Abstract
Psychiatric disorders and heart abnormality are closely interconnected. Previous knowledge has been well-established that psychiatric disorders can lead to increased cardiovascular morbidity and even sudden cardiac death. Conversely, whether heart abnormality contributes to psychiatric disorders remains rarely studied. The work by Zhang et al pointed out that chronic heart failure had effects on the anxiety and depression (AD) severity, and indices including left ventricular ejection fraction, N-terminal pro-brain natriuretic peptide and interleukin-6 were independent risk factors for AD severity. In addition to the aforementioned AD, we herein find that heart failure might additionally impact the development of autism spectrum disorder and post-traumatic stress disorder (albeit P > 0.05), and significantly protects against the presence of attention deficit hyperactivity disorder (ADHD), [odds ratio (OR) = 0.61, P = 0.0071] by using a Mendelian randomization analysis. Bradycardia is also a protective factor for ADHD (OR = 0.61, P = 0.0095), whereas hypertrophic cardiomyopathy is a mild risk factor for schizophrenia (OR = 1.02, P = 0.032). These data suggest a wide spectrum of psychiatric disorders secondary to heart abnormality, and we highlight more psychiatric care that should be paid to patients with heart abnormality.
Keywords: Psychiatric disorders, Schizophrenia, Heart abnormality, Heart failure, Mendelian randomization analyses
Core Tip: Numerous studies have reported the effects of psychiatric disorders on heart dysfunction. Little attention has been paid to the effects of heart abnormality on psychiatric status. We highlight that in addition to the impact on anxiety and depression, heart failure might further contribute to increased risks of autism spectrum disorder and post-traumatic stress disorder, and protects from the development of attention deficit hyperactivity disorder (ADHD). Furthermore, bradycardia is a protective factor for ADHD, and hypertrophic cardiomyopathy may significantly contribute to the presence of schizophrenia. Heart abnormality is associated with a wide spectrum of psychiatric disorders.
TO THE EDITOR
We read with interest the recent article by Zhang et al[1]. This paper demonstrates that heart disease influences the development of psychiatric disorders [anxiety and depression (AD)] through the humoral circulation approach. Myocardial markers and inflammatory factors such as left ventricular ejection fraction, N-terminal pro-Brain natriuretic peptide and interleukin-6 can predict the AD severity in patients with chronic heart failure. This study suggests that cardiac dysfunction may contribute to psychiatric disorders.
In recent years, an increasing amount of evidence has underscored the heart dysfunction in patients with psychiatric disorders (summarized in Table 1)[2-8]. For example, researchers found that depression[2], attention deficit hyperactivity disorder (ADHD)[3] and post-traumatic stress disorder (PTSD)[4] were associated with increased risks of cardiovascular disease. Similarly, a recent report[5], as well as our study[6], have found a significantly higher rate of sudden cardiac death in patients with schizophrenia. Activation of dopaminergic neurons linked to psychiatric disorders enhances cardiac remodeling following acute myocardial infarction[9]. The impact of these psychiatric disorders on cardiac function stems from genetic variations, modulation of neurocircuitry and the cardiotoxicity of anti-psychotropic medications[3,10].
Table 1.
Cardiovascular symptoms in patients with psychiatric disorders
|
Primary psychiatric disorder
|
Secondary cardiovascular symptom
|
Ref.
|
| Depression | Cardiovascular disease and mortality | Rajan et al[2] |
| ADHD | Hypertension and arterial disease | Zhang et al[3] |
| PTSD | Coronary artery disease | Walczewska et al[4] |
| Schizophrenia | Sudden cardiac death | Dimsdale[5]; Wang et al[6] |
| Autism | High heart rate | Klusek et al[7] |
| Bipolar disorder | Heart failure | Chen et al[8] |
ADHD: Attention deficit hyperactivity disorder; PTSD: Post-traumatic stress disorder.
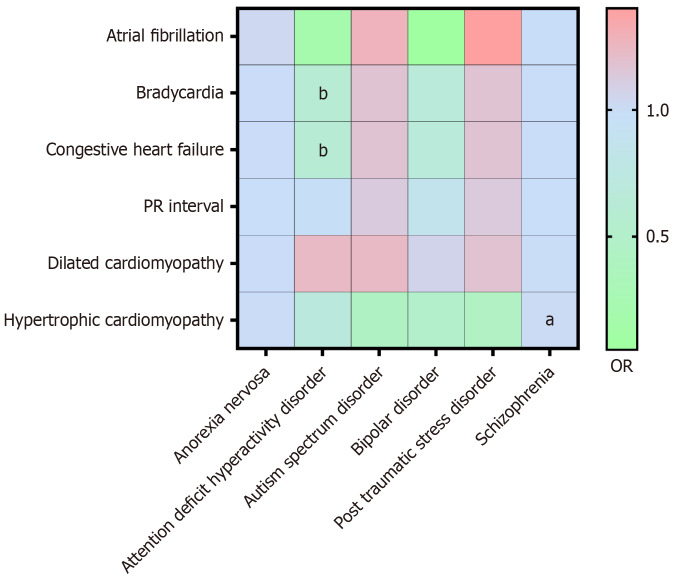
On the other hand, little attention has been paid to the impact of heart abnormality on psychiatric status. In addition to the aforementioned study[1], a pioneering study found that a faster heart rate can cause an increase in anxiety through activation of the insula cortex[11], shedding light on the potential role that normal heart function plays in maintaining mental health. Whether heart abnormality has any impact on other psychiatric disorders beyond AD, however, remains to be evaluated. Herein, using a Mendelian randomization analysis, we further assessed whether there is a causal relationship between genetic variation in heart phenotypes and the development of psychiatric disorders. Single nucleotide polymorphism data from genome-wide association study were extracted for exposure factors (heart abnormality) including atrial fibrillation, bradycardia, congestive heart failure, PR intervals, dilated cardiomyopathy, and hypertrophic cardiomyopathy, and for outcome factors (psychiatric disorder) encompassing anorexia nervosa, ADHD, autism disorders, bipolar disorder, PTSD, and schizophrenia (Figure 1). The results showed that heart failure might also contribute to the development of autism spectrum disorder [odds ratio (OR) = 1.1695, P = 0.3797] and PTSD (OR = 1.1725, P = 0.3358), albeit differences not reaching a statistical significance. Interestingly, heart failure (OR = 0.61, P = 0.0095) and bradycardia (OR = 0.61, P = 0.0071) are observed to significantly protect against the presence of ADHD. Hypertrophic cardiomyopathy, however, is observed to significantly contribute to the presence of schizophrenia (OR = 1.02, P = 0.032). These results extend the content of the original study[1] and illustrate the important regulatory role of heart abnormality in mental health.
Figure 1.
A Mendelian randomization analysis of heart abnormality (exposure factor, longitudinal axis) to psychiatric disorders (outcome, horizontal axis). The odds ratio (OR) is represented by color code, with OR values greater than 1 shown in red, less than 1 shown in green, and close to 1 shown in blue. OR values become greater from the bottom to the top of the color bar. Statistical significance is indicated by the letter, while the absence of letters indicates no statistical significance. aP < 0.05. bP < 0.01. OR: Odds ratio.
CONCLUSION
In summary, there is a close interplay between heart abnormality and mental health. Numerous studies have underscored the impact of psychiatric disorders on heart dysfunction, while less is known on whether heart abnormality influences psychiatric status. The study by Zhang et al[1] have confirmed that heart failure is indeed associated with the AD severity from a humoral cycle perspective, and our Mendelian randomization analysis further extends this conclusion from a genetic standpoint. The results indicate that heart failure might also contribute to the development of autism spectrum disorder and PTSD; heart failure and bradycardia are independent protective factors for ADHD. Hypertrophic cardiomyopathy is a significant risk factor for schizophrenia. Collectively, these data suggest a wide spectrum of psychiatric disorders following heart abnormality. Early screening and monitoring of psychiatric symptoms should be conducted in patients with heart abnormality especially heart failure and hypertrophic cardiomyopathy.
Footnotes
Conflict-of-interest statement: The authors declare that they have no conflict of interest.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country of origin: China
Peer-review report’s classification
Scientific Quality: Grade B, Grade B
Novelty: Grade B, Grade C
Creativity or Innovation: Grade C, Grade C
Scientific Significance: Grade B, Grade B
P-Reviewer: Krstulović J S-Editor: Fan M L-Editor: A P-Editor: Zheng XM
Contributor Information
Xue-Shi Chen, Department of Forensic Medicine, School of Basic Medical Sciences, Fudan University, Shanghai 200032, China.
Zi-Yan Song, Department of Forensic Medicine, School of Basic Medical Sciences, Fudan University, Shanghai 200032, China.
Xuan-Long Chen, Department of Forensic Medicine, School of Basic Medical Sciences, Fudan University, Shanghai 200032, China.
Yi-Ming Bo, Department of Forensic Medicine, School of Basic Medical Sciences, Fudan University, Shanghai 200032, China.
Li-Liang Li, Department of Forensic Medicine, School of Basic Medical Sciences, Fudan University, Shanghai 200032, China. liliangli11@fudan.edu.cn.
References
- 1.Zhang L, Wang Q, Cui HS, Luo YY. Assessing myocardial indices and inflammatory factors to determine anxiety and depression severity in patients with chronic heart failure. World J Psychiatry. 2024;14:53–62. doi: 10.5498/wjp.v14.i1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rajan S, McKee M, Rangarajan S, Bangdiwala S, Rosengren A, Gupta R, Kutty VR, Wielgosz A, Lear S, AlHabib KF, Co HU, Lopez-Jaramillo P, Avezum A, Seron P, Oguz A, Kruger IM, Diaz R, Nafiza MN, Chifamba J, Yeates K, Kelishadi R, Sharief WM, Szuba A, Khatib R, Rahman O, Iqbal R, Bo H, Yibing Z, Wei L, Yusuf S Prospective Urban Rural Epidemiology (PURE) Study Investigators. Association of Symptoms of Depression With Cardiovascular Disease and Mortality in Low-, Middle-, and High-Income Countries. JAMA Psychiatry. 2020;77:1052–1063. doi: 10.1001/jamapsychiatry.2020.1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang L, Li L, Andell P, Garcia-Argibay M, Quinn PD, D'Onofrio BM, Brikell I, Kuja-Halkola R, Lichtenstein P, Johnell K, Larsson H, Chang Z. Attention-Deficit/Hyperactivity Disorder Medications and Long-Term Risk of Cardiovascular Diseases. JAMA Psychiatry. 2024;81:178–187. doi: 10.1001/jamapsychiatry.2023.4294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walczewska J, Rutkowski K, Wizner B, Cwynar M, Grodzicki T. Stiffness of large arteries and cardiovascular risk in patients with post-traumatic stress disorder. Eur Heart J. 2011;32:730–736. doi: 10.1093/eurheartj/ehq354. [DOI] [PubMed] [Google Scholar]
- 5.Dimsdale JE. Sudden Cardiac Death and Schizophrenia. JACC Clin Electrophysiol. 2023;9:1319–1320. doi: 10.1016/j.jacep.2023.02.011. [DOI] [PubMed] [Google Scholar]
- 6.Wang S, He M, Andersen J, Lin Y, Zhang M, Liu Z, Li L. Sudden unexplained death in schizophrenia patients: An autopsy-based comparative study from China. Asian J Psychiatr. 2023;79:103314. doi: 10.1016/j.ajp.2022.103314. [DOI] [PubMed] [Google Scholar]
- 7.Klusek J, Roberts JE, Losh M. Cardiac autonomic regulation in autism and Fragile X syndrome: a review. Psychol Bull. 2015;141:141–175. doi: 10.1037/a0038237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen PH, Chiang SJ, Hsiao CY, Shen RS, Lin YK, Chung KH, Tsai SY. Echocardiographic study of cardiac structure and function in people with bipolar disorder after midlife. J Affect Disord. 2022;296:428–433. doi: 10.1016/j.jad.2021.09.089. [DOI] [PubMed] [Google Scholar]
- 9.Haykin H, Avishai E, Krot M, Ghiringhelli M, Reshef M, Abboud Y, Melamed S, Merom S, Boshnak N, Azulay-Debby H, Ziv T, Gepstein L, Rolls A. Reward system activation improves recovery from acute myocardial infarction. Nat Cardiovasc Res. 2024;3:841–856. doi: 10.1038/s44161-024-00491-3. [DOI] [PubMed] [Google Scholar]
- 10.Li XQ, Tang XR, Li LL. Antipsychotics cardiotoxicity: What's known and what's next. World J Psychiatry. 2021;11:736–753. doi: 10.5498/wjp.v11.i10.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hsueh B, Chen R, Jo Y, Tang D, Raffiee M, Kim YS, Inoue M, Randles S, Ramakrishnan C, Patel S, Kim DK, Liu TX, Kim SH, Tan L, Mortazavi L, Cordero A, Shi J, Zhao M, Ho TT, Crow A, Yoo AW, Raja C, Evans K, Bernstein D, Zeineh M, Goubran M, Deisseroth K. Cardiogenic control of affective behavioural state. Nature. 2023;615:292–299. doi: 10.1038/s41586-023-05748-8. [DOI] [PMC free article] [PubMed] [Google Scholar]