Abstract
Proton pump inhibitors (PPI) are widely used medications for gastrointestinal disorders. Recent research suggests a potential association between long-term PPI use and increased cardiovascular (CV) risk, creating a complex clinical dilemma. This review critically evaluates the current evidence for this association, considering the limitations of observational studies and the lack of definitive confirmation from randomized controlled trials.
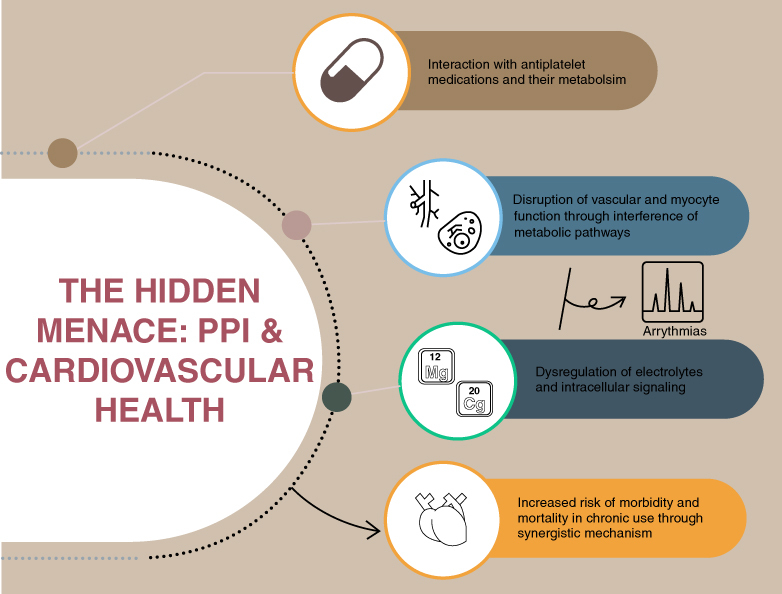
This review delves into the reported association between PPIs and adverse CV events, examining proposed mechanisms such as drug interactions, electrolyte imbalances induced by PPIs and their potential impact on cardiac and vascular function. Evidence suggests these mechanisms converge, with varying influence depending on patient populations.
Clinicians require a risk-benefit analysis for each patient considering their CV risk profile. Alternative gastrointestinal therapies should be explored for high-bleeding risk patients. Medications with lower cytochrome-P450 interaction potential may be preferable among essential PPI users. Elucidating the specific mechanisms by which PPIs might influence CV health, assessing long-term vascular effects and investigating interactions with newer anticoagulant medications are crucial for future research.
Keywords: : CAD, cardiovascular risk, CVD, electrolytes, magnesium, PPI, Torsades de pointes, ventricular arrhythmia
Plain Language Summary
Proton pump inhibitors (PPIs) are commonly used medications for gastrointestinal problems. However, recent studies have shown that long-term use of PPIs might increase the risk of heart problems. While this link hasn't been definitively proven, it's important to be aware of it.
Researchers think that several factors could contribute to this increased risk. PPIs might interact with other medications, cause electrolyte imbalances, or affect the way the heart and blood vessels work through multiple mechanisms.
Doctors need to carefully weigh the benefits of PPIs against the potential risks for each patient. For people at high risk of heart problems, alternative treatments might be better. If someone requires a PPI due to increased risk of gastrointestinal bleeding, providers need to take into account concurrent medications and carefully select those with the least risk of interactions.
Future research should focus on understanding how PPIs might impact the heart and blood vessels in the long term, especially considering the increasing use of newer blood-thinning medications.
Graphical Abstract
Plain language summary
Article highlights.
The widespread use of proton pump inhibitors (PPI) has risen dramatically in recent years, yet their potential cardiovascular risks remain uncertain.
PPIs can influence the metabolism of clopidogrel, an antiplatelet agent, by affecting hepatic cytochrome P450 (CYP) enzymes, particularly CYP2C19.
PPIs may elevate cardiovascular risk through mechanisms beyond drug interactions.
Chronic PPI use has been associated with electrolyte imbalances, notably hypocalcemia and hypomagnesemia, which are crucial for maintaining cellular homeostasis.
PPI-induced intracellular disturbances can precipitate life-threatening arrhythmias, including torsade de pointes.
PPIs, through both direct and indirect mechanisms, can disrupt cellular electrolyte balance, thereby impairing myocyte function and potentially contributing to the development of heart failure.
PPIs may exert a direct influence on vascular regulation, potentially accelerating vascular senescence through intricate cellular mechanisms.
Future research should investigate these mechanisms and potential interactions with novel cardiovascular medications.
1. Introduction
Proton pump inhibitors (PPIs) have established themselves as a cornerstone therapeutic modality for various gastrointestinal (GI) ailments, including peptic ulcer disease, gastroesophageal reflux disease and Helicobacter pylori eradication [1,2]. Their efficacy in suppressing gastric acid secretion has translated into widespread clinical use, with millions of prescriptions dispensed annually [2] (Table 1).
Table 1.
Common PPI and their interaction with CYP isoenzymes.
| PPI | CYP enzyme (strength of inhibition) | Common dosing |
|---|---|---|
| Pantoprazole | CYP2C19 (weak inhibitor) | 40 mg once daily |
| Omeprazole | CYP2C19 (moderate inhibitor) | 20 mg once daily |
| Esomeprazole | CYP2C19 (moderate inhibitor) | 20 mg–40 mg once daily |
| Rabeprazole | CYP2C19 (weak inhibitor) | 20 mg once daily |
| Lansoprazole | CYP2C19 (moderate inhibitor), CYP3A4 (weak inhibitor) | 15 mg–30 mg once daily |
While PPIs demonstrate a generally favorable tolerability profile, research suggests a potential association between prolonged PPI use and an increased risk of adverse cardiovascular (CV) outcomes [3–5]. However, discrepancies between studies underscore the multifaceted nature of this issue and necessitate further exploration to elucidate the potential link between PPIs and CV health [6].
Prompted by growing concerns, this review comprehensively assesses the current understanding of the potential link between PPIs and cardiovascular health. We delve into the effects of PPIs on CV outcomes, scrutinizing the proposed mechanisms by which they may exert influence.
2. Discussion
PPIs are among the most commonly prescribed medications, they are approved for the short-term management of a myriad of GI conditions such as reflux disease, esophagitis, peptic ulcer disease and dyspepsia [2]. Nonetheless, these medications are frequently used for extended periods for vague indications [7]. There is limited evidence of the long-term risk associated with their use and the evidence suggests that up to 86% of patients taking PPI are overprescribed [8]. In recent years, observational data have proposed an association between the chronic use of PPI and the development of micronutrient deficiencies, dementia, kidney disease and cardiovascular diseases [3–5].
While the American Heart Association advises clinicians to use anti-secretory medications to prevent gastrointestinal side effects like ulceration and bleeding, concerns have emerged in past decades regarding their potential association with poorer CV health outcomes [4,9]. However, the variability of the current evidence begs further exploration to elucidate the potential link between PPIs and CV health [10]. This review will explore proposed mechanisms for these potential adverse effects including disruption of the metabolism of certain commonly prescribed cardiovascular medications like antiplatelet drugs, dysregulation of mineral and micronutrient metabolism and interference with vascular and cardiac function [11].
2.1. Cardiovascular outcomes
The increasing use of PPIs to mitigate GI bleeding risk in CV patients on antithrombotic therapy has raised concerns about potential adverse cardiovascular effects [12,13]. Research over the past decade has sought to clarify this association [14]. While PPI-antiplatelet interactions remain a concern, leading medical societies recommend PPI use alongside antiplatelet therapy in high-risk patients, emphasizing that the benefits of antiplatelet therapy for cardiovascular disease outweigh the potential risks associated with judicious PPI use [15,16].
In 2009, a population-based case-control study by Juurlink et al. followed over 13,000 patients prescribed clopidogrel after a myocardial infarction (MI) [17]. They found that current PPI use was associated with an increased risk of reinfarction hospitalization (aOR1.27, 95% CI: 1.03–1.57). This association was not observed on patients with prior PPI exposure or in sensitivity analyses. Notably, pantoprazole was not associated with increased readmission for MI, sparking the suggestion of a metabolism mediated effect of other PPIs. (aOR 1.02; 95% CI: 0.70–1.47).
Kreutz et al. contributed additional data bolstering the potential link between PPI use and adverse CV events [18]. Their retrospective analysis, utilizing claims data, revealed a statistically significant increase in the one-year incidence of CV events within the PPI user group compared with the non-user group (32.5% vs. 21.2%, OR 1.79, 95% CI: 1.62–1.97). Notably, this association was even more pronounced in patients with a documented history of CV events (39.8% with PPI vs. 26.2% without, OR 1.86, 95% CI: 1.63–2.12). In contrast to Juurlink, the analysis did not detect a significant difference in risk across the various PPI medications employed [17].
As with other observational studies, the research by Kreutz et al. is subject to inherent limitations associated with claims data analysis such as coding errors and the presence of confounding variables [18]. The observed similarity in risk across different PPIs, including those with a weaker CYP inhibitory effect, weakens the argument for CYP-mediated metabolism as a primary mechanism. Furthermore, PPI use in this context might simply be a surrogate marker for a patient population with a higher baseline risk due to the presence of more severe underlying CV disease and a greater burden of comorbidities.
In 2010, the Clopidogrel and the Optimization of Gastrointestinal Events Trial (COGENT) randomized 3,873 patients with an indication for dual antiplatelet therapy (DAPT) to omeprazole versus a control group [19,20]. The study reported a decrease in GI bleeds between both groups without significant difference in the cardiovascular end point between the two groups (HR: 0.3, 95% CI, 0.13–0.66 and HR: 0.99, 95% CI, 0.68–1.44).
However, the study has several limitations. The study was terminated early and had lower rates of adverse events than expected, leading to a wider confidence interval and lower statistical power. The population consisted primarily of white race (94%), limiting the generalizability of the results to a broader population. Furthermore, the specific formulation of omeprazole used in the study may not be available to the general population.
In contrast, a Danish study of over 55,000 patients found a 29% increased risk of death within 30 days of hospital discharge among PPI users, regardless of clopidogrel use (HR: 1.29, 95% CI: 1.17–1.42) [13]. This suggests potential mechanisms beyond drug interaction contributing to PPIs' adverse cardiovascular effects, necessitating further research.
Following their 2010 study, Charlot et al. conducted a similar study investigating adverse cardiovascular events in patients admitted for MI who were also taking aspirin and a PPI [21]. The study focused on death from cardiovascular disease and readmission for MI or stroke as primary outcomes, with secondary outcomes including all-cause death and hospital readmission for MI or stroke. Their findings revealed an increased risk of composite adverse events in PPI users (HR: 1.46, 95% CI: 1.33–1.61). Notably, no such increased risk was observed in patients treated with aspirin and an H2RA.
While limitations inherent to observational studies, including potential bias due to pre-existing conditions arise, the study employed propensity score matching to account for baseline differences and benefitted from a large sample size. The authors propose impaired aspirin absorption secondary to reduced acid secretion as a potential explanation for their findings.
Stockl et al. conducted a retrospective cohort study investigating the association between PPI use and cardiovascular outcomes after stent placement [22]. Their findings revealed an increased risk of re-hospitalization due to MI in patients receiving both PPIs and clopidogrel compared with those on clopidogrel alone (HR: 1.93, 95% CI: 1.05–3.54).
A 2015 study, utilized data mining to query more than 2.9 million individuals, reported a 16% increased risk of MI and doubled cardiovascular mortality among PPI users compared with non-users (HR: 2.00, 95% CI: 1.07–3.78) [23]. Importantly, histamine H2-receptor antagonists (H2RA) users did not show this increased risk, which might suggest a specific effect of PPIs on cardiovascular health, not solely misdiagnosed angina driving the association.
A 2018 nested case-control study by Casula et al. demonstrated a significant association between PPI use and increased hospitalization for cardiovascular events regardless of the specific PPI used (aOR 1.61, 95% CI: 1.55–1.68) [12]. This study's innovative “user-only” design minimized confounding by selecting patients already taking H2RAs as the control group, comparing outcomes within a similar population with the same baseline risk factors for acid reflux. This approach reduced the influence of pre-existing conditions contributing to PPI use and cardiovascular events, leading to a more robust assessment of PPIs' independent effect on cardiovascular health.
A key consideration when comparing populations treated with PPIs and H2RAs is the potential for confounding biases. Given the more frequent recommendation of PPIs for patients with cardiovascular disease, the PPI-treated population may exhibit a higher baseline risk of cardiovascular events [24]. The Casula et al. study provides further insight into this matter [12]. The increased risk of cardiovascular events observed in the study was evident in both young patients and those not taking antiplatelet medication, suggesting mechanisms beyond impaired platelet aggregation.
While observational studies based on claims data are susceptible to limitations such as coding errors, incomplete data and confounding bias, the matched cohort methodology employed in this study helped to minimize baseline characteristic differences between groups. Interestingly, pantoprazole and rabeprazole, PPIs known for lower hepatic CYP pathway inhibition, were predominantly used in the PPI group [25]. This topic will be explored further in subsequent sections.
A 2017 prospective Spanish study by Lazaro et al. followed 706 patients with coronary artery disease (CAD) for an average of 2.2 years [26]. Statistical analysis showed that PPI use was an independent predictor of death or heart failure (HR: 2.12, 95% CI: 1.23–3.67), but not acute ischemic events. Patients taking PPIs were more likely to be older and have a history of stroke, suggesting a worse baseline cardiovascular profile. Limitations of the study include a high number of patients excluded due to strict exclusion criteria, which may introduce selection bias. Additionally, the study was non-randomized with limited statistical power, furthermore, they could not determine medication adherence.
To investigate the impact of long-term use of PPIs on cardiovascular health and its potential interaction with aspirin, Dahal et al. conducted a meta-analysis of nine studies [27]. The analysis included PPIs like rabeprazole, esomeprazole, lansoprazole and omeprazole. Their findings suggested that PPI use decreased the risk of GI events without a significant increase in major cardiovascular adverse events, including all-cause mortality, cardiovascular mortality and non-fatal MI. However, it's essential to acknowledge the limitation of this review: the lack of individual patient data and distinct methodologies among studies. Additionally, while all studies had a follow-up duration exceeding 1 month, there was significant heterogeneity in follow-up periods across the included studies.
Furthermore, a 2021 community-based cohort study linked long-term PPI exposure (>5 years) to a higher risk of total CV disease in users compared with non-users [28]. While observational, this study suggests a potential association between chronic PPI use and increased CVD risk. In contrast with the Casula et al. study, this association might be partially explained by the potential misdiagnosis of angina as dyspepsia in PPI users, masking underlying cardiovascular issues. Similar to previous studies, the risk wasn't as prominent in H2RA blocker users as previously seen by Shah et al. [23].
On the other hand, a randomized clinical trial of over 17,000 participants with stable CAD and peripheral artery disease demonstrated no difference in the CV composite of MI, stroke, or CV death in patients taking pantoprazole and aspirin/rivaroxaban (HR: 1.04, 95% CI, 0.93–1.15) when compared with placebo [29]. This study was conducted for a timeframe of three years at a cardiovascular center of excellence, which might limit the possible misclassification of angina in dyspepsia previously examined as a confounder. Although Rivaroxaban undergoes metabolism by a CYP pathway similar to clopidogrel, it does not require conversion to an active metabolite by this hepatic pathway [30]. Similarly, aspirin is absorbed in its active form and then undergoes hepatic metabolism for degradation and excretion [31].
A 2021 longitudinal cohort study by Rooney et al. investigated the association between PPI use and CV events [32]. The study revealed a higher prevalence of hypomagnesemia and CV events among elderly patients taking PPIs (HR: 1.31, 95% CI: 1.10–1.57). The association between CV events and PPI use was more pronounced in patients also taking diuretics (HR: 1.59, 95% CI: 1.17–2.17), suggesting a potential synergistic effect on electrolyte disturbances, thereby increasing the risk of CV complications. Similar to previous studies the use of H2RA did not demonstrate an increased risk [13,23].
A comprehensive meta-analysis by Nolde et al. synthesized evidence from the past two decades to evaluate the association between PPI use and cardiovascular events [6]. This meta-analysis included 17 studies and employed rigorous sensitivity and bias analyses. The pooled hazard ratio analysis, utilizing a random effects model, revealed no significant difference in the incidence of first myocardial infarction, ischemic stroke, or cardiovascular events (HR: 1.05, 95% CI: 0.83–1.32, HR: 1.08, 95% CI: 0.97–1.20; HR: 1.05, 95% CI: 0.96–1.15, respectively).
Due to the inherent limitations of the study design, subgroup analyses were not feasible. Such analyses, examining specific PPIs, long-term PPI use, or cumulative dosing, could potentially elucidate more nuanced associations. However, the pooled analysis provides a valuable overview of the overall relationship between PPIs and cardiovascular outcomes.
A meta-analysis by Jeridi et al. comprehensively evaluated the long-term impact of PPIs on CV health [33]. This study included ten observational and RCTs, encompassing over 53,000 patients. The primary end point of the analysis, assessing the overall effect of PPIs as a class, revealed no significant increase in MACE (OR 1.02, 95% CI: 0.94–1.11).
However, when adjusting for clopidogrel use, the meta-analysis yielded conflicting results. Sensitivity analyses suggested a positive association between PPI use and increased CV events (OR 1.45, 95% CI: 1.31–1.60). It remains unclear whether baseline patient characteristics within the clopidogrel group might have influenced these findings.
Consistent with the study by Nolde et al. this study was unable to definitively extrapolate specific PPI outcomes. The heterogeneity of evidence and the potential for distinct safety profiles among individual PPIs suggest that further exploration is warranted. To delve deeper into the potential mechanisms underlying PPI-induced cardiovascular risk, we will now examine specific pathways and interactions (Table 2).
Table 2.
Studies associating PPI with CV outcomes.
| Study (year) | Study type | Primary end point | Key findings | Ref. |
|---|---|---|---|---|
| Juurlink et al. (2010) | Case-Control | MI risk | Found evidence of a loss of beneficial effect on clopidogrel when used with PPI other than pantoprazole. | [17] |
| Kreutz et al. (2010) | Observational study | MACE | Observed an increased rate of MACE on concomitant PPI and clopidogrel use. | [18] |
| Bhatt et al. (2010) | Randomized controlled trial | MACE and GI events | Found decreased rate of GI events without increased risk of cardiovascular events with omeprazole use. | [20] |
| Charlot et al. (2010) | Observational cohort study | MACE and CV death | Observed increased cardiovascular risk associated with PPI use, independent of clopidogrel use | [13] |
| Charlot et al. (2011) | Observational cohort study | MACE and CV death | Observed increased risk of adverse cardiovascular events in aspirin and PPI-treated patients with first-time myocardial infarction. | [21] |
| Stockl et al. (2010) | Observational study | CV rehospitalization risk | Found increased risk of rehospitalization with PPI and clopidogrel use. | [22] |
| Shah et al. (2015) | Observational study | MI risk | Observed increased risk of myocardial infarction with PPI use. | [34] |
| Sherwood et al. (2015) | Meta-analysis | CV outcomes | Found increased risk of CV events of mortality in patients taking PPI. | [35] |
| Lázaro et al. (2017) | Observational study | Heart failure and death | Found increased risk of heart failure and death with PPI use. | [26] |
| Dahal et al. (2017) | Meta-analysis | MACE and GI events | Concluded that PPIs improve GI outcomes without an increased cardiovascular risk. | [27] |
| Moayyedi et al. (2019) | Randomized controlled trial | Safety of PPIs | Demonstrated no difference in CV outcomes in patients receiving PPI with either rivaroxaban or aspirin. | [29] |
| Rooney et al. (2021) | Longitudinal cohort | CV events and hypomagnesemia | Observed increase in CV events and hypomagnesemia in elderly PPI users. | [32] |
| Bell et al. (2021) | Observational study | Cardiovascular disease and heart failure | Found increased risk of cardiovascular disease and heart failure with PPI use. | [28] |
| Nolde et al. (2022) | Meta-analysis | Cardiovascular events | Found no increased risk on first CV events in long term PPI use. | [6] |
| Jeridi et al. (2023) | Meta-analysis of RCT | MACE | Found concomitant PPI and clopidogrel use was linked to an increased risk of MACE. | [33] |
CV: Cardiovascular; GI: Gastrointestinal; MACE: Major adverse cardiovascular event; MI: Myocardial infarction; PPI: Proton pump inhibitor; RCT: Randomized control trial” to table dictionary
2.2. PPI & antiplatelet therapy
2.2.1. Aspirin
Aspirin inhibits platelet aggregation by irreversibly inhibiting cyclooxygenase-1, thereby preventing the production of thromboxane A2, a potent stimulator of platelet aggregation. PPIs are often used in combination to avoid the formation of peptic ulcers and GIB. Although there are no established pharmacokinetic interactions between aspirin and PPI (like those with clopidogrel), some studies suggest that the suppressive effect exerted on gastric acid may reduce the bioavailability of aspirin. Reduced gastric acidity leads to reduced lipophilicity and drug uptake.
Studies investigating the interaction between PPIs and aspirin on platelet function have yielded conflicting results. A small Spanish study by Iñarrea et al. observed no significant differences in platelet aggregation in patients taking omeprazole and aspirin [36]. Similarly, a Taiwanese study by Özel et al. with 199 participants found no decrease in platelet antiaggregation activity when lansoprazole was co-administered [37]. However, a larger Danish study with over 400 patients, demonstrated increased residual platelet aggregation in those using aspirin concurrently with PPIs as compared to those without [38].
Several factors explain these discrepancies. One possibility is the use of higher aspirin doses in the studies by Iñarrea and Özel [36,37]. These higher doses could potentially overcome any inhibitory effect of PPI aspirin absorption. Also, methodological differences between the studies, such as sample size, patient characteristics and specific assays used to measure platelet aggregation, could contribute to the contrasting results.
The Danish study's larger sample size and longer time examined might have led to a more robust detection of the interaction [38]. However, it's important to note that the studies by Iñarrea and Özel examined short-term PPI use on aspirin anti-aggregation properties; hence results can not be extrapolated to the impact of chronic co-administration of aspirin and PPIs on platelet function.
2.3. PPI & P2Y12 inhibitors
P2Y12 inhibitors reduce platelet aggregation by blocking adenosine diphosphate P2Y12 receptors on platelets and play a significant role in reducing major adverse cardiovascular events (MACE) after percutaneous coronary (PCI) in patients with acute coronary syndrome (ACS). Clopidogrel, prasugrel and ticagrelor are this family's most common oral agents.
2.4. Clopidogrel
Clopidogrel remains the agent of choice for DAPT following PCI due to reduced costs and concerns of higher bleeding risks with prasugrel and ticagrelor. Clopidogrel is a pro-drug that requires hepatic activation by the CYP450, primarily CYP2C19, which is also responsible for the metabolism of PPI, leading to competitive inhibition. (Table 2, summarizes antiplatelet medication metabolism) [39–41].
Observational evidence by Juurlink et al. suggested that pantoprazole, a PPI with weak inhibition of the CYP450 2C19 enzyme, responsible for clopidogrel metabolism to its active form, had no association with readmission for MI [17] However, a crucial limitation of the study by Juurlink et al. is the lack of subgroup analysis for patients taking pantoprazole compared with those using other PPIs. This lack of detailed information regarding baseline characteristics hinders a definitive explanation for the observed difference with pantoprazole.
Observational data from Sherwood et al. and the COGENT trial further corroborate this interaction [35]. These studies have consistently demonstrated a significant association between omeprazole and clopidogrel, attributable to omeprazole's inhibition of the CYP2C19 enzyme. This interaction underscores the critical importance of considering its potential implications when prescribing these medications concurrently.
Gillard et al. conducted a double-blind study to directly assess the impact of PPIs on clopidogrel's effectiveness [42]. Their findings revealed a potential decrease in clopidogrel's platelet inhibitory function when used in conjunction with certain PPIs, particularly omeprazole.
Ho et al. found a significant association between clopidogrel use and PPI with re-hospitalization for ACS and all-cause mortality [43]. Rehospitalization or death due to ACS occurred in 29.8% of PPI users and 20.8% of non-PPI users (aOR, 1.25 95% CI: 1.11–1.41). The secondary outcomes analyzed were also higher between patients taking clopidogrel and PPI compared with those taking clopidogrel without PPI; recurrent hospitalization for ACS (14.6% vs. 6.9%, p < 0.001), revascularization procedures (15.5% vs 11.9%, p < 0.001) and death (19.9% vs. 16.6%, p < 0.001). The study identified a potential link between the duration of combined therapy and the severity of adverse outcomes. They reported that each 10% increase in the cumulative duration of co-treatment during the follow-up period was associated with a statistically significant increase in the risk of both death and hospitalization for ACS (OR 1.07, 95% CI: 1.05–1.09).
It is important to acknowledge potential limitations that might have influenced these findings. Patients prescribed PPIs in the study may have had a higher burden of pre-existing medical conditions compared with the non-PPI group. These comorbidities, such as coronary artery bypass surgery history, peripheral artery disease, chronic obstructive pulmonary disease, diabetes and lower left ventricular ejection fraction, could independently contribute to the worse clinical outcomes observed in the combined therapy group.
Another limitation to consider is the potential for bias due to undisclosed PPI use. Since the Ho et al. study was conducted, PPIs have become readily available over the counter, raising the possibility that some patients in both groups might have been taking PPIs without reporting it. This unreported use could have skewed the results toward a more negative association between combined therapy and adverse outcomes.
These studies highlighted an increased risk of major cardiac adverse events in patients with co-administered clopidogrel and PPIs. Consequently, the FDA issued a public health advisory in 2009, warning against the concomitant use of clopidogrel and omeprazole due to the potential for drug interactions [44].
2.5. Prasugrel
Prasugrel is a newer and more efficient agent for preventing thrombotic events after PCI. Like clopidogrel, it is a pro-drug metabolized primarily by CYP2B6 and CYP2C19 to a lesser extent. It is theorized that prasugrel's pharmacokinetics are less likely to be altered by CYP2C19 substrates or inhibitors.
O'Donoghue et al. performed an analysis of the PRINCIPLE (Prasugrel In Comparison to Clopidogrel for Inhibition of Platelet Activation and Aggregation)-TIMI 44 (primary end point: platelet function) and TRITON (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel)-TIMI 38 (primary end point: cardiovascular death, MI and stroke) [45]. In patients treated with clopidogrel, platelet aggregation was lower in those treated with PPI than in those not treated with PPI (23.2 ± 19.5 vs. 35.2 ± 20.9, p = 0.02). Similar findings were seen in patients treated with prasugrel and PPI versus those not treated with PPI (69.6 ± 13.5% vs. 76.7 ± 12.4, p = 0.054). When analyzing primary outcomes, they found no association between PPI use and treatment with clopidogrel or prasugrel (HR: 0.94, 95% CI, 0.80–1.11; HR: 1.00, 95% CI: 0.85–1.20).
An analysis of the TRANSLATE-ACS registry demonstrated an association between discharge on a PPI and elevated risk of MACE, defined as death, MI, revascularization, or stroke (HR: 1.38, 95% CI: 1.21–1.58) [46]. However, the effect of PPI use on the effectiveness of prasugrel and clopidogrel, in preventing MACE, was not statistically significant. Specifically, the HR for MACE with prasugrel compared with clopidogrel was similar for both patients taking PPIs and those not taking PPIs (HR: 1.07, 95% CI: 0.90–1.28 vs. HR: 0.88, 95% CI: 0.62–1.26). These findings suggest that while PPIs may independently increase MACE risk, they do not appear to moderate the response to either P2Y12 inhibitor significantly. This observation further supports the possibility of an intrinsic risk profile associated with PPI use in this patient population.
Nicolau et al. conducted a secondary analysis of the TRILOGY ACS trial to investigate the potential interaction between PPI use and clinical outcomes in patients with ACS managed conservatively (without revascularization) [47]. A concerning trend emerged from the analysis: patients receiving both a PPI and prasugrel exhibited a significantly increased risk of MI compared with those on prasugrel alone (HR: 1.38, 95% CI: 1.21–1.58). Notably, the risk of MI was even higher in the clopidogrel group receiving PPIs (HR: 1.61, 95% CI: 1.19–2.17).
Considering the potential metabolic interaction between PPIs and P2Y12 inhibitors, particularly clopidogrel, these findings suggest a possible attenuation of the beneficial antiplatelet effect when used concurrently. However, it's important to note that previous randomized controlled trials have also reported an increased rate of events in patients taking clopidogrel alone [48]. Interestingly, the study found no association between PPI use and altered platelet function as measured by platelet aggregation tests. This points toward a mechanism beyond direct inhibition of platelet activity, necessitating further investigation to elucidate the underlying processes.
2.6. Ticagrelor
Ticagrelor is a reversible antiplatelet agent approved for use in ACS that, unlike prasugrel and clopidogrel, does not require metabolic activation by CYP enzymes. However, ticagrelor is both a substrate and weak inhibitor for P-glycoprotein, an efflux transporter in the intestinal epithelium that plays a role in drug absorption, distribution and resistance [49]. PPIs may inhibit P-gp and promote drug-drug interactions by altering metabolism.
An ad hoc analysis of the PLATO trial by Goodman et al. determined that increased CV events were associated with both clopidogrel and ticagrelor regardless of PPI use [50]. Considering that ticagrelor does not require biotransformation by the CYP enzymes, it suggests that the association of the PLATO trial may be due to confounding and that it represents a marker of cardiovascular risk rather than a causative agent. This further supports the hypothesis by Nicolau et al. that PPI might just be a marker of increased comorbidities, as similar outcomes with prasugrel were seen [47] (Table 3).
Table 3.
Common antiplatelet drugs and metabolic pathway.
| Drug | Mechanism of action | Pro-drug | Metabolized by CYP (isoenzyme) | Common prescribed dose |
|---|---|---|---|---|
| Clopidogrel | P2Y12 receptor antagonist | Yes | Yes (CYP2C19, CYP3A4) | 75 mg once daily (loading dose of 300–600 mg) |
| Ticagrelor | P2Y12 receptor antagonist | No | Yes (CYP3A4, CYP3A5) | 90 mg twice daily (loading dose of 180 mg) |
| Prasugrel | P2Y12 receptor antagonist | Yes | Yes (CYP3A4, CYP2B6) | 10 mg once daily (loading dose of 60 mg) |
| Aspirin | COX-1 inhibitor | No | No | 75–162 mg once daily (loading dose of 324 mg) |
COX-1: Cyclooxygenase-1; CYP: Cytochrome P450.
2.7. PPI & electrolyte homeostasis
2.7.1. Calcium
Calcium is a critical intracellular molecule that plays multiple roles in myocardial depolarization, membrane stabilization and sarcomere contraction. Its absorption is presumed to be affected by PPI through several mechanisms as it depends on the stomach's acidic environment promoting the ionization of calcium before it can be absorbed [51–53]. Data also supports that PPI-induced hypochloremia reduces the bioavailability of calcium, especially in older adults [51].
Furthermore, increased gastrin secretion and subsequent suppression of somatostatin have also been studied in animals, increasing PTH expression and leading to bone resorption. These mechanisms were supported by the 2023 cross-sectional study conducted by Fitzpatrick et al. [52]. A retrospective study by Hinson et al. found higher levels of PTH (65.5 vs 30.3 pg/ml, p < 0.001, normal range 10–55 pg/ml) and lower calcium (9.1 vs. 9.4 mg/dl, p = 0.02; normal range 8.5–10.5 mg/dl) in PPI users versus non-users despite concomitant use of bisphosphonates [51].
Since the 1960s, research has linked hypocalcemia to significant cardiovascular complications [54]. This connection has been further strengthened by studies demonstrating poorer cardiovascular outcomes and increased mortality in patients with hypocalcemia [55,56]. A retrospective study by Yamaguchi et al. further supports this association, finding that hemodialysis patients with low ionized calcium levels were more likely to experience both increased mortality and cardiovascular issues [57].
Wang et al. also proposed an inverse association between serum calcium and outcome in CAD [58]. In this study, patients with lower serum calcium on admission presented with higher in-hospital mortality. They also propose alterations of the cardiac electrical activity extension in cardiomyocytes: lower calcium levels delay the closure of L-type calcium channels and extend the plateau phase (phase 2) of the cardiac action potential.
An increase in duration of the cardiac depolarization can lead to prolongation of the QT interval and the development of ventricular arrhythmias, a phenomenon that will be discussed in subsequent sections [59]. Moreover, hypocalcemia can also contribute to myocardial contractile dysfunction through impaired excitation-contraction coupling and decreased intracellular calcium levels, resulting in diminished contractility [60–63].
2.7.2. Potassium
The relationship between PPIs and potassium levels remains complex. While some studies suggest a potential association with a modest but statistically significant increase in serum potassium, particularly in the elderly and patients with baseline renal dysfunction, others report cases of refractory hypokalemia that resolved upon stopping PPIs [64–66]. This latter case involved diarrhea caused by PPI-induced microscopic colitis, suggesting an indirect effect. Further research is needed to clarify the mechanisms underlying these seemingly contradictory observations.
A meta-analysis by Xi et al. investigated the association between serum potassium levels and mortality in patients who had recently suffered an acute MI [67]. Their findings revealed a U-shaped relationship, indicating that elevated and decreased potassium levels from the normal range were associated with an increased risk of death. This observation aligns with previous research by Gu et al. who explored the impact of calcium levels on post-MI outcomes and similarly identified a U-shaped association with mortality [68]. These findings highlight electrolytes' critical role in maintaining myocytes' cellular homeostasis and electrical stability.
The study by Xi et al. suggests dyskalemias may be associated with an increased risk of coronary CV events [69,70]. Moreover, certain medications used in CAD management, such as angiotensin-converting enzyme inhibitors and aldosterone antagonists, can also affect potassium levels and potentially interact with PPIs [71]. While PPI use may be associated with a modest rise in serum potassium, the clinical significance and part of the impact on CV outcomes appear to be perpetuated by an indirect and synergistic mechanism on cellular action potentials and induction of myocyte failure and arrhythmias.
2.7.3. Magnesium
Magnesium is crucial in regulating ions' transfer across myocardial tissue and the intracellular balance of calcium currents [72]. PPIs can disrupt the delicate balance of magnesium in the body. This disruption primarily occurs through a reduction in intestinal absorption, mediated by the inhibition of transient receptor potential melastatin 6 and 7 channels in the apical membrane of enterocytes [73,74]. These channels play a pivotal role in facilitating magnesium uptake from the intestinal lumen and their inhibition can lead to hypomagnesemia.
Concerns about this association between PPI use and hypomagnesemia emerged in the early 20th century, leading to research that ultimately prompted the FDA to issue a safety communication in 2011 [75,76]. A systematic review of sixteen observational studies conducted by Srinutta et al. found that high-dose PPI was associated with higher odds of hypomagnesemia compared with low-dose PPI (OR 2.13, 95% CI: 1.26–3.59). Subsequently, low-dose PPI users had higher odds of hypomagnesemia compared with non-users (OR 2.61, 95% CI: 1.44–4.71) [74].
Building upon this research, Kieboom et al. investigated the potential link between hypomagnesemia and the combined use of PPIs and loop diuretics [77]. The study found that PPI use alone was associated with lower magnesium levels than no PPI use (OR 2.00, 95% CI: 1.36–2.93). This effect was further potentiated when loop diuretics were also administered (OR 7.22, 95% CI, 1.7–30.8).
A follow-up study by Kieboom et al. identified a significant association between low magnesium levels and an increased risk of both coronary heart disease (CHD) and sudden cardiac death (SCD) [78]. Individuals with hypomagnesemia exhibited a statistically significant increase in CHD and SCD (HR: 1.36, 95% CI: 1.09–1.69 and HR: 1.54, 95% CI: 1.12–2.1). Interestingly, the study also revealed a protective effect of higher magnesium levels against CHD development.
These findings align with the substantial influence of magnesium in regulating cellular homeostasis and function, which may contribute to elevated cardiovascular mortality through impaired myocyte homeostasis and function. Magnesium plays a crucial role in regulating the duration of the myocyte's action potential [79]. Hypomagnesemia can lead to electrocardiographic abnormalities such as ST-segment depressions, shortened PR intervals and prolonged QT intervals, all indicators of potential arrhythmias [80].
Magnesium also plays a role in the regulation of the vascular interface and myocyte functions. A seminal case report by Skogestad and Aronsen first hinted at a possible link between hypomagnesemia and coronary vasospasm [81]. Hiroki et al. investigated the effect of magnesium infusion on coronary vasospasm [82]. Their study demonstrated that intravenous magnesium infusion induced coronary vasodilation and counteracted the effects of acetylcholine-induced vasospasm.
In animal research, magnesium infusion before reperfusion of occluded coronaries led to a decrease in infarct size, an effect attributed to decreased reperfusion injury and direct cellular mechanism [83]. Nonetheless, large clinical trials comparing magnesium infusion to placebo failed to demonstrate the protective effect of magnesium post-MI and therefore have not translated into clinical practice [84].
Magnesium deficiency can disrupt ion gradients and calcium handling, potentially compromising cardiac function and precipitating arrhythmias. As a cofactor for Na/K-ATPase and sarcoplasmic/endoplasmic reticulum Ca2+-ATPase pumps, magnesium plays a pivotal role in maintaining proper ion balance and calcium regulation during myocyte contraction and the action potential [85,86]. The delicate equilibrium of calcium within the cellular cytoplasm is essential for myocyte contractility and action potential duration and can significantly influence the risk of heart failure and ventricular arrhythmias [86,87].
Additionally, observational evidence indicates a potential link between the combined use of PPIs and QT-prolonging drugs with an increased risk of QTc prolongation, a precursor to torsades de pointes (TdP), a potentially life-threatening ventricular arrhythmia [88]. In a small observational study, patients with TdP were frequently found to have PPI-induced hypomagnesemia, which was significantly associated with an increased risk of ventricular arrhythmias [89].
Following the studies linking PPI use to TdP, commonly prescribed PPIs (omeprazole, lansoprazole and pantoprazole) have been listed on crediblemeds.com as drugs associated with ventricular arrhythmias and TdP since 2020 [90]. Consequently, the FDA has recommended periodic magnesium monitoring for patients taking PPI for more than two weeks [59].
Larger studies have further corroborated this association. A nationwide Danish case-control study involving over 275,000 cases found an increased risk of out-of-hospital cardiac arrest (OHCA) in patients taking PPIs compared with non-users. (OR: 1.32, 95% CI: 1.28–1.37) [91]. Notably, current, but not past, use of pantoprazole and esomeprazole were associated with the highest odds of OHCA (aOR 1.52, 95% CI: 1.45–1.60 and aOR 1.34, 95% CI: 1.23–1.45, respectively).
Furthermore, a retrospective study by Fan et al. evaluated PPI-induced hypomagnesemia in a clinical setting by examining ECGs in over 24,000 intensive care unit patients [92]. They revealed a significant increase in QT prolongation among those taking PPIs compared with those taking H2RA or no acid suppression therapy (OR 1.66, 95% CI: 1.36–2.03 and OR 1.54, 95% CI: 1.31–1.82), independent of other known QT-prolonging factors. Notably, pantoprazole and lansoprazole demonstrated a higher risk of TdP than omeprazole, suggesting that different cellular mechanisms might be involved.
2.8. PPI effect on myocyte homeostasis
Beyond the electrolyte-altering effects of PPI, recent evidence has highlighted the direct effect on cellular electrophysiology in the cardiac myocyte. A common mechanism of QTc prolongation is the blockage of the human ether-à-go-go-related gene (hERG) channel which conducts the myocardial rapid delayed rectifier potassium current responsible for myocardial depolarization [93].
A study published in Circulation highlighted the class effect inhibition of PPIs by directly binding to the hERG channel [94]. The study analyzed over 4,000 US veterans, finding that PPI use was independently associated with a 20% to 40% increase in QTc duration, even when accounting for magnesium levels and other known QT-prolonging factors, suggesting the direct cellular mechanism to be in effect. Furthermore, the study identified sex, age and racial differences in susceptibility to PPI-induced QTc prolongation, suggesting potential phenotypic variations in the hERG channel across different population groups.
Additionally, a novel study by Lorberbaum et al. combined data mining and laboratory experiments to identify a concerning interaction between lansoprazole and ceftriaxone [95]. They detected longer QTc intervals in patients taking both medications. Follow-up experimental data revealed that both drugs block the hERG channel, leading to significant QTc prolongation, predominantly in white males (12 ms increase, 95% CI: 6.5 to 17 ms, p < 0.001). Although this effect was not observed with other cephalosporins, it is noteworthy due to the widespread concurrent use of ceftriaxone and PPIs in the hospitalized population.
Further supporting these findings, a Canadian study by Bai et al. retrospectively reviewed over 31,000 patients admitted to medicine wards and treated with both PPIs and ceftriaxone [96]. After propensity-matched scoring, patients prescribed lansoprazole had a higher risk of ventricular arrhythmias or cardiac arrest when compared with other PPIs (ARD 1.7%, 95% CI: 1.1–2.3). Similarly, a Japanese study demonstrated a mean increase in QTc prolongation (12 ms) and risk of ventricular arrhythmia and cardiac death in patients receiving lansoprazole and ceftriaxone despite administration route (oral vs intravenous) [97]. This effect was also seen in patients taking intravenous omeprazole but not orally. This could be related to the weaker effect of omeprazole on the hERG channel combined with lower plasma concentrations of the oral form [94].
2.9. PPI & vascular function
The vascular endothelium, a single layer of specialized cells lining the inner surface of blood vessels, plays a critical role in maintaining cardiovascular health. It orchestrates various vital functions, including regulating blood flow, vascular growth and permeability. A healthy endothelium actively releases signaling molecules that influence the growth and behavior of surrounding smooth muscle cells, ensuring proper vascular function. However, disruptions in these finely tuned processes can lead to vascular senescence, characterized by a decline in endothelial cell function and an increased risk of cardiovascular complications [98].
Aging contributes to vascular senescence by weakening endothelial cells' anti-inflammatory and antioxidant defenses, making them more susceptible to oxidative stress and inflammation. This age-related decline in endothelial function increases vulnerability to cardiovascular diseases in older individuals. We will explore the potential impact of PPIs on vascular senescence, considering the potential mechanisms by which PPIs might contribute to this process.
Emerging evidence suggests that PPIs might disrupt the delicate molecular balance within the vascular endothelium. In a biochemical ex vivo study, conducted with endothelial cell culture, Ghebremariam et al. propose a novel mechanism by which PPIs may contribute to vascular dysfunction [99]. Their findings indicate that PPIs inhibit the activity of dimethylarginine dimethylaminohydrolase (DDAH), an enzyme crucial for metabolizing asymmetrical dimethylarginine (ADMA). This inhibition leads to unimpeded ADMA accumulation, which competes with nitric oxide (NO) synthase for binding sites. Consequently, compromised NOS function results in decreased NO synthesis, potentially increasing the risk of vascular inflammation, thrombosis and impaired vasodilatory function.
To validate the results of their in vitro study, Ghebremarian et al. conducted a crossover study to investigate the effects of lansoprazole on vascular endothelial function [34]. In this study, participants received either lansoprazole or a placebo for four weeks, with measurements of ADMA levels compared with tonometric results of vascular blood flow. Even though patients taking PPI demonstrated worsening ADMA levels, the study did not reach statistically significant differences in vascular endothelial function between the two groups.
However, several limitations must be considered when interpreting these findings. Firstly, the sample size was relatively small, potentially limiting the study's ability to detect subtle effects. Secondly, more than the short duration of PPI use (four weeks) might have been required to capture long-term consequences on vascular health. As previously described, the vascular endothelium can compensate for short-term imbalances by utilizing alternative vasodilatory pathways independent of nitric oxide, the enzyme inhibited by elevated ADMA levels [100,101]. This compensatory mechanism might explain the absence of observed endothelial function differences despite potential changes in ADMA levels.
Further supporting this potential link, a 2016 meta-analysis by Schlesinger et al. demonstrated a significant association between elevated ADMA levels and increased cardiovascular events (RR 1.33, 95% CI: 1.22–1.45) [102]. This association strengthens the notion that impaired ADMA metabolism due to PPI use might contribute to vascular senescence. These findings highlight the intricate interplay between molecular processes and endothelial health, warranting further investigation into the long-term effects of PPIs on vascular function.
A German cross sectional study evaluated the effect of PPI use on vascular function by ultrasound flow mediated vasodilation measurements of the brachial artery [103]. The found lower endothelial function by FMD in patients taking PPI when compared with non users (-0.99, 95% CI: -1.96 to -0.02). Despite the limitations in this study, which included a relatively small sample size of 87 predominantly German participants, the findings offer valuable insights in an in vivo cohort. The predominant PPIs used were omeprazole and pantoprazole, with a mean duration of use of 7 days. This duration is notably shorter than the typical treatment course for most PPI indications, which often exceeds two weeks.
Yepuri et al. further explored the cellular effects of PPI [104]. Their study identified elevated protein aggregates, increased levels of reactive oxygen species and accelerated telomere erosion in individuals taking esomeprazole. These cellular changes have a cascading effect, ultimately leading to endothelial dysfunction. Interestingly, ranitidine did not exhibit these detrimental effects on cellular aging processes, suggesting that PPIs may have a specific mechanism affecting these pathways.
The previous findings suggest that PPI-induced dysregulation of vascular NOS and increased vascular senescence may be a novel mechanism explaining the association between PPI use and MACE and mortality. This alternative metabolic pathway offers a compelling explanation compared with CYP drug interactions with antiplatelets, as the increased risk is observed even with drugs not metabolized by this pathway.
3. Conclusion
While PPIs remain a mainstay in treating GI disorders, recent research suggests a potential association with increased CV risk during prolonged use, particularly through mechanisms involving cellular damage, drug interaction and metabolic abnormalities. However, the picture remains complex. Observational studies report a link with adverse CV events, yet randomized controlled trials lack consistent confirmation. Confounding by underlying medical conditions in PPI users is a concern in observational studies.
Mechanistic considerations include potential PPI-induced electrolyte imbalances affecting cardiac function and vascular integrity. However, evidence regarding these mechanisms remains largely theoretical.
Clinicians face a challenge in balancing PPI benefits against potential CV risks. A meticulous assessment of each patient's CV risk profile is essential and a risk-benefit discussion of PPI therapy is warranted. Alternative GI therapies should be explored for high-bleeding risk patients. For patients requiring long-term PPI therapy, careful monitoring of electrolyte levels and QTc intervals is essential. Additionally, selecting PPIs with a lower potential for CYP interactions, such as pantoprazole or rabeprazole, may be prudent. This approach can help mitigate the risk of adverse cardiovascular events associated with PPI use.
Further research is needed to elucidate the mechanisms linking PPIs to CV health and determine long-term vascular effects. Studies investigating interactions with novel anticoagulants are warranted due to their increased use in the past decade.
4. Future perspective
The intricate relationship between PPIs and CV risk necessitates ongoing investigation to fully elucidate its underlying mechanisms and implications. Future research should focus on evaluating interactions between PPIs and novel cardiovascular medications, exploring the direct cellular mechanisms by which PPIs might impact cardiovascular health and conducting more prospective studies to minimize bias and confounding variables. By addressing these research gaps, we can better understand the complex interplay between PPIs and cardiovascular health, enabling clinicians to make informed decisions regarding PPI use and mitigating potential cardiovascular risks for their patients.
Author contributions
GJ Duarte: writing – review & editing, writing – original draft, visualization, validation, data curation, conceptualization. J Lopez: writing – review & editing, F Sosa: writing – review & editing. G Molina: writing – review & editing. M Shaban: writing – review & editing. J Mark: writing – review & editing. A Khizar: writing – review & editing. A Sreenivasan: writing – review & editing. A Tran: writing – review & editing. MR Guerra: writing – review & editing.
Competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
References
Papers of special note have been highlighted as: • of interest; •• of considerable interest
- 1.Shanika LGT, Reynolds A, Pattison S, et al. Proton pump inhibitor use: systematic review of global trends and practices. Eur J Clin Pharmacol. 2023;79:1159–1172. doi: 10.1007/s00228-023-03534-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Masarwa R, Reynier P, Lefebvre C, et al. Prescribing trends of proton pump inhibitors and histamine blockers among children in the United Kingdom (1998–2019): a population-based assessment. Pharmacoepidemiol Drug Saf. 2024;33. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/pds.5752 [DOI] [PubMed] [Google Scholar]
- 3.Brisebois S, Merati A, Giliberto JP. Proton pump inhibitors: review of reported risks and controversies. Laryngoscope Investig Otolaryngol. 2018;3:457–462. doi: 10.1002/lio2.187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chinzon D, Domingues G, Tosetto N, et al. Safety of long-term proton pump inhibitors: facts and myths. Arq Gastroenterol. 2022;59:219–225. doi: 10.1590/S0004-2803.202202000-40 [DOI] [PubMed] [Google Scholar]
- 5.Makunts T, Cohen IV, Awdishu L, et al. Analysis of postmarketing safety data for proton-pump inhibitors reveals increased propensity for renal injury, electrolyte abnormalities, and nephrolithiasis. Sci Rep. 2019;9:2282. doi: 10.1038/s41598-019-39335-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nolde M, Ahn N, Dreischulte T, et al. Proton pump inhibitors and the risk of cardiovascular events and cardiovascular mortality: a systematic review and meta-analysis of observational studies. Eur J Intern Med. 2022;106:80–89. doi: 10.1016/j.ejim.2022.09.021 [DOI] [PubMed] [Google Scholar]; •• Nolde et al., in their meta-analysis, scrutinize observational data to highlight the association between PPI use and cardiovascular mortality, employing pooled hazard ratios (HR) to synthesize findings from various observational studies on cardiovascular outcomes.
- 7.Muheim L, Signorell A, Markun S, et al. Potentially inappropriate proton-pump inhibitor prescription in the general population: a claims-based retrospective time trend analysis. Therap Adv Gastroenterol. 2021;14:1756284821998928. doi: 10.1177/1756284821998928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Delcher A, Hily S, Boureau AS, et al. Multimorbidities and overprescription of proton pump inhibitors in older patients. PLOS ONE. 2015;10:e0141779. doi: 10.1371/journal.pone.0141779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Null N, Abraham NS, Hlatky MA, et al. ACCF/ACG/AHA 2010 expert consensus document on the concomitant use of proton pump inhibitors and thienopyridines: a focused update of the ACCF/ACG/AHA 2008 expert consensus document on reducing the gastrointestinal risks of antiplatelet therapy and NSAID use. Circulation. 2010;122:2619–2633. doi: 10.1161/CIR.0b013e318202f701 [DOI] [PubMed] [Google Scholar]; •• Summarizes the latest AHA expert consensus recommendations on PPI use in patients taking P2Y12 inhibitors. It serves as an essential tool for healthcare professionals to assess the appropriateness of PPI therapy in this specific patient population.
- 10.Batchelor R, Kumar R, Gilmartin-Thomas JFM, et al. Systematic review with meta-analysis: risk of adverse cardiovascular events with proton pump inhibitors independent of clopidogrel. Aliment Pharmacol Ther. 2018;48:780–796. doi: 10.1111/apt.14955 [DOI] [PubMed] [Google Scholar]
- 11.Masclee GMC, Sturkenboom MCJM, Kuipers EJ. A benefit-risk assessment of the use of proton pump inhibitors in the elderly. Drugs Aging. 2014;31:263–282. doi: 10.1007/s40266-014-0166-4 [DOI] [PubMed] [Google Scholar]
- 12.Casula M, Scotti L, Galimberti F, et al. Use of proton pump inhibitors and risk of ischemic events in the general population. Atherosclerosis. 2018;277:123–129. doi: 10.1016/j.atherosclerosis.2018.08.035 [DOI] [PubMed] [Google Scholar]
- 13.Charlot M, Ahlehoff O, Norgaard ML, et al. Proton-pump inhibitors are associated with increased cardiovascular risk independent of clopidogrel use: a nationwide cohort study. Ann Intern Med. 2010;153:378–386. doi: 10.7326/0003-4819-153-6-201009210-00005 [DOI] [PubMed] [Google Scholar]
- 14.Veettil SK, Sadoyu S, Bald EM, et al. Association of proton-pump inhibitor use with adverse health outcomes: a systematic umbrella review of meta-analyses of cohort studies and randomised controlled trials. Br J Clin Pharmacol. 2022;88:1551–1566. doi: 10.1111/bcp.15103 [DOI] [PubMed] [Google Scholar]
- 15.Kumbhani DJ, Cannon CP, Beavers CJ, et al. 2020 ACC expert consensus decision pathway for anticoagulant and antiplatelet therapy in patients with atrial fibrillation or venous thromboembolism undergoing percutaneous coronary intervention or with atherosclerotic cardiovascular disease: a report of the American college of cardiology solution set oversight committee. J Am Coll Cardiol. 2021;77:629–658. doi: 10.1016/j.jacc.2020.09.011 [DOI] [PubMed] [Google Scholar]
- 16.Abraham NS, Barkun AN, Sauer BG, et al. American college of gastroenterology-Canadian association of gastroenterology clinical practice guideline: management of anticoagulants and antiplatelets during acute gastrointestinal bleeding and the periendoscopic period. Am J Gastroenterol. 2022;117:542–558. doi: 10.14309/ajg.0000000000001627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Juurlink DN, Gomes T, Ko DT, et al. A population-based study of the drug interaction between proton pump inhibitors and clopidogrel. CMAJ. 2009;180:713–718. doi: 10.1503/cmaj.082001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kreutz RP, Stanek EJ, Aubert R, et al. Impact of proton pump inhibitors on the effectiveness of clopidogrel after coronary stent placement: the clopidogrel Medco outcomes study. Pharmacotherapy. 2010;30:787–796. doi: 10.1592/phco.30.8.787 [DOI] [PubMed] [Google Scholar]
- 19.Bhatt DL, Cryer BL, Contant CF, et al. Clopidogrel with or without omeprazole in coronary artery disease. The New England Journal of Medicine. 2010;363(20):1909–1917. doi: 10.1056/NEJMoa1007964 [DOI] [PubMed] [Google Scholar]
- 20.Bhatt DL, Cryer BL, Contant CF, et al. Clopidogrel with or without omeprazole in coronary artery disease. N Engl J Med. 2010;363:1909–1917. doi: 10.1056/NEJMoa1007964 [DOI] [PubMed] [Google Scholar]
- 21.Charlot M, Grove EL, Hansen PR, et al. Proton pump inhibitor use and risk of adverse cardiovascular events in aspirin treated patients with first time myocardial infarction: nationwide propensity score matched study. BMJ. 2011;342:d2690. doi: 10.1136/bmj.d2690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stockl KM, Le L, Zakharyan A, et al. Risk of rehospitalization for patients using clopidogrel with a proton pump inhibitor. Arch Intern Med. 2010;170:704–710. doi: 10.1001/archinternmed.2010.34 [DOI] [PubMed] [Google Scholar]
- 23.Shah NH, LePendu P, Bauer-Mehren A, et al. Proton pump inhibitor usage and the risk of myocardial infarction in the general population. PLOS ONE. 2015;10:e0124653. doi: 10.1371/journal.pone.0124653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ro Y, Eun CS, Kim HS, et al. Risk of Clostridium difficile infection with the use of a proton pump inhibitor for stress ulcer prophylaxis in critically ill patients. Gut Liver. 2016;10:581–586. Available from: https://www.gutnliver.org/journal/view.html [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zvyaga T, Chang S-Y, Chen C, et al. Evaluation of six proton pump inhibitors as inhibitors of various human cytochromes P450: focus on cytochrome P450 2C19. Drug Metab Dispos. 2012;40:1698–1711. doi: 10.1124/dmd.112.045575 [DOI] [PubMed] [Google Scholar]
- 26.Lázaro AMP, Cristóbal C, Franco-Peláez JA, et al. Use of proton-pump inhibitors predicts heart failure and death in patients with coronary artery disease. PLOS ONE. 2017;12:e0169826. https://journals.plos.org/plosone/article/file?id=10.1371/journal.pone.0169826&type=printable [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dahal K, Sharma SP, Kaur J, et al. Efficacy and safety of proton pump inhibitors in the long-term aspirin users: a meta-analysis of randomized controlled trials. Am J Ther. 2017;24:e559–e569. doi: 10.1097/MJT.0000000000000637 [DOI] [PubMed] [Google Scholar]
- 28.Bell EJ, Bielinski SJ, St Sauver JL, et al. Association of proton pump inhibitors with higher risk of cardiovascular disease and heart failure. Mayo Clin Proc. 2021;96:2540–2549. doi: 10.1016/j.mayocp.2021.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moayyedi P, Eikelboom JW, Bosch J, et al. Safety of proton pump inhibitors based on a large, multi-year, randomized trial of patients receiving rivaroxaban or aspirin. Gastroenterology. 2019;157:682–691.e2. doi: 10.1053/j.gastro.2019.05.056 [DOI] [PubMed] [Google Scholar]
- 30.Zhao T, Chen Y, Wang D, et al. Identifying the dominant contribution of human cytochrome P450 2J2 to the metabolism of rivaroxaban, an oral anticoagulant. Cardiovasc Drugs Ther. 2022;36:121–129. doi: 10.1007/s10557-020-07129-z [DOI] [PubMed] [Google Scholar]
- 31.Du G, Lin Q, Wang J. A brief review on the mechanisms of aspirin resistance. Int J Cardiol. 2016;220:21–26. doi: 10.1016/j.ijcard.2016.06.104 [DOI] [PubMed] [Google Scholar]
- 32.Rooney MR, Bell EJ, Alonso A, et al. Proton pump inhibitor use, hypomagnesemia and risk of cardiovascular diseases: the Atherosclerosis Risk in Communities (ARIC) study. J Clin Gastroenterol. 2021;55:677–683. doi: 10.1097/MCG.0000000000001420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jeridi D, Pellat A, Ginestet C, et al. The safety of long-term proton pump inhibitor use on cardiovascular health: a meta-analysis. J Clin Med Res. 2022;11:4096. doi: 10.3390/jcm11144096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ghebremariam YT, Cooke JP, Khan F, et al. Proton pump inhibitors and vascular function: a prospective cross-over pilot study. Vasc Med. 2015;20:309–316. doi: 10.1177/1358863X14568444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sherwood MW, Melloni C, Jones WS, Washam JB, Hasselblad V, Dolor RJ. Individual proton pump inhibitors and outcomes in patients with coronary artery disease on dual antiplatelet therapy: A systematic review. J Am Heart Assoc. 2015;4(11):e002245. doi: 10.1161/JAHA.115.002245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Iñarrea P, Esteva F, Cornudella R, et al. Omeprazole does not interfere with the antiplatelet effect of low-dose aspirin in man. Scand J Gastroenterol. 2000;35:242–246. doi: 10.1080/003655200750024083 [DOI] [PubMed] [Google Scholar]
- 37.Özel T, Ünal A, Özdem S, et al. Does proton pump inhibitor reduce the antiaggregant efficacy of aspirin in ischemic stroke? Acta Neurol Taiwan. 2023;32(1):9–15. Available from: https://www.ncbi.nlm.nih.gov/pubmed/36474449 [PubMed] [Google Scholar]
- 38.Würtz M, Grove EL, Kristensen SD, et al. The antiplatelet effect of aspirin is reduced by proton pump inhibitors in patients with coronary artery disease. Heart. 2010;96:368–371. doi: 10.1136/hrt.2009.181107 [DOI] [PubMed] [Google Scholar]
- 39.Steinhubl SR. Genotyping, clopidogrel metabolism, and the search for the therapeutic window of thienopyridines. Circulation. 2010;121:481–483. doi: 10.1161/CIR.0b013e3181d1e0e1 [DOI] [PubMed] [Google Scholar]
- 40.Shuldiner AR, O'Connell JR, Bliden KP, et al. Association of cytochrome P450 2C19 genotype with the antiplatelet effect and clinical efficacy of clopidogrel therapy. JAMA. 2009;302:849–857. doi: 10.1001/jama.2009.1232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lopez J, Mark J, Duarte GJ, et al. Role of genetic polymorphisms in clopidogrel response variability: a systematic review. Open Heart. 2023;10:e002436. doi: 10.1136/openhrt-2023-002436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gilard M, Arnaud B, Cornily J-C, et al. Influence of omeprazole on the antiplatelet action of clopidogrel associated with aspirin: the randomized, double-blind OCLA (Omeprazole CLopidogrel Aspirin) study. J Am Coll Cardiol. 2008;51:256–260. doi: 10.1016/j.jacc.2007.06.064 [DOI] [PubMed] [Google Scholar]
- 43.Ho PM, Maddox TM, Wang L, et al. Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome. JAMA. 2009;301:937–944. doi: 10.1001/jama.2009.261 [DOI] [PubMed] [Google Scholar]
- 44.Center for Drug Evaluation, Research . FDA Drug Safety Communication: Reduced effectiveness of Plavix (clopidogrel) in patients who are poor metabolizers of the drug [Internet]. U.S. Food and Drug Administration. FDA; 2019. [cited 2024 Mar 27]. Available from: https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/fda-drug-safety-communication-reduced-effectiveness-plavix-clopidogrel-patients-who-are-poor [Google Scholar]
- 45.O'Donoghue ML, Braunwald E, Antman EM, et al. Pharmacodynamic effect and clinical efficacy of clopidogrel and prasugrel with or without a proton-pump inhibitor: an analysis of two randomised trials. Lancet. 2009;374:989–997. doi: 10.1016/S0140-6736(09)61525-7 [DOI] [PubMed] [Google Scholar]
- 46.Jackson LR II, Peterson ED, McCoy LA, et al. Impact of proton pump inhibitor use on the comparative effectiveness and safety of prasugrel versus clopidogrel: Insights from the Treatment With Adenosine Diphosphate Receptor Inhibitors: Longitudinal Assessment of Treatment Patterns and Events After Acute Coronary Syndrome (TRANSLATE‐ACS) study. J Am Heart Assoc. 2016;5(10):e003829. doi: 10.1161/JAHA.116.00382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nicolau JC, Bhatt DL, Roe MT, et al. Concomitant proton-pump inhibitor use, platelet activity, and clinical outcomes in patients with acute coronary syndromes treated with prasugrel versus clopidogrel and managed without revascularization: insights from the targeted platelet inhibition to clarify the optimal strategy to medically manage acute coronary syndromes trial. Am Heart J. 2015;170:683–694.e3. doi: 10.1016/j.ahj.2015.05.017 [DOI] [PubMed] [Google Scholar]
- 48.Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001–2015. doi: 10.1056/NEJMoa0706482 [DOI] [PubMed] [Google Scholar]
- 49.Dobesh PP, Oestreich JH. Ticagrelor: pharmacokinetics, pharmacodynamics, clinical efficacy, and safety. Pharmacotherapy. 2014;34:1077–1090. doi: 10.1002/phar.1477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Goodman SG, Clare R, Pieper KS, et al. Association of proton pump inhibitor use on cardiovascular outcomes with clopidogrel and ticagrelor: insights from the platelet inhibition and patient outcomes trial. Circulation. 2012;125:978–986. doi: 10.1161/CIRCULATIONAHA.111.032912 [DOI] [PubMed] [Google Scholar]
- 51.Hinson AM, Wilkerson BM, Rothman-Fitts I, et al. Hyperparathyroidism associated with long-term proton pump inhibitors independent of concurrent bisphosphonate therapy in elderly adults. J Am Geriatr Soc. 2015;63:2070–2073. doi: 10.1111/jgs.13661 [DOI] [PubMed] [Google Scholar]
- 52.Fitzpatrick D, Lannon R, Laird E, et al. The association between proton pump inhibitors and hyperparathyroidism: a potential mechanism for increased fracture-results of a large observational cohort study. Osteoporos Int. 2023;34:1917–1926. doi: 10.1007/s00198-023-06867-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kopic S, Geibel JP. Gastric acid, calcium absorption, and their impact on bone health. Physiol Rev. 2013;93(1):189–268. doi: 10.1152/physrev.00015.2012 [DOI] [PubMed] [Google Scholar]
- 54.Johnson JD, Jennings R. Hypocalcemia and cardiac arrhythmias. Am J Dis Child. 1968;115:373–376. doi: 10.1001/archpedi.1968.02100010375014 [DOI] [PubMed] [Google Scholar]
- 55.Kazmi AS, Wall BM. Reversible congestive heart failure related to profound hypocalcemia secondary to hypoparathyroidism. Am J Med Sci. 2007;333:226–229. doi: 10.1097/MAJ.0b013e318039b9c6 [DOI] [PubMed] [Google Scholar]
- 56.Schmitz T, Thilo C, Linseisen J, et al. Low serum calcium is associated with higher long-term mortality in myocardial infarction patients from a population-based registry. Sci Rep. 2021;11:1–8. doi: 10.1038/s41598-021-81929-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yamaguchi S, Hamano T, Doi Y, et al. Hidden hypocalcemia as a risk factor for cardiovascular events and all-cause mortality among patients undergoing incident hemodialysis. Sci Rep. 2020;10:1–9. doi: 10.1038/s41598-020-61459-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang M, Yan S, Peng Y, et al. Serum calcium levels correlates with coronary artery disease outcomes. Open Med. 2020;15:1128–1136. doi: 10.1515/med-2020-0154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.In brief: PPIs and torsades de pointes. Med Lett Drugs Ther. 2016;58(1509):153. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27906148 [PubMed] [Google Scholar]
- 60.Alvarado FJ, Valdivia HH. Mechanisms of ryanodine receptor 2 dysfunction in heart failure. Nat Rev Cardiol. 2020;17:748. doi: 10.1038/s41569-020-00443-x [DOI] [PubMed] [Google Scholar]
- 61.Miotto MC, Reiken S, Wronska A, et al. Structural basis for ryanodine receptor type 2 leak in heart failure and arrhythmogenic disorders. Nat Commun. 2024;15:8080. doi: 10.1038/s41467-024-51791-y [DOI] [PMC free article] [PubMed] [Google Scholar]; • Delves into the biological and cellular underpinnings of cardiovascular events, with a particular emphasis on the intricate relationship between calcium homeostasis and ryanodine receptors. The authors elucidate the critical role of cellular homeostasis in the genesis of arrhythmia and heart failure, providing compelling evidence on the molecular basis of these receptors and their profound impact on cardiac function when modified.
- 62.Sung JK, Kim J-Y, Ryu D-W, et al. A case of hypocalcemia-induced dilated cardiomyopathy. J Cardiovasc Ultrasound. 2010;18:25–27. doi: 10.4250/jcu.2010.18.1.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Eryol NK, Colak R, Ozdoğru I, et al. Effects of calcium treatment on QT interval and QT dispersion in hypocalcemia. Am J Cardiol. 2003;91:750–752. doi: 10.1016/s0002-9149(02)03423-9 [DOI] [PubMed] [Google Scholar]
- 64.Gau J-T, Heh V, Acharya U, et al. Uses of proton pump inhibitors and serum potassium levels. Pharmacoepidemiol Drug Saf. 2009;18:865–871. doi: 10.1002/pds.1795 [DOI] [PubMed] [Google Scholar]
- 65.Ness-Jensen E, Fossmark R. Adverse effects of proton pump inhibitors in chronic kidney disease. JAMA Intern Med. 2016;176:868. doi: 10.1001/jamainternmed.2016.1857 [DOI] [PubMed] [Google Scholar]
- 66.Tagboto S. Severe electrolyte disturbances due to proton pump inhibitor therapy: an underrecognized problem with potentially severe sequelae. Am J Case Rep. 2022;23:e936893. doi: 10.12659/AJCR.936893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Xi H, Yu R-H, Wang N, et al. Serum potassium levels and mortality of patients with acute myocardial infarction: a systematic review and meta-analysis of cohort studies. Eur J Prev Cardiol. 2019;26:145–156. doi: 10.1177/2047487318780466 [DOI] [PubMed] [Google Scholar]
- 68.Gu X, Ding X, Sun H, et al. Usefulness of serum calcium in the risk stratification of midterm mortality among patients with acute coronary syndrome. Biomed Res Int. 2019;2019:9542054. doi: 10.1155/2019/9542054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kjeldsen K. Hypokalemia and sudden cardiac death. Exp Clin Cardiol. 2010;15:e96–e99. Available from: https://www.ncbi.nlm.nih.gov/pubmed/21264075 [PMC free article] [PubMed] [Google Scholar]
- 70.Toto RD. Serum potassium and cardiovascular outcomes: the highs and the lows. Clin J Am Soc Nephrol. 2017;12:220–221. doi: 10.2215/CJN.00030117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fiuzat M, Ezekowitz J, Alemayehu W, et al. Assessment of limitations to optimization of guideline-directed medical therapy in heart failure from the GUIDE-IT trial: a secondary analysis of a randomized clinical trial. JAMA Cardiol. 2020;5:757–764. doi: 10.1001/jamacardio.2020.0640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Baker WL. Treating arrhythmias with adjunctive magnesium: identifying future research directions. Eur Heart J Cardiovasc Pharmacother. 2017;3:108–117. doi: 10.1093/ehjcvp/pvw028 [DOI] [PubMed] [Google Scholar]
- 73.Luongo F, Pietropaolo G, Gautier M, et al. TRPM6 is essential for magnesium uptake and epithelial cell function in the colon. Nutrients. 2018;10(6):784. doi: 10.3390/nu10060784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Srinutta T, Chewcharat A, Takkavatakarn K, et al. Proton pump inhibitors and hypomagnesemia: a meta-analysis of observational studies. Medicine. 2019;98:e17788. doi: 10.1097/MD.0000000000017788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Center for Drug Evaluation, Research . FDA Drug Safety Communication: low magnesium levels can be associated with long-term use of Proton Pump Inhibitor drugs (PPIs) [Internet]. U.S. Food and Drug Administration. Silver Spring, MD: FDA; 2019. [cited 2024 Mar 27]. Available from: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-low-magnesium-levels-can-be-associated-long-term-use-proton-pump [Google Scholar]
- 76.Shechter M. Magnesium and cardiovascular system. Magnes Res. 2010;23:60–72. doi: 10.1684/mrh.2010.0202 [DOI] [PubMed] [Google Scholar]
- 77.Kieboom BCT, Kiefte-de Jong JC, Eijgelsheim M, et al. Proton pump inhibitors and hypomagnesemia in the general population: a population-based cohort study. Am J Kidney Dis. 2015;66:775–782. doi: 10.1053/j.ajkd.2015.05.012 [DOI] [PubMed] [Google Scholar]
- 78.Kieboom BCT, Niemeijer MN, Leening MJG, et al. Serum magnesium and the risk of death from coronary heart disease and sudden cardiac death. J Am Heart Assoc. 2016;5(1):e002707. doi: 10.1161/JAHA.115.002707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Redwood SR, Taggart PI, Sutton PM, et al. Effect of magnesium on the monophasic action potential during early ischemia in the in vivo human heart. J Am Coll Cardiol. 1996;28:1765–1769. doi: 10.1016/S0735-1097(96)00373-7 [DOI] [PubMed] [Google Scholar]
- 80.Yang Y, Chen C, Duan P, et al. The ECG characteristics of patients with isolated hypomagnesemia. Front Physiol. 2020;11:617374. doi: 10.3389/fphys.2020.617374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Skogestad J, Aronsen JM. Hypokalemia-induced arrhythmias and heart failure: new insights and implications for therapy. Front Physiol. 2018;9. doi: 10.3389/fphys.2018.01500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Teragawa H, Kato M, Yamagata T, Matsuura H, Kajiyama G. The preventive effect of magnesium on coronary spasm in patients with vasospastic angina. Chest. 2000;118(6):1690–1695. doi: 10.1378/chest.118.6.1690 [DOI] [PubMed] [Google Scholar]
- 83.Christensen CW, Rieder MA, Silverstein EL, et al. Magnesium sulfate reduces myocardial infarct size when administered before but not after coronary reperfusion in a canine model. Circulation. 1995;92:2617–2621. doi: 10.1161/01.CIR.92.9.2617 [DOI] [PubMed] [Google Scholar]
- 84.Baxter GF, Sumeray MS, Walker JM. Infarct size and magnesium: insights into LIMIT-2 and ISIS-4 from experimental studies. Lancet. 1996;348:1424–1426. doi: 10.1016/S0140-6736(96)07281-9 [DOI] [PubMed] [Google Scholar]
- 85.Gomes da Costa A, Madeira VM. Magnesium and manganese ions modulate Ca2+ uptake and its energetic coupling in sarcoplasmic reticulum. ArchBiochem Biophys. 1986;249:199–206. doi: 10.1016/0003-9861(86)90575-8 [DOI] [PubMed] [Google Scholar]
- 86.Negru AG, Pastorcici A, Crisan S, et al. The role of hypomagnesemia in cardiac arrhythmias: a clinical perspective. Biomedicines. 2022;10:2356. doi: 10.3390/biomedicines10102356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kansakar U, Varzideh F, Jankauskas SS, et al. Advances in the understanding of excitation-contraction coupling: the pulsing quest for drugs against heart failure and arrhythmias. Eur Heart J Cardiovasc Pharmacother. 2021;7:e91–e93. doi: 10.1093/ehjcvp/pvab069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hoorn EJ, van der Hoek J, de Man RA, et al. A case series of proton pump inhibitor-induced hypomagnesemia. Am J Kidney Dis. 2010;56:112–116. doi: 10.1053/j.ajkd.2009.11.019 [DOI] [PubMed] [Google Scholar]
- 89.Lazzerini PE, Bertolozzi I, Finizola F, et al. Proton pump inhibitors and serum magnesium levels in patients with torsades de pointes. Front Pharmacol. 2018;9:363. doi: 10.3389/fphar.2018.00363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Woosley RL, Heise CW, Gallo T, Woosley RD, Lambson J, Romero KA, et al. QTdrugs list. Tucson, AZ 85718; AZCERT; (Accessed 11 May 2018). 2020. Available at: www.CredibleMeds.org [Google Scholar]; • This website details a comprehensive list of QTc prolonging medications essential for clinical use to avoid synergistic effects of these medications.
- 91.Eroglu TE, Coronel R, Gislason GH. Use of proton pump inhibitors is associated with increased risk of out-of-hospital cardiac arrest in the general population: a nested case-control study. Eur Heart J Cardiovasc Pharmacother. 2024;10:413–419. doi: 10.1093/ehjcvp/pvae020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Fan W, Liu H, Shen Y, et al. The association of proton pump inhibitors and QT interval prolongation in critically ill patients. Cardiovasc Drugs Ther. 2023;38(3):517–525. doi: 10.1007/s10557-023-07425-4 [DOI] [PubMed] [Google Scholar]
- 93.Recanatini M, Poluzzi E, Masetti M, et al. QT prolongation through hERG K(+) channel blockade: current knowledge and strategies for the early prediction during drug development. Med Res Rev. 2005;25:133–166. doi: 10.1002/med.20019 [DOI] [PubMed] [Google Scholar]
- 94.Lazzerini PE, Cartocci A, Qu YS, et al. Proton pump inhibitors directly block hERG-potassium channel and independently increase the risk of QTc prolongation in a large cohort of US veterans. Circ Arrhythm Electrophysiol. 2021;14:e010042. doi: 10.1161/CIRCEP.121.010042 [DOI] [PubMed] [Google Scholar]
- 95.Lorberbaum T, Sampson KJ, Chang JB, et al. Coupling data mining and laboratory experiments to discover drug interactions causing QT prolongation. J Am Coll Cardiol. 2016;68:1756–1764. doi: 10.1016/j.jacc.2016.07.761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bai AD, Wilkinson A, Almufleh A, et al. Ceftriaxone and the risk of ventricular arrhythmia, cardiac arrest, and death among patients receiving lansoprazole. JAMA Netw Open. 2023;6:e2339893. doi: 10.1001/jamanetworkopen.2023.39893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mitsuboshi S, Imai S, Kizaki H, et al. Concomitant use of lansoprazole and ceftriaxone is associated with an increased risk of ventricular arrhythmias and cardiac arrest in a large Japanese hospital database. J Infect. 2024;89:106202. doi: 10.1016/j.jinf.2024.106202 [DOI] [PubMed] [Google Scholar]
- 98.Ghebre YT, Yakubov E, Wong WT, et al. Vascular aging: Implications for cardiovascular disease and therapy. Translational Medicine (Sunnyvale). 2016;6(4):183. doi: 10.4172/2161-1025.1000183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ghebremariam YT, LePendu P, Lee JC, et al. Unexpected effect of proton pump inhibitors: elevation of the cardiovascular risk factor asymmetric dimethylarginine. Circulation. 2013;128:845–853. doi: 10.1161/CIRCULATIONAHA.113.003602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kellogg DL Jr, Zhao JL, Coey U, et al. Acetylcholine-induced vasodilation is mediated by nitric oxide and prostaglandins in human skin. J Appl Physiol. 2005;98:629–632. doi: 10.1152/japplphysiol.00728.2004 [DOI] [PubMed] [Google Scholar]
- 101.Holowatz LA, Thompson CS, Minson CT, et al. Mechanisms of acetylcholine-mediated vasodilatation in young and aged human skin. J Physiol. 2005;563:965–973. doi: 10.1113/jphysiol.2004.080952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Schlesinger S, Sonntag SR, Lieb W, et al. Asymmetric and symmetric dimethylarginine as risk markers for total mortality and cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. PLOS ONE. 2016;11:e0165811. doi: 10.1371/journal.pone.0165811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Nolde M, Bahls M, Friedrich N, et al. Association of proton pump inhibitor use with endothelial function and metabolites of the nitric oxide pathway: a cross-sectional study. Pharmacotherapy. 2021;41:198–204. doi: 10.1002/phar.2504 [DOI] [PubMed] [Google Scholar]
- 104.Yepuri G, Sukhovershin R, Nazari-Shafti TZ, et al. Proton pump inhibitors accelerate endothelial senescence. Circ Res. 2016;118:e36–e42. doi: 10.1161/CIRCRESAHA.116.308807 [DOI] [PMC free article] [PubMed] [Google Scholar]


