Abstract
To investigate the safety and efficacy of balance training for stroke patients with reduced balance ability by performing a meta-analysis of randomized controlled trials. The PubMed, Embase, and Cochrane Central Register of Controlled Trials databases were searched up to February 2022. Quality assessment was performed using the using the Cochrane risk of bias tool. Studies were included if: 1) patient allocation was randomized; 2) the participant was composed of stroke patients with reduced balance ability (Berg Balance Scale [BBS] ≤ 40, Timed-Up and Go ≥ 14 seconds, or Mini-Balance Evaluation Systems Test ≤ 17.5); and 3) intervention was additional balance training for the experimental group. Six studies including 466 patients were included in the final analysis. The meta-analysis showed a significant improvement in the BBS (mean difference [MD], 8.14; 95% confidence interval [CI], 4.65, 11.64) and Trunk Impairment Scale (MD, 4.71; 95% CI, 3.45, 5.96) after balance training relative to the comparison group. Ambulation function was significantly improved (standardized MD, 0.98; 95% CI, 0.46, 1.49) after balance training. There was one report of a femur fracture among 230 participants in the balance training group. Balance training in addition to conventional rehabilitation program in stroke patients with reduced balance ability appears to be effective and safe.
Keywords: Stroke, Postural Balance, Rehabilitation, Systematic Review, Meta-Analysis
Highlights
• Balance training improved balance ability and ambulation function after stroke.
• Balance training in stroke patients with reduced balance ability seems to be safe.
• For stroke patients with reduced balance ability, balance training is recommended.
INTRODUCTION
Stroke is the second-leading cause of death and a major cause of disability worldwide, with significant impacts on patients’ quality of life and independence [1]. Among the various impairments that stroke survivors experience, reduced balance ability is one of the most common and debilitating consequences. The ability to maintain balance is fundamental to performing activities of daily living (ADL), mobility, and preventing falls.
Balance impairment affects up to 83% of stroke survivors, persisting long after the acute phase of recovery [2]. This high prevalence highlights the need for targeted interventions focused on balance rehabilitation. Emerging research suggests that balance ability is not only a key rehabilitation target but also a strong predictor of overall functional recovery after stroke [3]. Improvements in balance have been associated with enhanced mobility, increased independence in ADL, and better quality of life. This underscores the potential for balance-focused interventions to have wide-ranging benefits for stroke survivors.
In stroke patients with decreased balance ability, performing balance training itself could increase the risk of falls and related fractures, so it is necessary to elucidate whether applying balance training to these populations is safe and effective. Therefore, this study aimed to clarify the current evidence and to determine the efficacy and safety of balance training for stroke patients with reduced balance ability by performing an updated systematic review and meta-analysis of currently available data of randomized controlled trials.
MATERIAL AND METHODS
This systematic review was reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Study selection, eligibility criteria application, data extraction, and statistical analysis were performed in accordance with the Cochrane Collaboration guidelines [4].
Search strategy and study selection
We searched for references in the MEDLINE (PubMed), Embase, and Cochrane Central Register of Controlled Trials databases up to February 28, 2022 without any date restriction. Key terms used to conduct the literature search were selected and combined with the following English terms and their equivalents: “stroke” AND (“balance” or “fall”). The search strategies per database are outlined in Supplementary Data 1. Studies were included if: 1) patient allocation was randomized; 2) the participant was composed of stroke patients with reduced balance ability (Berg Balance Scale [BBS] ≤ 40 [5], Timed-Up and Go (TUG) ≥ 14 seconds [6], or Mini-Balance Evaluation Systems Test ≤ 17.5 [7]); and 3) intervention was additional balance training for the experimental group. Studies with lack of information on the objective balance ability for stroke patients were excluded. Abstracts and conference proceedings were excluded if they lacked sufficient reporting details. Review articles, editorials, and other nonclinical trials were also excluded.
Two reviewers (SYY and YWK) independently reviewed the titles and abstracts of the articles to determine their eligibility for inclusion. Studies that clearly failed to meet the inclusion criteria were not reviewed further. Those that could not be excluded were retrieved, and the full text was reviewed by the 2 reviewers. Studies that met the criteria were retrieved and reviewed in detail.
Data extraction and quality assessment
The following information was extracted from the included studies: first author, year of publication, patients’ demographics and clinical presentations, exercise protocols, total sample size and sample size per arm (balance training and comparison groups), scales and measures used to evaluate the efficacy of the interventions, and adverse events. The outcomes of interest were measures of balance ability, such as BBS or Trunk Impairment Scale (TIS), ambulation function, and ADL.
Study quality was assessed by rating the risk of selection bias, performance bias, detection bias, attrition bias, reporting bias, and other sources of bias using the Cochrane risk of bias tool [4]. Two reviewers (SYY and YWK) independently assessed whether each of the following domains was adequate (i.e., low, unclear, or high risk of bias): “sequence generation,” “allocation concealment,” “blinding,” “incomplete outcome data addressed,” “selective outcome reporting,” or “other bias.” The certainty of evidence in meta-analyses that included studies was assessed using the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) tool, which encompasses 5 aspects: 1) risk of bias, 2) inconsistency, 3) indirectness, 4) imprecision, and 5) publication bias. Ratings for the certainty of evidence were categorized as high, moderate, low, or very low.
Data synthesis and statistical analysis
A summary of the intervention effect was reported as the mean difference (MD) for balance ability and standardized mean difference (SMD) for ambulation function and ADL. Analyses were conducted using the RevMan 5.3 software (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). The degree of heterogeneity was assessed using I2. These statistics, expressed as a percentage between 0 and 100, can be interpreted as the percentage of heterogeneity in the system or basically the amount of total variation accounted for by between-study variances [8]. We used 2-tailed p values, and p values of < 0.05 were considered statistically significant.
RESULTS
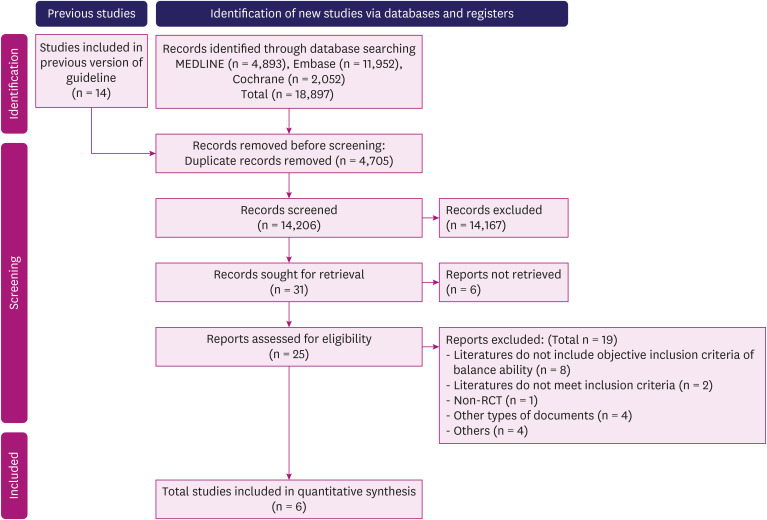
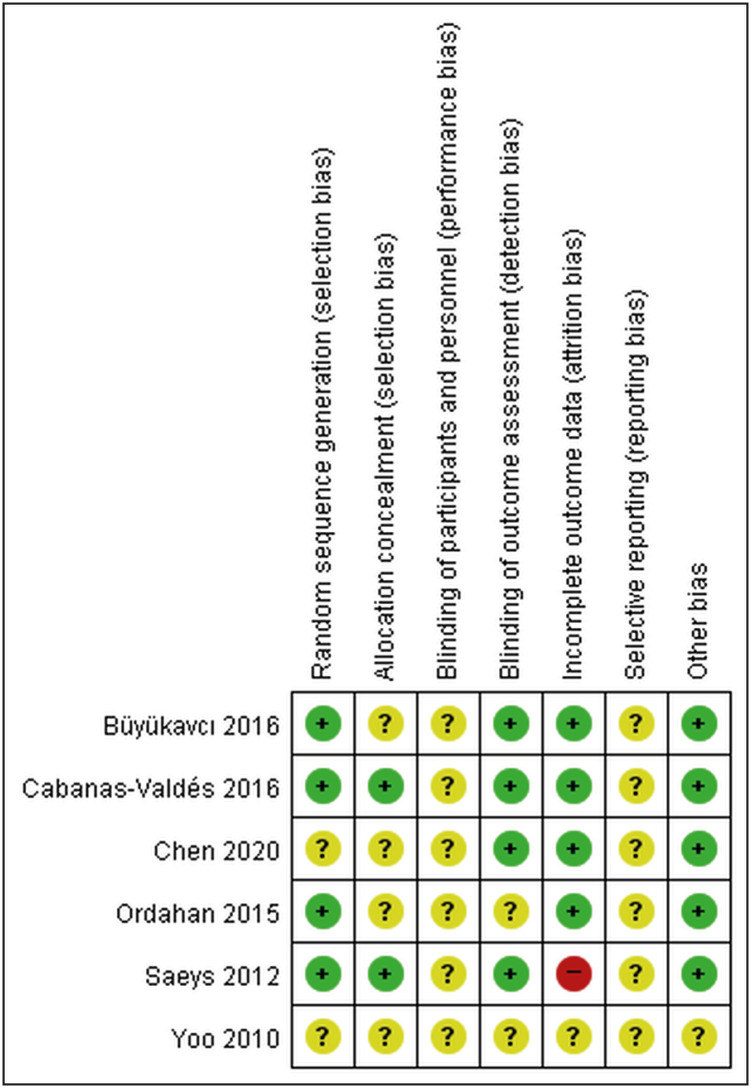
A flowchart of the search process is shown in Fig. 1. A total of 18,897 studies were identified in the initial search. After duplications were removed, 14,206 studies remained. After screening titles and abstracts, the full texts of the 25 remaining articles were assessed for eligibility. Finally, 6 studies [9,10,11,12,13,14] including 466 participants fulfilled the inclusion criteria and were included in the meta-analysis. The results of the risk of bias assessment for the 6 studies are presented in Fig. 2. The quality of evidence based on GRADE tool was estimated to be moderate.
Fig. 1. Flow chart of study search and selection methods.
RCT, randomized controlled trial.
Fig. 2. Risk of bias summary.
Study characteristics
The number of participants in the included studies ranged from 33 [11] to 180 [14]. Five studies performed additional core muscle training [10,11,12,13,14], and one study performed feedback training for postural balance improvement [9]. All 6 studies included in the meta-analysis reported BBS as an outcome variable [9,10,11,12,13,14], and TIS was reported in 3 studies [10,11,12]. Ambulation function [11,12,13] and ADL [9,12,13] were reported in 3 studies, respectively. Table 1 summarizes the characteristics of the included studies.
Table 1. Characteristics of the included studies.
| 1st author | Year | Experimental group | Intervention | Comparison group | Follow-up | Outcome measures |
|---|---|---|---|---|---|---|
| Büyükavcı | 2016 | Conventional exercise program + truncal exercise (n = 32) | Trunk exercises 2 hours/day/3 weeks | Conventional exercise program (n = 32) | 3 month | 1. BBS |
| 2. TIS | ||||||
| 3. FIM | ||||||
| 4. Rivermead Mobility Index | ||||||
| Cabanas-Valdés | 2016 | Conventional PT + core stability exercises (n = 40) | Core stability exercises for 15 min/day | Conventional PT (n = 40) | Post Tx. | 1. TIS |
| 2. Function in sitting test | ||||||
| 3. BBS | ||||||
| 4. Tinetti Test | ||||||
| 5. Brunel Balance Assessment | ||||||
| 6. Postural Assessment Scale for Stroke | ||||||
| 7. Barthel index | ||||||
| Chen | 2020 | Conventional hemiplegia rehabilitation therapy + core muscle stability training (n = 90) | Five times a week for a total of 8 weeks | Conventional hemiplegia rehabilitation therapy (n = 90) | Post Tx. | 1. BBS |
| 2. Brunnstrom staging | ||||||
| 3. Fugl-Meyer motor assessment | ||||||
| 4. 10 meter walking speed | ||||||
| 5. Abdominal muscle thickness | ||||||
| Ordahan | 2015 | Trained with balance trainer in addition to conventional rehabilitation program (n = 25) | 20 minutes a day, 5 days a week for a total of 6 weeks (30 sessions/600 minute in total) with the balance trainer (BALANCE-trainer, art.nr. 07001-001TM) | Conventional rehabilitation program (n = 25) | Post Tx. | 1. Timed-Up and Go Test |
| 2. BBS | ||||||
| 3. FIM | ||||||
| Saeys | 2012 | Conventional therapy + truncal exercise (n = 18) | 16 hours of truncal exercises | Conventional therapy + 16 hours sham Tx. (arm therapy) (n = 15) | Post Tx. | 1. TIS |
| 2. Tinetti Test | ||||||
| 3. Romberg test | ||||||
| 4. Four Test Balance Scale | ||||||
| 5. BBS | ||||||
| 6. Rivermead Motor Assessment Battery | ||||||
| 7. Functional Ambulation Categories | ||||||
| 8. Dynamic Gait Index | ||||||
| Yoo | 2010 | Conventional PT + additional core strengthening program (n = 28) | 30 minutes a day, 3 days per week for 4 weeks | Conventional PT (n = 31) | Post Tx., 4 weeks | 1. Trunk Control Test |
| 2. TIS | ||||||
| 3. BBS |
BBS, Berg Balance Scale; TIS, Trunk Impairment Scale; FIM, Functional Independence Measure; PT, physical therapy; Tx., treatment.
Add-on effects of balance training for stroke patients with reduced balance ability
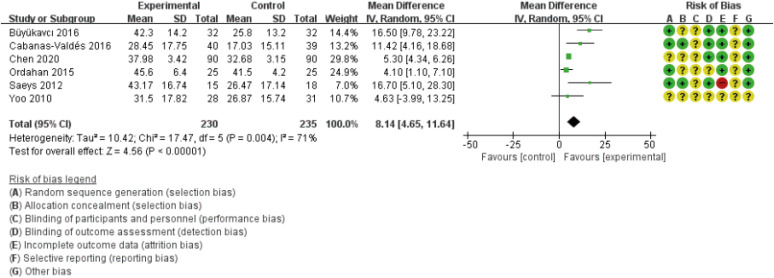
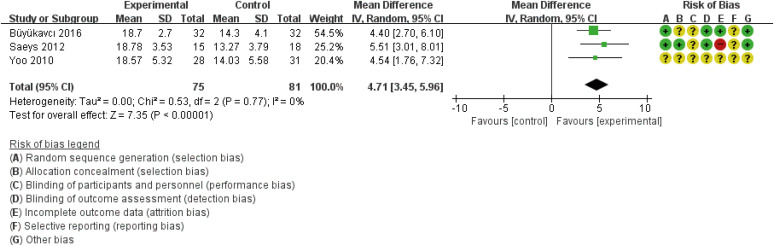
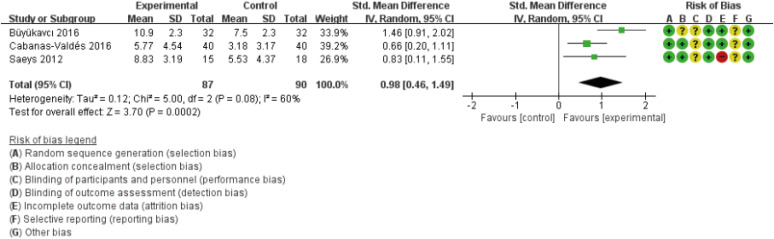
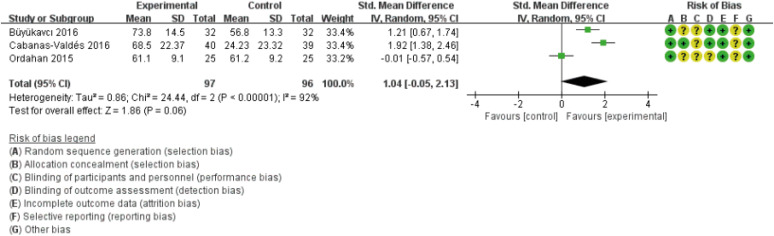
The 6 studies reported the BBS to reflect balance ability, and the meta-analysis showed a significant improvement in the BBS (MD, 8.14; 95% confidence interval [CI], 4.65, 11.64) after balance training relative to the comparison group (Fig. 3). Three studies assessed TIS, and TIS (MD, 4.71; 95% CI, 3.45, 5.96) was also significantly improved (Fig. 4). There were 3 studies evaluated ambulation function, and the meta-analysis showed significant improved ambulation function (SMD, 0.98; 95% CI, 0.46, 1.49) after balance training (Fig. 5). Three studies accessed ADL, and there were no significant differences in ADL between the 2 groups (SMD, 1.04; 95% CI, −0.05, 2.13) (Fig. 6).
Fig. 3. Meta-analysis of additional balance training for Berg Balance Scale.
SD, standard deviation; CI, confidence interval; IV, inverse variance.
Fig. 4. Meta-analysis of additional balance training for Trunk Impairment Scale.
SD, standard deviation; CI, confidence interval; IV, inverse variance.
Fig. 5. Meta-analysis of additional balance training for ambulation function.
SD, standard deviation; CI, confidence interval; IV, inverse variance.
Fig. 6. Meta-analysis of additional balance training for activities of daily living.
SD, standard deviation; CI, confidence interval; IV, inverse variance.
Adverse events
Of the 6 studies included in this review, there were no reports about falls during balance training in patients with reduced balance ability. One study reported a femur fracture in the experimental group [12], but the study did not clearly state whether the femur fracture occurred during balance training. The number of participants of the experimental group in this meta-analysis was 230, and the frequency of fracture was estimated approximately 0.4%.
DISCUSSION
This systematic review and meta-analysis aimed to evaluate safety and efficacy of balance training for stroke patients with reduced balance ability. The meta-analysis showed significant improvement in balance ability and ambulation function in patients who performed additional balance training compared to those who performed only conventional rehabilitation programs. However, there was no significant improvement in ADL after additional balance training. There was only one report of a femur fracture among 230 participants who performed balance training.
Although the incidence of stroke has gradually increased, mortality after stroke has decreased by 12.8% from 2014 to 2019 [15]. Many stroke survivors suffer from long-term sequelae, and reduced balance impairment is one of the most common problems after stroke. Reduced balance ability has a negative impact on functional independence and are one of the most important risk factors causing falls [16]. The ability to keep postural stability in sitting and standing positions is essential for functional activities such as transfer, walking, and even ADL [17]. There have been several evidences to support the effects of balance training in patients after stroke [18,19]. However, whether performing balance training in stroke patients with high risk of falls or reduced balance ability is safe and effective has not been elucidated yet. Therefore, in this meta-analysis, we investigated the effects of add-on balance training in stroke patients with reduced balance ability and whether it can be performed safely.
Our results showed that balance training in addition to conventional rehabilitation program improved balance ability and ambulation function even for stroke patients with balance impairment. One femur fracture was reported on balance training group, however there was no clear information whether the femur fracture was occurred during balance training. And the estimated incidence rate of fracture was 0.4%. Therefore, it appears that balance training can be performed in stroke patients with reduced ability safely. On the other hand, ADL was not improved after balance training in our study. Performing ADL is affected by cognition and hand fine motor function as well as balance ability [20,21], which can be a possible explanation for our results.
Of 6 studies included in this meta-analysis, 5 studies performed core muscle exercise [10,11,12,13,14]. Previous studies have suggested that stability exercises would a viable strategy for improving trunk performance and dynamic sitting balance, standing balance, and gait in post-stroke patients [22,23], which is inline with our results. One study investigated the effectiveness of visual feedback balance training [9], and participants were trained to maintain their posture steadily and symmetric while weight bearing and adapting to different static sensory conditions, through verbal and tactile cues. And the proposed mechanisms of feedback training consists of increasing the activity of the receptor organ in the inner ear during exercises, activating the integrating central nervous system by offering varying sensory inflow, and training the neuromuscular effecter system [24].
Our study has several limitations to be considered. First, the total number of included studies and participants was small. Although there have been many studies on the effects of balance training in patients after stroke, the number of studies which focused on stroke patients with reduced balance ability was small. Second, the diversity of the exercise protocols performed in each study, including exercise frequency and duration, may have caused variation in the results. With these various parameters and the low number of included studies, we could not perform subgroup analysis and draw conclusions on the optimal protocols of balance training.
In this study, we investigated the efficacy and safety of balance training in stroke patients with reduced balance ability. According to our results, adding balance training to conventional rehabilitation program appears to be effective and safe. Future studies are required to determine exercise types and optimal protocols of each exercise for stroke patients with reduced balance ability.
Footnotes
Funding: This study is supported by a research grant of Research Institute of Rehabilitation Medicine, Yonsei University College of Medicine for 2024.
Conflict of Interest: The authors have no potential conflicts of interest to disclose.
SUPPLEMENTARY MATERIAL
Search strategies
References
- 1.GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20:795–820. doi: 10.1016/S1474-4422(21)00252-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tyson SF, Hanley M, Chillala J, Selley A, Tallis RC. Balance disability after stroke. Phys Ther. 2006;86:30–38. doi: 10.1093/ptj/86.1.30. [DOI] [PubMed] [Google Scholar]
- 3.Verheyden G, Vereeck L, Truijen S, Troch M, Herregodts I, Lafosse C, Nieuwboer A, De Weerdt W. Trunk performance after stroke and the relationship with balance, gait and functional ability. Clin Rehabil. 2006;20:451–458. doi: 10.1191/0269215505cr955oa. [DOI] [PubMed] [Google Scholar]
- 4.The Cochrane Collaboration. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011] [accessed on 11 September 2024]. Available at www.cochrane-handbook.org.
- 5.Blum L, Korner-Bitensky N. Usefulness of the Berg Balance Scale in stroke rehabilitation: a systematic review. Phys Ther. 2008;88:559–566. doi: 10.2522/ptj.20070205. [DOI] [PubMed] [Google Scholar]
- 6.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80:896–903. [PubMed] [Google Scholar]
- 7.Potter K, Brandfass K. The Mini-Balance Evaluation Systems Test (Mini-BESTest) J Physiother. 2015;61:225. doi: 10.1016/j.jphys.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11:193–206. doi: 10.1037/1082-989X.11.2.193. [DOI] [PubMed] [Google Scholar]
- 9.Ordahan B, Karahan AY, Basaran A, Turkoglu G, Kucuksarac S, Cubukcu M, Tekin L, Polat AD, Kuran B. Impact of exercises administered to stroke patients with balance trainer on rehabilitation results: a randomized controlled study. Hippokratia. 2015;19:125–130. [PMC free article] [PubMed] [Google Scholar]
- 10.Yoo SD, Jeong YS, Kim DH, Lee M, Noh SG, Shin YW, Kim SH, Kim HS. The efficacy of core strengthening on the trunk balance in patients with subacute stroke. J Korean Acad Rehabil Med. 2010;34:677–682. [Google Scholar]
- 11.Saeys W, Vereeck L, Truijen S, Lafosse C, Wuyts FP, Heyning PV. Randomized controlled trial of truncal exercises early after stroke to improve balance and mobility. Neurorehabil Neural Repair. 2012;26:231–238. doi: 10.1177/1545968311416822. [DOI] [PubMed] [Google Scholar]
- 12.Büyükavcı R, Şahin F, Sağ S, Doğu B, Kuran KB. The impact of additional trunk balance exercises on balance, functional condition and ambulation in early stroke patients: randomized controlled trial. Turk Fizik Rehabil Derg. 2016;62:248–256. [Google Scholar]
- 13.Cabanas-Valdés R, Bagur-Calafat C, Girabent-Farrés M, Caballero-Gómez FM, Hernández-Valiño M, Urrútia Cuchí G. The effect of additional core stability exercises on improving dynamic sitting balance and trunk control for subacute stroke patients: a randomized controlled trial. Clin Rehabil. 2016;30:1024–1033. doi: 10.1177/0269215515609414. [DOI] [PubMed] [Google Scholar]
- 14.Chen X, Gan Z, Tian W, Lv Y. Effects of rehabilitation training of core muscle stability on stroke patients with hemiplegia. Pak J Med Sci. 2020;36:461–466. doi: 10.12669/pjms.36.3.1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jung SH. Stroke rehabilitation fact sheet in Korea. Ann Rehabil Med. 2022;46:1–8. doi: 10.5535/arm.22001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mackintosh SF, Hill KD, Dodd KJ, Goldie PA, Culham EG. Balance score and a history of falls in hospital predict recurrent falls in the 6 months following stroke rehabilitation. Arch Phys Med Rehabil. 2006;87:1583–1589. doi: 10.1016/j.apmr.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 17.Juneja G, Czyrny JJ, Linn RT. Admission balance and outcomes of patients admitted for acute inpatient rehabilitation. Am J Phys Med Rehabil. 1998;77:388–393. doi: 10.1097/00002060-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 18.An M, Shaughnessy M. The effects of exercise-based rehabilitation on balance and gait for stroke patients: a systematic review. J Neurosci Nurs. 2011;43:298–307. doi: 10.1097/JNN.0b013e318234ea24. [DOI] [PubMed] [Google Scholar]
- 19.van Duijnhoven HJ, Heeren A, Peters MA, Veerbeek JM, Kwakkel G, Geurts AC, Weerdesteyn V. Effects of exercise therapy on balance capacity in chronic stroke: systematic review and meta-analysis. Stroke. 2016;47:2603–2610. doi: 10.1161/STROKEAHA.116.013839. [DOI] [PubMed] [Google Scholar]
- 20.Raimo S, Maggi G, Ilardi CR, Cavallo ND, Torchia V, Pilgrom MA, Cropano M, Roldán-Tapia MD, Santangelo G. The relation between cognitive functioning and activities of daily living in normal aging, mild cognitive impairment, and dementia: a meta-analysis. Neurol Sci. 2024;45:2427–2443. doi: 10.1007/s10072-024-07366-2. [DOI] [PubMed] [Google Scholar]
- 21.Lee HC, Kuo FL, Lin YN, Liou TH, Lin JC, Huang SW. Effects of robot-assisted rehabilitation on hand function of people with stroke: a randomized, crossover-controlled, assessor-blinded study. Am J Occup Ther. 2021;75:7501205020p1–7501205020p11. doi: 10.5014/ajot.2021.038232. [DOI] [PubMed] [Google Scholar]
- 22.Cabanas-Valdés R, Cuchi GU, Bagur-Calafat C. Trunk training exercises approaches for improving trunk performance and functional sitting balance in patients with stroke: a systematic review. NeuroRehabilitation. 2013;33:575–592. doi: 10.3233/NRE-130996. [DOI] [PubMed] [Google Scholar]
- 23.Van Criekinge T, Truijen S, Schröder J, Maebe Z, Blanckaert K, van der Waal C, Vink M, Saeys W. The effectiveness of trunk training on trunk control, sitting and standing balance and mobility post-stroke: a systematic review and meta-analysis. Clin Rehabil. 2019;33:992–1002. doi: 10.1177/0269215519830159. [DOI] [PubMed] [Google Scholar]
- 24.Bulat T, Hart-Hughes S, Ahmed S, Quigley P, Palacios P, Werner DC, Foulis P. Effect of a group-based exercise program on balance in elderly. Clin Interv Aging. 2008;2:655–660. doi: 10.2147/cia.s204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search strategies