:1162–1169. doi: 10.1016/j.bjps.2006.03.041. [DOI] [PubMed] [Google Scholar]
- 10.Paik JH, Yoon JB, Sim WY, Kim BS, Kim NI. The prevalence and types of androgenetic alopecia in Korean men and women. Br J Dermatol. 2001;145:95–99. doi: 10.1046/j.1365-2133.2001.04289.x. [DOI] [PubMed] [Google Scholar]
- 11.Jung JH, Kim JE, Lew BL, Sim WY, Kang H. Survey of awareness, knowledge, treatment and behavior of scalp and hair loss disorders in adults. Korean J Dermatol. 2018;56:181–187. [Google Scholar]
- 12.Liu Y, Liu F, Qu Q, Fan ZX, Miao Y, Hu ZQ. Evaluating the satisfaction of patients undergoing hair transplantation surgery using the FACE-Q scales. Aesthetic Plast Surg. 2019;43:376–382. doi: 10.1007/s00266-018-1292-x. [DOI] [PubMed] [Google Scholar]
- 13.Salanitri S, Gonçalves AJ, Helene A, Jr, Lopes FH. Surgical complications in hair transplantation: a series of 533 procedures. Aesthet Surg J. 2009;29:72–76. doi: 10.1016/j.asj.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 14.Konior RJ. Complications in hair-restoration surgery. Facial Plast Surg Clin North Am. 2013;21:505–520. doi: 10.1016/j.fsc.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 15.Loganathan E, Sarvajnamurthy S, Gorur D, Suresh DH, Siddaraju MN, Narasimhan RT. Complications of hair restoration surgery: a retrospective analysis. Int J Trichology. 2014;6:168–172. doi: 10.4103/0974-7753.142861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bunagan MJ, Pathomvanich D, Laorwong K. Recipient area folliculitis after follicular-unit transplantation: characterization of clinical features and analysis of associated factors. Dermatol Surg. 2010;36:1161–1165. doi: 10.1111/j.1524-4725.2010.01601.x. [DOI] [PubMed] [Google Scholar]