Abstract
Paradoxical deterioration in patients with tuberculous meningitis is a significant diagnostic and treatment challenge. We present the case of a 55-year-old previously healthy male, human immunodeficiency virus (HIV)-negative, presenting with headache, fever, agitation and slurred speech, who was ultimately diagnosed with tuberculous meningoencephalitis confirmed by cerebrospinal fluid polymerase chain reaction positive for Mycobacterium tuberculosis complex. After initiation of a standard antitubercular therapy combined with glucocorticoids, the patient experienced an initial neurological improvement. However, after 3 months of therapy, he had a major stroke with neurological deterioration, clinically and radiologically attributable to a paradoxical deterioration or an immune reconstruction syndrome as described in HIV-positive patients. Due to the persistence of inflammatory symptoms and radiological evidence of worsening tuberculomas despite ongoing antituberculosis therapy, off-label use of the tumour necrosis factor (TNF) inhibitor infliximab was initiated. The patient received three doses of infliximab at 5 mg/kg at monthly intervals, which led to marked clinical and radiological improvement. Follow-up magnetic resonance imaging showed regression of lesions, and the patient was eventually discharged with a significant recovery of motor and speech functions. This case underscores the potential of TNF inhibitors in managing severe cases of paradoxical deterioration in patients with tuberculous meningitis, challenging existing treatment paradigms and suggesting a need for further research into the pathophysiology and treatment of this condition.
LEARNING POINTS
Patients with tuberculous meningitis may experience a paradoxical deterioration in spite of correct antituberculosis treatment.
The paradoxical deterioration may have a severe clinical presentation, requiring high vigilance and consideration of treatment escalation.
Here we report that off-label administration of tumour necrosis factor-alpha blocker infliximab induced a significant clinical and radiological improvement in a severe case of paradoxical deterioration in a patient with tuberculous meningitis, suggesting its potential as a treatment when standard therapies fail.
Keywords: Central nervous system tuberculosis, immune reconstitution inflammatory syndrome, IRIS, neurological complications, infliximab
INTRODUCTION
Paradoxical reaction with deterioration of the clinical state has been reported in about one third of correctly treated patients with tuberculous meningitis[1]. This paradoxical reaction is similar to the immune reconstitution syndrome (IRIS) described in human immunodeficiency virus (HIV)-positive patients, where an excessive inflammatory reaction leads to a temporary worsening of an existing or not yet adequately treated opportunistic infection. IRIS particularly occurs in patients with HIV who have a low CD4 count and have recently started antiretroviral therapy. A similar reaction is also observed in patients with mycobacterial infections, such as tuberculosis (TB), even without immunosuppression. The exact pathogenesis of the paradoxical reaction and IRIS is not entirely clear, but it is assumed that the improvement of immune function leads to an excessive reaction of the immune system with hyperinflammation. Both are characterized by paradoxical worsening symptoms of a treated patient, as in our case. Neurological paradoxical reaction in patients with tuberculous meningitis presents with fever, worsening meningitis and/or features of raised intracranial pressure.
CASE DESCRIPTION
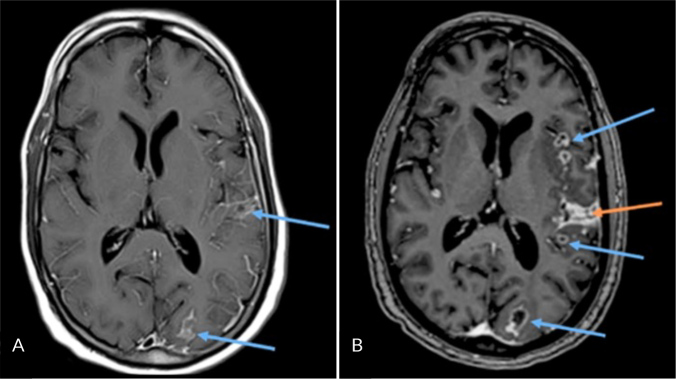
A 55-year-old previously healthy male, with a history of regular alcohol consumption, presented with progressive headache, agitation, disorientation, slurred speech, fever, and nausea for the last 5 days. Upon admission to the emergency ward, the patient was agitated, disoriented, somnolent (Glasgow coma scale: 12) with slurred speech and subfebrile. Neurological examination showed no focal neurological deficits and no signs of meningism. Due to his unclear clinical state with reduced vigilance, the patient was admitted to the intensive care unit. Laboratory analysis revealed a normal blood leukocyte counts of 8.0 ×109/l (normal range: 3.9 – 10.2 ×109/l) and normal C-reactive protein level (<5 mg/l). The remaining blood test results were normal including normal liver function tests. With a negative ethanol level and normal ammonia levels, there were no indications of hepatic encephalopathy. Cranial computed tomography (CT) scan provided no significant findings. Lumbar puncture revealed a pleocytosis with predominance of mononuclear cells and increased protein in cerebrospinal fluid (CSF) (Table 1). Due to suspected meningoencephalitis, empirical therapy with intravenous (IV) ceftriaxone 2 g two times a day, and IV acyclovir 1 g three times a day, was initiated, until the receipt of microbiological results. The meningitis/encephalitis multiplex polymerase chain reaction (PCR) and general bacteriology from the CSF were negative. Considering the clinical picture, the epidemiological risk and the CSF profile suggestive of tuberculous meningitis, empirical therapy with Rimstar® (rifampicin, isoniazid, pyrazinamide, ethambutol) was initiated and continued upon confirmation of CSF PCR positive for Mycobacterium tuberculosis complex. Mycobacterial culture was negative. Additionally, vitamin B6 doses were combined with dexamethasone. Chest CT scan revealed no signs of pulmonary tuberculosis. HIV serology was negative. On the third day of hospitalization at the intensive care unit, while still in a clinical state of hyperactive delirium with agitation and confusion, the patient developed anisocoria (right > left) without other focal neurological abnormalities. Cerebral magnetic resonance imaging (cMRI) showed a swollen left hemisphere in the context of tuberculous meningoencephalitis, with focal pachymeningeal and leptomeningeal enhancements (Fig. 1A). Due to the lack of clinical improvement (persistent agitation and confusion), the dexamethasone dose was increased from 24 to 32 mg per day, leading to an improvement in the patient’s condition over the next two weeks. The patient was then transferred to a rehabilitation unit. The restlessness and confusion disappeared, the motor functions of all four extremities and his gait were unremarkable and the anisocoria disappeared.
Table 1.
Cerebrospinal fluid analysis at admission.
| Liquor visualization | Result | Reference range |
|---|---|---|
| Colour | Colourless | Colourless |
| Appearance | Clear | Clear |
| Cell count/differentiation | ||
| Total cell count | 161 | <5 |
| Leukocytes (x106 /l) | 158 | <5 |
| Mononuclear cells (%) | 84.8 | - |
| Polymorphonuclear cells (%) | 15.2 | - |
| Erythrocytes (x106 /l) | 1000 | <5 |
| Clinical Chemistry Analyses | ||
| Glucose (mmol/l) | 1.9 | 2–4 |
| Lactate (mmol/l) | 6.2 | 1.2–2.1 |
| Protein (mg/l) | 3143 | 200–400 |
Figure 1.
A) Cerebral magnetic resonance imaging (cMRI) (T1 Blade after contrast administration) on the third day of hospitalization showing pachymeningeal enhancement (arrows) without amalgamation of cells; B) cMRI (T1-MPRAGE after contrast administration) three months after admission under continuing tuberculostatic therapy: progressive pachymeningeal enhancement (red arrow) and tuberculomas (blue arrow).
During rehabilitation, still under the tuberculostatic therapy and 3 months after the initial presentation, the patient had a subacute ischemic stroke due to acute occlusion of the arteria cerebri media on the left side, resulting in severe aphasia, dysarthria, and right-sided facio-brachio-crural hemisyndrome (with a National Institutes of Health stroke scale score of 6 points). An interventional treatment for the acute proximal M2 occlusion followed, with a thrombectomy using a stent retriever. Repeated cMRI revealed a progressive finding with numerous in size-increasing tuberculomas (Fig. 1B). Over the course of the next few days, the patient developed severe neurological complications, including an epileptic seizure, which was reflected in the electroencephalogram (EEG) as a continuous focal pattern centro-parietal to temporal, predominantly on the left side. Accordingly, antiepileptic therapy with levetiracetam was initiated.
We interpreted the situation as a paradoxical reaction/IRIS and initiated an off-label treatment with infliximab 5 mg/kg (total 3 doses at monthly intervals), which led to clinical improvement. Upon discharge from rehabilitation, the patient regained the ability to walk independently. Thanks to intensive speech therapy, he was able to regain articulation, although he still experienced some word-finding difficulties. A cMRI at 8 months follow-up after the initial diagnosis, showed that the lesions had regressed (Fig. 2). Twelve months after the initial presentation, the antituberculosis treatment was discontinued; the corticosteroid therapy tapered and ended after a total of 16 months.
Figure 2.
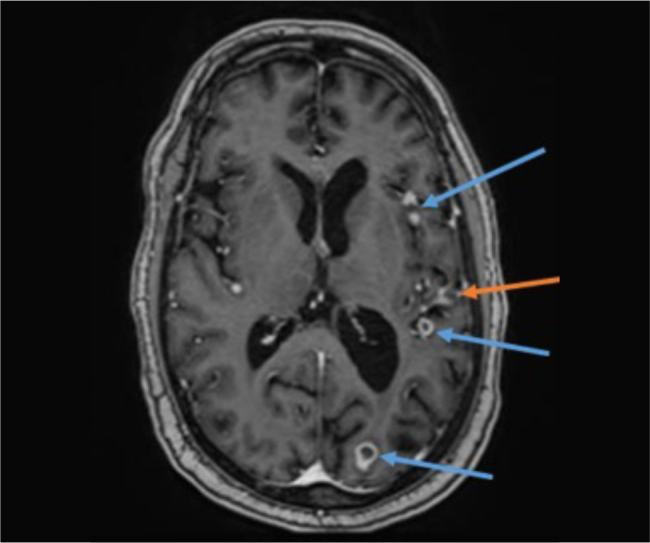
Cerebral magnetic resonance imaging (T1-MPRAGE after contrast medium administration) at 8 months after initial presentation. Size regression of the pachymeningeal enhancement (red) and the tuberculomas (blue).
DISCUSSION
CNS tuberculosis and IRIS are rare disease entities, which are associated with high mortality. IRIS occurs in 1–5% of all patients with tuberculosis and in 10% of patients with acquired immunodeficiency syndrome (AIDS)-related tuberculosis. Both CNS-TB and IRIS may lead to severe neurological complications with lasting functional impairment. IRIS commonly presents with persistent fever, increased intracranial pressure as well as arthritis and lymphadenopathy, depending on the location of tuberculosis. Neuroradiologically, signs of hydrocephalus are found in 75% of cases, basal-enhanced contrast enhancement in 38% of cases, and ischemia in 15–30% of cases. According to Singh et al[1], who followed 141 patients with tuberculous meningitis, paradoxical reaction occurs in about one third of the patients, more commonly in females, HIV-positive patients and shorter duration of illness. Differentiating paradoxical reaction with deterioration of the clinical state from an IRIS is not easy as both involve an exaggerated reaction of the immune system to mycobacterial antigens. IRIS occurs typically in patients with newly treated HIV infection. According to Marais et al, the pathophysiology of IRIS involves a complex interplay of high mycobacterial antigen load, neutrophil activation, cytokine dysregulation, and monocyte activation, leading to severe CNS inflammation[2].
Blockade of tumour necrosis factor (TNF) alpha seems to be an effective therapy of IRIS. TNF-α plays a central role in the inflammatory response[3]. Studies have indicated that tuberculostatic therapy was more effective when the host immune response was inhibited by adjunctive anti-TNF therapy. Moreover, discontinuing infliximab (a monoclonal antibody against TNF-α) after a diagnosis of tuberculosis led to a paradoxical reaction or clinical deterioration, which is why an adjunctive infliximab therapy was first initiated in 2008 in a patient with progressive CNS tuberculosis[4]. Under this treatment, an improvement in neurology was observed. Since then, similar cases have been published[5]. All patients tolerated the therapy well with rapid clinical improvement, which was also confirmed radiologically. Various regimens and dosages ranging from 2.5 to 10 mg/kg were used.
Our case is interesting due to the rather late development of the paradoxical reaction (3 months after diagnosis tuberculous meningitis) in a previously healthy patient without immunosuppression, under tapering the glucocorticoid therapy. In our patient the overreaction of the immune system led to significant progression of brain damage with a major stroke and severe neurological complications. The neurological deterioration persisted even after reintroduction of the high doses of glucocorticosteroids, which is why an immune-related paradoxical reaction was assumed and the off-label therapy with infliximab started, leading to a major improvement of the neurological condition. It is difficult to speculate whether our patient developed an IRIS or a paradoxical reaction. Our case corresponds to the series of paradoxical reactions in tuberculous meningitis reported by Singh et al. They observed the majority of paradoxical reactions to occur within 3 months after beginning of treatment[1]. Robert et al. reported that in HIV-negative patients with tuberculous meningitis, IRIS occurred at a median time of 2 months (interquartile range, 1–3 months) after starting antituberculosis treatment[6]. His study highlights that CNS-IRIS following tuberculous meningitis in non-HIV patients may occur frequently and in a severe form. The meningeal enhancement on brain MRI at diagnosis of tuberculous meningitis poses a significant risk factor for CNS-IRIS – which is also the case in our patient. The authors suggest that the pathogenesis of IRIS in non-HIV patients may be driven by an exaggerated immune response to the mycobacterial antigens released during effective antituberculosis therapy. This response may be amplified in patients with pre-existing meningeal inflammation (shown by MRI findings). Nevertheless, whether paradoxical reaction or CNS-IRIS, both conditions require high level of clinical vigilance and introduction or escalation of immunosuppressive treatment.
Our patient was generally healthy prior to the diagnosis and his alcohol consumption was moderate. Although he has a migration background, he has lived many years in Switzerland in good socioeconomic conditions and he did not have a relevant history of travel in the recent months/years. Therefore, we cannot explain why he developed tuberculous meningitis in the first place.
In summary, we present a case of severe paradoxical reaction with neurological deterioration occurring 3 months after the diagnosis of tuberculous meningitis in an HIV-negative patient, who did not respond adequately to glucocorticosteroids, necessitating the use of infliximab to ameliorate the condition. Infliximab appears to be a safe and effective off-label therapeutic option in patients presenting with worsening clinical and imaging signs of TB-IRIS despite high-dose glucocorticosteroid therapy.
Footnotes
Conflicts of Interests: The Authors declare that there are no competing interests.
Patient Consent: Patient consent was obtained. The patient agrees to the publication of information about him for a scientific publication, he knows that his name will not be mentioned but understands that complete anonymity cannot be guaranteed.
REFERENCES
- 1.Singh AK, Malhotra HS, Garg RK, Jain A, Kumar N, Kohli N, et al. Paradoxical reaction in tuberculous meningitis: presentation, predictors and impact on prognosis. BMC Infect Dis. 2016;16:306. doi: 10.1186/s12879-016-1625-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marais S, Wilkinson KA, Lesosky M, Coussens AK, Deffur A, Pepper DJ, et al. Neutrophil-associated central nervous system inflammation in tuberculous meningitis immune reconstitution inflammatory syndrome. Clin Infect Dis. 2014;59:1638–1647. doi: 10.1093/cid/ciu641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Donald PR, Schoeman JF, Beyers N, Nel ED, Carlini SM, Olsen KD, et al. Concentrations of interferon gamma, tumor necrosis factor alpha, and interleukin-1 beta in the cerebrospinal fluid of children treated for tuberculous meningitis. Clin Infect Dis. 1995;21:924–929. doi: 10.1093/clinids/21.4.924. [DOI] [PubMed] [Google Scholar]
- 4.Blackmore TK, Manning L, Taylor WJ, Wallis RS. Therapeutic use of infliximab in tuberculosis to control severe paradoxical reaction of the brain and lymph nodes. Clin Infect Dis. 2008;47:e83–5. doi: 10.1086/592695. [DOI] [PubMed] [Google Scholar]
- 5.Marais BJ, Cheong E, Fernando S, Daniel S, Watts MR, Berglund LJ, et al. Use of Infliximab to Treat Paradoxical Tuberculous Meningitis Reactions. Open Forum Infect Dis. 2020;8:ofaa604. doi: 10.1093/ofid/ofaa604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robert M, Mageau A, Gaudemer A, Thy M, Peiffer Smadja N, de Lastours V, et al. Incidence, risk factors and treatment of central nervous system immune reconstitution inflammatory syndrome in non-HIV patients with tuberculous meningitis: a multicentre observational study. Intern Med J. 2024;54:802–808. doi: 10.1111/imj.16295. [DOI] [PubMed] [Google Scholar]