Abstract
Background
Widespread antibiotic prescribing contributes to globally emerging antimicrobial resistance (AMR). Despite stewardship recommendations by the Infectious Diseases Society of America, there is a lack of literature identifying barriers and facilitators to antimicrobial stewardship programs (ASPs) in United States (U.S.) carceral settings.
Methods
Guided by the Theoretic Domains Framework, we performed in-depth interviews with 68 key stakeholders in Massachusetts carceral settings to contextualize barriers and facilitators to ASP implementation. We recruited 32 people incarcerated in Massachusetts jails and 36 carceral clinicians, correctional officers/administrators in Massachusetts and other U.S. states, and Massachusetts community clinicians for interviews.
Results
From the completed semi-structured in-depth interviews, we identified seven salient themes—four barriers and three facilitators—both specific to and across stakeholder groups. Barriers included the following: (1) jail being viewed as a “dirty place” that increases the risk of infections; (2) variable awareness and knowledge of AMR and ASPs; (3) clinicians’ opposition to change and oversight of their antibiotic prescribing; (4) competing priorities taking precedence over ASP implementation. Facilitators included (5) interest in changing the narrative about carceral healthcare through ASP implementation; (6) opportunities for education about ASP and AMR; and (7) the development of systems, policies, and regulations to improve antibiotic prescribing.
Conclusions
To our knowledge, this is the first qualitative study to leverage broad criminal-legal stakeholder groups to inform the next steps in developing and implementing ASPs in carceral settings in the U.S.
Supplementary Information
The online version contains supplementary material available at 10.1186/s44263-024-00090-1.
Keywords: Jails, Prisons, Antimicrobial resistance, Antimicrobial stewardship program, Qualitative research
Background
By 2050, an estimated 10 million people will die annually from antimicrobial-resistant (AMR) infections [1]. To facilitate AMR prevention, the United States (U.S.) Centers for Disease Control and Prevention (CDC) encourages the implementation of antimicrobial stewardship programs (ASP) in all healthcare facilities [2–4]. Core elements of ASPs focus on tracking antimicrobial prescriptions, gathering local resistance data, providing feedback to prescribers, and educating about the dangers of AMR. Optimally, ASP initiatives involve prescribers, nurses, pharmacists, healthcare administrators, and patients, while also adjusting to setting-specific needs [2].
In the U.S., an estimated 1.8 million people are incarcerated, a population greater than any other country in the world [5]. The spectrum of U.S. carceral settings is broad, people jails (short-term detention centers), prisons (long-term detention centers), and also extends to community carceral programs (e.g., probation and parole.) Healthcare coverage for people who are incarcerated is a complex system, although there are several useful resources published that can help guide learning [6, 7]. People who are incarcerated typically lose their insurance coverage [8], and healthcare is provided by clinicians employed either by a government-entity (either at the county, state, or federal level) or by for-profit medical vendors [9]. The level of infectious diseases healthcare delivery available varies depending on the state and the type of settings. Most jails and prisons have clinicians who provide acute and chronic infection management and have the ability to send people to community emergency rooms for evaluation of life-threatening infections. Most clinical interactions in jails and prisons occur with nurses [10–12], who then escalate concerns to the staff clinicians, including Nurse Practitioners (NP), Physician Associates (PA), Doctors of Medicine (MD), and Doctors of Osteopathic Medicine (DO).
People with criminal-legal experience—a term used to describe persons who are either currently incarcerated or have been incarcerated—are at increased risk for several infectious diseases (e.g., methicillin-resistant Staphylococcus aureus (MRSA), pneumococcal disease, meningococcus) [13–18]. A recent study from Chicago found that about 1/5 of men entering the jail were colonized with MRSA [19]. Psychiatric diseases and drug use disorder, which are highly prevalent in carceral facilities, are also linked to an increased risk of infectious diseases [20–23]. Although vaccines are powerful tools to prevent bacterial infections, as evidence by the COVID-19 pandemic, people who are incarcerated report increase mistrust in vaccines and face systemic barriers to vaccination [24–26]. Rates of vaccination, health literacy, and preventative care received in the community setting are lower among people who have lived experience of incarceration—people who are disparately marginalized in society, including individuals who are Black, Hispanic/Latinx, Indigenous, of lower socioeconomic classes, or people with substance use disorder [27–31].
Despite the prevalence of infectious diseases in carceral settings, there are, to our knowledge, only two peer-reviewed articles on ASP implementation in U.S. carceral settings—both from the Federal Bureau of Prisons [32, 33]. In 2021, our research team found heterogeneity in antibiotic prescribing in Massachusetts (MA) houses of corrections [34], which has motivated the development of this project. The goal of the current qualitative study was to conduct in-depth interviews to understand the perspectives of people who reside in, work in, or collaborate with carceral facilities in MA to identify barriers and facilitators related to the implementation of ASP.
Methods
Identification of stakeholders
We identified four groups of people for in-depth interviews and partnered with five jails in MA to facilitate participant recruitment. The first group included adult men and women currently incarcerated in four MA jails aged 18 or older who spoke English or Spanish. We will refer to this group as “people who are incarcerated” henceforth. The second group included clinicians (MD, DO, PA, NP, PharmD, Dentists, Dental Assistants, Registered Nurse (RN), and Licensed Practical Nurse (LPN)) at five MA jails. We will refer to them as “carceral clinicians.” The third group included jail administrators (e.g., correctional officers and superintendents) from three MA jails. This group will be referred to as “carceral administrators.” The fourth and final group included clinicians who either worked in Massachusetts providing healthcare to people in the community (i.e., not during incarceration) but worked in settings with high rates of people getting healthcare who had a history of incarceration. We will refer to them as “community clinicians” henceforth. Table 1 demonstrates where recruitment was approved for each carceral-based stakeholder group. As there are different models of healthcare, we included sites with healthcare through medical vendors and sites with healthcare through the county.
Table 1.
Groups interviewed at five Massachusetts jails
| People who are incarcerated | Carceral clinicians | Carceral administrators | |
|---|---|---|---|
| Jail 1 | Yes | Yes | - |
| Jail 2 | Yes | Yes | Yes |
| Jail 3 | Yes | Yes | Yes |
| Jail 4 | Yes | Yes | Yes |
| Jail 5 | - | Yes | - |
Interview guide development
Following a literature review of qualitative methodology on barriers and facilitators to ASP implementation in healthcare settings, the research team iteratively developed interview guides for each of the four groups described using inductive and deductive practices. The Theoretical Domains Framework (TDF) and Consolidated Framework for Implementation Research (CFIR) guided the inductive question development. CFIR provided a “meta-view” of ASP implementation, and the TDF helped to conceptualize behaviors that support or deter ASP implementation [35]. The interview guide for carceral clinicians also included questions about the existence of or potential for CDC’s Core Elements for Outpatient Antibiotic Stewardship (Commitment, Action for Policy & Change, Antibiotic Tracking, and Expertise) [36]. All interview guides included an informational introduction, which included verbal consent for recording to proceed with the interview. Upon interview conclusion, interviewers asked demographic questions, including age, race, ethnicity, and highest level of education. All interview guides were piloted and refined (Additional file 1).
Recruitment and data collection
People who are incarcerated were invited to participate during their group programming, such as morning meetings, infectious diseases education classes, and when visiting the facility’s infirmary. A script was read in both English and Spanish at these events and people interested in participating met individually with research team members. Carceral clinicians and carceral administrators were recruited during visits to jails and via emails. Community clinicians were identified through networks of research team members. Depending on the jail and other employment regulations, carceral clinicians, carceral administrators, and community clinicians were offered a $50 payment in the form of an Amazon or Home Depot gift card. The institutional review board and jail policies did not allow for payments to be made to people who were incarcerated. Participants were also given the option to donate their $50 to Big Brothers Big Sisters of Eastern Massachusetts or to refuse any payment. Audio recording of interviews was requested. Participants could opt out, in which case written notes were taken by a research team member. Individuals completed the interview with study a team member in private and confidential rooms identified by the hosting facility for people who were incarcerated, carceral clinicians, and carceral administrators. Carceral clinicians, carceral administrators, and community clinicians had the option to complete interviews via Zoom. Interviews were conducted until thematic saturation was reached.
Data analysis
Transcripts (audio) and notes (written notes) were uploaded to Dedoose [37]. Inductive Thematic Analysis (ITA) methods guided data analysis [38]. An initial codebook (Additional file 2) was developed based on interview guides, and the review of 10 randomly selected transcripts to represent each participant group and subgroup. The analytic team (RAT, EDG, YN, AGW, DM) compared coding patterns, and the codebook was refined until a consensus was reached. Discrepancies were resolved through a comparison and consensus process [39]. Quotations were compiled, and concepts and relationships leading to codes and core themes were identified.
A consolidated criteria for reporting qualitative research (COREQ) checklist has been completed to ensure study credibility (Additional file 3).
Results
Sixty-eight participants completed an in-depth interview, including 32 people who are incarcerated, 22 carceral clinicians, 7 correctional administrators and officers, and 7 community clinicians (Table 2). The self-reported race and ethnicity and gender demonstrate successful recruitment of people who are from racially and ethnically minoritized communities. Two interviews were not audio recorded per participant preference. Two interviews were conducted in Spanish with incarcerated people.
Table 2.
Participant demographics
|
People who are incarcerated n = 32 |
Carceral clinicians, carceral administrators, and community clinicians n = 36 |
Totals | |
|---|---|---|---|
| Gender | |||
| Male | 18 | 19 | 37 |
| Female | 13 | 16 | 29 |
| Did not report | 1 | 1 | 2 |
| Race and ethnicity | |||
| White, Non-Hispanic/Latino | 15 | 32 | 47 |
| White Hispanic/Latino | 5 | 1 | 6 |
| Black, Non-Hispanic/Latino | 2 | 1 | 3 |
| Asian, Non-Hispanic/Latino | 0 | 1 | 1 |
| Native American Non-Hispanic/Latino | 1 | 0 | 1 |
| Biracial/multiracial | 6 | 0 | 6 |
| Did not report | 3 | 1 | 4 |
| Age | |||
| < 29 | 3 | 1 | 4 |
| 30–50 | 22 | 20 | 42 |
| > 51 | 5 | 14 | 19 |
| Did not report | 2 | 1 | 3 |
| Education level | |||
| Did not graduate High school | 2 | 0 | 2 |
| High school/GED | 14 | 0 | 14 |
| Some college | 11 | 5 | 16 |
| College degree | 4 | 8 | 12 |
| Masters/Doctorate | 0 | 22 | 22 |
| Undisclosed | 1 | 1 | 2 |
| Total | 32 | 36 | 68 |
Barriers
Theme 1: Jail being viewed as a “dirty place” that increases the risk of infections
Many participants expressed concern that carceral settings are seen as “dirty places” where infections are common, especially MRSA. A person who was incarcerated conveyed this sentiment as, “If it wasn’t that somebody told me about the whole MRSA thing, or anything in here, I would not have a clue about how dirty this place is until I actually came in here and started meeting people and started talking to people.” There is also a perception among healthcare providers that people who are incarcerated frequently request antibiotics for minor ailments or injuries due to a heightened sense of paranoia about the cleanliness of the jail environment and concerns about potential infections like MRSA. A carceral clinician described this as, “[People who are incarcerated] usually want antibiotics for just about everything. They come up with just a little nick on their finger and think they need an antibiotic with no signs of infection at all. They’re really paranoid about the dirtiness of the jail. And they also think that everything is MRSA, which I understand.” A personal perspective from a person who was incarcerated illustrates how even minor injuries are perceived as serious health risks in the carceral setting, leading to a desire for immediate medical intervention, such as antibiotics, to prevent further complications. This participant said, “I have a little tiny cut on my finger from a razor. Something like that could actually get severely worse…to the point that literally my finger could get infected, and down the road, I’m dealing with a way serious issue other than a little tiny baby cut from a razor blade… but now I’m like, ‘Oh shit, give me a band aid. Give me this, give me that, give me antibiotics, which I was happy that they were already putting me on.’”.
Because of this sentiment, carceral clinicians face pressure from people who are incarcerated when it comes to medical treatment, particularly regarding their choice of antibiotics. People who are incarcerated expressing a preference for the medication can be perceived as undermining by the carceral clinician, contributing to tension between the two individuals. Additionally, some clinicians may be concerned about potential legal ramifications, such as lawsuits, which influence their decision-making process regarding medical care in the carceral setting. A carceral administrator noted, “I think the providers get a lot of pressure from inmates also….. I want this. I don’t want that antibiotic. It didn’t work for me. I want this. And some providers will push back and say, ‘Well, we’re going to try this, and this is it.’ ….patients can be pretty pushy about what they want, and then the providers are not wanting to get a lawsuit or get sued, because there’s a lot of litigation in corrections.” A carceral clinician talked about their experience providing care, “You really feel that tension that you want to get to the next patient, but you have to take care of the person who’s in front of you. You don’t wanna shortchange or cut corners and give shoddy care so you’re looking at that tension between giving good care and seeing patients in a timely fashion. That’s the reality.” Another carceral clinician said, “I think most patients want the antibiotic. They understand that jail and prison is a dirty place. They’re scared. They want something. It’s easier to take a pill than fix a problem.”
Theme 2: Variable awareness and knowledge about AMR and ASPs
Although many people who are incarcerated mentioned MRSA, there was a lack of general knowledge about AMR. This was exemplified when asked what they thought the term “antimicrobial resistance” meant. One person who was incarcerated said, “Maybe that you’re allergic?” and another responded with, “Maybe when your antibodies don’t work anymore?”.
There were some people who were incarcerated who conveyed an understanding about the difference between bacterial and viral infections as it relates to treatment they received in the past. One person who was incarcerated said, “The willingness just to sort of give in to people because they think they need an antibiotic, when you are the prescriber, and you theoretically should probably know better than them if they need an antibiotic. You know those Z-Paks, those five-day packs, they used to hand those out. I had a doctor who gave them to me without even prescribing to me. Just gave me samples of them from the office. Like, ‘Here, take a Z-Pak.’ And I’m like, ‘Buddy, I have a cold.’”.
While many did not, several people who were incarcerated were able to identify hallmarks of AMR when probed. For example: “I know all about it. The human body and the bugs adapt much like viruses do. And the more we use antibiotics, the more virulent the bacteria become because they become adapted to it. Well, probably not a good example, but just like people using drugs and alcohol. You use more and more of it, you need more and more of it to get the job done, and it gets to the point where antibiotics stop being effective.” Regardless of whether people who were incarcerated knew about AMR or ASPs, most were interested in improving the healthcare they received and felt AMR should be addressed. One person who was incarcerated did not know what AMR was, but when informed, they said, “We need more awareness…so we can know what’s going on. What’s getting us to the point where we’re using so much [sic] antibiotics? Why are we using antibiotics? What infections are you getting that we have to do this? Why does it keep happening?”.
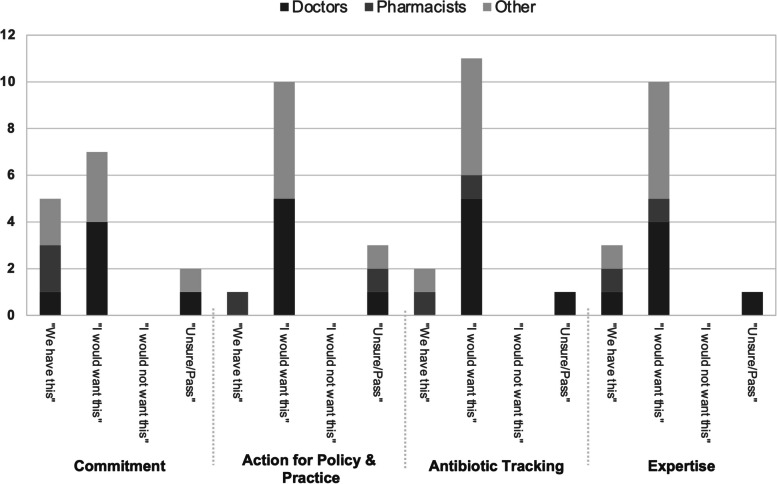
Less than 50% of the clinicians interviewed were aware of and knowledgeable about ASPs. When presented with the CDC Core Elements, clinicians employed in the same facility gave discordant answers to those core elements (Fig. 1). This lapse in knowledge among carceral clinicians was evident to the people who were incarcerated as well. When asked about the perspectives of jail clinicians on AMR, someone who was incarcerated responded, “I’m not so sure they are even aware of it.”
Fig. 1.
Prescriber-specific responses to CDC core elements matrix
Several carceral clinicians did reveal their concerns about AMR and steps taken to mitigate its spread. One explained their patient education about antibiotic use, stating that, “Certain providers definitely are more concerned about it.” One of the carceral clinicians who expressed concern about AMR shared their perspective: “[Explaining why antibiotics are not appropriate] is actually really important to me because it’s a huge problem. Well, around the world and in our country, we over-prescribe antibiotics.” Another carceral clinician talked about how they took stock of their own antibiotic choices internally, “I’m watching every patient I’m seeing, the clinical response, and ultimately I want make sure that they get the right response and I’m choosing my antibiotics based on, what is the evidence and what I think would be the best one to use and with the scenario focus, so that I’m not overutilizing or using too much of an antibiotic.”
While these carceral clinicians were concerned about AMR and even undertook individual stewardship methods, the majority of carceral clinicians were not. Typical responses from carceral clinicians, when probed about their concern level for AMR, were “I don’t think we really have any concerns about AMR,” and, “Certain providers are definitely more concerned about it [than me].” Often, this lack of concern was not due to apathy about AMR in general, but due to competing interests. One carceral clinician stated, “There’s just other issues that are being talked about more often.”
Theme 3: Clinicians’ opposition to change and oversight of their antibiotic prescribing
When asked about optimizing antibiotic prescribing and administration, one carceral clinician expressed confidence in the current practices, stating, “I think we pretty much have everything covered, as far as we have access to everything here. I think we do exactly what we’re supposed to be doing. I can’t see that we could do anything differently.” Similarly, other carceral clinicians echoed this response, remarking, “I don’t see a problem with the way that things are done now.” Additionally, there was a prevalent culture of refraining from questioning fellow prescribers’ antibiotic choices, as exemplified by a carceral clinician who stated, “There’s not a lot of situations where I question their medical judgment or their course of treatment…They have their practice pattern and I certainly respect that, but like I said, I practice differently.”
One carceral clinician shared how some healthcare providers might be resistant to feedback and adhere to personal practice preferences, “We had a doctor here that [sic] thought he was treating very aggressively, so he would order Bactrim DS two tablets twice a day for 14 days, and it came to be his thing. And we were like, ‘Doc, it’s too much for somebody that size. The pharmacy didn’t like that order.’ He’s like, ‘That’s ridiculous. I’m the doctor. I’ve done this in the past, I’m comfortable with it.’” Another carceral clinician pointed out that standardizing antibiotic prescribing practices is challenging due to the variability of infections and individual responses to treatments, acknowledging the complexity of the issue and the difficulty in finding a straightforward solution, commenting that, “It’s hard to really streamline antibiotic prescribing because everyone’s different and there’s different bugs that cause different infections. You can’t say, ‘Oh, put everybody on amoxicillin for a dental infection.’ It doesn’t always work that way, even though that’s the standard of care for, let’s say a simple infection in the mouth. It’s hard to streamline that. It really is. I don’t know if there’s a way to do it. If there is, I’m not that aware of it or it doesn’t come to my mind readily.” Another carceral clinician said, “A lot of people in general, just in life in general don’t like change. All of a sudden, you’re bringing in a new program, like, ‘What does this mean? Do people start reflecting on their own practice? Are they gonna start to scrutinize what I do?’” A person who was incarcerated echoed this sentiment when talking about carceral clinicians at their facility, “They’re pretty set in their ways.” During an interview, it was noted that one clinician was using a 2009 antibiotic guideline to make decisions on antibiotics. When asked if he would ever seek out an updated reference text, the clinician said that he felt the information was still accurate.
Theme 4: Competing priorities more important than ASP implementation
Constraints in resources such as time and money were repeatedly reported as impacting the focus on AMR and ASPs. According to one carceral administrator, “The reason that there are not already ASPs in correctional settings is because there’s not a lot of glamour here, not a lot of investment.” Carceral clinicians, carceral administrators, and community clinicians commented on the challenges of prioritizing ASPs in the already overwhelmed carceral facility. A carceral clinician elaborated, “Not to take away from antibiotic resistance, but there’s just other issues that are being talked about more often. I don’t mean to sound like it doesn’t get brought up. I know that it’s at the forefront of all the providers’ minds when they’re prescribing, especially because a lot of these patients are constantly in and out of here. They’re in and out of ERs. They’ve been prescribed antibiotics a lot. We have a lot of substance users that get abscesses from needles and certain things like that. So, there are a lot of infections, there are a lot of sicknesses, but I just don’t hear about it as much.”
A carceral administrator reflected on the prioritization of healthcare issues within correctional facilities, noting, “I think if you’re looking at the top 10 issues that happen at a site, we’re focused on deaths, suicides, homicides, COVID, trauma, drugs, and I think it’s one of those things where it’s like it hasn’t happened where we’re in a position where we can’t prescribe any longer. It’s like this isn’t good for the future, this isn’t good for this patient, but it’s not actually impacting them in any way. So, I think it’s just kind of on the back burner.” Aside from their opinion on the importance of AMR, many carceral administrators felt that they were overburdened by medical issues. One individual stated, “I do not wish I was more integrated into the medical sector of this facility because I already do enough.”
A community clinician offered further insights into the challenges faced by healthcare systems within correctional facilities, explaining, “My impression of healthcare systems within the carceral system is that there is a lot more need than there is bandwidth or money or services or resources. And so, I think making the case that this is important, and matters is probably going to be the biggest thing. I don’t imagine that correctional officers are just morally opposed to antibiotic stewardship or something like that. I don’t think that that’s the case, but I think it does need to be impressed upon on people that this is actually a big, really bad problem.”
Facilitators
Theme 5: Interest in changing the narrative about carceral healthcare through ASP implementation
Several participants recognized society’s negative perception of jail conditions and emphasized the potential for those working within these institutions to drive significant change for people who are incarcerated. A carceral administrator said, “I’ve been doing work on my side of the business for more than 30 years. I think there is a, sometimes, an unfair characterization of corrections as being not humanistic and not empathetic. My experience, and particularly my experience over the last several years, has been quite the opposite. I would encourage the work that you're doing. Know that there are allies in the field that [sic] would help support you in your work, that appreciate your work, and would really like to help to partner to bring that work behind the walls.”
Administrators also reflected on previous healthcare initiatives to gauge the potential for ASP implementation success and interest in improving healthcare delivery to people who are incarcerated. Discussions often revolved around initiatives such as medication-assisted treatment provision for individuals with substance use disorder within several Massachusetts jails. One jail, in particular, was proud to have been the first in the country to offer this medical treatment to people who are incarcerated. Additionally, participants noted improved intake procedures, indicating an existing culture of reform and a drive to enhance carceral healthcare. The shared commitment among participants to improve carceral resources and conditions serves as a significant facilitator for the implementation of ASPs.
Theme 6: Opportunities for education about ASP and AMR
People who were incarcerated emphasized the need for increased education about AMR, with one participant stating, “Educate more. Educate the nurses in the prisons and the doctors in the prisons. You know what I’m saying? Explain to the inmates too. They all have to know about what’s going on with this [ASP and AMR]. What the antibiotics are for or what they do or how they prescribed.” Another participant who was also incarcerated, stressed the importance of raising awareness, noting, “We need more awareness. Like I barely know much. I know a little bit. I scratched the surface on that…What’s getting us to the point where we’re using so much antibiotics?” People who were incarcerated had no preference of who would provide this information, acknowledging that any increased interaction with medical staff and clinicians would open a space for greater learning opportunities.
A carceral clinician discussed their efforts to provide communicable diseases training for all staff, highlighting the importance of understanding antibiotics, the difference between viral and bacterial infections, and the emergence of superbugs like MRSA. They remarked, “It’s interesting to see how many people don’t know the reason for that [drug-resistant bacteria] …” Regarding awareness of AMR, one carceral clinician acknowledged, “I think we are very aware that there's a lot of antibiotic resistance,” while another carceral clinician expressed less concern, stating, “I don't think we really have any concerns about [AMR].”
Regarding the discussion among clinicians in the jail, a carceral administrator noted, “I’ve never heard them [clinicians] speak about it. I’ve heard them speak about other opinions on medications that we’ve prescribed here, but I’ve never once heard anybody ever say anything about antibiotics.”
Theme 7: The development of systems, policies, and regulations to improve antibiotic prescribing
When discussing avenues to enhance antibiotic prescribing in carceral settings, a person who was incarcerated emphasized the involvement of the medical industry, stating, “The medical industry [needs to be involved]. I mean, I’m not so sure the government needs to step in and create hard, fast regulations, but certainly the medical industry and the licensing bodies could insist that that education be provided and that that information be disseminated right on down the chain to the people who are finally using them.”
A carceral clinician suggested increased oversight through prescription monitoring, proposing, “…[Having] somebody who has the time to go into EMR [electronic medical records], and look at [prescribing] …I think you would just say, ‘Okay, in the last three months, [look] how often penicillin was prescribed, how often sulfa was prescribed and for what.’ And you can kind of look at the chart and see why it was used and how long it was used…I don’t think you’d have to have that the long term. It would just be something you could do and use it as a teaching tool, and that would be specific for that physician and the mid-levels [NPs and PAs] at that site. Because if you go somewhere else, they may have a whole different way of doing it.’” Another carceral clinician proposed incorporating ASP into electronic medical records, “If we can institute [ASP] into an electronic medical record, that’s smart because we have a medical record that is very archaic…ultimately we have so much time in a day and we wanna make sure that we prioritize…”.
Carceral and community clinicians advocated for the involvement of an infectious diseases (ID) physician in antibiotic tracking and oversight. An expert in carceral healthcare who worked outside of Massachusetts said, “If there is a requirement for antibiotic stewardship to get [American Correctional Association (ACA) or National Commission on Correctional Health Care (NCCHC)] accreditation, that would definitely make jails and prisons jump to do it.” A carceral clinician recommended scheduling sessions with an ID physician to discuss antibiotic prescribing and implementing policies promptly indicating that, “Let’s say [an ID physician] plans to come on Monday during the lunch hour to talk to us about antibiotic prescribing. And then, we come up at that time for one policy that would make sense to implement right away.” Moreover, a community clinician highlighted the differences in healthcare system funding between jails/prisons and the community, suggesting that financial incentives for ASP aligned more effectively in carceral settings while also acknowledging how that might appear to the incarcerated patient. They speculated, “To restrict certain antibiotics might help with the budget, as well. I can also imagine that that people who are incarcerated might feel skeptical of restricting antibiotics because they probably are already feeling like they’re not getting the best medical care.”
Discussion
Using robust research methods and the engagement of participants across the spectrum of criminal-legal settings, our research adds context to why carceral settings have largely been absent from research and clinical work done on the implementation of ASPs to improve healthcare. Although antimicrobial stewardship’s necessity as a critical aspect of high-quality acute healthcare seems obvious to many, when ASP champions first implemented programming in hospitals, barriers emerged that were similar to those identified in this study. Some of the first qualitative studies done in non-carceral settings aimed at contextualizing barriers to implementation found that prescribing clinicians feared that ASPs were overly restrictive and impinge on decision-making autonomy [40, 41], a barrier that continues even in the most recently published qualitative work [42]. Similarly, clinicians in this study expressed concerns about antibiotics being scrutinized or being restricted to specific treatment algorithms. The fact that this barrier has been largely overcome in non-carceral settings suggests it is surmountable in carceral settings as well. Interestingly, it was clear from several interactions that the clinicians themselves were aware that the current antibiotic prescribing practices were outdated.
A recent meta-analysis of influential factors in antibiotics prescribing found that the development of ASP programs should ideally be done through co-design to ensure all stakeholders’ voices are heard [43]. The development of ASP programs for jails and prisons is necessary, but the specifics of any program will need to be designed with the input of prescribing clinicians and imposed with sufficient planning. As evidenced from previous experiences in other settings, early engagement of those who make administrative and financial decisions is critical to secure their support. They must be made aware of the cost savings and value added [44]. In any intervention, especially within carceral settings, champions are critical to motivate change, encourage the process of adaptation, and ensure that a diverse group of voices are represented in the process of implementation. Ideally, champions would be medical staff embedded in the jail healthcare system, and the staff would have protected time to develop and oversee an ASP program. In several healthcare settings, nurses and pharmacists have been the most effective champions of antimicrobial stewardship [45, 46]. The current healthcare framework within carceral settings predominantly relies on nursing professionals. Nurse-led quality healthcare initiatives in prisons and jails have been successful [47–49]. For the implementation of new programming in carceral settings, special attention is needed to address complex organizational and inter-agency dynamics [50]. Nurses in jails will make excellent champions because they work with the carceral staff and the medical staff.
It is widely accepted that the most effective interventions to decrease antibiotics should involve the use of multiple components [51]. The published work from the Federal Bureau of Prisons (BOP) both from in 2017 described how a hybrid system of education, closed formulary, clinical practice guidelines, and an antimicrobial stewardship team led by pharmacists to effectively decrease antibiotic prescription recipients from 829/1000 people who were incarcerated in 2010 to 625/1000 people who were incarcerated in 2015 [21]. Then, in 2019, the BOP successfully employed a pharmacist-driven audit and feedback approach which reduced the number of fluoroquinolone prescriptions [33]. In our interviews, many participants suggested strengthening the role of an ID specialist or pharmacist within the jails to support gathering of ASP metrics such as average length of antibiotic course, use of broad antibiotics, or use of antibiotics for likely viral infections. Several carceral systems purchase medications through large distribution centers, pharmacists could be trained to review and approve orders as a form of auditing and feedback and use the data as benchmarking metrics. Increased use of pharmacy residents and students in carceral settings are one way to overcome the potential financial barrier [52]. Telehealth pharmacy oversight is another potential avenue for optimizing antibiotic prescribing [53].
Consistent with other work done in resource-limited settings, participants described competing needs for time and money, thus impeding ASP prioritization. ASP cost-effectiveness has been demonstrated across several healthcare settings, yet not in jails or prisons. Confirming the cost-savings and continued high-quality care after implementation of ASP programs in carceral settings is a necessary research study, although the complexities of healthcare financing in jails and prisons may present a challenge. While antibiotics themselves are usually inexpensive, the staffing required to culture patient samples and administer directly observed antibiotic therapy multiple times a day can pose a significant financial strain on jails and prisons’ healthcare systems.
Notably, included in our research are those who were currently incarcerated. Most participants who were incarcerated expressed comfort in being able to access antibiotics. We highlighted several concerns from patients about MRSA, and one quote in which someone with a cut felt better being on prophylactic antibiotics. The importance of educating on the dangers of inappropriate antibiotic use cannot be overstated [54]. Although some people who were incarcerated were aware of the risks with antibiotic use, they were in the minority. Even with multiple carceral education initiatives, including those designed to mitigate MRSA outbreaks in jails [55–57], there have been no documented programs that specifically discuss the risks of AMR or the dangers associated with antibiotics. As a follow-up to this research, we hope to collaborate with leaders in health literacy and antimicrobial resistance to develop tools aimed at educating people who are incarcerated. To further this success, educational materials must be made available in other languages and at different reading levels to ensure that all individuals have equitable access to improve their AMR awareness and knowledge. Our team’s previous collaboration with local pastors and medical students to facilitate increased COVID-19 vaccine uptake in Massachusetts jails [58] demonstrates that bringing in outside representatives to discuss antibiotic harms may be a useful strategy.
Benchmarking is a system of comparing healthcare process measures that has been effective in curbing unnecessary antibiotic prescriptions [59]. Currently, benchmarking antibiotic use in jails or prisons is not required by the CDC or other national correctional healthcare credentialing agencies. However, we believe that making antibiotic tracking mandatory that ASP efforts could be bolstered. Clinical decision tools embedded in EMR have emerged as an effective strategy for outpatient monitoring of antibiotics [52]. Interestingly, EMR did not emerge in our interviews as either a barrier or facilitator to antimicrobial stewardship. An interesting aspect of jail healthcare is that even in abutting counties, the jails may use totally different EMR systems. For example, in Massachusetts jails, we are aware of at least five different EMRs. Therefore, an integrated EMR across state-specific jails would support the development of benchmarking systems.
This study was subject to several important limitations. Perspectives from people working in Massachusetts may differ from geographic regions of the U.S. Due to limitations in study resources, we were not able to interview people who were incarcerated who spoke a language other than Spanish or English, thus limiting potential perspectives we heard. In comparison to people who were incarcerated, we interviewed a relatively small size of the carceral administrators and community clinician participants. Therefore, when reporting demographic information, researchers had to group responses to protect confidentiality. The potential influence of social desirability bias may have affected our findings, as participants might have felt inclined to adjust their responses to align with support for ASPs. However, it is noteworthy that a considerable number of interviewees either lacked awareness of antimicrobial resistance or deemed it unimportant. This suggests that we likely managed to capture a diverse range of perspectives on the matter.
Despite these limitations, this is the first study to our knowledge that engaged stakeholders from a broad spectrum of lived experience across the spectrum of criminal-legal sector to be participants in research about antibiotic resistance. There are recent initiatives in carceral healthcare to encourage quality improvement projects, and we encourage readers to consider partnership on antibiotic-related projects with partners working in jails and prisons. Although barriers emerged from our discussions with participants, we also identified several facilitators that, if leveraged with support of champions, can positively impact and improve systems of antimicrobial prescribing and counter the threat of antimicrobial resistance.
Conclusions
The benefits of optimizing antibiotic prescribing are clear, but most carceral settings do not have routine systems of antibiotic use evaluation. We identified barriers and facilitators that can provide a scaffold for next steps to asses and improve antibiotic prescribing in jails. We hope this research encourages other people working in carceral settings to ask questions about the gap between community and carceral healthcare and develop systems to equitable care for people incarcerated in jails and prisons.
Supplementary Information
Supplementary Material 1. A collection of all interview guides used to guide conversations with each stakeholder group. Interviews are collated into one file
Supplementary Material 2. The initial codebook developed based on 10 interview guides. Guides were randomly selected to represent each participant group and subgroup
Supplementary Material 3. Reflects the consolidated criteria for reporting qualitative research (COREQ) checklist
Acknowledgements
We would like to thank those who are incarcerated, carceral clinicians, correctional officers, administrative staff, and participants from the community for their collaboration.
Abbreviations
- AMR
Antimicrobial resistance
- ASP
Antimicrobial stewardship program
- U.S.
United States
- CDC
U.S. Centers for Disease Control and Prevention
- NP
Nurse Practitioner
- PA
Physician Associate
- MD
Doctors of Medicine
- DO
Doctors of Osteopathic Medicine
- MRSA
Methicillin-resistant Staphylococcus aureus
- MA
Massachusetts
- RN
Registered Nurse
- LPN
Licensed Practical Nurse
- TDF
Theoretical Domains Framework
- CFIR
Consolidated Framework for Implementation Research
- ITA
Inductive Thematic Analysis
- BOP
Federal Bureau of Prisons
- EMR
Electronic medical record
Authors’ contributions
R.A.T. and E.D.G. are joint first authors and co-wrote the main manuscript text, E.D.G. prepared Table 1, R.A.T. prepared Fig. 1 and Table 2, R.A.T., E.D.G., and Y.N. conducted interviews, R.A.T., E.D.G., Y.N., A.G.W. and D.M analyzed interviews, All authors read and approved the final manuscript.
Funding
This study is supported by the Tufts Springboard Grant, Stuart B. Levy Center for Integrated Management of Antimicrobial Resistance (CIMAR) at Tufts University.
Availability of data and materials
The codebook generated for this study’s analysis is included in this published article (Additional File 2). The transcripts generated from our interviews during the current study are not publicly available to maintain privacy of the participants. They may be made available from the corresponding author at rebeccatenner@gmail.com on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Tufts University Health Sciences Institutional Review Board (STUDY:00002828: Qualitative Methods to Improve ASP in Carceral Settings). All participants were required to obtain informed consent before participating in any study-related interviews. The study fulfills the principles of the Helsinki Declaration, ensuring respect to all participants and adequate training of all researchers.
Consent for publication
Not applicable.
Competing interests
AGW works as an Infectious Diseases Liaison to the Massachusetts Sheriffs Association The remaining authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rebecca A. Tenner and Emily D. Grussing are joint first authors.
References
- 1.CDC. National infection & death estimates for antimicrobial resistance. CDC. Antimicrobial Resistance Web site. https://www.cdc.gov/drugresistance/national-estimates.html. Published 2021. Accessed.
- 2.Centers for Disease Control aP. Core elements of antibiotic stewardship. Antibiotic Prescribing and Use Web site. https://www.cdc.gov/antibiotic-use/core-elements/index.html. Published 2021. Accessed.
- 3.Cunha CB. Antimicrobial stewardship programs: principles and practice. Med Clin North Am. 2018;102(5):797–803. [DOI] [PubMed] [Google Scholar]
- 4.Reece R, Chace P, Ranucci S. Antimicrobial stewardship in long-term care facilities. R I Med J (2013). 2018;101(5):42–4. [PubMed] [Google Scholar]
- 5.Kang-Brown J, Montagnet C, Heiss J. People in jail and prison in 2020. Vera: Vera Institute of Justice; 2021. [Google Scholar]
- 6.Gates A, Artiga S, Rudowitz R. Health coverage and care for the adult criminal justice-involved population. https://www.kff.org/uninsured/issue-brief/health-coverage-and-care-for-the-adult-criminal-justice-involved-population/. Published 2014. Accessed.
- 7.Trusts P. Jails: inadvertent health care providers. https://www.pewtrusts.org/en/research-and-analysis/reports/2018/01/jails-inadvertent-health-care-providers. Published 2018. Accessed.
- 8.Wurcel AG, London K, Crable EL, Cocchi N, Koutoujian PJ, Winkelman TNA. Medicaid inmate exclusion policy and infectious diseases care for justice-involved populations. Emerg Infect Dis. 2024;30(13):S94-s99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carda-Auten J, Dirosa EA, Grodensky C, et al. Jail health care in the Southeastern United States from entry to release. Milbank Q. 2022;100(3):722–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosen DL, Carda-Auten J, DiRosa E, Travers D. Jail healthcare staffing in the US southeast: a cross-sectional survey. J Gen Intern Med. 2024;39(4):603–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coll SW. The jail health-care crisis. The New Yorker. 2019;95(2):28–28. [Google Scholar]
- 12.Shelton D, Maruca AT, Wright R. Nursing in the American justice system. Arch Psychiatr Nurs. 2020;34(5):304–9. [DOI] [PubMed] [Google Scholar]
- 13.Bick JA. Infection control in jails and prisons. Clin Infect Dis. 2007;45(8):1047–55. [DOI] [PubMed] [Google Scholar]
- 14.Bigham Z, Boms O, Guardado R, Bunn DA, Glenn JE, Wurcel AG. Increased mortality of black incarcerated and hospitalized people: a single state cohort analysis. J Racial Ethn Health Disparities. 2023. [DOI] [PubMed]
- 15.Harris E. Disproportionate death rates reported in US prisons early in the COVID-19 pandemic. JAMA. 2024;331(3):190. [DOI] [PubMed] [Google Scholar]
- 16.Silver IA, Semenza DC, Nedelec JL. Incarceration of youths in an adult correctional facility and risk of premature death. JAMA Netw Open. 2023;6(7):e2321805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tappero JW, Reporter R, Wenger JD, et al. Meningococcal disease in Los Angeles County, California, and among men in the county jails. N Engl J Med. 1996;335(12):833–40. [DOI] [PubMed] [Google Scholar]
- 18.Sanchez GV, Bourne CL, Davidson SL, et al. Pneumococcal disease outbreak at a state prison, Alabama, USA, September 1-October 10, 2018(1). Emerg Infect Dis. 2021;27(7):1949–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Popovich KJ, Thiede SN, Zawitz C, et al. Genomic epidemiology of MRSA during incarceration at a large inner-city jail. Clin Infect Dis. 2021;73(11):e3708–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu YE, LeBoa C, Rodriguez M, et al. COVID-19 Preventive measures in Northern California jails: perceived deficiencies, barriers, and unintended harms. Front Public Health. 2022;10:854343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Beaudry G, Zhong S, Whiting D, Javid B, Frater J, Fazel S. Managing outbreaks of highly contagious diseases in prisons: a systematic review. BMJ Glob Health. 2020;5(11):e003201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hammett TM, Harmon MP, Rhodes W. The burden of infectious disease among inmates of and releases from US correctional facilities, 1997. Am J Public Health. 2002;92(11):1789–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Montoya-Barthelemy AG, Lee CD, Cundiff DR, Smith EB. COVID-19 and the correctional environment: the American prison as a focal point for public health. Am J Prev Med. 2020;58(6):888–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Laryea-Adekimi F, D’Arcy J, Bardelli A, et al. RISE-Vac-Co-production of vaccine education materials with persons living in prison. Emerg Infect Dis. 2024;30(13):S56-s61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bonney LE, Rose JS, Clarke JG, Hebert MR, Rosengard C, Stein M. Correlates of acceptance of a hypothetical gonorrhea vaccine by incarcerated women. Sex Transm Dis. 2007;34(10):778–82. [DOI] [PubMed] [Google Scholar]
- 26.Vicente-Alcalde N, Tuells J, Egoavil CM, Ruescas-Escolano E, Altavilla C, Caballero P. Immunization coverage of inmates in Spanish prisons. Int J Environ Res Public Health. 2020;17(21):8045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Treadwell HM, Nottingham JH. Standing in the gap. Am J Public Health. 2005;95(10):1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Valles SA. Fifty years of U.S. mass incarceration and what it means for bioethics. Hastings Cent Rep. 2023;53(6):25–35. [DOI] [PubMed] [Google Scholar]
- 29.Morrison M. The mass incarceration trauma framework: a conceptual model for understanding trauma among individuals who experience incarceration. Soc Work. 2023;69(1):8–16. [DOI] [PubMed] [Google Scholar]
- 30.Washington L, Bronson J, Timko C, Han B, Blue-Howells J, Finlay AK. Health conditions and treatment utilization among older male veterans incarcerated in prisons. J Gen Intern Med. 2024;39:1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pro G, Camplain R, Lea CH 3rd. The competing effects of racial discrimination and racial identity on the predicted number of days incarcerated in the US: a national profile of Black, Latino/Latina, and American Indian/Alaska Native populations. PLoS One. 2022;17(6):e0268987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Long MJ, LaPlant BN, McCormick JC. Antimicrobial stewardship in the Federal Bureau of Prisons: approaches from the national and local levels. J Am Pharm Assoc (2003). 2017;57(2):241–7. [DOI] [PubMed] [Google Scholar]
- 33.Long D, Edmunds A, Campbell T, Long M. Targeted outpatient fluoroquinolone intervention utilizing an integrated electronic health record in the Bureau of Prisons. Infect Control Hosp Epidemiol. 2020;41(S1):s402–s402. [Google Scholar]
- 34.Szewczyk BR, Tenner R, Grussing E, et al. Establishing a baseline of antibiotic use in Massachusetts jails reveals heterogeneity in quantity of prescriptions and duration of therapy. Antimicrob Steward Healthc Epidemiol. 2023;3(1):e106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Birken SA, Powell BJ, Presseau J, et al. Combined use of the Consolidated Framework for Implementation Research (CFIR) and the Theoretical Domains Framework (TDF): a systematic review. Implement Sci. 2017;12(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sanchez GV, Fleming-Dutra KE, Roberts RM, Hicks LA. Core elements of outpatient antibiotic stewardship. Morb Mortal Wkly Rep. 2016;65(6):1–12. [DOI] [PubMed] [Google Scholar]
- 37.SocioCultural Research Consultants. Dedoose Version 9.0.17, web application for managing, analyzing, and presenting qualitative and mixed method research data. Los Angeles, CA: SocioCultural Research Consultants, LLC. www.dedoose.com. Published 2021. Accessed May 24, 2022.
- 38.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 39.Miles MB HA, Saldaña J. Qualitative data analysis: a methods sourcebook: Sage publications; 2018.
- 40.Charani E, Castro-Sanchez E, Sevdalis N, et al. Understanding the determinants of antimicrobial prescribing within hospitals: the role of “prescribing etiquette.” Clin Infect Dis. 2013;57(2):188–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stach LM, Hedican EB, Herigon JC, Jackson MA, Newland JG. Clinicians’ attitudes towards an antimicrobial stewardship program at a children’s hospital. J Pediatric Infect Dis Soc. 2012;1(3):190–7. [DOI] [PubMed] [Google Scholar]
- 42.Tjilos M, Drainoni ML, Burrowes SAB, et al. A qualitative evaluation of frontline clinician perspectives toward antibiotic stewardship programs. Infect Control Hosp Epidemiol. 2023;44(12):1995–2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Acampora M, Paleologo M, Graffigna G, Barello S. Uncovering influential factors in human antibiotic prescribing: a meta-synthesis study informed by the Theoretical Domains Framework. J Hosp Infect. 2024;144:28–55. [DOI] [PubMed] [Google Scholar]
- 44.Spellberg B, Bartlett JG, Gilbert DN. How to pitch an antibiotic stewardship program to the hospital C-suite. Open forum infectious diseases. 2016;3(4):2016. [DOI] [PMC free article] [PubMed]
- 45.Sloan AML, Dudjak L. Bedside nurses: champions of antimicrobial stewardship. Crit Care Nurse. 2020;40(6):16–22. [DOI] [PubMed] [Google Scholar]
- 46.Waters CD. Pharmacist-driven antimicrobial stewardship program in an institution without infectious diseases physician support. Am J Health Syst Pharm. 2015;72(6):466–8. [DOI] [PubMed] [Google Scholar]
- 47.Kelly C, Templeton M, Allen K, Lohan M. Improving sexual healthcare delivery for men in prison: a nurse-led initiative. J Clin Nurs. 2020;29(13–14):2285–92. [DOI] [PubMed] [Google Scholar]
- 48.Mills L. A prison based nurse-led specialist diabetes service for detained individuals. Eur Diab Nurs. 2014;11(2):53–7. [Google Scholar]
- 49.Papaluca T, McDonald L, Craigie A, et al. Outcomes of treatment for hepatitis C in prisoners using a nurse-led, statewide model of care. J Hepatol. 2019;70(5):839–46. [DOI] [PubMed] [Google Scholar]
- 50.Van Deinse TB, Zielinski MJ, Holliday SB, Rudd BN, Crable EL. The application of implementation science methods in correctional health intervention research: a systematic review. Implement Sci Commun. 2023;4(1):149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Actions to fight antimicrobial resistance. https://www.cdc.gov/drugresistance/actions-to-fight.html. Published 2021. Accessed 11 Mar 2024.
- 52.Laible BR, Nazir J, Assimacopoulos AP, Schut J. Implementation of a pharmacist-led antimicrobial management team in a community teaching hospital: use of pharmacy residents and pharmacy students in a prospective audit and feedback approach. J Pharm Pract. 2010;23(6):531–5. [DOI] [PubMed] [Google Scholar]
- 53.Vento TJ, Veillette JJ, Gelman SS, et al. Implementation of an infectious diseases telehealth consultation and antibiotic stewardship program for 16 small community hospitals. Open Forum Infect Dis. 2021;8(6):ofab168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ewers T, Knobloch MJ, Safdar N. Antimicrobial stewardship: the role of the patient. Curr Treat Options Infect Dis. 2017;9:92–103. [Google Scholar]
- 55.Elias AF, Chaussee MS, McDowell EJ, Huntington MK. Community-based intervention to manage an outbreak of MRSA skin infections in a county jail. J Correct Health Care. 2010;16(3):205–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Malcolm B. The rise of methicillin-resistant Staphylococcus aureus in US correctional populations. J Correct Health Care. 2011;17(3):254–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Webb JA, Czachor JS. MRSA prevention and control in county correctional facilities in Southwestern Ohio. J Correct Health Care. 2009;15(4):268–79. [DOI] [PubMed] [Google Scholar]
- 58.Erfani P, Sandoval RS, Rich KM, et al. “Ask Me Anything”: lessons learned in implementing a COVID-19 vaccine information initiative in Massachusetts jails. Vaccine. 2022;40(22):2981–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Polk RE, Hohmann SF, Medvedev S, Ibrahim O. Benchmarking risk-adjusted adult antibacterial drug use in 70 US academic medical center hospitals. Clin Infect Dis. 2011;53(11):1100–10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material 1. A collection of all interview guides used to guide conversations with each stakeholder group. Interviews are collated into one file
Supplementary Material 2. The initial codebook developed based on 10 interview guides. Guides were randomly selected to represent each participant group and subgroup
Supplementary Material 3. Reflects the consolidated criteria for reporting qualitative research (COREQ) checklist
Data Availability Statement
The codebook generated for this study’s analysis is included in this published article (Additional File 2). The transcripts generated from our interviews during the current study are not publicly available to maintain privacy of the participants. They may be made available from the corresponding author at rebeccatenner@gmail.com on reasonable request.