Abstract
BACKGROUND
Non-suicidal self-injury (NSSI) is common among adolescents and frequently co-occurs with depression. Understanding the distinct patterns of NSSI behaviors, along with their associated risk and protective factors, is crucial for developing effective interventions.
AIM
To classify NSSI behaviors and examine interactions between risk and resilience factors in Chinese adolescents.
METHODS
A cross-sectional study involving 3967 Chinese students (51.7% female, mean age 13.58 ± 2.24 years) who completed questionnaires on parenting styles, bullying, childhood maltreatment, depression, resilience, and NSSI. Latent profile analysis (LPA) was used to identify NSSI subtypes, and network analysis explored interactions between risk and resilience factors.
RESULTS
Three NSSI subtypes were identified: NSSI with depression (18.8%), NSSI without depression (12.3%), and neither (68.9%). Bullying was the central risk factor across subtypes, while emotional control and family support were key protective factors. Statistical analyses showed significant differences between groups (P < 0.001).
CONCLUSION
This study identified three NSSI subtypes among Chinese adolescents. Bullying emerged as a central risk factor, while emotional control and family support were key protective factors. Targeting these areas may help reduce NSSI behaviors in this population.
Keywords: Non-suicidal self-injury, Adolescent, Network analysis, Latent profile analysis, Resilience
Core Tip: Latent profile analysis (LPA): Utilized LPA based on self-injury and patient health questionnaire-9 depression assessments to uncover distinct non-suicidal self-injury (NSSI) profiles in adolescents, addressing the hypothesized heterogeneity between NSSI with and without depression. Network analysis insights: Identified differences in risk and resilience factors across NSSI subgroups. Bullying and depression connection: Demonstrated a strong link between bullying and depressive symptoms in NSSI subgroups. Intervention focal points: Pinpointed emotional control and family support as key areas for targeted interventions derived from LPA findings.
INTRODUCTION
Non-suicidal self-injury (NSSI), defined as deliberate self-harm without suicidal intent, is an escalating public health concern, particularly among adolescents. Common methods include cutting, scratching, and hitting oneself-behaviors prevalent worldwide. Studies indicate that approximately 17.2% of adolescents in non-clinical settings engage in NSSI, with rates as high as 27.4% reported among Chinese adolescents aged 13-18 years[1,2]. The high incidence of NSSI in China highlights the urgent need for effective interventions, as individuals engaging in NSSI have a 66-fold increased risk of suicide[3].
The etiology of NSSI is complex, involving genetic, psychological, and sociocultural factors. Significant contributors include chronic stress, adverse childhood experiences, and digital media use[4]. Emotional dysregulation resulting from childhood trauma and a lack of parental support are key predictors of NSSI[5,6]. In China, societal factors such as academic pressure, filial piety, and traditional family dynamics further exacerbate these risks.
Despite extensive research on NSSI risk factors, a gap remains in understanding how these factors interact within specific adolescent subgroups. Existing studies often employ binary classifications, which fail to capture the complexity of these behaviors. This oversimplification overlooks the interplay between risk factors and protective factors-such as resilience and emotional regulation-that are crucial for developing effective interventions[7].
Latent profile analysis (LPA) offers a more nuanced method for identifying NSSI subtypes by classifying adolescents based on their behaviors and associated factors. Network analysis further explores the interactions among risk and resilience factors[8], revealing how these elements interrelate across different subtypes.
This study fills a critical gap by integrating LPA and network analysis to examine NSSI among Chinese adolescents. We identify distinct NSSI subtypes and analyze how risk factors-such as bullying, parenting style, and digital media use-interact with protective factors such as emotional control (EC) and SF within these subtypes. Our research provides new insights into the underlying mechanisms of NSSI, offering implications for tailored interventions to meet the diverse needs of adolescent subgroups.
MATERIALS AND METHODS
Participants
Participants were recruited from the Yuxi cohort of the Mental Health Survey for Children and Adolescents, which is part of the broader Yunnan Mental Health Survey. We employed a two-stage cluster sampling technique to obtain a representative sample of adolescents aged 10-18 years. In the first stage, schools were randomly selected using probability proportional to size sampling. In the second stage, within each selected school, 2-4 classes from each grade level were chosen through random sampling to participate in the study. The survey was conducted in two phases: Initially, participants completed a self-administered questionnaire, followed by a diagnostic assessment for those who screened positive, conducted by qualified psychiatric professionals. The study was conducted in accordance with ethical standards, with approval from the Ethics Committee of Kunming Medical University (Approval Number: KMMU2020MEC047). Written informed consent was obtained from the legal guardians of all participants in September 2021.
Measures
Table 1 presents the key details regarding the measures used in this study.
Table 1.
Measures of variables in risk factor-resilience networks across all study participants
|
Measure
|
Description
|
Scoring
|
Total score/subscales
|
α
|
| PHQ-9 (Martin et al[34], 2006) | Measures the severity of depression | 9 items 4-point scale ranging from "never" (1 point) to "very often" (4 points) | 0.886 | |
| MASHS (Feng et al[35], 2008) | Measure the method and severity of self-harming behavior in an adolescent's lifetime |
18-item, the first part: A 4-point scale ranging from (0, 1, 2–4, 5, and more); the second part: A 5-point scale (0 = none to 5 = extremely severe | The frequency of NSSI behavior is categorized into two parts (frequency and severity) | 0.84 |
| S-EMBU-C ( Jiang et al[36], 2010) | Assess parenting styles experienced during childhood years | 21 items. 4-point scale ranging from “Never” (1 point), “Occasionally” (2 points), “Frequently” (3 points), and “Always” (4 points) | Two parts to three dimensions: Rejection, emotional warmth, and overprotection | 0.827 |
| CTQ-SF (Bernstein and Fink[37], 1998) | Measure traumatic childhood experiences | 28-item 5-point scale (1 = never, 2 = once, 3 = twice to four times, 4 = five times or more) | PA, EA, SA, PN, and EN | 0.871 |
| OBVQ (Solberg and Olweus[38], 2003) | Evaluate traditional school bullying, encompassing physical, verbal, and relation and attitude to bully | 14 item 5-point Likert scale (1 = never happened, 2 = altogether once or twice, 3 = 2–3 times per month, 4 = once a week, 5 = several times a week) | Traditional bullying, another to physical bullying, and a third to attitudes towards bullying behaviors | 0.72 |
| RSCA (Hu and Gan[39], 2008) | Assess resilience | 27-item 5-point scale (1 = never, 2 = once, 3 = twice to four times, 4 = five times or more) | Five components of resilience (goal concentration, emotion regulation, positive perception, FS, and interpersonal help) | 0.82 |
| MPAI(Leung[40], 2008) | Assess the levels of mobile phone addiction among the participants, and it has good reliability and validity | 17 items 5-point Likert scale (1 = never, 5 = always) | 4 subscales: ICCS, FALS, WES, and PLS | 0.86 |
PHQ-9: The Patient Health Questionnaire nine-item depression scale; MASHS: Modified adolescents self-harm survey; S-EMBU-C: The short Chinese Egna Minnen av Barndoms Uppfostra; CTQ-SF: The Childhood Trauma Questionnaire-Short Form; OBVQ: The Chinese version of the Orvis Bullying/Victimization Questionnaire; RSCA: Resilience Scale for Chinese Adolescents; MPAI: The mobile phone addiction index scale amended by Leung; PLS: The productivity loss subscale; WES: The withdrawal and escape subscale; FALS: The feeling anxious and lost subscale; ICCS: The inability to control cravings subscale; FS: Family support; EN: Emotional neglect; PN: Physical neglect; SA: Sexual abuse; EA: Emotional abuse; PA: Physical abuse; NSSI: Non-suicidal self-injury.
Statistical analysis
Our statistical analysis comprised several key steps: Handling missing data, performing LPA, and conducting network analysis, which included network estimation, inference, stability assessment, and comparison. All analyses were conducted using R version 4.3.1. Specific packages used included “qgraph” for network visualization “bootnet” for network stability[9], and “NetworkComparisonTest” for network comparison.
Missing data handling: Missing data were addressed using full information maximum likelihood (FIML) estimation, allowing the use of all available data without imputing values[10]. FIML provides unbiased parameter estimates under the assumption of data missing at random, avoiding biases from methods like listwise deletion. Sensitivity analyses confirmed that missing data did not significantly affect the findings, ensuring the robustness of the results.
LPA: We conducted LPA to classify adolescent subgroups based on NSSI behaviors and depressive symptoms measured by the modified adolescents' self-harm survey and the patient health questionnaire-9. LPA is suitable for identifying hidden subgroups, providing a nuanced understanding of heterogeneity in NSSI behaviors and depression levels.
To determine the optimal number of latent profiles, we explored models with varying profile numbers. Model selection was guided by the Akaike information criterion (AIC), Bayesian information criterion (BIC), and adjusted BIC (aBIC), where lower values indicate better fit[11]. We used the Lo-Mendell-Rubin adjusted likelihood ratio test and bootstrapped likelihood ratio test to compare models, considering P values less than 0.05 as a significant improvement in fit. An entropy value assessed classification accuracy; our entropy of 0.89 suggested excellent classification quality.
Network analysis: Network analysis explored interactions between risk and resilience factors across the NSSI subgroups, following these steps: (1) Network Estimation: The Gaussian graphical model with graphical LASSO was used to capture partial correlations among variables[12]. LASSO regularization prevents overfitting by shrinking weaker edges; (2) Inference: Centrality measures-node strength, closeness, and betweenness-were calculated to assess each variable's role within the network[13], identifying key factors for intervention; (3) Stability: Bootstrapping through the “bootnet” package provided confidence intervals for edge weights and centrality measures, ensuring the stability of results. Stability coefficients above 0.5 confirmed robustness; (4) Comparison: The network comparison test (NCT) evaluated differences in network structure across NSSI subgroups[14]. Holm-Bonferroni corrections were applied to adjust for multiple comparisons, ensuring reliable inferences; and (5) Network density: Network density, defined as the average strength of all edges, was compared between subgroups. Higher density indicates a more interconnected network, which may have implications for the persistence and resilience of NSSI behaviors within subgroups.
RESULTS
Descriptive analyses
This study included 3967 participants (51.7% female, mean age = 13.58, SD = 2.24). Table 2 presents the means and standard deviations for each variable. Bonferroni correction revealed significant differences in paternal warmth (PW), maternal warmth (MW), and bullying between NSSI subgroups, with the NSSI-D group showing the lowest levels. These findings suggest that targeted interventions focusing on family dynamics and bullying may be critical for these subgroups.
Table 2.
Overview of influence factors (including means and standard deviations) from subgroup data
| No. | Risk factor | Short codes |
M (SD)
|
||
|
X1
|
X2
|
X3
|
|||
| 1 | Paternal warmth | PW | 19.73 (4.99) | 21.21 (5.03) | 20.85 (5.04) |
| 2 | Maternal warmth | MW | 20.68 (5.05) | 20.71 (4.82) | 21.89 (4.66) |
| 3 | Father reject | FR | 8.17 (2.76) | 7.54 (2.44) | 7.7 (2.49) |
| 4 | Mother reject | MR | 9.94 (2.28) | 9.7 (2.01) | 9.73 (2.15) |
| 5 | Father overprotective | FO | 15.91 (3.8) | 15.18 (4.01) | 15.39 (3.9) |
| 6 | Mother overprotective | MO | 16.85 (4.05) | 16.16 (4.44) | 16.21 (4.18) |
| 7 | Emotional abuse | EA | 6.78 (2.53) | 6.68 (2.53) | 6.81 (2.62) |
| 8 | Physical abuse | PA | 5.71 (1.48) | 5.72 (1.6) | 5.84 (1.8) |
| 9 | Sexual abuse | SA | 5.12 (0.6) | 5.15 (0.66) | 5.14 (0.67) |
| 10 | Emotional neglect | EN | 10.5 (4.01) | 10.4 (4.19) | 10.41 (4.23) |
| 11 | Physical neglect | 6.71 (2.29) | 6.62 (2.43) | 6.74 (2.47) | |
| 12 | Bullied | BL | 8.56 (2.76) | 7.26 (0.67) | 8.04 (2.44) |
| 13 | Attitudes bullying | AB | 17.08 (3.4) | 17.45 (3.16) | 17.46 (3.29) |
| 14 | Bullying | PB | 6.5 (1.21) | 6.07 (0.53) | 6.17 (0.65) |
| 15 | Targeted focus | TF | 17.95 (4.52) | 19.38 (4.28) | 18.72 (4.67) |
| 16 | Emotional control | EC | 19.39 (4.05) | 20.47 (4.04) | 20.3 (4.02) |
| 17 | Positive cognition | PC | 14.53 (3.72) | 15.32 (3.47) | 14.97 (3.73) |
| 18 | Interpersonal interactions | II | 20.84 (5.92) | 22.33 (5.79) | 22.25 (5.77) |
| 19 | Family support | FS | 23.82 (4.56) | 23.42 (4.68) | 23.3 (4.67) |
| 20 | Smartphone addiction - withdrawal | SW | 6.9 (3.76) | 5.84 (3.01) | 6.35 (3.54) |
| 21 | Smartphone addiction - out of control | SO | 17.23 (7.31) | 15.72 (7.25) | 15.89 (7.39) |
| 22 | Smartphone addiction - avoidance | SV | 7.41 (3.59) | 6.52 (3.35) | 6.92 (3.62) |
| 23 | Smartphone addiction - inefficiency | SI | 5.42 (2.66) | 4.89 (2.44) | 5.08 (2.61) |
Influence factor names and No. Short codes were applied completely by paper.
LPA
LPA identified three subgroups: NSSI with depression (NSSI-D; 18.8%), NSSI without depression (NSSI-ND; 12.3%), and no NSSI (NNSSI-ND; 68.9%). Model fit indices (AIC = 353719.4, BIC = 371608.7, aBIC = 282288.2) supported the three-profile solution, with an entropy value of 0.89 indicating high classification accuracy.
The NSSI-D group had higher depressive symptoms and emotional dysregulation, while the NSSI-ND group exhibited impulsive and externalizing behaviors, pointing to the need for distinct interventions for each subgroup (Table 3).
Table 3.
Fit indices for three models using latent profile analysis (n = 3967)
|
M
|
df
|
χ2
|
G2
|
aBIC
|
AIC
|
Entropy
|
LMR
|
BLRT
|
Group size for each profile (%)
|
|||
|
1
|
2
|
3
|
4
|
|||||||||
| 1 | 2963 | 16130 | 312372 | 386431 | 380120.1 | - | - | - | 3967 (100) | |||
| 2 | 2742 | 12040 | 290985.2 | 366874.6 | 359174.5 | 0.781 | 0.043 | 0.001 | 1225 (35.7) | 2742 (64.3) | ||
| 3 | 1121 | 23910 | 282288.2 | 371608.7 | 353719.4 | 0.742 | 0.342 | 0.001 | 488 (12.3) | 747 (18.8) | 2732 (68.9) | |
| 4 | 1292 | 26059 | 279126.3 | 367029.9 | 350215.5 | 0.670 | 0.471 | 0.001 | 1067 (26.9) | 603 (15.2) | 1944 (49) | 353 (0.088) |
Numbers in bold indicate “best” fit. AIC: Akaike information criterion; BIC: Bayesian information criterion; aBIC: Adjusted Bayesian information criterion; pLMR: P value for LoMendell-Rubin adjusted likelihood ratio test for K vs K-1 profiles; pBLRT: P value for bootstrapped likelihood ratio test.
Network analysis
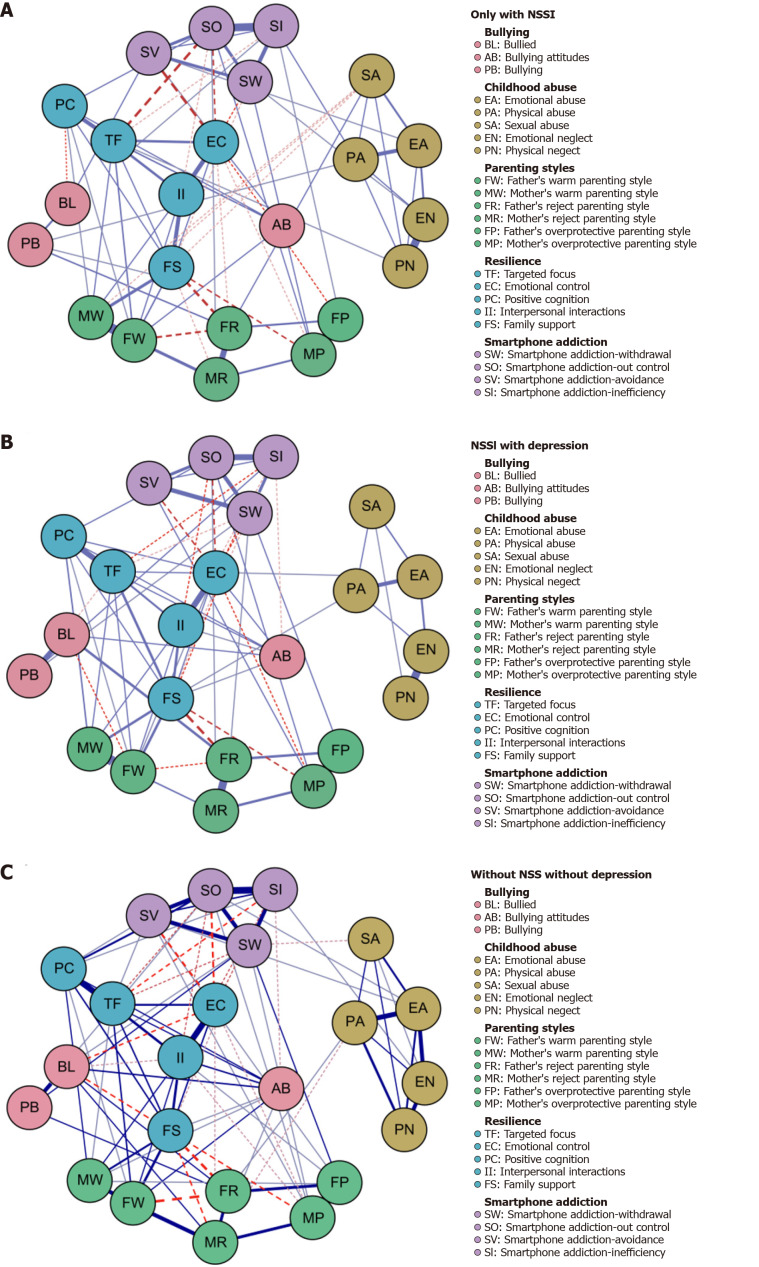
Network estimation: Figure 1 illustrates the networks for the NSSI-ND, NSSI-D, and NNSSI-ND groups. The network densities were 0.490 (NSSI-ND, 4/529 edges), 0.451 (NSSI-D, 12/529 edges), and 0.585 (NNSSI-ND, 2/529 edges), reflecting varying levels of connectivity. Mean absolute edge weights were 0.094 (NSSI-ND), 0.079 (NSSI-D), and 0.055 (NNSSI-ND), indicating different strengths of associations within each group.
Figure 1.
Regularized partial correlation influence factor-resilience network across three subgroups: Edge thickness represents the strength of association. Blue (solid) lines indicate positive relationships, whereas red (dashed) lines indicate negative relationships. Only edges with weights greater than 0.05 are displayed. Edge weights are scaled according to the maximum edge weight across all points (0.65). A: Subgroup designations: Non-suicidal self-injury (NSSI)-without depression (ND); B: Subgroup designations: NSSI-with depression; C: Subgroup designations: No NSSI-ND.
Across all groups, strong positive correlations were observed between MW and PW, with edge weights ranging from 0.639 to 0.712. Negative correlations revealed unique family dynamics, such as the -0.165 edge between family support (FS) and father reject in the NSSI-ND group and the -0.218 edge between FS and PW in the NSSI-D group. These findings highlight how family dynamics vary across NSSI subgroups, suggesting different intervention targets depending on family structure and relationships.
Network inference: Bridge strength analyses provided key insights into the influence of risk and resilience factors across NSSI subgroups. As presented in Table 4, PW, MW, and FS exhibited high centrality and bridge strength, emphasizing their crucial roles in shaping NSSI behaviors, particularly concerning EC. These factors consistently emerged as central nodes across the NSSI-ND, NSSI-D, and NNSSI-ND groups.
Table 4.
Centrality measures of key risk and resilience factors across non-suicidal self-injury subgroups
|
Factor
|
NSSI-ND (strength)
|
NSSI-D (strength)
|
NNSSI-ND (strength)
|
| Paternal warmth | 0.72 | 0.68 | 0.75 |
| Maternal warmth | 0.69 | 0.71 | 0.74 |
| Family support | 0.63 | 0.60 | 0.70 |
| Bullying | 0.75 | 0.78 | 0.65 |
NSSI-ND: Non-suicidal self-injury-without depression; NSSI-D: Non-suicidal self-injury-with depression; NNSSI-ND: No non-suicidal self-injury-without depression.
Predictability scores, which indicate the proportion of variance explained by neighboring nodes, were 47.3% for NSSI-D, 48.1% for NSSI-ND, and 49.3% for NNSSI-ND, highlighting how risk factors interact within the network. Additionally, correlations between centrality strength and predictability were strong, with values of 0.826 (NSSI-ND), 0.590 (NSSI-D), and 0.730 (NNSSI-ND), suggesting varying impacts of these factors across different groups.
These findings highlight the importance of family dynamics and EC in addressing NSSI behaviors, particularly for adolescents with co-occurring depressive symptoms (NSSI-D) (Table 4 and Figure 2).
Figure 2.
Standardized node strength centrality and bridge strength of influence factors across three non-suicidal self-injury datasets. A: Node strength; B: Bridge strength. The networks are labeled as follows: Network 1 = Non-suicidal self-injury (NSSI)-without depression (ND), Network 2 = NSSI-with depression, Network 3 = No NSSI-ND. Refer to Table 2 for the complete names of influence risk factors.
Network stability: Stability analysis revealed that edge weights had slight to moderate confidence intervals, with a correlation stability coefficient for strength centrality of 0.75 in all networks, exceeding the recommended 0.50 threshold[15]. Detailed information is available in Figure 3.
Figure 3.
Estimated correlation stability coefficient (cs-coefficient) with bootstrapped 95%CI: The CS-coefficient ranges from 0 to 1, where values above 025 indicate moderate stability, and values above 05 indicate strong stability. Edge-weight difference tests and centrality difference tests were conducted for each network. A: Non-suicidal self-injury (NSSI)-without depression (ND); B: NSSI-with depression; C: No NSSI-ND. AB: Bullying Attitudes; BL: Bullied; EA: Emotional abuse; EC: Emotional control; EN: Emotional neglect; FP: Father's overprotective parenting style; FR: Father's reject parenting style; FS: Family support; FW: Father's Warm Parenting Style; Il: Interpersonal interactions; MP: Mother's overprotective parenting style; MR: Mother's reject parenting style; MW: Mother's warm parenting style; PA: Physical abuse; PB: Bullying; PC: Positive cognition; PN: Physical neglect; SA: Sexual abuse; SI: Smartphone addiction-inefficiency; SO: Smartphone addiction-out control; SV: Smartphone addiction-avoidance; SW: Smartphone addiction-withdrawal; TF: Targeted focus.
Network comparison: Spearman correlations revealed high network similarity: 0.95 between NSSI-ND and NSSI-D, and 0.97 between NSSI-ND and NNSSI-ND. The NCT found no significant global strength differences across networks (NSSI-ND: 8.67, NSSI-D: 9.09, NNSSI-ND: 10.97; S = 0.418, P = 0.39), indicating overall connectivity consistency. However, significant structural differences were observed between the NSSI-ND and NSSI-D networks (M = 0.301, P < 0.001), with one significantly different edge and four specifically identified edges. Centrality invariance tests (C = 0.05, P = 0.007) revealed distinct centrality patterns, particularly in bullied nodes within the NSSI-D network.
A noteworthy finding was the unique centrality of bullying in the NSSI-D group, suggesting that bullying plays a more prominent role in adolescents with both NSSI and depression, compared to those without depression. This insight highlights the need for targeted anti-bullying interventions in this subgroup.
No significant global strength or structural differences were found between the NSSI-ND and NNSSI-ND, or between NSSI-D and NNSSI-ND networks. However, node centrality differences emerged between NSSI-ND and NNSSI-ND. Pairwise NCT analyses identified significant differences in 12 out of 529 edges (4.74%) between NSSI-ND and NNSSI-ND and in two pairs between NSSI-D and NNSSI-ND. For detailed comparisons of edge weights and significant variance, refer to Supplementary Tables 1-3.
DISCUSSION
This study provides significant insights into the complex nature of NSSI among Chinese adolescents by employing a combination of LPA and network analysis. By identifying distinct subgroups based on NSSI behaviors and depressive symptoms, and exploring the interactions between risk and protective factors, we have advanced the understanding of NSSI's multifaceted etiology.
Interpretation of key findings
The identification of three distinct subgroups-NSSI-D, NSSI-ND, and NNSSI-ND-highlights the heterogeneity of NSSI behaviors. This heterogeneity underscores the importance of not treating NSSI as a homogeneous behavior, as different subgroups may have unique underlying mechanisms and require tailored interventions[16].
Our network analysis revealed that bullying is a central risk factor, especially in the NSSI-D subgroup. This finding aligns with prior research indicating that experiences of bullying are significantly associated with both depressive symptoms and NSSI behaviors[17]. Adolescents who are bullied may internalize negative self-perceptions and experience heightened emotional distress, leading to depressive symptoms. Consequently, the likelihood of engaging in NSSI as a maladaptive coping mechanism increases[18].
In contrast, the NSSI-ND subgroup showed a distinct pattern where smartphone addiction emerged as a notable factor. This suggests that adolescents engaging in NSSI without concurrent depressive symptoms may be using excessive smartphone use as an alternative or complementary coping strategy to manage emotional distress[19]. The accessibility and immediacy of digital media may provide temporary relief but could also reinforce avoidance behaviors and hinder the development of healthier coping mechanisms[20].
FS and EC were identified as key protective factors across all subgroups. High levels of FS may buffer the impact of stressors by providing emotional resources and a sense of belonging, which can mitigate the need for self-injurious behaviors[21]. EC, as an aspect of emotional regulation, enables adolescents to manage negative emotions more effectively, reducing the reliance on NSSI as a means of coping[22].
Theoretical implications
The findings support the interpersonal theory of NSSI, which posits that social factors such as bullying and family dynamics play a critical role in the initiation and maintenance of self-injurious behaviors[23]. The centrality of bullying in the NSSI-D subgroup suggests that negative interpersonal experiences are particularly detrimental when coupled with internalizing symptoms like depression.
Moreover, the study extends the application of the diathesis-stress model to NSSI by illustrating how individual vulnerabilities (e.g., poor EC) interact with environmental stressors (e.g., bullying) to influence the onset of self-injury[24]. The identification of protective factors such as FS highlights the potential moderating effects these elements can have on the stress-NSSI relationship.
Clinical implications
The differentiated profiles of NSSI behaviors have important implications for intervention strategies. For adolescents in the NSSI-D subgroup, interventions should involve a multi-faceted approach that addresses both depressive symptoms and experiences of bullying. Cognitive-behavioral therapy techniques can be effective in challenging negative thought patterns and enhancing problem-solving skills[25]. School-based programs that foster a positive social climate and implement anti-bullying policies may also reduce the prevalence of both bullying and NSSI[26].
For the NSSI-ND subgroup, interventions might focus on regulating technology use and promoting alternative coping strategies. Digital literacy programs that educate adolescents about the risks of excessive smartphone use and provide tools for managing screen time could be beneficial[27]. Incorporating mindfulness and stress management techniques can help adolescents develop healthier ways to cope with emotional distress[28].
Family-based interventions are crucial across all subgroups. Enhancing communication within the family, increasing parental awareness of NSSI, and fostering supportive relationships can strengthen the protective role of the family environment[29]. Parental training programs that focus on emotion coaching and responsive parenting may improve adolescents' emotional regulation abilities and reduce NSSI behaviors[30].
Cultural considerations
The cultural context in China, characterized by collectivism and strong familial ties, amplifies the influence of FS on adolescent behavior[31]. The emphasis on academic achievement and adherence to social norms may contribute to stress and emotional difficulties among adolescents[32]. Understanding these cultural factors is essential for designing interventions that are culturally sensitive and resonate with adolescents and their families.
Additionally, the stigma associated with mental health issues in Chinese society may hinder help-seeking behaviors. Efforts to destigmatize mental health problems through public education campaigns and integrating mental health services within schools could improve access to support and reduce the incidence of NSSI.
Limitations
This study has several limitations. The cross-sectional design limits the ability to infer causal relationships between risk factors, protective factors, and NSSI behaviors. Therefore, longitudinal studies are needed to examine how these relationships evolve and identify potential causal pathways.
The reliance on self-reported data may introduce biases, such as social desirability or recall inaccuracies. Future research could incorporate multiple data sources, including reports from parents, teachers, or clinical assessments, to enhance the validity of the findings.
The sample was drawn from a specific geographic region in China, which may limit the generalizability of the results to other regions or cultural contexts. Replication studies in diverse settings are necessary to confirm the applicability of these findings more broadly.
Future research directions
Building on the current findings, future research should employ longitudinal designs to explore the developmental trajectories of NSSI behaviors and the temporal dynamics between risk and protective factors. Investigating the mechanisms through which bullying leads to NSSI, particularly the mediating role of depression and emotional regulation, could inform more targeted interventions.
Examining the impact of digital media use in greater depth is also warranted, given the evolving nature of technology and its pervasive influence on adolescents' lives. Studies could explore how online interactions, cyberbullying, and social media exposure contribute to NSSI behaviors and mental health outcomes[33].
Additionally, qualitative research methods could provide richer insights into adolescents' subjective experiences of NSSI, capturing the nuances of their motivations, feelings, and contextual factors. Such insights could enhance the development of personalized intervention strategies that resonate with adolescents' lived experiences.
CONCLUSION
This study enhances the understanding of NSSI among Chinese adolescents by identifying distinct behavioral subgroups and elucidating the complex interplay of associated risk and protective factors. The findings emphasize the importance of considering individual differences and cultural contexts in both research and clinical practice. By tailoring interventions to address specific needs-such as bullying prevention, emotional regulation training, and FS enhancement-we can develop more effective strategies to reduce NSSI behaviors and promote mental well-being among adolescents.
ACKNOWLEDGEMENTS
The authors would like to thank Lei Zhang and Yun-Yong Gao for their assistance in data collection. We also extend our gratitude to Professor Yuan-Yuan Xiao from Kunming Medical University for providing valuable guidance on the questionnaire survey, project design, and data analysis.
Footnotes
Institutional review board statement: The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Kunming Medical University (Approval Number: KMMU2020MEC047) in September 2021.
Clinical trial registration statement: This study does not involve clinical trials and is not applicable.
Informed consent statement: All study participants or their legal guardians provided informed written consent before study enrollment.
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade C
Novelty: Grade B
Creativity or Innovation: Grade B
Scientific Significance: Grade B
P-Reviewer: Zeng P S-Editor: Li L L-Editor: A P-Editor: Zheng XM
Contributor Information
Wei Yang, Department of Psychiatry, The First Affiliated Hospital of Kunming Medical University, Kunming 650032, Yunnan Province, China.
Kun Lian, Department of Neurosurgery, The Second Affiliated Hospital of Kunming Medical University, Kunming 650101, Yunnan Province, China.
Yu-Qi Cheng, Department of Psychiatry, The First Affiliated Hospital of Kunming Medical University, Kunming 650032, Yunnan Province, China.
Xiu-Feng Xu, Department of Psychiatry, The First Affiliated Hospital of Kunming Medical University, Kunming 650032, Yunnan Province, China. xfxu2004@sina.com.
Xin-Cen Duan, Department of Psychiatry, Zhongshan Hospital Affiliated to Fudan University, Shanghai 201100, China.
Xu You, Department of Psychiatry, Honghe Second People's Hospital, Honghe 651400, Yunnan Province, China.
Data sharing statement
Data supporting the findings of this study are available from the corresponding author upon reasonable request at xfxu2004@sina.com.
References
- 1.Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life Threat Behav. 2014;44:273–303. doi: 10.1111/sltb.12070. [DOI] [PubMed] [Google Scholar]
- 2.Baldwin JR, Arseneault L, Caspi A, Moffitt TE, Fisher HL, Odgers CL, Ambler A, Houts RM, Matthews T, Ougrin D, Richmond-Rakerd LS, Takizawa R, Danese A. Adolescent Victimization and Self-Injurious Thoughts and Behaviors: A Genetically Sensitive Cohort Study. J Am Acad Child Adolesc Psychiatry. 2019;58:506–513. doi: 10.1016/j.jaac.2018.07.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawton K, Casañas I Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013;147:17–28. doi: 10.1016/j.jad.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 4.Wang YJ, Li X, Ng CH, Xu DW, Hu S, Yuan TF. Risk factors for non-suicidal self-injury (NSSI) in adolescents: A meta-analysis. EClinicalMedicine. 2022;46:101350. doi: 10.1016/j.eclinm.2022.101350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Teicher MH, Samson JA, Anderson CM, Ohashi K. The effects of childhood maltreatment on brain structure, function and connectivity. Nat Rev Neurosci. 2016;17:652–666. doi: 10.1038/nrn.2016.111. [DOI] [PubMed] [Google Scholar]
- 6.Brown RC, Heines S, Witt A, Braehler E, Fegert JM, Harsch D, Plener PL. The impact of child maltreatment on non-suicidal self-injury: data from a representative sample of the general population. BMC Psychiatry. 2018;18:181. doi: 10.1186/s12888-018-1754-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Borsboom D, Cramer AO. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9:91–121. doi: 10.1146/annurev-clinpsy-050212-185608. [DOI] [PubMed] [Google Scholar]
- 8.van Borkulo CD, van Bork R, Boschloo L, Kossakowski JJ, Tio P, Schoevers RA, Borsboom D, Waldorp LJ. Comparing network structures on three aspects: A permutation test. Psychol Methods. 2023;28:1273–1285. doi: 10.1037/met0000476. [DOI] [PubMed] [Google Scholar]
- 9.Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: A tutorial paper. Behav Res Methods. 2018;50:195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.He H, Hong L, Jin W, Xu Y, Kang W, Liu J, Song J, Zheng T, Chen H, Zhao K. Heterogeneity of non-suicidal self-injury behavior in adolescents with depression: latent class analysis. BMC Psychiatry. 2023;23:301. doi: 10.1186/s12888-023-04808-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nylund KL, Asparouhov T, Muthén BO. Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14:535–569. [Google Scholar]
- 12.Friedman J, Hastie T, Tibshirani R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics. 2008;9:432–441. doi: 10.1093/biostatistics/kxm045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mcnally RJ, Robinaugh DJ, Wu GWY, Wang L, Deserno MK, Borsboom D. Mental Disorders as Causal Systems. Clin Psychol Sci. 2015;3:836–849. [Google Scholar]
- 14.Borsboom D, Fried EI, Epskamp S, Waldorp LJ, van Borkulo CD, van der Maas HLJ, Cramer AOJ. False alarm? A comprehensive reanalysis of "Evidence that psychopathology symptom networks have limited replicability" by Forbes, Wright, Markon, and Krueger (2017) J Abnorm Psychol. 2017;126:989–999. doi: 10.1037/abn0000306. [DOI] [PubMed] [Google Scholar]
- 15.Epskamp S, Kruis J, Marsman M. Estimating psychopathological networks: Be careful what you wish for. PLoS One. 2017;12:e0179891. doi: 10.1371/journal.pone.0179891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zetterqvist M. The DSM-5 diagnosis of nonsuicidal self-injury disorder: a review of the empirical literature. Child Adolesc Psychiatry Ment Health. 2015;9:31. doi: 10.1186/s13034-015-0062-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baiden P, Stewart SL, Fallon B. The mediating effect of depressive symptoms on the relationship between bullying victimization and non-suicidal self-injury among adolescents: Findings from community and inpatient mental health settings in Ontario, Canada. Psychiatry Res. 2017;255:238–247. doi: 10.1016/j.psychres.2017.05.018. [DOI] [PubMed] [Google Scholar]
- 18.Guan K, Fox KR, Prinstein MJ. Nonsuicidal self-injury as a time-invariant predictor of adolescent suicide ideation and attempts in a diverse community sample. J Consult Clin Psychol. 2012;80:842–849. doi: 10.1037/a0029429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elhai JD, Rozgonjuk D, Yildirim C, Alghraibeh AM, Alafnan AA. Worry and anger are associated with latent classes of problematic smartphone use severity among college students. J Affect Disord. 2019;246:209–216. doi: 10.1016/j.jad.2018.12.047. [DOI] [PubMed] [Google Scholar]
- 20.Nikolic A, Bukurov B, Kocic I, Vukovic M, Ladjevic N, Vrhovac M, Pavlović Z, Grujicic J, Kisic D, Sipetic S. Smartphone addiction, sleep quality, depression, anxiety, and stress among medical students. Front Public Health. 2023;11:1252371. doi: 10.3389/fpubh.2023.1252371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tatnell R, Kelada L, Hasking P, Martin G. Longitudinal analysis of adolescent NSSI: the role of intrapersonal and interpersonal factors. J Abnorm Child Psychol. 2014;42:885–896. doi: 10.1007/s10802-013-9837-6. [DOI] [PubMed] [Google Scholar]
- 22.Adrian M, Zeman J, Erdley C, Lisa L, Sim L. Emotional dysregulation and interpersonal difficulties as risk factors for nonsuicidal self-injury in adolescent girls. J Abnorm Child Psychol. 2011;39:389–400. doi: 10.1007/s10802-010-9465-3. [DOI] [PubMed] [Google Scholar]
- 23.Nock MK. Why do People Hurt Themselves? New Insights Into the Nature and Functions of Self-Injury. Curr Dir Psychol Sci. 2009;18:78–83. doi: 10.1111/j.1467-8721.2009.01613.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O'Connor TG, Matias C, Futh A, Tantam G, Scott S. Social learning theory parenting intervention promotes attachment-based caregiving in young children: randomized clinical trial. J Clin Child Adolesc Psychol. 2013;42:358–370. doi: 10.1080/15374416.2012.723262. [DOI] [PubMed] [Google Scholar]
- 25.Muehlenkamp JJ, Kerr PL, Bradley AR, Adams Larsen M. Abuse subtypes and nonsuicidal self-injury: preliminary evidence of complex emotion regulation patterns. J Nerv Ment Dis. 2010;198:258–263. doi: 10.1097/NMD.0b013e3181d612ab. [DOI] [PubMed] [Google Scholar]
- 26.Evans CB, Fraser MW, Cotter KL. The effectiveness of school-based bullying prevention programs: A systematic review. Aggress Violent Behav. 2014;19:532–544. [Google Scholar]
- 27.Kuss DJ, Lopez-Fernandez O. Internet addiction and problematic Internet use: A systematic review of clinical research. World J Psychiatry. 2016;6:143–176. doi: 10.5498/wjp.v6.i1.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hasking P, Whitlock J, Voon D, Rose A. A cognitive-emotional model of NSSI: using emotion regulation and cognitive processes to explain why people self-injure. Cogn Emot. 2017;31:1543–1556. doi: 10.1080/02699931.2016.1241219. [DOI] [PubMed] [Google Scholar]
- 29.Guilé JM, Boissel L, Alaux-Cantin S, de La Rivière SG. Borderline personality disorder in adolescents: prevalence, diagnosis, and treatment strategies. Adolesc Health Med Ther. 2018;9:199–210. doi: 10.2147/AHMT.S156565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eisenberg N, Spinrad TL, Eggum ND. Emotion-related self-regulation and its relation to children's maladjustment. Annu Rev Clin Psychol. 2010;6:495–525. doi: 10.1146/annurev.clinpsy.121208.131208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang T, Gai X, Wang S, Gai S. The Relationship between Parenting Behaviors and Adolescent Well-Being Varies with the Consistency of Parent-Adolescent Cultural Orientation. Behav Sci (Basel) 2024;14:193. doi: 10.3390/bs14030193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jiang MM, Gao K, Wu ZY, Guo PP. The influence of academic pressure on adolescents' problem behavior: Chain mediating effects of self-control, parent-child conflict, and subjective well-being. Front Psychol. 2022;13:954330. doi: 10.3389/fpsyg.2022.954330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Moreno MA, Jelenchick LA, Egan KG, Cox E, Young H, Gannon KE, Becker T. Feeling bad on Facebook: depression disclosures by college students on a social networking site. Depress Anxiety. 2011;28:447–455. doi: 10.1002/da.20805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Martin A, Rief W, Klaiberg A, Braehler E. Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. Gen Hosp Psychiatry. 2006;28:71–77. doi: 10.1016/j.genhosppsych.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 35.Feng X, Shaw DS, Silk JS. Developmental trajectories of anxiety symptoms among boys across early and middle childhood. J Abnorm Psychol. 2008;117:32–47. doi: 10.1037/0021-843X.117.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jiang J, Lu ZR, Jiang BJ, Xu Y. [Revision of the Short-form Egna Minnenav Barndoms Uppfostran for Chinese] Xinli Fazhan Yu Jiaoyu. 2010;26:94–99. [Google Scholar]
- 37.Bernstein DP, Fink L. Childhood Trauma Questionnaire: A retrospective self-report manual. San Antonio, TX: The Psychological Corporation, 1998. [Google Scholar]
- 38.Solberg M, Olweus D. Prevalence estimation of school bullying with the Olweus Bully/Victim Questionnaire. Aggressive Behav. 2003;29:239–268. [Google Scholar]
- 39.Hu YQ, Gan YQ. [Development and psychometric validity of the resilience scale for Chinese adolescents] Xinli Xuebao. 2008;40:902–912. [Google Scholar]
- 40.Leung L. Linking psychological attributes to addiction and improper use of the mobile phone among adolescents in Hong Kong. J Child Media. 2008;2:93–113. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data supporting the findings of this study are available from the corresponding author upon reasonable request at xfxu2004@sina.com.