Abstract
Background
Computed tomography (CT) scans play a crucial role in emergency surgical care, serving both diagnostic and prognostic functions. They significantly contribute to timely and effective patient care. This study aims to compare abdominal CT scan reports prepared by locally employed radiologists with those from outsourced radiology reporting services for patients presenting with acute surgical conditions. Additionally, the study evaluates how different reporting styles, such as free-text versus structured formats, influence the overall quality of the reports.
Methods
The study was conducted in the general surgery unit of North Manchester General Hospital, Manchester, a district general hospital in North West England. Patients admitted through the accident and emergency (A&E) under the general surgery team who underwent abdominal CT scans between August 2023 and October 2023 were included. Trauma patients and those who received non-abdominal CT scans were excluded. Local radiology reports were compared to outsourced reports using statistical analysis. The clarity and comprehensiveness of the reports were carefully evaluated, and the impact of free-text versus structured reporting formats was also considered.
Results
A total of 192 patients were included in the study, with a median age of 59 years. Compared to locally reported scans, outsourced radiology reports frequently omitted commentary on key anatomical structures, including the biliary system, spleen, kidneys, lymph nodes, mesentery and peritoneum, vasculature, bones and soft tissues, and lung bases. Reports using a structured format provided more thorough commentary on the spleen, adrenal glands, mesentery and peritoneum, and bones and soft tissues compared to free-text reports.
Conclusion
Outsourced radiology reports significantly underreported important abdominal anatomical structures. Free-text reporting was associated with significant omissions in abdominal anatomical structures, which could negatively affect clinical decision-making and management plans. Further studies are recommended to evaluate the comprehensiveness of outsourced radiology reporting and to ensure standardization in reporting, ultimately providing patients with high-quality emergency care.
Keywords: ct (computed tomography) imaging, free-text report, outsourced radiology, radiology reporting, structured report
Introduction
Computed tomography (CT) scans play a crucial role in emergency surgical care. They are used in the investigation of acute abdominal pain, alongside physical examination and laboratory tests, to determine the most likely diagnosis [1]. Computed tomography scans visualise most abdominal and pelvic structures, enabling the detection of acute surgical pathologies [1]. They also contribute to prompt decision-making and appropriate management, which improves patient outcomes in acute surgical pathologies [2].
With the introduction of teleradiology in the mid-1990s, the interpretation of diagnostic scan images at geographically distant sites became possible [3]. Technological advancements and the power of market forces have driven the prevalence and availability of such practices [3]. Consequently, radiology reports are not necessarily written by locally employed radiologists. The images can be digitally transferred and interpreted by radiologists working remotely [3].
In 2023, a census published by the Royal College of Radiologists (RCR) reported that over 83% of radiology departments in the United Kingdom (UK) were outsourcing radiology reports to external companies [4]. This is due to a considerable discrepancy between service demand and the availability of the local workforce. In the same year, the combined cost of outsourcing, insourcing, and ad hoc locum staffing to meet the NHS's high demand was reported to be £276 million [4].
Reports by locally employed radiologists offer the opportunity for direct communication between clinical and reporting teams. Additionally, locally employed radiologists have direct access to patients' records within the same institution, a resource not available to outsourced reporting services [5]. Consequently, concerns about the quality of outsourced radiology reports have been frequently raised [5].
With the growing availability of electronic patient records, patients have increased access to their radiology reports [6]. Therefore, a standardised writing style reflecting the needs of both patients and referring clinicians as the primary end-readers should be considered. Two commonly used reporting styles are structured and free-text formats. Structured reports are typically organised based on anatomical organs and body systems, often written as a list, while free-text reports document findings in continuous prose [7]. Structured reports enable easy extraction and assimilation of information, whilst free-text reports are often more concise [7]. Further studies are needed to identify the optimal format for radiology reports [7].
This study aims to compare abdominal CT scan reports composed by locally employed radiologists to those composed by an outsourced radiology reporting service for patients admitted with acute surgical pathologies. This study also assesses the impact of reporting style (free-text versus structured format) on the comprehensiveness of abdominal CT scan reports.
This article was previously presented as a meeting abstract at the 27th Association of Upper Gastrointestinal Surgery of Great Britain and Ireland (AUGIS) Annual Scientific Meeting on September 12, 2024.
Materials and methods
Study design and patient selection
The study was conducted as a retrospective cohort study. The Strengthening the Reporting of Cohort Studies in Surgery (STROCSS) guidelines for observational research were followed [8]. A predefined protocol, in accordance with local Clinical Governance Unit policies, was implemented. As the study was retrospective, contained non-identifiable data, and did not meet the NHS Health Research Authority criteria for ethical review, ethical approval and patient consent were not required [9]. The study was undertaken in the general surgery unit of North Manchester General Hospital, Manchester, a district general hospital in North West England. Data were collected from the hospital’s electronic healthcare records between August 2023 and October 2023. All patients aged 18 years or older who underwent emergency abdominal CT scans were included. Patients who underwent abdominal CT for trauma, non-emergency reasons, or other imaging modalities such as ultrasound, magnetic resonance imaging (MRI), or non-abdominal CT scans were excluded.
Comparisons and outcomes
The primary outcome compared abdominal CT reports from locally employed radiologists to outsourced reports for patients with acute abdominal pathologies. We analysed and compared the comments on anatomical organs and structures, documented within the reports, between the two groups. The organs assessed included the liver, biliary system, spleen, pancreas, adrenal glands, kidneys, gastrointestinal tract, lymph nodes, vasculature, mesentery, peritoneum, bones, soft tissues, and lung bases. The study also evaluated the impact of free-text and structured reporting formats on report comprehensiveness.
Data collection
An electronic data collection proforma was developed to gather the necessary data for the study. Patient demographics, including age and gender, were recorded. The indication for the CT scan, CT results, including incidental findings and systematic commentary on abdominal anatomy, and the format of the report were also recorded.
Data synthesis and statistical analyses
All categorical variables were summarised using absolute and relative frequencies. Continuous variables were summarised using the median (minimum-maximum). Logistic regression was used to compare categorical variables. Regression coefficients (B), standard errors (SE), odds ratios (OR), 95% confidence interval of the odds ratios (95% CI), and the p-values (p) were calculated. All statistical analyses were performed with a 95% confidence interval. Statistical significance was defined as a p-value of less than 0.05. The data analyses were conducted using IBM SPSS Statistics software, version 29.0.1.0 (IBM Corp., Armonk, NY).
Results
Patient characteristics
A total of 192 abdominal CT scan reports identified between August 2023 and October 2023 met the inclusion criteria. Of these scans, 109 (56.8%) were performed on male patients. The median age at the time of the CT scan was 59 years (range: 18-97 years). Locally employed radiologists reported 113 scans (58.9%), while 79 scans (41.1%) were reported by outsourced radiology services. Incidental findings were noted in 36 scans (18.8%). The most common indication for CT was suspected appendicitis (30 (15.6%)), followed by abdominal pain (28 (14.6%)). Three scans (1.6%) did not have a documented indication. No abnormalities were detected in 42 scans (21.9%), and appendicitis was diagnosed in 21 scans (10.9%). The free-text reporting format was used in 149 scans (77.6%) (Table 1).
Table 1. Baseline characteristics of patients and abdominal CT scan reports.
The table summarises patient demographics, reporting formats, and the personnel responsible for interpreting the scans, as well as the indications for abdominal CT and the findings from the scans. Frequencies and percentages are provided for each category. Additionally, the table details the number and percentage of reports that included comments on key anatomical structures, such as the liver, biliary tree, spleen, pancreas, and others. It also indicates the number of incidental findings recorded.
SD: standard deviation; CT: computed tomography; PR: per rectal
| Patient and report characteristics | Total number = 192 |
| Age (years) | |
| Mean ± SD | 56.27 ± 17.67 |
| Median (range) | 59 (18-97) |
| Sex | |
| Female | 109 (56.8%) |
| Male | 83 (43.2%) |
| Reporting format | |
| Free-text | 149 (77.6%) |
| Structured | 43 (22.4%) |
| Reporting personnel | |
| Locally employed radiologists | 113 (58.9%) |
| Outsourced reporting service | 79 (41.1%) |
| Indication for CT scan | |
| Appendicitis | 30 (15.6%) |
| Abdominal pain | 28 (14.6%) |
| Bowel obstruction | 27 (14.1%) |
| Gallbladder and biliary system pathology | 18 (9.4%) |
| Abdominal wall hernias (complicated and uncomplicated) | 16 (8.3%) |
| PR bleed | 10 (5.2%) |
| Post-op collection | 10 (5.2%) |
| Malignancy | 9 (4.7%) |
| Diverticular disease (complicated and uncomplicated) | 9 (4.7%) |
| No specified indication | 3 (1.6%) |
| Others | 32 (16.6%) |
| CT results | |
| No abnormality detected | 42 (21.9%) |
| Acute appendicitis | 21 (10.9%) |
| Gallbladder and biliary system pathology | 18 (9.4%) |
| Diverticular disease (complicated and uncomplicated) | 12 (6.3%) |
| Inconclusive results | 15 (7.8%) |
| Abdominal wall hernias (complicated and uncomplicated) | 16 (8.3%) |
| Bowel obstruction (small and large bowel) | 16 (8.3%) |
| Pancreatitis | 7 (3.6%) |
| Colitis | 8 (4.2%) |
| Malignancy | 5 (2.6%) |
| Others | 32 (16.6%) |
| Anatomical structures commented on | |
| Liver | 172 (89.6%) |
| Biliary system | 173 (90.1%) |
| Spleen | 167 (87.0%) |
| Pancreas | 170 (88.5%) |
| Adrenals | 166 (86.5%) |
| Kidneys | 170 (88.5%) |
| Gastrointestinal tract | 176 (91.7%) |
| Lymph nodes | 147 (76.6%) |
| Mesentery and peritoneum | 56 (29.2%) |
| Vasculature | 87 (45.3%) |
| Bones and soft tissue | 164 (85.4%) |
| Lung bases | 168 (87.5%) |
| Incidental findings | 36 (18.8%) |
Comparison of abdominal CT scan reports: outsourced vs. locally employed radiologists
This study found that the outsourced radiology service was significantly less likely to report on several important intra-abdominal structures when compared to the locally employed radiologists. These structures included the biliary system (OR = 0.396, p = 0.046), spleen (OR = 0.414, p = 0.044), kidneys (OR = 0.354, p = 0.027), gastrointestinal tract (OR = 0.286, p = 0.026), lymph nodes (OR = 0.412, p = 0.011), mesentery and peritoneum (OR = 0.364, p = 0.004), vasculature (OR = 0.381, p = 0.002), bones and soft tissues (OR = 0.273, p = 0.003), as well as lung bases (OR = 0.300, p = 0.009).
While the outsourced service was less likely to comment on the pancreas (OR = 0.439, p = 0.075) and adrenals (OR = 0.460, p = 0.070), these differences were not statistically significant. However, there was no significant difference in reporting on the liver (OR = 0.839, p = 0.712) or other incidental findings (OR = 1.181, p = 0.656) (Table 2).
Table 2. Logistic regression analysis of abdominal CT reports: locally employed vs. outsourced radiologists.
This table shows the logistic regression analysis results comparing the likelihood of various abdominal structures being reported on by locally employed radiologists vs. outsourced radiology services. The table includes the number of scans with comments on each anatomical structure based on reporting personnel, logistic regression coefficients (B), standard errors (SE), odds ratios (OR), 95% confidence intervals (CI), and p-values. Statistically significant differences are indicated by p-values less than 0.05.
N: number; B: regression coefficient; SE: standard error; OR: odds ratio; CI: confidence interval; GIT: gastrointestinal tract
| Anatomical structures commented on | Locally employed (N=113) | Outsourced reporting (N=79) | B | SE | OR (95% CI) | p-value |
| Liver | 102 (90.3%) | 70 (88.6%) | -0.176 | 0.476 | 0.839 (0.330 - 2.130) | 0.712 |
| Biliary system | 106 (93.8%) | 67 (84.8%) | -0.998 | 0.501 | 0.369 (0.138 - 0.983) | 0.046 |
| Spleen | 103 (91.2%) | 64 (81%) | -0.881 | 0.438 | 0.414 (0.175 - 0.978) | 0.044 |
| Pancreas | 104 (92%) | 66 (83.5%) | -0.822 | 0.461 | 0.439 (0.178 - 1.085) | 0.075 |
| Adrenals | 102 (90.3%) | 64 (81%) | -0.776 | 0.428 | 0.460 (0.199 - 1.064) | 0.070 |
| Kidneys | 105 (92.9%) | 65 (82.3%) | -1.039 | 0.470 | 0.354 (0.141 - 0.890) | 0.027 |
| GIT | 108 (95.6%) | 68 (86.1%) | -1.251 | 0.561 | 0.286 (0.095 - 0.860) | 0.026 |
| Lymph nodes | 94 (83.2%) | 53 (67.1%) | -0.887 | 0.347 | 0.412 (0.209 - 0.814) | 0.011 |
| Mesentery and peritoneum | 42 (37.2%) | 14 (17.7%) | -1.010 | 0.353 | 0.364 (0.182 - 0.727) | 0.004 |
| Vasculature | 62 (54.9%) | 25 (31.6%) | -0.965 | 0.307 | 0.381 (0.209-0.695) | 0.002 |
| Bones and soft tissues | 104 (92%) | 60 (75.9%) | -1.297 | 0.436 | 0.273 (0.116 - 0.642) | 0.003 |
| Lung bases | 105 (92.9%) | 63 (79.7%) | -1.204 | 0.461 | 0.300 (0.121 - 0.741) | 0.009 |
| Incidental findings | 20 (17.7%) | 16 (20.3%) | 0.166 | 0.373 | 1.181 (0.569 - 2.453) | 0.656 |
Comparison of abdominal CT scan reports: free-text vs. structured formats
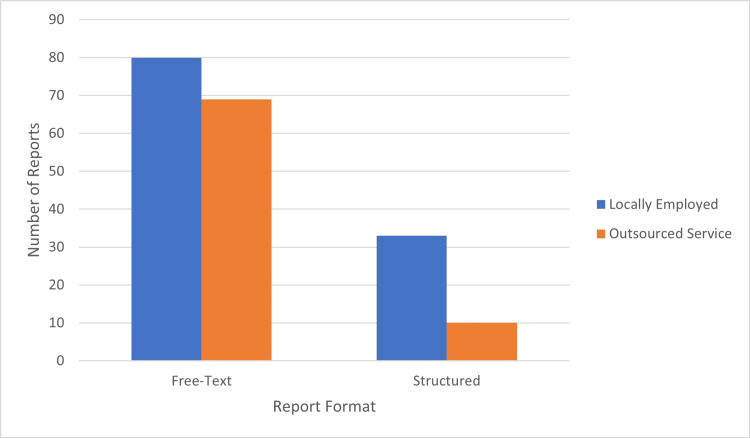
This study compared abdominal CT reports written in free-text and structured formats using logistic regression analysis. Of the structured reports, 33 (76.7%) were written by locally employed radiologists, while 10 (23.3%) were written by the outsourced radiology reporting service. Conversely, similar proportions of free-text reports were generated by locally employed radiologists (80 (53.7%)) and the outsourced service (69 (46.3%)) (Figure 1).
Figure 1. Comparison of reporting personnel by report format.
The bar chart illustrates the distribution of abdominal CT scan reports based on the personnel responsible for interpreting the reports (locally employed radiologists vs. outsourced radiology services) and the format used (free-text vs. structured), where blue bars represent locally employed radiologists and orange bars represent outsourced reporting services, with the y-axis showing the count of reports and the x-axis distinguishing between free-text and structured formats.
Structured reports were more likely to document most intra-abdominal structures, including incidental findings, compared to free-text reports. However, some of these findings were not statistically significant. The structured reports were significantly more likely to include comments on the following structures: spleen (OR = 8.064, p = 0.044), adrenals (OR = 8.468, p = 0.039), mesentery and peritoneum (OR = 1.949, p = 0.057) and bones and soft tissues (OR = 9.295, p = 0.031). While trends suggested that structured reports were more likely to include comments on the biliary system, pancreas, vasculature, and incidental findings, these differences were not statistically significant. Additionally, structured reports consistently included comments on the liver, kidneys, gastrointestinal tract, lymph nodes, and lung bases, leading to extremely high ORs without calculable confidence intervals (Table 3).
Table 3. Logistic regression analysis of abdominal CT report format: free-text vs. structured formats.
This table presents the results of a logistic regression analysis comparing abdominal CT scan reports written in free-text versus structured formats. It includes counts of reports with and without comments on key intra-abdominal structures for both formats. The analysis provides regression coefficients (B), standard errors (SE), odds ratios (OR), and 95% confidence intervals (95% CI) for each structure (some of which were incalculable), alongside p-values indicating statistical significance. Statistically significant values are indicated with p < 0.05.
N: number; B: regression coefficient; SE: standard error; OR: odds ratio; CI: confidence interval; GIT: gastrointestinal tract
| Anatomical structures commented on | Free-text (N = 149) | Structured (N = 43) | B | SE | OR (95% CI) | p-value |
| Liver | 129 (86.6%) | 43 (100%) | 19.339 | 6129.370 | 250461215.946 (incalculable) | 0.997 |
| Biliary system | 131 (87.9%) | 42 (97.7%) | 1.753 | 1.043 | 5.771 (0.748 - 44.536) | 0.093 |
| Spleen | 125 (83.9%) | 42 (97.7%) | 2.087 | 1.036 | 8.064 (1.058 - 61.443) | 0.044 |
| Pancreas | 128 (85.9%) | 42 (97.7%) | 1.930 | 1.039 | 6.891 (0.899 - 52.789) | 0.063 |
| Adrenals | 124 (83.2%) | 42 (97.7%) | 2.136 | 1.035 | 8.468 (1.113 - 64.421) | 0.039 |
| Kidneys | 127 (85.2%) | 43 (100%) | 19.450 | 6129.370 | 279846035.769 (incalculable) | 0.997 |
| GIT | 133 (89.3%) | 43 (100%) | 19.085 | 6129.370 | 194342838.238 (incalculable) | 0.998 |
| Lymph nodes | 104 (69.8%) | 43 (100%) | 20.365 | 6129.370 | 699003537.772 (incalculable) | 0.997 |
| Mesentery and peritoneum | 32 (21.5%) | 24 (55.8%) | 1.530 | 0.366 | 4.618 (2.253 - 9.467) | 0.000 |
| Vasculature | 62 (41.6%) | 25 (58.1%) | 0.667 | 0.351 | 1.949 (0.980 - 3.877) | 0.057 |
| Bones and soft tissues | 122 (81.9%) | 42 (97.7%) | 2.229 | 1.034 | 9.295 (1.225 - 70.526) | 0.031 |
| Lung bases | 125 (83.9%) | 43 (100%) | 19.553 | 6129.370 | 310171169.827 (incalculable) | 0.997 |
| Incidental findings | 24 (16.1%) | 12 (27.9%) | 0.701 | 0.407 | 2.016 (0.909 - 4.472) | 0.085 |
Discussion
Outsourced radiology reporting has become a valid resource utilised worldwide [5]. It enables efficient reporting of time-critical scans performed in emergency care [5]. Previous studies have shown that outsourced reporting services handle a higher volume of scans compared to local radiology reporting services [10]. However, there is an increased risk of diagnostic errors, given the lack of direct communication between the outsourced radiologist and the clinical team [5].
In this study, emergency abdominal CT scan reports from the outsourced radiology reporting service were found to underreport critical information about various intra-abdominal organs. Specifically, outsourced reports frequently omitted comments on the biliary system, spleen, kidneys, lymph nodes, mesentery, peritoneum, vasculature, bones, soft tissues, and lung bases. As a result, this raises significant concerns regarding the possible omission of important scan findings. These findings align with those of Hohmann et al., who reported similar concerns in their prospective study at University College London Hospitals, where the rate of diagnostic errors in outsourced scan reports was 0.8% [11]. In 2023, Çetin et al. demonstrated comparable concerns regarding the diagnostic accuracy of outsourced thoracic CT scan reports in a Turkish cohort of patients [5].
In a 2018 survey, Graham et al. highlighted that local clinical teams frequently distrust the precision of outsourced CT scan reports [12]. More importantly, they highlighted that report clarifications and reviews were undertaken by locally employed radiologists when requested [12]. This contributes to a higher workload for local radiology teams, resulting in work duplication and inefficiencies in patient care [12]. Conversely, Olofsson et al. reported that fewer scans reported by locally employed radiologists needed reassessment compared to outsourced radiology services [13]. They recommended that clear communication with the outsourced radiology team is needed to guarantee a cost-effective service, shorter reporting time, and efficient management of patients [13]. In contrast, Storjohann et al. analysed 7761 out-of-hours CT scan reports, over 21 months, reported by locally employed and outsourced radiologists [14]. They concluded that there were no significant discrepancies in the accuracy of scan reports between the two groups [14].
This study also compared the effect of structured and free-text reporting formats on report comprehensiveness. According to the analyses, the free-text format was found to be more likely to underreport some of the important anatomical structures seen in abdominal CT scans. Notable examples of frequently omitted structures include the spleen, adrenal glands, mesentery and peritoneum, and bones and soft tissues. Several studies have compared structured and free-text reporting formats. Lam et al. described free-text CT reports as being more ambiguous compared to structured reports [15]. McFarland et al. and Dimarco et al. noted that the structured reporting style was superior and less prone to errors than the free-text style [7,16]. Errors in the free-text style may lead to misdiagnosis and unnecessary intervention [7,16]. Similarly, Jorg et al. acknowledged that structured reports are more concise [17]. However, they highlighted that the structured format is limiting when unexpected findings are uncovered [17]. Thus, a free-text format facilitates a more expansive description of uncertain findings [17].
The European Society of Radiology recommended the structured reporting format in Good Practice for Radiological Reporting in 2011 [18]. They highlighted that the structured format prompts radiologists to complete all required fields [18]. It is also suggested that the structured format is more time-efficient and enables easier retrieval of data for audit and research purposes [18].
This study has several limitations. Its retrospective design is a potential source of inherent biases, and being conducted at a single centre further increases the risk of these biases. Additionally, it was limited to abdominal CT scans, which may reduce the generalisability of findings to other imaging modalities. Furthermore, the CT images were not re-evaluated by independent radiologists, which could have helped identify potential omissions in the scan reports. Lastly, the relatively small sample size may also limit the strength of the conclusions drawn.
Conclusions
In conclusion, this study highlights that the outsourced radiology service significantly underreported many key elements of abdominal CT scans when compared to the local radiology service. This underreporting can complicate the assessment and management of acute surgical patients. Additionally, the free-text reporting format was also found to omit critical details of abdominal CT scans. Further studies auditing a broader range of outsourced radiology services are thus recommended. This is essential to ensure that treating clinicians receive high-quality reports, enabling effective and efficient emergency surgical care.
Disclosures
Human subjects: Consent for treatment and open access publication was obtained or waived by all participants in this study.
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Author Contributions
Concept and design: Emmanuel Obayi, Mohammed Barghash, Moustafa Mansour
Acquisition, analysis, or interpretation of data: Emmanuel Obayi, Mohammed Barghash, Ye H. Aung, Zoe Furber, Shua Haq, Katie McComb
Drafting of the manuscript: Emmanuel Obayi, Mohammed Barghash, Ye H. Aung, Zoe Furber, Shua Haq, Katie McComb
Critical review of the manuscript for important intellectual content: Emmanuel Obayi, Mohammed Barghash, Moustafa Mansour, Katie McComb
Supervision: Emmanuel Obayi, Mohammed Barghash, Moustafa Mansour
References
- 1.Giangola M, Havens JM. Emergency General Surgery. Cham: Springer; 2019. Imaging in emergency general surgery; pp. 27–39. [Google Scholar]
- 2.Does timely reporting of preoperative CT scans influence outcomes for patients following emergency laparotomy? Ikram S, Mirtorabi N, Ali D, Aain H, Naumann DN, Dilworth M. Ann R Coll Surg Engl. 2024 doi: 10.1308/rcsann.2023.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Emerging challenges and opportunities in the evolution of teleradiology. Hanna TN, Steenburg SD, Rosenkrantz AB, Pyatt RS Jr, Duszak R Jr, Friedberg EB. AJR Am J Roentgenol. 2020;215:1411–1416. doi: 10.2214/AJR.20.23007. [DOI] [PubMed] [Google Scholar]
- 4.Clinical radiology census reports. 2024. https://www.rcr.ac.uk/news-policy/policy-reports-initiatives/clinical-radiology-census-reports/ https://www.rcr.ac.uk/news-policy/policy-reports-initiatives/clinical-radiology-census-reports/
- 5.Efficiency of outsourcing reporting in thorax computed tomography evaluation: retrospective analysis of 350 thoracic surgery cases. Çetin M, Solak N, Türk İ, Güreşci K. Thorac Res Pract. 2023;24:34–39. doi: 10.5152/ThoracResPract.2023.22100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Radiology reporting: current practices and an introduction to patient-centered opportunities for improvement. Mityul MI, Gilcrease-Garcia B, Mangano MD, Demertzis JL, Gunn AJ. AJR Am J Roentgenol. 2018;210:376–385. doi: 10.2214/AJR.17.18721. [DOI] [PubMed] [Google Scholar]
- 7.Objective comparison of errors and report length between structured and freeform abdominopelvic computed tomography reports. McFarland JA, Elkassem AM, Casals L, Smith GD, Smith AD, Gunn AJ. Abdom Radiol (NY) 2021;46:387–393. doi: 10.1007/s00261-020-02646-9. [DOI] [PubMed] [Google Scholar]
- 8.STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Mathew G, Agha R, Albrecht J, et al. Int J Surg. 2021;96:106165. doi: 10.1016/j.ijsu.2021.106165. [DOI] [PubMed] [Google Scholar]
- 9.Health Research Authority: defining research table. [ Oct; 2024 ]. 2022. http://www.hra-decisiontools.org.uk/research/docs/DefiningResearchTable_Oct2022.pdf http://www.hra-decisiontools.org.uk/research/docs/DefiningResearchTable_Oct2022.pdf
- 10.Error and discrepancy in radiology: inevitable or avoidable? Brady AP. Insights Imaging. 2017;8:171–182. doi: 10.1007/s13244-016-0534-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Quality assessment of out sourced after-hours computed tomography teleradiology reports in a Central London University Hospital. Hohmann J, de Villiers P, Urigo C, Sarpi D, Newerla C, Brookes J. Eur J Radiol. 2012;81:0–9. doi: 10.1016/j.ejrad.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 12.Clinicians' perceptions of the quality of outsourced radiology and actions taken around perceived imaging errors in practice. Graham Y, Hayes C, Mehrotra P, Spratt J, Siddle K, Cox J. Eur Radiol. 2019;29:1649–1654. doi: 10.1007/s00330-018-5873-5. [DOI] [PubMed] [Google Scholar]
- 13.The impact of contracts on outsourcing computed tomography examinations from a Swedish public university hospital to a private radiology unit. Olofsson PT, Aspelin P, Bohlin J, Blomqvist L. Radiography (Lond) 2019;25:148–154. doi: 10.1016/j.radi.2018.12.014. [DOI] [PubMed] [Google Scholar]
- 14.The accuracy of on-call CT reporting in teleradiology networks in comparison to in-house reporting. Storjohann S, Kirsch M, Rosenberg B, et al. Healthcare (Basel) 2021;9:405. doi: 10.3390/healthcare9040405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Emergency medicine summary code for reporting CT scan results: implementation and survey results. Lam J, Coughlin R, Buhl L, Herbst M, Herbst T, Martillotti J, Coughlin B. Emerg Radiol. 2018;25:303–310. doi: 10.1007/s10140-018-1583-1. [DOI] [PubMed] [Google Scholar]
- 16.Impact of structured report on the quality of preoperative CT staging of pancreatic ductal adenocarcinoma: assessment of intra- and inter-reader variability. Dimarco M, Cannella R, Pellegrino S, et al. Abdom Radiol (NY) 2020;45:437–448. doi: 10.1007/s00261-019-02287-7. [DOI] [PubMed] [Google Scholar]
- 17.Structured reporting of CT scans of patients with trauma leads to faster, more detailed diagnoses: an experimental study. Jorg T, Heckmann JC, Mildenberger P, et al. Eur J Radiol. 2021;144:109954. doi: 10.1016/j.ejrad.2021.109954. [DOI] [PubMed] [Google Scholar]
- 18.Good practice for radiological reporting. Guidelines from the European Society of Radiology (ESR) Insights Imaging. 2011;2:93–96. doi: 10.1007/s13244-011-0066-7. [DOI] [PMC free article] [PubMed] [Google Scholar]