Abstract
Objective
To explore variation in rates of acute care utilization for mental health conditions, including hospitalizations and emergency department (ED) visits, across high‐income countries before and during the COVID‐19 pandemic.
Data Sources and Study Setting
Administrative patient‐level data between 2017 and 2020 of eight high‐income countries: Canada, England, Finland, France, New Zealand, Spain, Switzerland, and the United States (US).
Study Design
Multi‐country retrospective observational study using a federated data approach that evaluated age‐sex standardized rates of hospitalizations and ED visits for mental health conditions.
Principal Findings
There was significant variation in rates of acute mental health care utilization across countries. Among the subset of four countries with both hospitalization and ED data, the US had the highest pre‐COVID‐19 combined average annual acute care rate of 1613 episodes/100,000 people (95% CI: 1428, 1797). Finland had the lowest rate of 776 (686, 866). When examining hospitalization rates only, France had the highest rate of inpatient hospitalizations of 988/100,000 (95% CI 858, 1118) while Spain had the lowest at 87/100,000 (95% CI 76, 99). For ED rates for mental health conditions, the US had the highest rate of 958/100,000 (95% CI 861, 1055) while France had the lowest rate with 241/100,000 (95% CI 216, 265). Notable shifts coinciding with the onset of the COVID‐19 pandemic were observed including a substitution of care setting in the US from ED to inpatient care, and overall declines in acute care utilization in Canada and France.
Conclusion
The study underscores the importance of understanding and addressing variation in acute care utilization for mental health conditions, including the differential effect of COVID‐19, across different health care systems. Further research is needed to elucidate the extent to which factors such as workforce capacity, access barriers, financial incentives, COVID‐19 preparedness, and community‐based care may contribute to these variations.
What is known on this topic
Approximately one billion people globally live with a mental health condition, with significant consequences for individuals and societies.
Rates of mental health diagnoses vary across high‐income countries, with substantial differences in access to effective care.
The COVID‐19 pandemic has exacerbated mental health challenges globally, with varying impacts across countries.
What this study adds
This study provides a comprehensive international comparison of hospitalization and emergency department visit rates for mental health conditions across eight high‐income countries.
It highlights significant variations in acute care utilization patterns, particularly in countries that are more likely to care for people with mental health conditions in emergency departments rather than inpatient facilities
The study identifies temporal and cross‐country differences in acute care management of mental health conditions coinciding with the onset of the COVID‐19 pandemic.
Keywords: access/demand/utilization of services, acute inpatient care, comparative health systems/international health, health care organizations and systems, mental health
1. INTRODUCTION
Addressing issues related to mental health and well‐being are global priorities. 1 Approximately one billion people globally—or about one in every eight people—live with a mental health condition, including depression, bipolar disorder, anxiety, and schizophrenia or related psychotic disorders. 2 The consequences of poorly controlled mental health can be substantial for individuals, including increased risk of unemployment, substance use, homelessness, incarceration, suicide, worsening of other underlying medical conditions, and poor quality of life. 3 , 4 , 5 , 6 Globally, in 2019, mental illness was estimated to account for 418 million disability‐adjusted life years with an economic cost of approximately USD $5 trillion. 7
Among adults in high‐income countries, there is considerable variation in the estimated annual prevalence of mental health conditions, ranging from 13.5% in Canada to 17.2% in New Zealand. 8 Some estimates suggest that the lifetime prevalence of mental health disorders in the United States may be as high as 23%. 9 While effective prevention and treatment options exist, most people with mental health conditions do not have access to effective care. 10 For example, globally, only 29% of people with psychosis 11 , 12 and only one‐third of those with depression receive formal mental health care treatment. 13 Moreover, the Organization for Economic Co‐operation and Development (OECD) reported that the prevalence of anxiety and depression symptoms has substantially increased around the world since the COVID‐19 pandemic, with significant variation across countries. 14 , 15
Therefore, there is a widespread concern that countries are facing substantial challenges caring for people with mental health conditions. This may result in individuals increasingly seeking care in acute hospitals and emergency rooms. Over recent years, there has been a fundamental shift in mental health care, moving from institutionalization to community‐based treatment that promotes social integration for patients. 16 However, among Western countries, this transition has varied significantly. Moreover, cross‐country differences in health system organizational and financial structures, mental health workforce capacity and capability, and cost‐related access to care barriers, 9 mean there is likely to be considerable variation in the absolute and relative use of hospitalizations and emergency department (ED) visits among people with mental health conditions. Publicly funded and universal coverage health care systems often emphasize outpatient and community‐based care but can face challenges such as long wait times, insufficient funding, and workforce shortages. 17 , 18 By contrast, predominantly private systems or systems with high out‐of‐pocket costs and cost‐sharing, like in the United States, can experience significant gaps in service coverage and financial barriers to access that may lead to higher rates of acute care use than other countries. 19
While some research has been conducted comparing mental health outcomes across countries, the literature remains sparse, particularly regarding acute care mental health events. For example, a Commonwealth Fund survey analysis compared mental health service utilization and unmet needs between the United States and 10 other high‐income countries. 9 It found significant disparities in mental health diagnosis and suicide rates, access and affordability, and workforce capacity. The OECD's “Health at a Glance” report provides data on mental health services across various countries, but it largely discusses broader health care system metrics rather than acute care specifics. 20 Additionally, a study on adolescent psychosomatic symptoms in Nordic countries offered some insights into health care impacts on mental health, yet it does not directly explore acute mental health care events. 21 Therefore, the extent to which countries are treating people for mental health conditions in acute care settings, or whether there is evidence of differential treatment in emergency rooms versus inpatient hospital settings, is not well understood, especially during the COVID‐19 pandemic. To improve health care for this population, understanding variation in differences of acute health care service use can be informative for national policymakers and health system leaders' efforts to inform potential strategies and tailor interventions. If concerning high rates of acute care use exist in some countries, it can also guide policymakers and clinical leaders into further inquiry to identify underlying mechanisms of why their population may be more at risk for acute care use with mental health conditions.
Therefore, as part of the International Collaborative of Costs, Outcomes, and Needs in Care, a research collaborative focused on international health comparisons, 22 , 23 , 24 we sought to answer the following key questions using nationally representative data across eight countries: Canada, England, Finland, France, New Zealand, Spain, Switzerland, and the United States.
First, are there differences across high‐income countries and over time in rates of hospitalizations related to mental health conditions, including conditions related to serious mental health versus other mental health conditions? Second, among a subset of countries with ED data available, are there differences in rates of ED visits for mental health conditions that do not result in hospital admission as well as in the relative rate of treatment in the ED versus inpatient setting? Third, is there variation across countries in acute care episodes related to mental health conditions arising during the first year of the COVID‐19 pandemic?
2. METHODS
2.1. Study design and data
This study was a multi‐country retrospective, observational study using administrative patient‐level data from 2017 to 2020 across eight countries: Canada, England, Finland, France, New Zealand, Spain, Switzerland, and the United States. Participating countries were selected as they are high‐income countries with access to high‐quality individual‐level administrative health data and represent a mix of health system types. All countries except Finland were original members of the International Collaborative of Costs, Outcomes, and Needs in Care network which formed in 2018. Finland was a recent addition to the collaborative in 2020. Collectively, these nations represent high‐income countries with significant health care expenditures. However, there is notable heterogeneity in their funding mechanisms and organizational structures that may drive differences in acute care visits related to mental health conditions (for more details on health system differences, see Table S1).
Datasets for this study were prioritized for inclusion if they were nationally representative or at least covered a substantial proportion of a country's population. Five countries—England, Finland, France, New Zealand, and Switzerland—used national datasets that covered the entire country's population. Three countries—Canada, Spain, and the United States—used large datasets that covered a substantial proportion of their populations. Data for Canada were from the province of Ontario, which represents 39.4% of the Canadian population. Data from Spain covered 88.2% of the Spanish population. These data did not include the Ceuta, Melilla, Castilla y León y Galicia regions from which data were not available the years of study. Data from the United States were from a national sample of insurance claims that included about 90 million unique beneficiaries between 2017 and 2020; in 2020, the sample included 49,059,761 unique people, representing about 15% of the United States population. Each country provided data for the time period January 1, 2017, until December 31, 2020.
Each country provided inpatient admissions data; however, ED data were only available for four countries: Canada, Finland, France, and the United States. Canada utilized the Canadian Institute for Health Information administrative claims data from the province of Ontario, a comprehensive dataset that includes records of health service utilization covered under the Ontario Health Insurance Plan, to provide inpatient and ED events. Hospital admissions data for England were derived from Hospital Episode Statistics Admitted Patient Care, a national collection of all NHS‐funded hospital admissions. Inpatient and ED data for Finland were drawn from the Care Register for Health Care, a whole‐of‐population administrative data set of all inpatient admissions and ED presentations. France provided inpatient and ED data from the Système National des Données de Santé (National Health Data System), a universal whole‐of‐population, health insurance claims database. Hospital admission data from the National Minimum Dataset, a national collection of all publicly funded hospital inpatient stays, were used for New Zealand. Switzerland used data from the Statistique médicale des hôpitaux/Medizinische Statistik der Krankenhäuser (Medical Hospital Statistics of the Federal Statistical Office), an administrative claims database of all hospitalizations. For the United States, the Real‐World Data from Inovalon Insights—a medical claims database that includes a large sample of insured populations in the US enrolled in Medicaid (42%), Medicare (6%), and commercial insurance (57%)—was used to provide inpatient and ED event information (for more detail pertaining to each country's data, see Table S2).
2.2. Defining episodes for mental health conditions
We used the International Classification of Diseases, Tenth Revision diagnostic codes to identify inpatient hospitalizations and ED visits with a primary diagnosis related to mental health conditions overall as well by two categorizations: (1) serious mental health conditions, which include conditions for major depressive disorder, bipolar disorder, schizophrenia, or related psychotic disorders, as defined by prior work, 25 , 26 and (2) other mental health conditions, which included the remaining mental health conditions like mood disorders, eating disorders, obsessive compulsive disorders, and specific personality disorders (see Table S3). Following the Substance Abuse and Mental Health Services Administration categorization of mental health disorders, 27 we excluded certain conditions like dementias, cerebral degenerations, intellectual disability, and transient mental health disorders caused by substances.
2.3. Study outcomes
Primary outcomes for this study were inpatient hospital stays and ED visits where the primary diagnosis was related to a mental health condition in either acute general care hospitals or in psychiatric hospitals. For patients who presented to ED and were subsequently admitted, we classified them as an inpatient hospital stay only. We further examined inpatient hospital stays and ED visits related to serious mental health conditions versus other mental health conditions. A composite category of overall episodes related to either inpatient hospital stays or ED visits was also constructed. These groupings were designed to accommodate cell‐size restrictions from data providers. In the United States, we classified observation stays as inpatient hospital stays given that many patients stay in a hospital for up to 48 hours under this designation and the fact that the other countries do not have observation stays as a comparable designation.
2.4. Demographic variables
Sex (male/female) and age, categorized into four groups (<18, 18–40, 41–64, and 65+ years), were used. Sex was categorized as male or female based on biological sex information recorded in administrative records. Age groupings were selected to minimize data suppression in accordance with country‐specific regulations.
2.5. Analysis
Participating countries used patient‐level event data to generate aggregate annual age‐sex counts of acute care mental health events. These aggregate data were pooled to construct a multi‐country database for analysis. Age and sex direct standardization was employed to compare yearly mental health event rates per 100,000 people across all primary outcomes, using the yearly OECD average population as the reference. Age‐sex standardized rates of ED visits for mental health were only compared for four countries with available ED data—Canada, Finland, France, and the United States.
To test the significance of within‐ and between‐country variation in acute care mental health event rates, a series of negative binomial regression models were employed. We used negative binomial models with fixed effects for sex, age, and an interaction between country and an indicator for COVID‐19 (2017–2019 or 2020). Models were stratified by setting (hospitalizations only, ED visits only, combined across both settings) and mental health conditions (serious, other, and overall). Using predicted margins, we estimated the adjusted mental health acute care event rates for each country for the 2017–2019 (pre‐COVID) period, and for the 2020 (COVID‐19) year with associated 95% confidence intervals.
The overall study was reviewed by the Institutional Review Board at the Harvard T.H. Chan School of Public Health and was deemed exempted, and informed consent was waived given that it used aggregated, de‐identified patient data across countries. In addition, researchers from each country obtained approval for this study through each country‐specific data holder.
3. RESULTS
3.1. Sample characteristics
Table 1 shows the sample characteristics of people who were admitted to hospital or who presented to ED with a primary diagnosis of a mental health condition across eight countries during the 4‐year study period (2017–2020). There were 223,206 total inpatient hospitalizations in Canada, 315,206 in England, 120,461 in Finland, 2,763,940 in France, 72,357 in New Zealand, 157,452 in Spain, 251,528 in Switzerland, and 1,950,840 in the United States. The majority of inpatient hospitalizations were related to admissions for serious mental health conditions, ranging from 55% in England to 82% in the United States. Across all countries, the proportion of hospitalizations among females was slightly higher than among males. Four countries were able to provide ED visit data. Canada identified 479,280 ED events, 58,656 in Finland, 670,209 in France, and 2,770,958 in the United States. In contrast to inpatient events, the majority of ED visits were for other mental health conditions, ranging from 58% in France to 70% in Canada, except in the United States where the proportions were similar. Age and sex distributions for ED visits were similar to those of inpatient hospitalizations for each of the four countries.
TABLE 1.
Demographics of patients experiencing hospitalizations and emergency department (ED) visits related to mental health conditions, 2017–2020.
| Canada | England | Finland | France | New Zealand | Spain | Switzerland | United States | |
|---|---|---|---|---|---|---|---|---|
| Hospitalizations | ||||||||
| Total hospitalizations | 223,206 | 315,206 | 120,461 | 2,763,940 | 72,357 | 157,452 | 251,528 | 1,950,840 |
| Serious mental health | 171,700 (76.9) | 173,696 (55.1) | 95,828 (79.6) | 1,917,068 (69.4) | 53,934 (74.5) | 103,452 (65.7) | 181,905 (72.3) | 1,589,654 (81.5) |
| Other mental health | 51,506 (23.1) | 141,510 (44.9) | 24,633 (20.4) | 846,872 (30.6) | 18,423 (25.5) | 54,000 (34.3) | 69,623 (27.7) | 361,186 18.5) |
| Age (years) | ||||||||
| <18 | 34,294 (15.4) | 22,942 (7.3) | 13,306 (11.0) | 201,072 (7.3) | 4413 (6.1) | 8656 (5.5) | 22,813 (9.1) | 510,261 (26.2) |
| 18–40 | 105,524 (47.3) | 133,210 (42.3) | 50,399 (41.8) | 938,485 (34.0) | 32,181 (44.5) | 52,842 (33.6) | 79,980 (31.8) | 826,025 (42.3) |
| 41–64 | 64,273 (28.8) | 109,654 (34.8) | 34,152 (28.4) | 1,158,171 (41.9) | 24,627 (34.0) | 75,774 (48.1) | 110,090 (43.8) | 543,050 (27.8) |
| 65+ | 19,115 (8.6) | 49,400 (15.7) | 22,604 (18.8) | 466,212 (16.9) | 11,136 (15.4) | 20,178 (12.8) | 38,645 (15.4) | 71,504 (3.7) |
| Sex | ||||||||
| Female | 121,301 (54.3) | 179,369 (56.9) | 70,864 (58.8) | 1,523,074 (55.1) | 38,829 (53.7) | 83,940 (53.3) | 142,368 (56.6) | 1,053,586 (54.0) |
| Male | 101,905 (45.7) | 135,837 (43.1) | 49,597 (41.2) | 1,240,866 (44.9) | 33,528 (46.3) | 73,512 (46.7) | 109,160 (43.4) | 897,254 (46.0) |
| ED visits | ||||||||
| Total ED visits | 479,280 | 58,656 | 670,209 | 2,770,958 | ||||
| Serious mental health | 143,182 (29.9) | 23,835 (40.6) | 280,089 (41.8) | 1,450,896 (52.4) | ||||
| Other mental health | 336,098 (70.1) | 34,821 (59.4) | 390,120 (58.2) | 1,320,062 (47.6) | ||||
| Age (years) | ||||||||
| <18 | 66,416 (13.9) | 7371 (12.6) | 47,084 (7.0) | 443,396 (16.0) | ||||
| 18–40 | 254,106 (53.0) | 30,508 (52.0) | 292,513 (43.6) | 1,405,721 (50.7) | ||||
| 41–64 | 122,403 (25.5) | 14,097 (24.0) | 247,132 (36.9) | 823,385 (29.7) | ||||
| 65+ | 36,355 (7.6) | 6680 (11.4) | 83,480 (12.5) | 98,456 (3.6) | ||||
| Sex | ||||||||
| Female | 266,142 (55.5) | 34,856 (59.4) | 384,226 (57.3) | 1,572,919 (56.8) | ||||
| Male | 213,138 (44.5) | 23,800 (40.6) | 285,983 (42.7) | 1,198,039 (43.2) | ||||
Note: Table shows the number of mental health‐related hospitalizations and Emergency Department visits that were captured in each country from 2017 to 2020. The patient demographics associated with each care episode are shown. England, New Zealand, Spain, and Switzerland did not have data on ED visits available for analysis. Given data restrictions, the Swiss administrative data reflects slightly different age groups stratified into the following categories: <20, 20–39, 40–64, and 65+.
3.2. Temporal and cross‐country variation in mental health inpatient hospitalization
Figure 1 presents annual age‐sex standardized hospitalization rates per 100,000 people from 2017 to 2020. Overall, France had the highest rate of mental health hospitalizations (4‐year average rate of 1023 hospitalizations per 100,000 people), followed by Switzerland (709 per 100,000 people), and the United States (704 per 100,000 people) and with Spain observing the lowest rate (87 per 100,000 people). For all countries, hospitalization rates related to serious mental health conditions were higher than other mental condition rates, particularly in the United States at over four to one.
FIGURE 1.
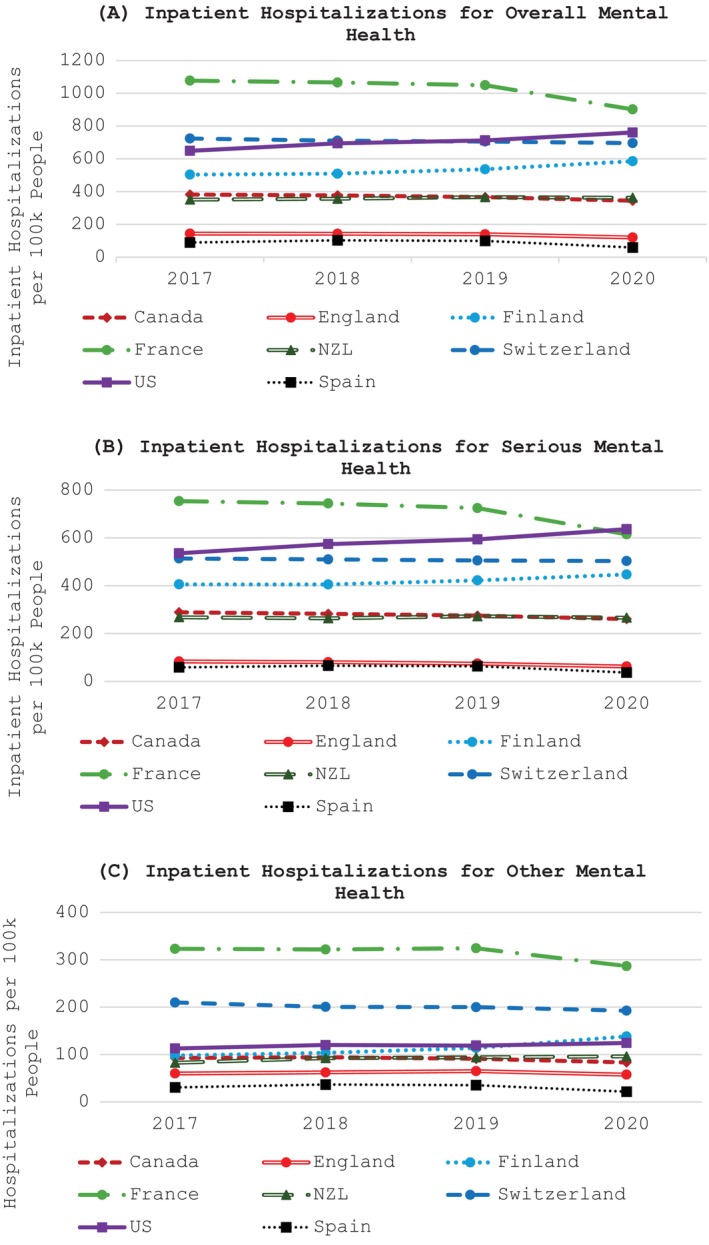
Age‐sex standardized hospitalization rates per 100,000 people related to mental health conditions across high‐income countries, 2017 to 2020. Figures show the age‐sex standardized rates of hospitalizations related to mental health conditions per 100 k people.
Temporal differences in hospitalization rates were observed across all countries, including moving into the COVID‐19 pandemic period. The United States and Finland each had increasing hospitalization rates over all years but experienced a more pronounced increase in 2020. England, France, and Canada all had relatively stable hospitalization rates from 2017 to 2019 but experienced substantial drops in 2020, ranging from −6.0% (Canada) to −14.1% (France). Spain observed a more marked decrease in 2020 (−40.7%). These patterns were generally similar for both serious mental health conditions and other mental health conditions.
3.3. Temporal and cross‐country variation in mental health ED rates
Figure 2 presents annual age‐sex standardized ED visit rates per 100,000 people from 2017 to 2020. Overall, the United States had the highest ED visit rates (4‐year average rate of 1002 visits per 100,000 people) followed by Canada (781 per 100,000 people), substantially higher than both Finland (263 per 100,000 people) and France (248 per 100,000 people). ED visit rates for serious mental health conditions were lower than for other mental health conditions for all countries except the United States, where rates were higher.
FIGURE 2.
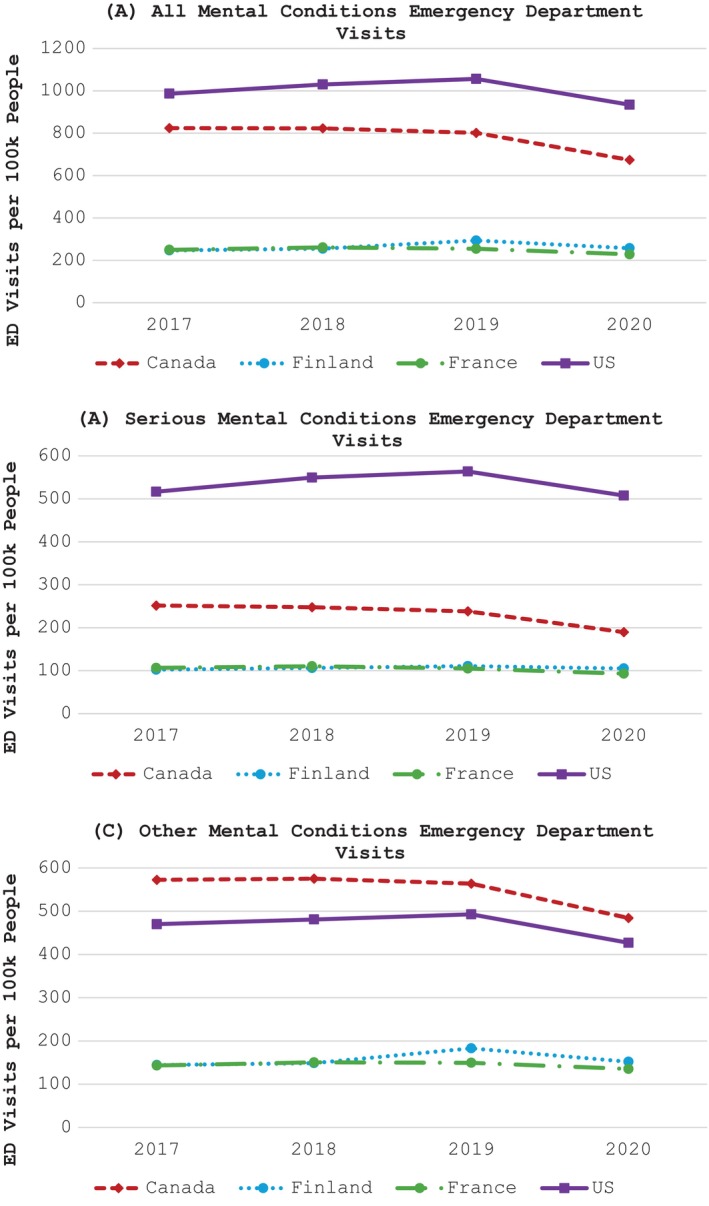
Age‐sex standardized emergency department (ED) visit rates per 100,000 people related to mental health conditions across high‐income countries, 2017 to 2020. Figures show the age‐sex standardized rates of ED visits for mental health conditions per 100 k people.
The United States and Finland each observed increasing rates of ED visits from 2017 to 2019 with substantial declines in 2020 of −11.5% and −12.4%, respectively. Rates of mental health ED visits for Canada and France were relatively flat from 2017 to 2019, but they also observed substantial declines in 2020 of −15.9% and −10.3%, respectively. For standardized acute care mental health event rates by age and sex, see Tables S4 and S5, respectively.
3.4. Cross‐country differences in overall and relative utilization of acute care for mental health conditions by care setting before and during the COVID‐19 pandemic
Table 2 presents age‐sex standardized rates of acute care mental health events (and associated 95% confidence intervals) overall and by care setting, before (2017–2019 yearly average) and during (2020) the COVID‐19 pandemic. Among countries with ED and inpatient event data, there was significant variation in combined acute care event rates. The United States had the highest rates in both the pre‐COVID and during‐COVID periods (1613 and 1602 per 100,000 people, respectively). The lowest rates were observed in Finland (776 and 817 per 100,000 people, respectively). Table 2 also confirms significant variation across countries in hospitalization and ED rates for all mental health categorizations.
TABLE 2.
Adjusted rates of hospitalizations and emergency department (ED) visits per 100,000 people for mental health conditions pre‐COVID (2017–2019 annual average) and during‐COVID (2020).
| Setting | Mental health conditions (Overall) | Serious mental condition | Other mental condition | |||
|---|---|---|---|---|---|---|
| 2017–2019 | 2020 | 2017–2019 | 2020 | 2017–2019 | 2020 | |
| Inpatient hospitalizations | ||||||
| Canada | 386.9 (335.2, 438.6) | 344.0 (265.7, 422.3) | 302.1 (255.2, 349.1) | 260.7 (192.1, 329.4) | 83.0 (70.5, 95.5) | 73.2 (54.3, 92.1) |
| England | 133 (115.5, 150.5) | 115.9 (89.6, 142.2) | 72.8 (61.7, 83.9) | 58.6 (43.2, 74) | 60.6 (51.5, 69.7) | 55.5 (41.2, 69.8) |
| Finland | 520.6 (451.7, 589.4) | 578.2 (446.8, 709.6) | 426.0 (360.5, 491.6) | 451.9 (333.0, 570.8) | 103.4 (87.8, 118.9) | 127.9 (94.9, 160.9) |
| France | 987.6 (857.6, 1117.6) | 837.9 (648.0, 1027.8) | 653.9 (554.5, 753.3) | 547.3 (404.0, 690.6) | 328 (278.7, 377.2) | 286.9 (213, 360.8) |
| NZL | 333.3 (289.4, 377.3) | 342.1 (264.3, 419.8) | 234.8 (199.0, 270.6) | 237.2 (174.9, 299.5) | 91.0 (77.2, 104.8) | 93.0 (68.9, 117.1) |
| Spain | 87.4 (75.9, 98.9) | 53.9 (41.7, 66.2) | 52.4 (44.4, 60.4) | 30.8 (22.7, 38.9) | 32.3 (27.4, 37.1) | 20.4 (15.1, 25.7) |
| Switzerland | 689.5 (598.4, 780.5) | 677.3 (523.5, 831.1) | 497.0 (420.9, 573.2) | 509.9 (375.8, 644.1) | 204.8 (174.1, 235.5) | 191.7 (142.2, 241.2) |
| US | 713.0 (617.5, 808.4) | 813.1 (627.2, 999.0) | 637.8 (537.9, 737.8) | 745.5 (547.6, 943.5) | 125.7 (106.6, 144.8) | 130.4 (96.5, 164.3) |
| p‐value across 8 countries | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| ED visits | ||||||
| Canada | 808.3 (725.9, 890.8) | 646.5 (535.7, 757.4) | 238.0 (204.7, 271.4) | 177.1 (135.4, 218.7) | 570.9 (524.1, 617.6) | 469.6 (404.9, 534.2) |
| Finland | 255.3 (229.4, 281.3) | 248.4 (205.6, 291.3) | 105.0 (90.3, 119.7) | 102.4 (78.2, 126.7) | 150.2 (137.8, 162.5) | 145.8 (125.4, 166.2) |
| France | 240.5 (216.1, 264.9) | 217.3 (180.0, 254.6) | 99.7 (85.7, 113.6) | 87.2 (66.7, 107.7) | 139.7 (128.3, 151.1) | 129.4 (111.6, 147.2) |
| US | 958.0 (861.4, 1054.6) | 863.7 (716, 1011.3) | 502.6 (433.1, 572.1) | 466.2 (356.9, 575.4) | 455.9 (419.0, 492.9) | 398.6 (343.9, 453.3) |
| p‐value across 4 countries | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
| Combined inpatient and ED | ||||||
| Canada | 1150.5 (1016.6, 1284.3) | 957.5 (768.6, 1146.4) | 515.4 (440.4, 590.3) | 420.9 (317.7, 524.0) | 629.4 (575.8, 683.0) | 527.8 (451.2, 604.5) |
| Finland | 776.0 (685.8, 866.2) | 817.1 (655.7, 978.5) | 516.1 (441.4, 590.8) | 532.1 (401.7, 662.5) | 254.2 (232.4, 276.0) | 275.4 (235.1, 315.7) |
| France | 1268.3 (1120.1, 1416.5) | 1082.8 (868.6, 1297.0) | 772.0 (660.2, 883.8) | 645.2 (486.9, 803.5) | 477.5 (436.2, 518.8) | 423.3 (361.5, 485.1) |
| US | 1612.6 (1425.9, 1799.4) | 1602.4 (1285.8, 1919.0) | 1066.8 (912.1, 1221.4) | 1108.1 (835.4, 1380.7) | 578.2 (528.8, 627.6) | 529.3 (452.3, 606.4) |
| p‐value across 4 countries | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 |
Canada observed the highest proportion of ED visits with approximately two thirds of events occurring in the ED setting. Likewise, the United States also treated the majority of mental health events in the ED setting. By contrast, Finland and France had comparably low proportions of mental health events occurring in the ED setting.
Table 2 also demonstrates directional shifts in acute care mental health rates overall and by care setting in relation to the COVID‐19 pandemic. Combined acute care mental health rates were relatively stable for the US but increased for Finland from a 2017 to 2019 average of 776 per 100,000 people to 817 per 100,000 people in 2020 and decreased for Canada (1150 per 100,000 people to 958 per 100,000 people) and France (1268 per 100,000 people to 1083 per 100,000 people). However, these changes were not statistically significant. Similarly, directional changes in inpatient and ED rates were observed for several countries. For example, in the inpatient setting the United States observed an increase from a 2017 to 2019 average of 713 per 100,000 people to 813 per 100,000 people in 2020. Finland observed a similar increase from 521 per 100,000 people to 578 per 100,000 people. By contrast, Canada and France both observed declining rates of 387 per 100,000 people to 344 per 100,000 people and 988 per 100,000 to 838 per 100,000, respectively. Spain observed a statistically significant decrease from 87 per 10,000 people to 54 per 100,000 people. In the ED setting, the rate of mental health visits for Canada, France, and the United States decreased during the COVID‐19 pandemic. The largest decline was in Canada from a 2017 to 2019 average of 808 per 100,000 people to 647 per 100,000 people in 2020.
4. DISCUSSION
In this retrospective international comparison study across eight high‐income countries, we found significant variation in acute care rates for mental health conditions across countries including in both the inpatient and ED settings. The United States observed the highest acute care rates per capita, significantly higher than all other countries including Finland with the lowest rate. The highest hospitalization rates were observed in France and the lowest in Spain. In the ED setting the United States had the highest rates and Finland the lowest. Furthermore, distinct temporal differences in acute care mental health rates were evident, including marked variations coinciding with the onset of the COVID‐19 pandemic.
These results have important implications for clinical leaders and policymakers interested in managing and improving care for people with mental health conditions. Prior work has shown that the United States has a much lower capacity related to its mental health care workforce compared with other high‐income countries—including lower per capita number of social workers, psychologists, and psychiatric nurses—to meet the needs of their patient population. 9 , 28 There is also substantial concern that patients in the United States are more likely to experience significant cost‐related access barriers to mental health care treatment, including high out‐of‐pocket costs and cost‐sharing for medications, primary care, and specialty services. 9 , 29 These health system shortcomings may explain why the United States had the highest rate of acute care mental health treatment in the present study. In France, the mental health care system is predominantly hospital‐centered, leading to high hospitalization rates. 30 This is partly because hospitals serve as the main entry point for mental health care, given the lack of alternative ambulatory structures like walk‐in centers and social support services. France has approximately 85 psychiatric beds per 100,000 people, significantly higher than the roughly 25 beds per 100,000 in the United States, perhaps explaining its high inpatient hospitalization rate. 31 However, France also experiences access issues related to community‐based specialist mental health services, 30 and while general practitioners are more accessible, they are not adequately trained to detect and manage mild to moderate mental health conditions. 32 , 33 By contrast, Finland's comparatively low rates of acute mental health care can likely be attributed to major reforms over the last few decades that have shifted the focus from institutional to outpatient care. Legislation, such as the 1991 Act on Mental Health and the Health Care Act of 2010, emphasized outpatient care, integration with social services, and low‐threshold access. 34 Additionally, the expansion of outpatient services and the critical role of psychiatric nurses in early detection of depressive disorders have significantly reduced the need for in‐hospital care. 35
The high hospitalization rates in France and the United States relative to other countries may also be partially explained by the fact that patients in these countries are much more likely to report having high rates of unmet need than countries such as Canada and England. 9 , 29 For example, the Commonwealth Fund International Health Policy survey found that people in the United States and France are more likely to report being unable to afford mental health care or receive appropriate and timely treatment when experiencing emotional distress than other countries. 29 Additionally, in an international survey of primary care physician (PCP) practices in 2019, only 46% of PCP practices in the US and 31% in France reported being well‐prepared to care for people with mental health conditions compared with a majority of PCP practices in other countries, including 66% in New Zealand, 63% in Switzerland, and 56% in England. 9 Taken together, the higher burden of unmet need and limited PCP capacity may explain why people with mental health conditions in the United States and France are more likely to require acute inpatient care for management of their underlying illness. High rates of inpatient hospitalizations in Switzerland may be due to heterogeneity in mental health care provision across cantons, high psychiatric bed capacity, and a reimbursement system that incentivizes inpatient over outpatient care. 36 , 37 , 38
Despite having a similar burden of mental health conditions compared with other OECD countries, 14 Spain and England reported the lowest utilization of inpatient medical services for mental health conditions. This may be driven by multiple factors. For example, these countries have limited inpatient psychiatric capacity. An OECD report noted that both countries had significantly fewer beds available per capita than the OECD average. 31 The limited inpatient capacity for psychiatric care may strain patient access and bottleneck inpatient hospitalizations. Indeed, in England, declining mental health bed numbers have coincided with higher thresholds for admission. 39 That said, the emphasis of England's NHS is on community‐based mental health care through extensive use of Crisis Resolution and Home Treatment Teams, which provide intensive support to individuals in their homes to prevent the need for hospitalization. 17 In the case of Spain, since the 2007 National Strategy for Mental Health, the Spanish National Health Service has promoted a more holistic community‐based approach to mental care (inclusion of mental health workers in community centers, rapid intervention teams, assertive community treatments), and social measures meant to keep the patient autonomy within the community as well as to help families in their role of informal carers. 40
Among the subset of four countries with both ED and hospitalization data, we found that proportionally the United States and Canada cared for more people in the ED compared with France and Finland, which both hospitalized the majority of people who presented with a mental health condition. Plausible explanation for these results likely varies depending on the country. In Canada, for example, it is possible that the high rates of ED use with relatively lower rates of hospitalizations reflect a substitution effect. Canada has comparatively low psychiatric bed capacity, and therefore, it is possible that these are reserved for the most severely ill presentations, with a preference for acute care management in the ED setting without hospital admission. 31 , 41 In the US, prior work suggests that health care market forces and financial reimbursement by insurers have led to a decrease of inpatient psychiatric beds over time, which has resulted in more psychiatric care occurring in EDs of general acute care hospitals that have limited inpatient capacity to address mentally ill patients while favoring caring for medical and surgical conditions that may reimburse better. 42
Interestingly, our study also found notable temporal differences between and within countries in acute care mental health treatments at the onset of the COVID‐19 pandemic. Canada and France observed declines in both inpatient and ED mental health rates in 2020. Several countries who only reported inpatient data—including Spain, Switzerland, and England—also observed declining mental health acute care rates. These findings are consistent with international evidence showing reduced rates of acute care for mental health problems, particularly during the early stages of the COVID‐19 pandemic. 43 , 44 , 45 , 46 This likely reflected significantly reduced health care capacity in hospital settings and possible avoidance of hospitals by patients due to an underlying fear of contracting COVID‐19 or the moral conscious of avoiding seeking hospital care so as not to consume much‐needed health resourcing responding to COVID‐19. 46 , 47 , 48 It is also consistent with a reorganization of mental health services for more community‐based care including telehealth services for lower acuity mental health concerns. 43 , 44 In the United States, there was a marked shift between treatment settings in 2020, with increased inpatient hospitalizations countered by considerably reduced ED visits. This may reflect substantially constrained ED capacity due to the influx of COVID‐19 cases as well as limited outpatient options and a subsequent substitution effect to inpatient admissions. 49 Alternatively, it may suggest that individuals delayed seeking treatment for mental health concerns until they had a crisis resulting in higher severity presentations and a greater requirement for inpatient‐based care. 50
4.1. Study limitations
This study has important limitations. Most notably, the use of administrative data for research, a purpose for which they were not originally collected, presents challenges related to data accuracy, completeness, and potential biases, which can impact the validity and generalizability of study findings. 51 Moreover, this issue may be exacerbated in cross‐country analyses as recording practices, quality issues, completeness, and representativeness of samples may vary across countries. While we have done our best to ensure comparability across countries, including limiting the patient cohort identification criteria to primary diagnoses, key differences may influence results. For example, data for England do not have complete coverage of hospitalizations to some specialized mental health and psychiatric hospitals. The level of undercount is quite small, however, and is unlikely to materially impact on the key findings. Likewise, data for Spain include psychiatric episodes admitted to acute care hospitals but not in long‐term psychiatric hospitals. For France, coding practices for ED presentations can be heterogenous across psychiatric hospitals. 52 The extent to which limitations related to data quality might affect study findings is likely to be small. Finally, across countries, there are structural differences in how countries capture and incentivize coding of secondary comorbidities. Therefore, we did not include secondary diagnoses for risk adjustment given underlying differences likely do not capture variations in risk but rather coding practices across countries.
Other key limitations of the research include that the underlying mental health needs of the study populations are unknown, and the data cannot distinguish between prevalent and incident cases of mental health service use. Consequently, the study's ability to accurately identify the level of unmet needs across countries is limited. Second, we were not able to adjust for underlying comorbidities that may contribute to the need for acute care, as available data do not capture comorbidities with enough accuracy to sufficiently make such adjustments. Third, while we used large, nationally representative datasets to capture inpatient hospitalizations across eight countries, only four participating countries had access to ED data that included diagnostic coding of visits to identify those related to mental health conditions. Fourth, time coverage of data varied across countries limiting our ability to look at time periods before 2017 or after 2020. This restricted our ability to examine the longer‐term impacts relating to the COVID‐19 pandemic. Fifth, this study was limited to examinations of age and sex differences, and it did not evaluate differences by other potentially important demographics such as prevalent racial, ethnic, and cultural groups. For example, there is prior evidence of significant inequities in access to mental health care among Māori and Pacific populations compared with non‐Māori/non‐Pacific in New Zealand, 53 , 54 Black and Hispanic populations in the United States relative to non‐Hispanic White populations, 55 , 56 , 57 and minoritized ethnic groups, especially Black groups, in England. 58 Moreover, variation in rates of acute mental health care may also be significantly influenced by cultural stigma and the extent to which this differs across countries. The cultural stigma of accessing mental health services due to fear of discrimination and social judgment is well documented. 59 , 60 Heterogeneity in the cultural make‐up of participating countries and the extent to which stigmatizing beliefs prevail may help explain observed differences. 54 , 61 Likewise, the study did not examine social determinants of health such as income, education, and occupation. Extant literature has shown that disadvantaged populations tend to disproportionately experience mental health concerns. 62 , 63 For example, a recent systematic review highlighted the significant relationship between lower income and higher prevalence of mental health disorders in studies across many of our participant countries, including the US, England, Germany, Canada, France, and New Zealand. 64 Finally, this study was limited to examining variation in utilization patterns for acute care events related to mental health conditions. Future work should closely examine the implications of these patterns on other important measures, including the impact on quality of care, health outcomes, and patient satisfaction.
5. CONCLUSION
In this international comparison across high‐income countries, we found considerable variation in both the absolute and relative rates of ED visits and hospitalizations related to mental health conditions, including the differential effect of COVID‐19. Notably, the United States experienced the highest overall rate of hospitalizations and ED visits related to mental health conditions compared with other countries. Further research is needed to elucidate the extent to which factors such as workforce capacity, higher cost‐related access barriers, COVID‐19 preparedness, and higher burdens of unmet mental health need among patient populations may contribute to these variations.
FUNDING INFORMATION
This work was partially supported by a grant from the Health Foundation (UK). The University of Otago provided funding support for the New Zealand analysis. Ontario analyses were undertaken by the Health System Performance Network, which receives funding from the Ontario Ministry of Health and the Ontario SPOR Support Unit. Dr. Figueroa was partially supported by the Robert Wood Johnson Foundation Harold Amos Medical Faculty Development Award. Dr. Bowden was partially funded by Health Research South.
Supporting information
Table S1. Health system characteristics by country.
Table S2. Country datasets.
Table S3. ICD‐10 codes for mental health conditions.
Table S4. Standardized rates of mental health hospitalization, ED, and combined hospitalization + ED per 100,000 people by age.
Table S5. Standardized rates of mental health hospitalizations, ED visits, and combined hospitalizations + ED visits per 100,000 people by sex.
ACKNOWLEDGMENT
The authors have nothing to report.
Bowden N, Hedquist A, Dai D, et al. International comparison of hospitalizations and emergency department visits related to mental health conditions across high‐income countries before and during the COVID‐19 pandemic. Health Serv Res. 2024;59(6):e14386. doi: 10.1111/1475-6773.14386
REFERENCES
- 1. World Health Organization . World Mental Health Day 2022 ‐ Make mental health & well‐being for all a global priority. Accessed July 11, 2024. https://www.who.int/news-room/events/detail/2022/10/10/default-calendar/world-mental-health-day-2022---make-mental-health-and-well-being-for-all-a-global-priority
- 2. Institute of Health Metrics and Evaluation . Global Health Data Exchange (GHDx). Accessed October 31, 2022. https://vizhub.healthdata.org/gbd-results/
- 3. Gibb S, Brewer N, Bowden N. Social impacts and costs of schizophrenia: a national cohort study using New Zealand linked administrative data. N Z Med J. 2021;134(1537):66‐83. [PubMed] [Google Scholar]
- 4. Butterworth P, Leach LS, Pirkis J, Kelaher M. Poor mental health influences risk and duration of unemployment: a prospective study. Soc Psychiatry Psychiatr Epidemiol. 2012;47(6):1013‐1021. [DOI] [PubMed] [Google Scholar]
- 5. San Too L, Spittal MJ, Bugeja L, Reifels L, Butterworth P, Pirkis J. The association between mental disorders and suicide: a systematic review and meta‐analysis of record linkage studies. J Affect Disord. 2019;259:302‐313. [DOI] [PubMed] [Google Scholar]
- 6. Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta‐regression analysis. PLoS Med. 2008;5(12):e225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Arias D, Saxena S, Verguet S. Quantifying the global burden of mental disorders and their economic value. EClinicalMedicine. 2022;54:101675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. IHME . Mental Health. Accessed July 6, 2024. https://www.healthdata.org/research-analysis/health-risks-issues/mental-health
- 9. Tikkanen R, Fields K, Williams R, Abrams M. Mental Health Conditions and Substance Use: Comparing US Needs and Treatment Capacity with Those in Other High‐Income Countries. Commonwealth Fund; 2020. doi: 10.26099/09ht-rj07 [DOI] [Google Scholar]
- 10. World Health Organization . Mental Health Disorders. Accessed 31 October, 2022. https://www.who.int/news-room/fact-sheets/detail/mental-disorders
- 11. World Health Organization . Mental Health Atlas. World Health Organization; 2020. Accessed July 11, 2024. https://www.who.int/publications/i/item/9789240036703 [Google Scholar]
- 12. World Health Organization . Mental health atlas 2020. 2021.
- 13. Moitra M, Santomauro D, Collins PY, et al. The global gap in treatment coverage for major depressive disorder in 84 countries from 2000–2019: a systematic review and Bayesian meta‐regression analysis. PLoS Med. 2022;19(2):e1003901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. OECD . Health at a Glance 2023. OECD Publishing; 2023. Accessed July 11, 2023. https://www.oecd-ilibrary.org/content/publication/health_glance-2017-en [Google Scholar]
- 15. COVID‐19 Mental Disorders Collaborators . Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID‐19 pandemic. Lancet. 2021;398(10312):1700‐1712. doi: 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lin E, Or Z, Coldefy M, et al. Medical practice variations in mental health and addictions care. In: Johnson A, Stukel T, eds. Medical Practice Variations. Springer; 2016:1‐41. [Google Scholar]
- 17. Anderson M, Pitchforth E, Edwards N, Alderwick H, McGuire A, Mossialos E. United Kingdom: health system review. Accessed July 11, 2024. https://eurohealthobservatory.who.int/publications/i/united-kingdom-health-system-review-2022 [PubMed]
- 18. Cunningham R, Kvalsvig A, Peterson D, et al. Stocktake report for the mental health and addiction inquiry. Accessed July 11, 2024. https://mentalhealth.inquiry.govt.nz/assets/Summary‐reports/Otago‐stocktake.pdf
- 19. Rice T, Rosenau P, Unruh LY, et al. United States of America: health system review. Accessed July 11, 2024. https://eurohealthobservatory.who.int/publications/i/united-states-health-system-review-2020 [PubMed]
- 20. OECD . Mental health. Accessed July 11, 2024. https://www.oecd-ilibrary.org/content/component/c7a518c0-en
- 21. Hagquist C, Due P, Torsheim T, Välimaa R. Cross‐country comparisons of trends in adolescent psychosomatic symptoms–a Rasch analysis of HBSC data from four Nordic countries. Health Qual Life Outcomes. 2019;17:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Figueroa J, Horneffer K, Riley K, Abiona O, Arvin M, Atsma F. A methodology for identifying high‐need, high‐cost patient personas for international comparisons: the international collaborative on costs outcomes, and needs in care (ICCONIC) project. Health Serv Res. 2021;56:1302‐1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Figueroa JF, Papanicolas I, Riley K, et al. International comparison of health spending and utilization among people with complex multimorbidity. Health Serv Res. 2021;56:1317‐1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Papanicolas I, Figueroa JF, Schoenfeld AJ, et al. Differences in health care spending and utilization among older frail adults in high‐income countries: ICCONIC hip fracture persona. Health Serv Res. 2021;56:1335‐1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Figueroa JF, Phelan J, Orav EJ, Patel V, Jha AK. Association of Mental Health Disorders with health care spending in the Medicare population. JAMA Netw Open. 2020;3(3):e201210. doi: 10.1001/jamanetworkopen.2020.1210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Figueroa J, Phelan J, Newton H, Orav E, Meara E. ACO participation associated with decreased spending for medicare beneficiaries with serious mental illness. Health Aff (Millwood). 2022;41(8):1182‐1190. doi: 10.1377/hlthaff.2022.00096 [DOI] [PubMed] [Google Scholar]
- 27. SAMHSA . Behavioral Health Spending and Use Accounts, 1986‐2014. 2016. Accessed July 11, 2024. https://store.samhsa.gov/product/behavioral‐health‐spending‐and‐use‐accounts‐1986‐2014/sma16‐4975
- 28. World Health Organization . The Global Health Observatory. Accessed July 11, 2024. https://www.who.int/data/gho
- 29. Commonwealth Fund . International Health Policy Survey. Accessed July 11, 2024. https://www.commonwealthfund.org/publications/surveys/2016/nov/2016‐commonwealth‐fund‐international‐health‐policy‐survey‐adults
- 30. Or Z, Gandré C, Seppänen A‐V, et al. France: Health System Review. World health organization. Regional Office for Europe; 2023. Accessed July 11, 2024. https://eurohealthobservatory.who.int/publications/i/france-health-system-review-2023 [Google Scholar]
- 31. OECD . A New Benchmark for Mental Health Systems: Tackling the Social and Economic Costs of Mental Ill‐Health. OECD Publishing; 2021. doi: 10.1787/4ed890f6-en [DOI] [Google Scholar]
- 32. Dumesnil H, Cortaredona S, Cavillon M, et al. Prise en charge de la dépression en médecine générale de ville: Résultats issus d'une enquête menée auprès d'un panel national de médecins généralistes français. Inf Psychiatr. 2014;5:341‐352. [Google Scholar]
- 33. Norton J, David M, Gandubert C, et al. Ability of French general practitioners to detect common mental disorders identified using the patient health questionnaire: has this changed with the introduction of gatekeeping and registration with a chosen doctor? L'encephale. 2016;44(1):22‐31. [DOI] [PubMed] [Google Scholar]
- 34. Keskimaki I, Tynkkynen L‐K, Reissell E, et al. Finland: Health System Review. Accessed July 11, 2024. https://eurohealthobservatory.who.int/publications/i/finland-health-system-review-2019 [PubMed]
- 35. Pirkola S, Sund R, Sailas E, Wahlbeck K. Community mental‐health services and suicide rate in Finland: a nationwide small‐area analysis. Lancet. 2009;373(9658):147‐153. [DOI] [PubMed] [Google Scholar]
- 36. Stulz N, Jörg R, Reim‐Gautier C, et al. Mental health service areas in Switzerland. Int J Methods Psychiatr Res. 2023;32(1):e1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Stocker D, Stettler P, Jäggi J, et al. Versorgungssituation Psychisch Erkrankter Personen in der Schweiz. Büro für Arbeits‐Und Sozialpolitische Studien BASS; 2016. [Google Scholar]
- 38. De Pietro C, Camenzind P, Sturny I, et al. Switzerland: health system review. Accessed July 11, 2024. https://eurohealthobservatory.who.int/publications/i/switzerland-health-system-review-2015 [PubMed]
- 39. The Strategy Unit . Exploring mental health inpatient capacity across Sustainability and Transformation Partnerships in England. Accessed July 11, 2024. https://www.strategyunitwm.nhs.uk/publications/exploring-mental-health-inpatient-capacity
- 40. Ministry of Health SSaE . Mental Health Strategy of the Spanish National Health System: 2009‐2013. 2012. Accessed Jul 11, 2024. https://www.sanidad.gob.es/areas/calidadAsistencial/estrategias/saludMental/docs/MentalHealthStrategySpanishNationalHS.pdf
- 41. Lebenbaum M, Chiu M, Vigod S, Kurdyak P. Prevalence and predictors of involuntary psychiatric hospital admissions in Ontario, Canada: a population‐based linked administrative database study. BJPsych Open. 2018;4(2):31‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Nordstrom K, Berlin J, Siris Nash S, Shah S, Schmelzer N, Worley L. Boarding of mentally ill patients in emergency departments: American Psychiatric Association resource document. Focus (Am Psychiatr Publ). 2023;21(1): 74‐79. doi: 10.1176/appi.focus.23022001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pignon B, Gourevitch R, Tebeka S, et al. Dramatic reduction of psychiatric emergency consultations during lockdown linked to COVID‐19 in Paris and suburbs. J Neuropsychiatry Clin Neurosci. 2020;74(10):557‐559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Flevaud L, Pham A, Gourevitch R. A sharp drop in psychiatric emergency admissions during lockdown. Ann Med Psychol. 2020;179(2):123‐127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kim HK, Carvalho AF, Gratzer D, et al. The impact of COVID‐19 on psychiatric emergency and inpatient services in the first month of the pandemic in a large urban mental health hospital in Ontario, Canada. Front Psychiatry. 2021;12:563906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Gonçalves‐Pinho M, Mota P, Ribeiro J, Macedo S, Freitas A. The impact of COVID‐19 pandemic on psychiatric emergency department visits–a descriptive study. Psychiatry Q. 2021;92(2):621‐631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sandhu P, Shah AB, Ahmad FB, et al. Emergency department and intensive care unit overcrowding and ventilator shortages in US hospitals during the COVID‐19 pandemic, 2020‐2021. Public Health Rep. 2022;137(4):796‐802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Gutovitz S, Pangia J, Finer A, Rymer K, Johnson D. Emergency department utilization and patient outcomes during the COVID‐19 pandemic in America. J Emerg Med. 2021;60(6):798‐806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Holland KM, Jones C, Vivolo‐Kantor AM, et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID‐19 pandemic. JAMA Psychiatry. 2021;78(4):372‐379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Duncan A, Herrera C‐N, Okobi M, Nandi S, Oblath R. Locked down or locked out? Trends in psychiatric emergency services utilization during the COVID‐19 pandemic. J Health Serv Res Policy. 2023;28(2):80‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Iezzoni LI. Assessing quality using administrative data. Ann Intern Med. 1997;127(8 Pt 2):666‐674. [DOI] [PubMed] [Google Scholar]
- 52. Richaud‐Eyraud E, Ellini A, Clément M‐C, Menu A, Dubois J. Qualité du codage des diagnostics et motifs de prise en charge (principal et associés) dans le recueil d'informations médicalisé en psychiatrie (RIM‐P) en 2015 et 2016, France. Rev Epidemiol Sante Publique. 2019;67(5):337‐344. [DOI] [PubMed] [Google Scholar]
- 53. Theodore R, Bowden N, Kokaua J, et al. Mental health inequities for Māori youth: a population‐level study of mental health service data. N Z Med J. 2022;135(1567):79‐90. [PubMed] [Google Scholar]
- 54. Ruhe T, Bowden N, Theodore R, et al. Identification of mental health and substance use‐related conditions among Pasifika young people in Aotearoa New Zealand‐a national cross‐sectional study using the integrated data infrastructure (IDI). Pac Health Dialog. 2023;21(10):663‐672. [Google Scholar]
- 55. Alegría M, Chatterji P, Wells K, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv. 2008;59(11):1264‐1272. doi: 10.1176/ps.2008.59.11.1264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. McGuire TG, Miranda J. New evidence regarding racial and ethnic disparities in mental health: policy implications. Health Aff (Millwood). 2008;27(2):393‐403. doi: 10.1377/hlthaff.27.2.393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Enslow MR, Galfalvy HC, Sajid S, Pember RS, Mann JJ, Grunebaum MF. Racial and ethnic disparities in time to first antidepressant medication or psychotherapy. Psychiatry Res. 2023;326:115324. doi: 10.1016/j.psychres.2023.115324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Halvorsrud K, Nazroo J, Otis M, Brown Hajdukova E, Bhui K. Ethnic inequalities and pathways to care in psychosis in England: a systematic review and meta‐analysis. BMC Med. 2018;16(1):1‐17. doi: 10.1186/s12916-018-1201-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Ojeda VD, Bergstresser SM. Gender, race‐ethnicity, and psychosocial barriers to mental health care: an examination of perceptions and attitudes among adults reporting unmet need. J Health Soc Behav. 2008;49(3):317‐334. [DOI] [PubMed] [Google Scholar]
- 60. Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychol Sci Public Interest. 2014;15(2):37‐70. [DOI] [PubMed] [Google Scholar]
- 61. Bracke P, Delaruelle K, Verhaeghe M. Dominant cultural and personal stigma beliefs and the utilization of mental health services: a cross‐national comparison. Front Sociol. 2019;4:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Allen J, Balfour R, Bell R, Marmot M. Social determinants of mental health. Int Rev Psychiatry. 2014;26(4):392‐407. [DOI] [PubMed] [Google Scholar]
- 63. Knapp M, Wong G. Economics and mental health: the current scenario. World Psychiatry. 2020;19(1):3‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Thomson RM, Igelström E, Purba AK, et al. How do income changes impact on mental health and wellbeing for working‐age adults? A systematic review and meta‐analysis. Lancet Public Health. 2022;7(6):e515‐e528. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Health system characteristics by country.
Table S2. Country datasets.
Table S3. ICD‐10 codes for mental health conditions.
Table S4. Standardized rates of mental health hospitalization, ED, and combined hospitalization + ED per 100,000 people by age.
Table S5. Standardized rates of mental health hospitalizations, ED visits, and combined hospitalizations + ED visits per 100,000 people by sex.


