Abstract
Background
Social determinants of health (SDOH) have been associated with diabetes risk; however, their association with cardiovascular disease (CVD) events in individuals with diabetes is poorly described. We hypothesized that a greater number of SDOH among individuals with diabetes would be associated with a higher risk of CVD events.
Methods
The REasons for Geographic and Racial Differences in Stroke (REGARDS) study is a national, biracial cohort of 30,239 individuals ≥45 years old recruited in 2003–2007. We included 6,322 participants with diabetes at baseline, defined as healthcare professional diagnosis, diabetes medication use, or blood glucose values. Seven SDOH that were individually associated with CVD events were included (P<0.20). The outcome was CVD events, a composite of expert-adjudicated myocardial infarction, stroke, or cardiovascular death. We estimated Cox proportional hazard models to examine associations between number of SDOH (0, 1, 2, ≥3) and CVD events.
Results
In an age and sex adjusted model, the presence of multiple SDOH significantly increased the risk of any CVD event (hazard ratio [HR], 1.48; 95% confidence interval [CI], 1.26 to 1.74 for two SDOH; HR, 1.68; 95% CI, 1.43 to 1.96 for ≥3 SDOH). This finding was attenuated but remained statistically significant in a fully adjusted model (HR, 1.19; 95% CI, 1.01 to 1.40 for two SDOH; HR, 1.27; 95% CI, 1.07 to 1.50 for ≥3 SDOH).
Conclusion
Having multiple SDOH was independently associated with an increased risk of CVD events, a finding driven by cardiovascular death. Identifying individuals with diabetes who have multiple SDOH may be helpful for detecting those at higher risk of experiencing or dying from CVD events.
Keywords: Cardiovascular diseases, Diabetes mellitus, Myocardial infarction, Social determinants of health, Stroke
GRAPHICAL ABSTRACT
Highlights
• This study explores social determinants of health and cardiovascular events.
• Having multiple SDOH significantly increased the risk of any cardiovascular event.
• This finding was driven by cardiovascular death.
• Identifying social determinants may help detect risk of cardiovascular events.
INTRODUCTION
Diabetes is one of the leading causes of morbidity and mortality in the United States, affecting 34.1 million United States adults in 2018 [1]. Among individuals with diabetes, cardiovascular disease (CVD) is a major cause of death and disability. Globally, CVD affects approximately 32.2% of individuals diagnosed with type 2 diabetes mellitus (T2DM) [2]. The sequelae of diabetes are significant—CVD death rates are 1.7 times higher, hospitalization for heart attack is 1.8 times higher, and hospitalization for stroke is 1.5 times higher for those diagnosed with diabetes compared to those without diabetes [3]. In addition, these cardiovascular consequences are higher in women with diabetes, who have a greater relative risk of developing myocardial infarction (MI), fatal coronary heart disease, and stroke [4]. CVD accounts for approximately half of all deaths among those with type 1 diabetes mellitus and T2DM, highlighting the importance of understanding the relationship between diabetes and CVD [2,5].
Social determinants of health (SDOH), such as income, education, housing, and access to nutritious food, have been shown to influence the development of diabetes and diabetes clinical outcomes [6]. A systematic review by Walker et al. [7] reported that beyond racial and ethnic differences in diabetes outcomes, psychosocial factors (e.g., self-efficacy, depression, social support) and neighborhood factors (e.g., food insecurity, social cohesion, neighborhood esthetics) were associated with glycemic control, low-density lipoprotein (LDL), and blood pressure. However, the review also found at the time that many scientific reports were only tangentially related to SDOH and did not explicitly examine their influence on outcomes [6]. Recent analyses of the REasons for Geographic and Racial Differences in Stroke (REGARDS) study have demonstrated that SDOH often cluster within individuals and multiple SDOH can affect health outcomes including incident coronary heart disease, incident heart failure hospitalization, 90-day mortality after discharge for heart failure, and incident stroke [8-14]. Though there is also evidence on the impact of multiple SDOH on diabetes incidence, to date, the influence of within-person multiple SDOH on clinical outcomes, such as cardiovascular risk, in patients with diabetes is not well described [13].
The combined effect of multiple vulnerabilities, such as poverty, lack of social support, and limited access to healthcare are likely to exert a larger influence on CVD in adults with diabetes than any one SDOH alone. The self-reported and rigorously assessed physiologic data and expert-adjudicated CVD endpoints of the national biracial REGARDS cohort offers a unique opportunity to examine the association of multiple SDOH and cardiovascular risk among the populations most vulnerable to poor diabetes outcomes. We hypothesized that in individuals with diabetes, a greater number of SDOH vulnerabilities would be associated with a higher risk for cardiovascular events.
METHODS
Study population
This study was approved by Institutional Review Boards of Weill Cornell Medical College (IRB No. 1603017100) and participating institutions, and all participants provided written informed consent. REGARDS is a longitudinal, observational cohort study of 30,239 community-dwelling individuals ≥45 years of age living in the 48 contiguous United States and District of Columbia. Participants were enrolled between January 2003 and October 2007. The primary objective of the REGARDS study was to determine the causes for excess stroke mortality in the Southeastern United States and among African Americans. As a result, study participants were oversampled from the Stroke Buckle (coastal areas of Georgia, North Carolina, and South Carolina) and Stroke Belt (remaining areas of Georgia, North Carolina, South Carolina, Louisiana, Arkansas, Alabama, Tennessee, and Mississippi). At baseline (2003 to 2007), participant information including sociodemographic information, medical history, and risk factors were collected via computer assisted telephone interview, followed by an in-home visit in which physiological parameters (height, weight, blood pressure), electrocardiography, and urine and blood samples. Labs were assessed at the study’s central laboratory at the University of Vermont. Medication inventory was also performed through pill bottle review. Participants were contacted every 6 months for the next ≥10 years to assess health status. Further details on the REGARDS methodology have been described previously [15].
For this study, we selected REGARDS participants with complete information on diabetes status at baseline. This includes participants with a self-reported diagnosis of diabetes from a healthcare professional, participants being treated with diabetes medications or insulin, or participants with a fasting glucose ≥126 mg/dL or random glucose ≥200 mg/dL.
Outcomes: incident and recurrent MI, stroke, and fatal cardiovascular disease
Incident and recurrent MI, stroke, and CVD death were based on expert adjudication after medical record review. MI events were defined as (1) a clinical presentation consistent with ischemia; (2) a rising and/or falling pattern of troponin over at least 6 hours with a peak at least twice the upper limit of normal; or (3) imaging findings consistent with ischemia. Stroke events were defined as (1) focal neurological deficit consistent with ischemia lasting for >24 hours and confirmed with medical records; (2) clinical strokes (focal or nonfocal neurological deficit with diagnostic brain imaging regardless of symptom duration); and (3) expert-adjudicated stroke deaths. Events were adjudicated through examination of medical records and disagreements were resolved by committee.
Cardiovascular death was defined as death from definite, probable, or possible MI, stroke, sudden death, heart failure, other cardiac cause, or not cardiac but other cardiovascular cause. The main underlying cause of death was determined by two trained adjudicators who examined all available information including interviews with next of kin, death certificates, autopsy reports, medical history, and the National Death Index. Events through December 31, 2018 were available for this study.
Primary exposure: social determinants of health
The primary exposures were SDOH, guided by the Agency for Healthcare Research and Quality National Healthcare Quality and Disparities Report [16] and the Center for Disease Control Health Disparities and Inequalities Report [17] and categorized according to five domains of the Healthy People 2030 framework of SDOH [18]. We selected nine candidate SDOH shown to associated with health outcomes in CVD more broadly, an approach that has been used previously by other REGARDS investigators [8-14]. Each SDOH was dichotomized and investigated separately for their association with CVD. The social and community context domain included social isolation, determined through questions regarding not seeing friends or family members in the past month or not having someone to care for you if you became ill. The education domain included educational attainment less than high school. The economic stability domain included annual household income ≤$35,000. The health and health care domain included residence in a healthcare professional shortage area, lacking health insurance, and residence in a state in the bottom 20% of United States states for at least 8 years of a 10-year (1993 to 2002) period of a measure of public health infrastructure derived from America’s Health Ranking. The neighborhood and built environment domain included rural residence and residing in a zip code with >25% of residents living below the federal poverty line.
Covariates
Baseline covariates included sociodemographics, medical conditions, medications, health status, health behaviors, and physiological factors. Sociodemographics included age, race, sex, and residence in the Stroke Belt or Buckle. Medical conditions included history of hypertension (self-report, use of antihypertensive medication, or systolic/diastolic blood pressure ≥140/90 mmHg), hyperlipidemia (self-report, use of lipid-lowering medications, total cholesterol ≥200 mg/dL, high-density lipoprotein cholesterol [HDL-C] <40 mg/dL, or LDL cholesterol >100 mg/dL), heart disease (self-reported MI, coronary artery bypass grafting, angioplasty, stenting, or evidence of MI from initial electrocardiogram), or stroke (self-report). Medications included use of baseline antihypertensives, statins, or insulin. Health status was assessed using Physical Component Summary and Mental Component Summary scores from the Short Form-12. Health behaviors included cigarette smoking, risky alcohol consumption (heavy drinking based on sex-specific National Institute of Alcohol Abuse and Alcoholism cut points vs. moderate or no consumption), physical activity (1 or more times per week of exercise vs. none), adherence to the Mediterranean diet using the Mediterranean diet score (≥6 as adherent), and adherence to medications without regard to specific medications (any adherence vs. none) [19]. Physiological factors included body mass index (BMI), systolic blood pressure, diastolic blood pressure, total cholesterol, HDL-C, C-reactive protein, urinary albumin-to-creatinine ratio, and estimated glomerular filtration rate.
Statistical analysis
We first examined bivariate associations between each dichotomized candidate SDOH and time to composite endpoint of MI, stroke, or cardiovascular death using Cox proportional hazards models adjusted for sex and age at baseline. SDOH that demonstrated a statistically significant association at the P<0.20 level with the composite endpoint were retained for further analysis. We then evaluated correlations among all selected SDOH to confirm the absence of multicollinearity. Using the smaller list of SDOH, we created a count of SDOH (0, 1, 2, 3, or more), which became our main exposure.
We evaluated age-adjusted incidence rates per 1,000 person-years of the composite outcome (MI, stroke, or cardiovascular death), and for each outcome separately. To determine the independent effects of SDOH count on time to event for MI/stroke/cardiovascular death, we first estimated Cox proportional hazards model adjusted only for age and sex. We then sequentially adjusted for covariates in groups: (1) sociodemographics, (2) medical conditions, (3) medications, (4) health status, (5) health behaviors, and (6) physiological factors, observing changes in the direction and magnitude of the associations with SDOH count. We tested interactions between the SDOH count and age, race, insulin use, and history of CVD. We evaluated Kaplan-Meier survival curves of the SDOH count for the composite outcome as well as for individual outcomes (MI, stroke, and cardiovascular death), and compared survival curves using log-rank test.
We then determined the effect of a greater number of SDOH on time to each outcome separately (MI, stroke, or cardiovascular death). We fitted a minimally adjusted Cox model, adjusting for age and gender, and fully adjusted Cox models (adjusted for sociodemographics, medical conditions, medications, health status, health behaviors, physiological factors) for each of these outcomes separately.
We performed multiple imputations by chained equations to address missing data [20]. All analyses were conducted in STATA version 14 (StataCorp., College Station, TX, USA), R version 4.0.5 (R Foundation for Statistical Computing, Vienna, Austria), and SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
RESULTS
The study sample included 6,322 individuals with diabetes at baseline. The follow-up period of the REGARDS study is still ongoing. For this study, data through December 2018 were available and the median follow-up time was 8.7 years (interquartile range, 4.4 to 12.4). Individuals who died due to other causes were censored at the time of death (see Supplementary Fig. 1 for exclusion cascade).
Selection of SDOH
Table 1 displays the minimally adjusted associations and P values for the nine considered SDOH and the composite endpoint of MI, stroke, or cardiovascular death. The SDOH associated with the composite endpoint at P<0.20 were retained for further analysis. The inclusion of SDOH variables based on a P value threshold of <0.20 was based on previously published REGARDS methodology and was also influenced by recent literature on the reporting and interpretation of P values in epidemiological and medical research [12,21,22]. The seven SDOH associated with the composite endpoint at P<0.20 and retained for further analysis were social isolation from friends/family, social isolation from caregivers, low education, low income, zip code level poverty, residence in a healthcare professional shortage area, and lack of health insurance.
Table 1.
Bivariate associations between SDOH and composite endpoint (myocardial infarction/stroke/cardiovascular death)
| Healthy People 2030 domain | SDOH | HR (95% CI) | P value |
|---|---|---|---|
| Social and community context | Social isolation from friends/familya,b | 1.33 (1.09–1.62) | 0.004 |
| Social isolation from caregiversa,c | 1.19 (1.04–1.36) | 0.014 | |
| Education | Low education (<high school)a | 1.32 (1.18–1.48) | <0.001 |
| Economic stability | Low annual household income (<$35,000)a | 1.57 (1.40–1.75) | <0.001 |
| Neighborhood/built environment | Zip code level povertya,d | 1.11 (1.00–1.24) | 0.046 |
| Rural residence | 1.02 (0.73–1.42) | 0.899 | |
| Health and healthcare | Residence in HPSAa | 1.09 (1.00–1.20) | 0.065 |
| Lack of health insurancea | 1.15 (0.94–1.42) | 0.176 | |
| Poor state public health infrastructuree | 1.02 (0.93–1.13) | 0.665 |
SDOH, social determinants of health; HR, hazard ratio; CI, confidence interval; HPSA, Health Professional Shortage Area.
P<0.20,
Social isolation from friends/family defined as those who have 0 or 1 friend/family that they have seen in the past month,
Social isolation from caregivers defined as participants who reported they had no one to care for them if they became ill,
Zip code level poverty defined as residence in zip code with >25% of residents living below the federal poverty line,
Public health infrastructure vulnerability includes nine states whose ranking had been in the bottom 20% for poor health infrastructure for greater than or equal to 80% of the time between 1993 and 2002.
The time period reflects the 10 years preceding when REasons for Geographic and Racial Differences in Stroke (REGARDS) baseline data collection started in 2003.
Baseline characteristics of participants
Participants characteristics by number of SDOH are displayed in Table 2. The median age of the sample at baseline was 66±9 years; 53% were female and 58% were Black. Participants with a greater burden of SDOH were more likely to be older, female, Black, have hypertension, have hyperlipidemia, use insulin, and have poorer physical and mental functioning. Those participants also had higher BMI, higher blood pressure, higher total and HDL-C, C-reactive protein >3 mg/L, urinary albumin-to-creatinine ration >30 mg/g, and higher estimated glomerular filtration rate. The variables with the highest proportion of missing data were dietary patterns (39.0%), income (12.8%), and C-reactive protein values (7.3%).
Table 2.
Characteristics of participants in the REGARDS study with diabetes at baseline, by count of SDOH
| Characteristic | 0 SDOH | 1 SDOH | 2 SDOH | ≥3 SDOH | P value |
|---|---|---|---|---|---|
| Number | 859 | 1,524 | 1,326 | 1,566 | - |
| Events (composite) | 194 (22.6) | 387 (25.4) | 400 (30.2) | 490 (31.3) | <0.001 |
| Social determinants | |||||
| Less than high school education | 0 | 34 (2.2) | 245 (18.5) | 775 (49.5) | <0.001 |
| <$35,000 Annual household income | 0 | 726 (47.6) | 1,042 (78.6) | 1,378 (88.0) | <0.001 |
| Zip code poverty (>25% residents living below federal poverty line) | 0 | 115 (7.5) | 317 (23.9) | 973 (62.1) | <0.001 |
| Residence in HPSA | 0 | 527 (34.6) | 680 (51.3) | 1,170 (74.7) | <0.001 |
| Lack of health insurance | 0 | 20 (1.3) | 82 (6.2) | 300 (19.2) | <0.001 |
| Social isolation (caregivers)a | 0 | 74 (4.9) | 219 (16.5) | 494 (31.5) | <0.001 |
| Social isolation (friends/family)b | 0 | 28 (1.8) | 67 (5.1) | 192 (12.3) | <0.001 |
| Sociodemographics | |||||
| Age, yr | 63.7±8.1 | 65.2±8.7 | 66.1±8.7 | 66.0±8.7 | <0.001 |
| Male sex | 558 (65.0) | 821 (53.9) | 609 (45.9) | 571 (36.5) | <0.001 |
| Black | 345 (40.2) | 713 (46.8) | 791 (59.7) | 1,201 (76.7) | <0.001 |
| Stroke Belt or Stroke Buckle | 538 (62.6) | 862 (56.6) | 747 (56.3) | 894 (57.1) | 0.008 |
| Medical conditions | |||||
| Hypertension | 624 (72.6) | 1,186 (77.8) | 1,037 (78.2) | 1,300 (83.0) | <0.001 |
| Hyperlipidemia | 618 (71.9) | 1,134 (74.4) | 900 (67.9) | 1,047 (66.9) | <0.001 |
| History of heart disease | 215 (25.0) | 416 (27.3) | 369 (27.8) | 427 (27.3) | 0.407 |
| History of stroke | 64 (7.5) | 144 (9.4) | 152 (11.5) | 210 (13.4) | <0.001 |
| Medications | |||||
| Antihypertensives | 598 (69.6) | 1,152 (75.6) | 1,006 (75.9) | 1,257 (80.3) | <0.001 |
| Statin | 434 (50.5) | 773 (50.7) | 631 (47.6) | 714 (45.6) | 0.017 |
| Insulin | 197 (22.9) | 366 (24.0) | 363 (27.4) | 491 (31.4) | <0.001 |
| Not taking any diabetes medications | 95 (11.1) | 186 (12.2) | 130 (9.8) | 158 (10.1) | 0.110 |
| Health status | |||||
| SF-12 physical component scorec | 45.2±10.8 | 43.2±11.2 | 40.7±11.5 | 40.0±11.2 | <0.001 |
| SF-12 mental component scorec | 55.4±7.2 | 54.6±8.2 | 53.2±9.2 | 50.8±11.0 | <0.001 |
| Health behaviors | |||||
| Current cigarette smoking | 97 (11.3) | 163 (10.7) | 210 (15.8) | 287 (18.3) | <0.001 |
| Risky alcohol consumption | 20 (2.3) | 32 (2.1) | 19 (1.4) | 26 (1.7) | 0.390 |
| Physical activityd | 550 (64.0) | 912 (59.8) | 779 (58.7) | 811 (51.8) | <0.001 |
| High adherence to Mediterranean diet | 154 (17.9) | 228 (15.0) | 168 (12.7) | 172 (11.0) | 0.039 |
| Adherence to medications | 558 (65.0) | 1,030 (67.6) | 886 (66.8) | 1,010 (64.5) | 0.170 |
| Physiological factors | |||||
| BMI, kg/m2 | 31.8±5.9 | 32.4±6.6 | 32.4±6.8 | 32.7±6.9 | 0.032 |
| Systolic blood pressure, mm Hg | 128.8±14.9 | 131.3±16.9 | 131.7±17.1 | 134.3±18.1 | <0.001 |
| Diastolic blood pressure, mm Hg | 75.5±9.5 | 76.4±10.0 | 76.3±10.4 | 77.7±11.1 | <0.001 |
| Total cholesterol, mg/dL | 176.4±38.7 | 176.6±39.7 | 181.2±42.8 | 183.8±42.4 | <0.001 |
| HDL-C, mg/dL | 43.0 (36.0–52.5) | 43.0 (36.0–52.0) | 45.0 (37.0–54.0) | 46.0 (38.0–56.0) | <0.001 |
| C-reactive protein >3 mg/L | 337 (39.2) | 682 (44.8) | 628 (47.4) | 786 (50.2) | <0.001 |
| Urinary albumin/creatinine ratio >30 mg/g | 207 (24.1) | 403 (26.4) | 412 (31.1) | 502 (32.1) | <0.001 |
| eGFR <60 mL/min/1.73 m2 | 130 (15.1) | 259 (17.0) | 267 (20.1) | 304 (19.4) | 0.005 |
| Fasting glucose level, mg/dL | 136.0±52.3 | 136.5±50.9 | 140.0±56.3 | 144.9±59.3 | <0.001 |
| Non-fasting glucose level, mg/dL | 163.4±66.6 | 170.3±75.1 | 172.2±80.0 | 174.5±73.5 | 0.611 |
Values are presented as number (%), mean±standard deviation, or median (interquartile range). Percentage calculations do not include missing values in denominator.
REGARDS, REasons for Geographic and Racial Differences in Stroke; SDOH, social determinants of health; HPSA, Health Professional Shortage Area; SF-12, 12-Item Short Form Health Survey; BMI, body mass index; HDL-C, high-density lipoprotein cholesterol; eGFR, estimated glomerular filtration rate.
Social isolation from caregivers defined as participants who reported they had no one to care for them if they became ill,
Social isolation from friends/family defined as those who have 0 or 1 friend/family that they have seen in the past month,
Range 0 to 100 with higher scores indicating better physical functioning,
Getting enough physical activity to work up a sweat on most days of the week.
SDOH and time to cardiovascular events
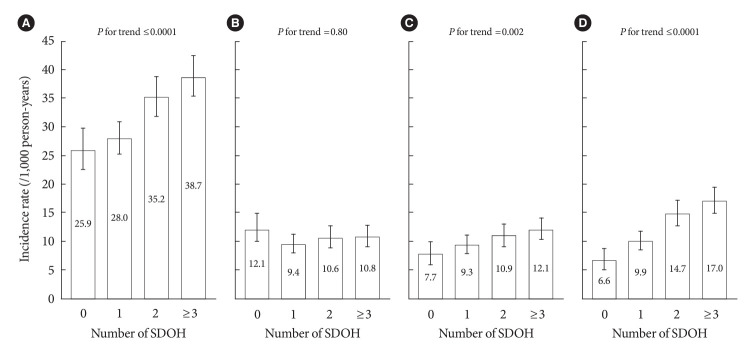
A total of 1,775 cardiovascular events were observed over a median follow-up time of 8.7 years in participants with diabetes at baseline. Of these, 194 events (23%) occurred among participants with no SDOH, 387 (25%) occurred among participants with one SDOH, 400 (30%) occurred among participants with two SDOH, and 490 (31%) occurred among participants with three or more SDOH. Age-adjusted incidence rates of the composite endpoint and individual endpoints of stroke and cardiovascular death increased with increasing numbers of SDOH (Fig. 1). The incidence of the composite endpoint was 1.5 times higher for those with ≥3 SDOH (38.7/1,000 person-years) compared with those without any SDOH (25.9/1,000 person-years). As the number of SDOH increased, participants had a progressively lower survival probability (Supplementary Fig. 2). The log-rank test P value was <0.0001 for differences in survival among the different SDOH groups.
Fig. 1.
Number of social determinants of health (SDOH) and incidence of (A) composite endpoint, (B) myocardial infarction, (C) stroke, and (D) cardiovascular death in the REasons for Geographic and Racial Differences in Stroke (REGARDS) study.
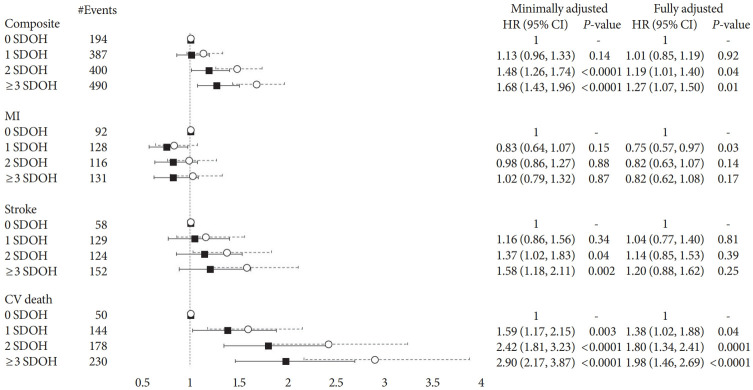
Number of SDOH and hazard of cardiovascular events
In a fully adjusted model, the presence two or more SDOH significantly increased the risk of CVD events (hazard ratio [HR], 1.19; 95% confidence interval [CI], 1.01 to 1.40 for two SDOH; HR, 1.27; 95% CI, 1.07 to 1.50 for ≥3 SDOH) (Fig. 2). There was no association for incident or recurrent MI or stroke. However, there was a graded association for cardiovascular death beginning at one SDOH (HR, 1.38; 95% CI, 1.02 to 1.88 for one SDOH; HR, 1.80; 95% CI, 1.34 to 2.41 for two SDOH; HR, 1.98; 95% CI, 1.46 to 2.69 for ≥3 SDOH). The stepwise results of the modeling process, adjusting for demographic characteristics, medical conditions, medication use, functional status, health behaviors, and physiologic factors, are presented in Supplementary Table 1. Addition of medical conditions, functional status, and physiologic factors produced the largest attenuation. There were no interactions between the composite endpoint and age, gender, and insulin use (P>0.10). There was an interaction between history of CVD and the composite endpoint (P=0.03) and a stratified analysis is presented in Supplementary Table 2.
Fig. 2.
Hazard ratios of composite endpoint, myocardial infarction (MI), stroke, and cardiovascular (CV) death from minimally and fully adjusted models, by number of social determinants of health (SDOH), in the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Black square=fully adjusted; white circle=minimally adjusted. Minimally adjusted model adjusts for age and sex. Fully adjusted model adjusts for sociodemographics, medical conditions, medications, health status, health behaviors, and physiological factors. HR, hazard ratio; CI, confidence interval.
DISCUSSION
In this study of a national, biracial prospective cohort of individuals with diabetes, we observed an increased risk of cardiovascular events (MI, stroke, or cardiovascular death) with an increasing number of SDOH. The incidence of cardiovascular events in individuals with two SDOH was nearly 50% higher and with ≥3 SDOH was 68% higher than in those with no SDOH. In a fully adjusted model, individuals with two SDOH had a 19% higher and ≥3 SDOH had a 27% higher risk of cardiovascular events compared with those with none. The mechanism through which SDOH exerted their influence may have been in part due to the greater burden of chronic medical conditions, lower functional status, and worse risk factor control among those with a greater burden of SDOH, but SDOH maintained an independent association even after controlling for these factors. Similar patterns were seen individually for stroke and cardiovascular death, but not for MI.
Prior studies of SDOH and their influence on diabetes outcomes have primarily focused on measures of diabetes management, such as glycemic control, blood pressure, and cholesterol [6,7]. A systematic review by Walker et al. [7] found that when categorizing by the Healthy People 2020 framework, most studies investigating SDOH and diabetes outcomes tended to examine economic stability, social and community context, and health and health care, while fewer investigated education or neighborhood and built environment, and no studies investigated all five categories simultaneously. Recent studies have examined SDOH and measures of diabetes control, but few have examined SDOH and risk for cardiovascular events [23-28]. By examining the cumulative burden of SDOH and its association with cardiovascular events, our study offers a broader look at how social disadvantage can affect cardiovascular risk in individuals with diabetes beyond the known burden of chronic diseases and physiologic factors.
Our study also elucidates the high burden of chronic disease in individuals with diabetes and its impact on cardiovascular outcomes, especially for those with multiple SDOH. Diabetes is a well-known risk factor for CVD, including coronary heart disease and stroke [29-32]. Previous REGARDS research has demonstrated the age-adjusted incidence for fatal coronary heart disease in the general study population to be far below the incidence demonstrated in this study of individuals with diabetes only. Although not a direct comparison, as our study examined cardiovascular death encompassing events beyond coronary heart disease, the incidence of cardiovascular death in our study was five times higher than the incidence of fatal coronary heart disease in the general study population with no SDOH (6.6 vs. 1.3/1,000 person-years) and increasing to nearly six times higher in individuals with ≥3 SDOH (17.0 vs. 2.9/1,000 person-years) [10]. This increase in incidence across groups of SDOH may also imply that an increasing number of SDOH is further contributing to the risk of cardiovascular death events in individuals with diabetes.
In our analyses, we found a graded association between the number of SDOH and the risk of cardiovascular events in individuals with diabetes, consistent with previous REGARDS studies, which have demonstrated greater risk of incident fatal coronary heart disease, stroke, and heart failure with increased number of SDOH in the general population [9,10,14]. Several psychological, behavioral, and biological mechanisms have been hypothesized for the impact of SDOH on cardiovascular health, and our study demonstrated evidence of these influences [33]. Chronic negative psychological states including stress, depression, anxiety, or isolation, may result in dysregulation of the autonomic nervous system and increased allostatic stress response [34-36]. Two of the main SDOH included in our study examined social isolation from friends, family, or caregivers, which when added together, may further aggregate into psychological mechanisms for worse CVD outcomes. In diabetes, behavioral mechanisms may have a particularly large impact, as diabetes is a chronic disease requiring regular glucose control and medication adherence [37].
Over the past two decades, the mortality and incidence of CVD events has declined substantially among individuals with diabetes, likely due to advances in integrated care of patients with chronic diseases, improved patient education, and improved management of risk factors such as hypertension, cholesterol, and glycemic control [38]. In our study, individuals with ≥3 SDOH had a hazard of 1.68 that reduced to 1.27 after adjusting for risk factors such as medical conditions, medications, health behaviors, and physiologic factors. However, our study also demonstrates the magnitude of the residual risk not attributable to those risk factors. Assessing these SDOH vulnerabilities may help identify high-risk individuals who can be targeted for intervention. Incorporating SDOH into risk prediction tools for CVD in diabetes could aid clinicians in further identifying individuals vulnerable to CVD events. Existing tools rely mostly on clinical and physiologic characteristics such as glycemic control, blood pressure, and medication use, with only the QRISK2 score incorporating the Townsend social deprivation score [39-43]. As such, further expanding risk assessment tools to incorporate SDOH may increase their predictive value. Population health managers may also be able to use a simple count of SDOH to identify individuals at greatest need of intervention.
In our study, individuals with greater number of SDOH had higher levels of antihypertensive medication use and lower levels of statin use, which provides an interesting insight into how health system interventions can impact individuals. Previous REGARDS research demonstrated that only 54% of Black women who have indications for statin prescriptions are actually prescribed the medication compared to 66% of White men [11]. As seen in Table 2, the proportion of both men and White individuals decreases as SDOH increase. Therefore, the higher population of black individuals in our population with a greater number of SDOH may drive lower rates of hyperlipidemia, as it is historically underdiagnosed in the population, as well as the lower level of statin prescriptions as they are also historically less likely to be prescribed statins even when indicated. When comparing the use of antihypertensive medications to statin medications, research has shown that there has been much more increasing awareness and treatment of hypertension across all racial groups, especially with the Healthy People campaigns [44,45]. Our results both reflect the prior success of health system interventions on hypertension yet also highlight the persistent need for systematic interventions for atherosclerotic disease prevention.
Our study’s strengths include a large, national sample with rigorously collected data and adjudicated cardiovascular endpoints, as well as the collection of multiple SDOH across all five domains of the Healthy People framework. The limitations of our study include the use of some self-reported variables in data collection, as well as the use of SDOH characteristics from the baseline survey of participants, which may have occurred several years before cardiovascular events. The study was also observational in nature, and causal inferences cannot be made. In addition, although we found a graded association for the composite endpoint (which included both incident and recurrent events) and stroke and cardiovascular death individually, there was no association between number of SDOH and MI in the minimally or fully adjusted models. This lack of association is difficult to explain and has not been seen in previous REGARDS studies examining incident nonfatal MI, thus presenting an area for further investigation [10]. Last, no direct measures of diabetes duration or severity were available, thus since this sample of older adults includes T2DM patients, we used insulin as a proxy for duration and severity.
In conclusion, we found a graded association between number of SDOH and risk of CVD events in individuals with diabetes, independent of a host of covariates including demographics, medical conditions, and other physiologic factors. These findings suggest that SDOH have an independent effect on cardiovascular events in individuals with diabetes, beyond measures of diabetes control such as glycemic control and blood pressure management. Counting and aggregating SDOH in individuals with diabetes may help elucidate those at higher risk of experiencing or dying from CVD events, allowing clinicians, healthcare professionals, and population health managers to target and intervene in those most vulnerable to poor health outcomes.
Acknowledgments
The authors thank the other investigators, the staff, and the participants of the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at: https://www.uab.edu/soph/regardsstudy.
Footnotes
CONFLICTS OF INTEREST
April Carson and Monika M. Safford have received investigator-initiated support from Amgen, Inc. for work unrelated to this work. Doyle M. Cummings has received research grant funding from Novo Nordisk Pharmaceuticals for research unrelated to this work. Raegan W. Durant has received research grant funding from Amarin Corporation unrelated to this work. Monika M. Safford is the founder of the company Patient Activated Learning System, Inc., which is not related to the current article. No other potential conflicts of interest were reported.
AUTHOR CONTRIBUTIONS
Conception or design: L.Z., M.M.S.
Acquisition, analysis, or interpretation of data: all authors.
Drafting the work or revising: all authors.
Final approval of the manuscript: all authors.
FUNDING
This research project is supported by cooperative agreement U01 NS041588 co-funded by the National Institute of Neurological Disorders and Stroke (NINDS) and the National Institute on Aging (NIA), National Institutes of Health, Department of Health and Human Service. The content is solely the responsibility of the authors and does not necessarily represent the off icial views of the NINDS or the NIA. Representatives of the NINDS were involved in the review of the manuscript but were not directly involved in the collection, management, analysis, or interpretation of the data.
Additional funding was provided by grants R01HL080477 and K01HL133468 from the National Heart, Lung, and Blood Institute. Representatives from National Heart, Lung, and Blood Institute did not have any role in the design and conduct of the study, the collection, management, analysis, and interpretation of the data, or the preparation or approval of the article.
SUPPLEMENTARY MATERIALS
Supplementary materials related to this article can be found online at https://doi.org/10.4093/dmj.2023.0380.
Multiply imputed effect of SDOH count on composite endpoint
HRs of composite endpoint in individuals without and with history of heart disease from minimally and fully adjusted models, by number of SDOH
Exclusion cascade for number of social determinants of health and composite endpoint. REGARDS, REasons for Geographic and Racial Differences in Stroke.
Kaplan-Meier curve by number of social determinants of health (SDOH) and composite endpoint.
REFERENCES
- 1.Centers for Disease Control and Prevention . National diabetes statistics report, 2020. Atlanta: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2020. [Google Scholar]
- 2.Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol. 2018;17:83. doi: 10.1186/s12933-018-0728-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention . National diabetes statistics report, 2014. Atlanta: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2014. [Google Scholar]
- 4.Recarti C, Sep SJ, Stehouwer CD, Unger T. Excess cardiovascular risk in diabetic women: a case for intensive treatment. Curr Hypertens Rep. 2015;17:554. doi: 10.1007/s11906-015-0554-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H. Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia. 2001;44 Suppl 2:S14–21. doi: 10.1007/pl00002934. [DOI] [PubMed] [Google Scholar]
- 6.Walker RJ, Strom Williams J, Egede LE. Influence of race, ethnicity and social determinants of health on diabetes outcomes. Am J Med Sci. 2016;351:366–73. doi: 10.1016/j.amjms.2016.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Walker RJ, Smalls BL, Campbell JA, Strom Williams JL, Egede LE. Impact of social determinants of health on outcomes for type 2 diabetes: a systematic review. Endocrine. 2014;47:29–48. doi: 10.1007/s12020-014-0195-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joseph JJ, Bennett A, Echouffo Tcheugui JB, Effoe VS, Odei JB, Hidalgo B, et al. Ideal cardiovascular health, glycaemic status and incident type 2 diabetes mellitus: the REasons for Geographic and Racial Differences in Stroke (REGARDS) study. Diabetologia. 2019;62:426–37. doi: 10.1007/s00125-018-4792-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pinheiro LC, Reshetnyak E, Sterling MR, Levitan EB, Safford MM, Goyal P. Multiple vulnerabilities to health disparities and incident heart failure hospitalization in the REGARDS study. Circ Cardiovasc Qual Outcomes. 2020;13:e006438. doi: 10.1161/CIRCOUTCOMES.119.006438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Safford MM, Reshetnyak E, Sterling MR, Richman JS, Muntner PM, Durant RW, et al. Number of social determinants of health and fatal and nonfatal incident coronary heart disease in the REGARDS study. Circulation. 2021;143:244–53. doi: 10.1161/CIRCULATIONAHA.120.048026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schroff P, Gamboa CM, Durant RW, Oikeh A, Richman JS, Safford MM. Vulnerabilities to health disparities and statin use in the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study. J Am Heart Assoc. 2017;6:e005449. doi: 10.1161/JAHA.116.005449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sterling MR, Ringel JB, Pinheiro LC, Safford MM, Levitan EB, Phillips E, et al. Social determinants of health and 90-day mortality after hospitalization for heart failure in the REGARDS study. J Am Heart Assoc. 2020;9:e014836. doi: 10.1161/JAHA.119.014836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ringel JB, Carson AP, Cummings DM, Pena J, Gamboa C, Schroff P, et al. Abstract MP01: Multiple social determinants of health disparities increase the risk of diabetes and mortality in the Reasons for Geographic and Racial Differences in Stroke Study. Circulation. 2020;141(Suppl 1):AMP01. [Google Scholar]
- 14.Reshetnyak E, Ntamatungiro M, Pinheiro LC, Howard VJ, Carson AP, Martin KD, et al. Impact of multiple social determinants of health on incident stroke. Stroke. 2020;51:2445–53. doi: 10.1161/STROKEAHA.120.028530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25:135–43. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 16.Agency for Healthcare Research and Quality . 2021 National healthcare quality and disparities report. Rockville: Agency for Healthcare Research and Quality; 2021. [Google Scholar]
- 17.Frieden TR, Centers for Disease Control and Prevention (CDC) CDC health disparities and inequalities report-United States, 2013. Foreword. MMWR Suppl. 2013;62:1–2. [PubMed] [Google Scholar]
- 18.Office of Disease Prevention and Health Promotion Healthy People 2030. Available from: https://health.gov/healthypeople/objectives-and-data/browse-objectives/diabetes (cited 2024 May 10)
- 19.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45:1–67. [Google Scholar]
- 21.Aguinis H, Vassar M, Wayant C. On reporting and interpreting statistical significance and p values in medical research. BMJ Evid Based Med. 2021;26:39–42. doi: 10.1136/bmjebm-2019-111264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amrhein V, Greenland S, McShane B. Scientists rise up against statistical significance. Nature. 2019;567:305–7. doi: 10.1038/d41586-019-00857-9. [DOI] [PubMed] [Google Scholar]
- 23.Patel MR. Social determinants of poor management of type 2 diabetes among the insured. Curr Diab Rep. 2020;20:67. doi: 10.1007/s11892-020-01354-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Le-Scherban F, Ballester L, Castro JC, Cohen S, Melly S, Moore K, et al. Identifying neighborhood characteristics associated with diabetes and hypertension control in an urban AfricanAmerican population using geo-linked electronic health records. Prev Med Rep. 2019;15:100953. doi: 10.1016/j.pmedr.2019.100953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McDoom MM, Cooper LA, Hsu YJ, Singh A, Perin J, Thornton RL. Neighborhood environment characteristics and control of hypertension and diabetes in a primary care patient sample. J Gen Intern Med. 2020;35:1189–98. doi: 10.1007/s11606-020-05671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walker RJ, Garacci E, Palatnik A, Ozieh MN, Egede LE. The longitudinal influence of social determinants of health on glycemic control in elderly adults with diabetes. Diabetes Care. 2020;43:759–66. doi: 10.2337/dc19-1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hill-Briggs F, Adler NE, Berkowitz SA, Chin MH, Gary-Webb TL, Navas-Acien A, et al. Social determinants of health and diabetes: a scientific review. Diabetes Care. 2020;44:258–79. doi: 10.2337/dci20-0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cummings DM, Patil SP, Long DL, Guo B, Cherrington A, Safford MM, et al. Does the association between hemoglobin A1c and risk of cardiovascular events vary by residential segregation?: the REasons for Geographic And Racial Differences in Stroke (REGARDS) Study. Diabetes Care. 2021;44:1151–8. doi: 10.2337/dc20-1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Preis SR, Pencina MJ, Hwang SJ, D’Agostino RB, Sr, Savage PJ, Levy D, et al. Trends in cardiovascular disease risk factors in individuals with and without diabetes mellitus in the Framingham Heart Study. Circulation. 2009;120:212–20. doi: 10.1161/CIRCULATIONAHA.108.846519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chiha M, Njeim M, Chedrawy EG. Diabetes and coronary heart disease: a risk factor for the global epidemic. Int J Hypertens. 2012;2012:697240. doi: 10.1155/2012/697240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Glovaci D, Fan W, Wong ND. Epidemiology of diabetes mellitus and cardiovascular disease. Curr Cardiol Rep. 2019;21:21. doi: 10.1007/s11886-019-1107-y. [DOI] [PubMed] [Google Scholar]
- 32.Dal Canto E, Ceriello A, Ryden L, Ferrini M, Hansen TB, Schnell O, et al. Diabetes as a cardiovascular risk factor: an overview of global trends of macro and micro vascular complications. Eur J Prev Cardiol. 2019;26(2 suppl):25–32. doi: 10.1177/2047487319878371. [DOI] [PubMed] [Google Scholar]
- 33.Havranek EP, Mujahid MS, Barr DA, Blair IV, Cohen MS, Cruz-Flores S, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–98. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 34.Christensen AJ, Smith TW. Cynical hostility and cardiovascular reactivity during self-disclosure. Psychosom Med. 1993;55:193–202. doi: 10.1097/00006842-199303000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Gruenewald TL, Karlamangla AS, Hu P, Stein-Merkin S, Crandall C, Koretz B, et al. History of socioeconomic disadvantage and allostatic load in later life. Soc Sci Med. 2012;74:75–83. doi: 10.1016/j.socscimed.2011.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McEwen BS, Gianaros PJ. Central role of the brain in stress and adaptation: links to socioeconomic status, health, and disease. Ann N Y Acad Sci. 2010;1186:190–222. doi: 10.1111/j.1749-6632.2009.05331.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huh JH, Kwon S, Kim GO, Kim BY, Ha KH, Kim DJ. Long-term effectiveness of the national diabetes quality assessment program in South Korea. Diabetes Care. 2023;46:1700–6. doi: 10.2337/dc23-0444. [DOI] [PubMed] [Google Scholar]
- 38.Rawshani A, Rawshani A, Franzen S, Eliasson B, Svensson AM, Miftaraj M, et al. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med. 2017;376:1407–18. doi: 10.1056/NEJMoa1608664. [DOI] [PubMed] [Google Scholar]
- 39.Chamnan P, Simmons RK, Sharp SJ, Griffin SJ, Wareham NJ. Cardiovascular risk assessment scores for people with diabetes: a systematic review. Diabetologia. 2009;52:2001–14. doi: 10.1007/s00125-009-1454-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cederholm J, Eeg-Olofsson K, Eliasson B, Zethelius B, Nilsson PM, Gudbjornsdottir S, et al. Risk prediction of cardiovascular disease in type 2 diabetes: a risk equation from the Swedish National Diabetes Register. Diabetes Care. 2008;31:2038–43. doi: 10.2337/dc08-0662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stevens RJ, Kothari V, Adler AI, Stratton IM, United Kingdom Prospective Diabetes Study (UKPDS) Group The UKPDS risk engine: a model for the risk of coronary heart disease in type II diabetes (UKPDS 56) Clin Sci (Lond) 2001;101:671–9. [PubMed] [Google Scholar]
- 42.Donnan PT, Donnelly L, New JP, Morris AD. Derivation and validation of a prediction score for major coronary heart disease events in a U.K. type 2 diabetic population. Diabetes Care. 2006;29:1231–6. doi: 10.2337/dc05-1911. [DOI] [PubMed] [Google Scholar]
- 43.Read SH, van Diepen M, Colhoun HM, Halbesma N, Lindsay RS, McKnight JA, et al. Performance of cardiovascular disease risk scores in people diagnosed with type 2 diabetes: external validation using data from the national Scottish diabetes register. Diabetes Care. 2018;41:2010–8. doi: 10.2337/dc18-0578. [DOI] [PubMed] [Google Scholar]
- 44.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303:2043–50. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 45.Gu A, Yue Y, Desai RP, Argulian E. Racial and ethnic differences in antihypertensive medication use and blood pressure control among US adults with hypertension: the National Health and Nutrition Examination Survey, 2003 to 2012. Circ Cardiovasc Qual Outcomes. 2017;10:e003166. doi: 10.1161/CIRCOUTCOMES.116.003166. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multiply imputed effect of SDOH count on composite endpoint
HRs of composite endpoint in individuals without and with history of heart disease from minimally and fully adjusted models, by number of SDOH
Exclusion cascade for number of social determinants of health and composite endpoint. REGARDS, REasons for Geographic and Racial Differences in Stroke.
Kaplan-Meier curve by number of social determinants of health (SDOH) and composite endpoint.