Abstract
Purpose:
To search, evaluate, and summarize the relevant evidence of voice rehabilitation training in adults with unilateral vocal fold paralysis (UVFP).
Methods:
Using the ‘6S’ model, the database of UpToDate, BMJ Best Practice, domestic and foreign guidelines, and voice rehabilitation training for adults with UVFP were systematically searched. The search includes clinical decisions, guidelines, systematic reviews, randomized controlled trials, and expert consensus. Data search since the establishment of the database to 27 November 2023. The quality evaluation of the literature methodology and the extraction and integration of evidence were carried out independently by two researchers.
Results:
A total of 12 literature were included, including 2 systematic reviews, 2 expert consensus, 4 guidelines, 2 clinical decisions, and 2 randomized controlled trials. Four categories of 16 pieces of evidence were summarized: evaluation of vocal cord paralysis, voice rehabilitation training, health education, joint decision-making, and multidisciplinary cooperation.
Conclusion:
This study summarized the best evidence of voice rehabilitation training for adults with UVFP and provided evidence-based summary for clinical staff to carry out relevant interventions.
Keywords: evidence-based nursing, summary of evidence, vocal cord paralysis, voice recovery
Introduction
Highlights
There is less summary of the unilateral vocal fold paralysis(UVFP) rehabilitation. This study summarizes the best evidence for voice rehabilitation training in adult UVFP from four aspects: evaluation of vocal cord paralysis, voice rehabilitation training methods, health education, and joint decision-making and multidisciplinary cooperation. This summary provides a reference for clinical practice.
It is found that the effective evaluation, individual rehabilitation treatment, training intensity and duration, and follow-up of UVFP can be further explored in the future.
Unilateral vocal fold paralysis (UVFP) is caused by unilateral damage to the vagus or recurrent laryngeal nerve, and the causes may include infection, iatrogenic injury, malignant tumor, metabolic, toxic, or idiopathic influencing factors1. The clinical manifestations are dysphonia and hoarseness2. Dysphonia affects the daily communication needs of patients and usually requires behavioral or surgical intervention, and some patients still need voice rehabilitation training after surgery to help patients return to normal life as soon as possible3,4.
At present, there is no optimal evidence summary for voice rehabilitation training for adults with UVFP, and no systematic rehabilitation strategy, which hinders the clinical practice to a certain extent5. This study summarized the best evidence for voice rehabilitation of patients with UVFP through systematic retrieval, evaluation, and analysis of domestic and foreign relevant literature, aiming to provide evidence-based support for clinical medical personnel to carry out voice rehabilitation training.
Materials and method
Identification of issues and exclusion criteria
This paper uses the population, Intervention, Profession, Outcome, Setting, and Type of Evidence (PIPOST) model to identify the basic research questions6. The inclusion criteria for evidence were as follows: (1) P (population): evidence target population was adults with UVFP, (2) I (intervention): measures aimed at UVFP voice rehabilitation training, (3) P (professional): evidence applicable to medical personnel, adult UVFP patients. (4) O (outcome): Outcomes are outcome indicators related to voice rehabilitation, (5) S (Settings): evidence applicable to all levels of medical institutions, and (6) T (type of evidence): types of evidence resources include clinical decision-making, clinical guidelines, systematic reviews, expert consensus, and relevant original research. The exclusion criteria are as follows: 1.The content is incomplete or the full text cannot be obtained; 2. Updated old guidelines and interpretation of the guidelines; and 3. Documents in languages other than English and Chinese.
Search strategy
According to the ‘6S’ model of evidence resources and the principle of top-down retrieval7, Computer search Web of Science, Cochrane Library, JBI, PubMed, Embase, CNKI, VIP Database, Wanfang database, EBSCO, UpToDate, BMJ Best Clinical Practice, International Guidelines Collaboration, Ontario Registered Nurses Association, UK National Institute for Health and Clinical Excellence, and China Biomedical Literature Database, including systematic reviews, expert consensus, guidelines, and clinical decision-making. When searching guide websites or evidence-based databases, Use the search term ‘Voice Training’/’Voice exercise’/‘Voice therapy*’/‘Speech pathology’/‘Speech therapy’/‘speech training’ or ‘speech rehabilitation’. Data search since the establishment of the database to 27 November 2023.
Taking CNKI as an example, the Chinese search strategy is as follows: SU % = (‘Vocal cord paralysis/laryngeal paralysis/vocal cord paresis/unilateral vocal cord paralysis’) * (‘Voice training/articulation training/speech training/vocal rehabilitation/vocal cord training/Voice correction/Voice care/Voice health/voice function training/speech exercise/Pronunciation/speech recovery’) * (‘Guidelines/Expert consensus/Systematic review/Clinical decision/Summary of evidence /Meta Analysis /RCT’).
Taking PubMed as an example, the English search strategy is as follows:
#1 (((((((((((‘Vocal Cord Paralysis’[MeSH Terms]) OR (‘Vocal fold par*’[Title/Abstract])) OR (‘Vocal Cord Palsy’[Title/Abstract])) OR (‘Laryngeal Paralys*’[Title/Abstract])) OR (‘Unilateral Vocal Cord Par*’[Title/Abstract])) OR (‘Acquired Vocal Cord Palsy’[Title/Abstract])) OR (‘Unilateral vocal fold paralysis’[Title/Abstract])) OR (‘Recurrent laryn*’[Title/Abstract])) OR (‘Unilateral recurrent laryn*’[Title/Abstract])) OR (‘Vocal fold immobility’[Title/Abstract])) OR (‘Voice disorder’[Title/Abstract])), #2(((((((‘Voice Training’[MeSH Terms]) OR (‘Voice exercise’[Title/Abstract])) OR (‘Voice therap*’[Title/Abstract])) OR (‘Speech pathology’[Title/Abstract])) OR (‘Speech therapy’[Title/Abstract])) OR (‘speech training’[Title/Abstract])) OR (‘speech rehabilitation’[Title/Abstract])), #3 (Guidelines/Expert consensus/Systematic review/Clinical decision-making/evidence summary/meta-analysis /RCT), and #4 (#1 AND #2 AND #3).
Literature quality evaluation
The quality evaluation criteria for guidelines were from the Appraisal of Guidelines for Research and Evaluation Instrument (AGREE II)8,9. AGREE II includes 23 items in 6 areas, including scope and purpose, participants, rigor of formulation, clarity of expression, application, and editorial independence. Each item is scored from 1 to 7 points (1= strongly disagree, 7= strongly agree)10.
The expert consensus was evaluated using the evaluation tool recommended by the Joanna Briggs Institute (JBI) Centre for Evidence-Based Health Care in Australia, and the randomized controlled trial (RCT) articles were evaluated using the JBI Centre for Evidence-Based Health Care randomized Controlled trial evaluation criteria.
The quality of evidence and the level of recommendation were independently assessed by two researchers. When there are differences in evaluation opinions, we will discuss them with the third researcher to decide whether to include them. In the event of discrepancies in the content of evidence, we give priority to the principle of newly published and high-quality evidence.
All evidence is graded A–B according to the 2014 edition of the JBI Evidence-Based Health Care Center’s Evidence recommendation level system with A as a strong recommendation and B as a weak recommendation11.
Results
Literature screening results
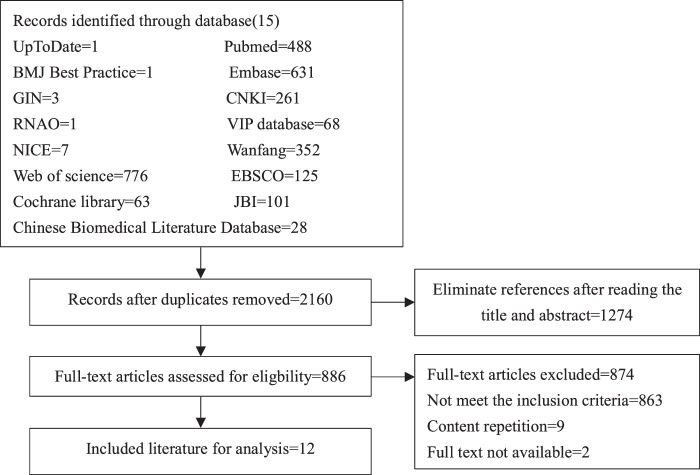
A total of 2906 literature were retrieved and imported into the Endnote literature manager. After de-duplicated and preliminary screening, 2160 literature remained. Two researchers selected the literature independently, and when there was a conflict of opinion, the third researcher participated in the discussion to decide whether to include them.
In the end, 12 literature were included (Fig. 1). There were two clinical decision-making, four guidelines, two expert consensus, two systematic reviews, and two RCTs. The basic information of the included literature is shown in Table 1.
Figure 1.
Literature screening process and results.
Table 1.
General characteristics of the included literature (n=12).
| Included literature | Publication time | Source | Type | Theme |
|---|---|---|---|---|
| Zelazny et al.12 | 2021 | BMJ best practice | Clinical decision | Assessment of hoarseness and dysphonia |
| Bruch et al.13 | 2023 | Up to date | Clinical decision | The adult’s voice is hoarse |
| Korean Society of Laryngology et al.14 | 2020 | PubMed | Guide | Management of unilateral vocal cord paralysis |
| Stachler et al.15 | 2018 | GIN | Guide | Hoarseness (dysphonia) |
| Chandrasekhar et al.16 | 2013 | GIN | Guide | Improves sound effects after thyroid surgery |
| Korean Society of Laryngology et al.17 | 2022 | PubMed | Guide | Nursing and management of sound changes during thyroid surgery |
| Mattei et al.18 | 2017 | PubMed | Expert consensus | Basic sound assessment of unilateral vocal cord paralysis |
| Chinese Medical Association Otolaryngology, Head and Neck Surgery Branch, Pharyngology Group et al.19 | 2020 | Wang fang | Expert consensus | Diagnosis and treatment of vocal cord paralysis |
| Walton et al.20 | 2016 | PubMed | Systematic evaluation | Unilateral vocal cord paralysis: speech pathology management |
| Alegria et al.21 | 2020 | Web of Science | Systematic evaluation | Effects of speech therapy on unilateral vocal cord paralysis - measurement of visual perception outcomes |
| Mari et al.22 | 2022 | PubMed | RCT | Voice tele-rehabilitation of iatrogenic unilateral vocal cord paralysis: From necessity to opportunity in the COVID-19 era |
| Liu et al.23 | 2021 | CNKI | RCT | Effect of early voice training on improving voice quality in patients with vocal cord paralysis after thyroid surgery |
RCT, randomized controlled trial.
Quality evaluation results of the guide
A total of four guidelines were included in this study, and their quality evaluation results are shown in Table 2.
Table 2.
Quality evaluation of guidelines (n=4).
| Inclusion guide | Percentage of standardized scores in each area | ≥60% Number of fields (PCS) | ≥30% Number of fields (PCS) | Recommended level (level) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Scope and purpose | Participant | The rigor with which guidelines are developed | Clarity of expression | Application of the guidelines | Independence of the guide editor | ||||
| Korean Society of Laryngology et al.14 | 100 | 100 | 98.9 | 94.4 | 87.5 | 91.6 | 6 | 6 | A |
| Stachler et al.15 | 100 | 100 | 95.8 | 100 | 72.9 | 100 | 6 | 6 | A |
| Chandrasekhar et al.16 | 100 | 100 | 88.5 | 97.2 | 75 | 100 | 6 | 6 | A |
| Korean Society of Laryngology et al.17 | 66.7 | 58.3 | 79.2 | 83.3 | 46.9 | 50 | 3 | 6 | B |
Quality evaluation results of expert consensus
A total of two expert consensus articles were included in this study, and their quality evaluation is shown in Table 3.
Table 3.
Methodological quality evaluation results incorporating expert consensus (n=2).
| Included literature | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Mattei et al.18 | Y | Y | Y | Y | Y | Y |
| Chinese Medical Association Otolaryngology, Head and Neck Surgery Branch, Pharyngology Group et al.19 | Y | Y | Y | N | Y | Y |
Note: 1: Whether the source of the opinion is clearly stated; 2. Whether the ideas come from influential experts in the field; 3: Whether the proposed viewpoint is centered on the interests of the relevant population; 4: Are the stated conclusions based on the results of the analysis? Are ideas expressed logically? 5: Whether it has referred to other existing literature; 6: Is there any inconsistency between the proposed views and the previous literature?
Quality evaluation results of system evaluation
A total of two systematic reviews20,21 were included in this study. Except for item 11 of Walton’s et al.20, the evaluation result of ‘whether the relevant conflict of interest is indicated’ was ‘unclear’, the evaluation result of the other items was ‘yes’, and the overall quality was high, so inclusion was allowed.
RCT quality evaluation results
A total of two RCTs22,23 were included in this study, and the evaluation criteria of the JBI Evidence-Based Center randomized controlled trial were used. Item 5 of the literature quality evaluation by Walton’s et al.20was ‘no’, items 1-2 were ‘unclear’, and other items were ‘Yes’. Items 2, 4–6, and 8 of the literature quality evaluation by Liu et al.23 are ‘unclear’, and other items are ‘yes’.
Evidence description and summary
According to the principle of evidence synthesis, the researchers summarized the evidence. A total of 16 pieces of evidence were summarized, including 4 evidence topics, as shown in Table 4.
Table 4.
Summary of the best evidence for vocal rehabilitation training in adults with unilateral vocal cord paralysis.
| Item | Content of evidence | Source | Class of evidence | Recommendation level |
|---|---|---|---|---|
| Evaluation of vocal cord paralysis | 1. Early identification of patients with dysphonia, and timely referral for professional evaluation15,16 | Clinical decisions, guidelines, expert consensus, and systematic reviews | 2 | A |
| 2. The patient’s medical history should be asked in detail and a more detailed physical examination should be given12–15 | 5 | A | ||
| 3. Suggest subjective and objective assessments. The selection of assessment tools should be based on the patient’s ability to effectively participate and the examiner’s ability to equip the assessment tools14–20 | 2 | B | ||
| 4. The subjective assessment is recommended using the Voice Handicap Index (VHI) and/or Grade, Rough, Breathy, Asthenic, and Strained (GRBAS), and/or Consensus Auditory-Perceptual Evaluation of Voice (CAPE-V)12,14,16–20 | 2 | B | ||
| 5. Objective evaluation Acoustic analyzer, aerodynamic evaluation, and laryngoscopy are recommended12,14–20 | 2 | A | ||
| Voice rehabilitation training | 6. When to start: ①For patients with mild symptoms, no contraindications, and who are willing to treat, rehabilitation therapy is recommended as soon as possible14,16,17,22,23. ②For patients who need surgery, it is recommended to start voice training before surgery14. ③ For patients who have undergone surgery, it is recommended to start treatment after the swelling at the surgical site has subsided14 |
Guidelines, expert consensus, systematic review, RCT | 1 | A |
| 7. Rehabilitation training twice a week, 30 min each time, at least 15 times, face-to-face treatment by speech therapists, patients repeat the practice every day during treatment20,22. Training includes14,17,19–21: ①a cough attack: forced expiration with closed glottis. ②a cough with vowel: cough and then release a vowel (/i/ /e/ /a/ /o/). ③a quick and energic emission of a vowel (/i/ /e/ /a/ /o/ /u/), occlusive dull (/kà/ /kè/ /kò/) and sonant (/gà/ /gè/ /gò/) syllables; (/kaka/ /kekè/ /gogò/ /dedè/) with truncation of the final vowel; a single vowel (/aaaaa/ /eeeee/) or syllable (/kaaaa/ /kiiii/ /ghee/). ④Relaxation training: chest expansion ‐ arm stretching ‐ shoulder relaxation ‐ neck stretching ‐ head and neck rotation ‐ jaw stretching ‐ chin massage ‐ face massage ‐ throat massage, yawn, tongue extension and other sequence relaxation ⑤ Breathing training: the patient is instructed to relax the upper body, shrink the diaphragm, increase the upper and lower diameter of the chest, expand the chest space, shrink the abdominal space, and protrude the abdomen when inhaling. When exhaling, the diaphragm relaxes and restores, the abdominal space recovers, and the abdomen recovers. ⑥Pronunciation training: hold your breath while pushing against a wall or pulling out a chair; Cough vigorously; Sound /i/, /e/, /a/, /o/ after coughing; The hard accent pronounces /e/ with a lower pitch; Exertion exercise: Exertion (sharp rise) to sound vowels in a comfortable pitch, and add sounds, words, and paragraphs. ⑦Resonance training: adjust the relationship between the cavity of the mouth, nasal cavity, chest cavity, etc., to improve the efficiency of pronunciation |
1 | A | ||
| 8. Quality control and efficacy monitoring: ①Use a structured framework treatment plan to control the intensity and duration of treatment21. ②Improve patient compliance: for example, establish a trusting relationship with patients, actively follow-up, use smart devices to record, and perform imitation exercises, and fill in training manuals every day15,19. ③ At the end of treatment, the patient’s response to treatment and voice status were recorded15 |
1 | A | ||
| Health education | 9. During the third week of voice training, the voice function was evaluated again and the training plan was adjusted according to the results19 | Guidelines, clinical decisions, systematic reviews, expert consensus | 2 | A |
| 10. It is suggested that patients should be routinely consulted on the mechanism of voice production and educated on voice health12,14,15,17,19–21 | 1 | B | ||
| 11. It is recommended to drink more water every day to keep indoor air humidity15,19 | 5 | A | ||
| 12. Reduce irritating food intake to prevent throat reflux disease15,19 | 4 | A | ||
| 13. Prevent voice fatigue, exertion, and overuse, and correct bad pronunciation habits14,15,17,19 | 1 | A | ||
| Joint decision-making and multidisciplinary cooperation | 14. Patients are advised to participate in the decision-making of voice rehabilitation treatment16 | Clinical decisions, guidelines | 1 | B |
| 15. Provide a variety of decision aids, including brochures, photos, videos and/or web-based tools, to promote shared decision-making15,16 | 2 | B | ||
| 16. Speech therapists should take the lead in voice therapy and cooperate fully with otolaryngologists, psychologists psychiatrists, and other health professionals12,15,16 | 2 | B |
Discussion
Voice changes will have a significant impact on patients’ work, social activities, psychological state, and social quality of life. As an auxiliary means of voice rehabilitation, the clinical staff should pay attention to voice therapy to improve the quality of voice rehabilitation in UVFP patients.
Selection of appropriate methods to assess vocal cord paralysis
In clinical practice, the clinical specialist should evaluate the tone, tone quality, and vocal function of the patient’s voice. Patients with voice disorders should be identified as early as possible and referred promptly to an ear, nose, and throat specialist (ENT) or speech therapist for professional evaluation15,16. Meanwhile, a more detailed physical examination and history assessment should be performed to see if the patient has a history of surgical procedures that may affect future voice training, including the neck and mouth.
The evaluation of voice training should be a combination of subjective and objective. Patient-reported outcome measures such as the Voice Handicap Index (VHI), perceptual voice evaluation such as Grade, Rough, Breathy, Asthenic, and Strained (GRBAS), and Consensus Auditory-Perceptual Evaluation of Voice (CAPE-V) are recommended for the subjective evaluation14–20. The VHI-30 developed by Jacobson et al. consists of three dimensions, Emotional (E), Physical (P), and Functional (F), with 30 items. The VHI-10 established by Rosen et al. is based on VHI-30 and simplified into 10 items, which confirmed that can be used as an alternative to the VHI-30 for the assessment of vocal cord paralysis. The Chinese version of the VHI scale mainly evaluates the impact of voice abnormality on patients’ quality of life, which is divided into three parts: physiological, functional, and emotional24. Perceptual voice evaluation such as GRBAS is proposed by the Japanese Speech and Speech Association and is the most commonly used subjective auditory perception assessment method in the world. CAPE-V was created by the American Speech-Language-Hearing Association (ASHA)25. It is an interval scale provided by the 100 mm visual analog line, it also includes the ordinal ratings of mild, moderate, and severe, printed below the measurement line. CAPE-V is shown to better accommodate the task of measurement of multidimensional features, such as vocal quality25. Acoustic analysis and aerodynamic evaluation are recommended for objective evaluation. Acoustic analysis includes jitter, shimmer, noise harmonic ratio, and cepstrum peak prominence to objectively assess the patient’s sound quality. Aerodynamic assessments, including maximum phonation time and average airflow rate, can be used to assess glottic insufficiency in patients with UVFP26.
In addition, multiple evidence suggests that laryngoscopy should be used before and after evaluation. To enhance clarity, it would be beneficial to choose the different types of laryngoscope examinations that are available, such as rigid and flexible scopes, laryngeal stroboscopy, and laryngeal high-speed imaging. Furthermore, artificial intelligence (AI) technology also plays its role in this field. Żurek et al.27 found that AI shows very high accuracy, sensitivity, and specificity when using laryngeal endoscopy to evaluate images of laryngeal lesions. AI starts focused on vocal fold vibration analysis, lesion recognition, and vocal cords paralysis28. Endoscopic results of laryngeal structure and function provide information on vocal cord motion, glottic closure, vocal cord level differences, and laryngeal compensation in UVFP patients, and these data results correlate strongly with perceptual and subjective voice outcome measures12,14–19.
However, due to different selection tools in clinical evaluation, there are differences between the same indicators in the same patient. Therefore, the selection of appropriate assessment tools according to the existing tools of the evaluator and the patient’s participation can effectively improve the evaluation efficiency of patients with voice disorders3. In clinical work, medical staff should closely monitor voice change, appropriate methods should be selected to carry out voice evaluation.
Find the right time to carry out effective training; encourage active participation to improve patient compliance
At present, it is not clear when voice training begins in patients with vocal cord paralysis29. High-quality evidence recommends voice training as soon as indicators or clinical symptoms of voice training are present in patients14,16,17,22,23. Timely and effective pronunciation training can improve the outcome of voice rehabilitation. For patients who need surgery, the guidelines recommend that voice training be used as adjuvant therapy before surgery to improve the efficiency of voice rehabilitation. Voice therapy for patients after surgery may be effective as soon as the swelling subsides after surgery. At this time, the goal of voice therapy is to help patients adapt to the new vocal system after surgery14.
Studies by Mattioli et al.30 showed that vocal cord motion recovery rates were higher when voice training was performed within 4 weeks after surgery compared to other groups. The Korean Phonetic Society has shown that atrophic changes in muscle tone are related to the duration of lack of muscle use, and early intervention in patients with voice disorders can prevent or delay muscle atrophy17.
Two systematic reviews and one RCT recommended that voice therapy should be conducted face-to-face with an experienced speech therapist, and take 30 min twice a week at least 15 times20–22. Alegria et al.21use a structured framework treatment plan to control the intensity and duration of treatment to improve the efficiency of voice rehabilitation. Voice rehabilitation is influenced by many factors, such as individual, environment, and psychology, so compliance and guidance training is the basis for improving rehabilitation efficiency17. Evidence shows that the daily recording of patients’ voices can provide decision-making information for doctors, and patients actively participate in treatment decisions, which can increase their subjective initiative, improve training compliance, ensure training quality, and help promote the formulation of personalized treatment plans.
Improve health education, promote joint decision-making, and suggest multidisciplinary participation to ensure the comprehensiveness and continuity of rehabilitation treatment
Evidence shows that patients with vocal cord paralysis should pay attention to voice rest. Relevant consultation methods were provided to patients, and patients were suggested to participate in the decision-making of voice rehabilitation therapy.
Most research and evidence in this field are conducted by ENT specialists and speech therapists20–23. However, clinical practice is limited to the decision of clinicians, ignoring the recommendations of ENT specialists and speech therapists12. In the future, multidisciplinary teams can be formed to further explore the effect of voice rehabilitation training management for patients with UVFP.
This study primarily focuses on phonation function, but the significance of dysphagia and the risk of aspiration pneumonia in patients with vocal paralysis could not be underestimated. Therefore, speech therapy should always be arranged for vocal paralysis.
Conclusions
This study summarized 16 best evidence for voice rehabilitation of adults with UVFP, including the evaluation of vocal cord paralysis, voice rehabilitation training methods, health education, joint decision-making, and multidisciplinary cooperation, providing evidence-based evidence for clinical staff to carry out relevant interventions and providing evidence-based guidance for the optimization of voice rehabilitation programs. At the same time, it is found that the effective evaluation, individual rehabilitation treatment, training intensity, training duration, follow-up, and other aspects of UVFP can be further explored in the future, to update and improve the evidence.
Limitations
This study has certain limitations. This evidence summary only includes published studies in Chinese and English. The literature included in this study was mainly from Asia. Future research should aim to incorporate high-quality original research to gain a deeper understanding of the best protocols for voice rehabilitation therapy.
Ethical approval
This manuscript is a summary of the best evidence and does not require ethical approval.
Consent
This manuscript is a summary of the best evidence and does not require ethical approval.
Source of funding
This research received a grant from the funding agency Department of Education of Zhejiang Province (Y202249502).
Author contribution
C.T. and X.Z.: developed the search strategies; H.H. and L.J.: participated in literature screening, extracting, and recording the information from the enrolled studies; W.T. and X.Z.: evaluation in quality in individual studies; C.T.: responsible for writing the article; Y.S.: responsible for guiding the writing and participating in the revision of the article. All authors read and approved the final article.
Conflicts of interest disclosure
The authors declare that they have no financial conflict of interest with regard to the content of this report.
Research registration unique identifying number (UIN)
http://ebn.nursing.fudan.edu.cn/resource/summary
UIN:ES20233886.
Guarantor
Yulan Shi is the one who accept full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Data availability statement
The datasets generated during and/or analyzed during the current study are publicly available.
Provenance and peer review
Not commissioned.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Caihong Tang, Email: zrtch@zju.edu.cn.
Xinxin Zhang, Email: 2522087@zju.edu.cn.
Hong He, Email: zrhh@zju.edu.cn.
Lingling Jing, Email: jll320818@zju.edu.cn.
Wangyang Tuo, Email: tuowangy@163.com.
Yulan Shi, Email: 2187009@zju.edu.cn.
References
- 1. Naunheim ML, Yung KC, Schneider SL, et al. Vocal motor control and central auditory impairments in unilateral vocal fold paralysis. Laryngoscope 2019;129:2112–2117. [DOI] [PubMed] [Google Scholar]
- 2. Wen MH, Wang CT. Treatment options and voice outcomes for patients with unilateral vocal fold paralysis after thyroidectomy. Front Endocrinol (Lausanne) 2022;13:886924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Walton C, Carding P, Conway E, et al. Voice outcome measures for adult patients with unilateral vocal fold paralysis: a systematic review. Laryngoscope 2019;129:187–197. [DOI] [PubMed] [Google Scholar]
- 4. Kurz A, Leonhard M, Denk-Linnert DM, et al. Comparison of voice therapy and selective electrical stimulation of the larynx in early unilateral vocal fold paralysis after thyroid surgery: a retrospective data analysis. Clin Otolaryngol 2021;46:530–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Desuter G, Dedry M, Schaar B, et al. Voice outcome indicators for unilateral vocal fold paralysis surgery: A survey among surgeons. Eur Ann Otorhinolaryngol Head Neck Dis 2019;136:343–347. [DOI] [PubMed] [Google Scholar]
- 6. Zhu Z, Hu Y, Xing W, et al. The composition of different types of evidence-based questions. J Nurses Train 2017;32:1991–1994. [Google Scholar]
- 7. D’Andrea VD, Melnick K, Yim K, et al. Evidence-based analysis of the critical steps of radical cystectomy for bladder cancer. J Clin Med 2023;12:6845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gu Y, Zhang H, Zhou Y, et al. JBI evidence-based health center’s quality assessment tool for different types of research – the quality evaluation of systematic review. J Nurses Train 2018;33:701–703. [Google Scholar]
- 9. Brouwers MC, Kho ME, Browman GP, et al. AGREE II: advancing guideline development, reporting, and evaluation in health care. Prev Med 2010;51:421–424. [DOI] [PubMed] [Google Scholar]
- 10. Gavriilidis P, Askari A, Roberts KJ, et al. Appraisal of the current guidelines for management of cholangiocarcinoma-using the Appraisal of Guidelines Research and Evaluation II (AGREE II) Instrument. Hepatobiliary Surg Nutr 2020;9:126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jordan Z, Lockwood C, Munn Z, et al. Redeveloping the JBI model of evidence based healthcare. Int J Evid Based Healthc 2018;16:227–241. [DOI] [PubMed] [Google Scholar]
- 12. Zelazny SK, Thibeault SL, Dailey S. Assessment of hoarseness and dysphonia. June 22, 2021. Accessed November 28, 2023. https://bestpractice.bmj.com/topics/zhcn/845?q=%E5%A3%B0%E9%9F%B3%E5%98%B6%E5%93%91%E5%92%8C%E5%8F%91%E9%9F%B3%E9%9A%9C%E7%A2%8D%E7%9A%84%E8%AF%84%E4%BC%B0&c=recentlyviewed
- 13. Bruch JM, Kamani DV. Hoarseness in adults. August 7, 2023. Accessed November 28, 2023. https://www.uptodate.com/contents/zh-Hans/hoarseness-in-adults
- 14. Korean Society of Laryngology. Phoniatrics and Logopedics Guideline Task Force. Ryu CH, et al. Guidelines for the management of unilateral vocal fold paralysis from the Korean Society of Laryngology, Phoniatrics and Logopedics. Clin Exp Otorhinolaryngol 2020;13:340–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stachler RJ, Francis DO, Schwartz SR, et al. Clinical practice guideline: hoarseness (Dysphonia) (Update). Otolaryngol Head Neck Surg 2018;158(1_suppl):S1–S42. [DOI] [PubMed] [Google Scholar]
- 16. Chandrasekhar SS, Randolph GW, Seidman MD, et al. Clinical practice guideline: improving voice outcomes after thyroid surgery. Otolaryngol Head Neck Surg 2013;148(6 Suppl):S1–S37. [DOI] [PubMed] [Google Scholar]
- 17. Korean Society of Laryngology. Phoniatrics and Logopedics Guideline Task Force. Ryu CH, Lee SJ, et al. Care and management of voice change in thyroid surgery: Korean Society of Laryngology, Phoniatrics and Logopedics Clinical Practice Guideline. Clin Exp Otorhinolaryngol 2022;15:24–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mattei A, Desuter G, Roux M, et al. International consensus (ICON) on basic voice assessment for unilateral vocal fold paralysis. Eur Ann Otorhinolaryngol Head Neck Dis 2018;135:S11–S15. [DOI] [PubMed] [Google Scholar]
- 19. Subspecialty Group of Laryngopharyngology. Editorial Board of Chinese Journal of Otorhinolaryngology Head and Neck Surgery. Subspecialty Group of Laryngopharyngology . Experts consensus on diagnosis and treatment of vocal fold paralysis. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2021;56:198–209. [DOI] [PubMed] [Google Scholar]
- 20. Walton C, Conway E, Blackshaw H, et al. Unilateral vocal fold paralysis: a systematic review of speech-language pathology management. J Voice 2017;31:509.e7–509.e22. [DOI] [PubMed] [Google Scholar]
- 21. Alegria R, Vaz Freitas S, Manso MC. Efficacy of speech language therapy intervention in unilateral vocal fold paralysis - a systematic review and a meta-analysis of visual-perceptual outcome measures. Logoped Phoniatr Vocol 2021;46:86–98. [DOI] [PubMed] [Google Scholar]
- 22. Mari G, Marchese MR, Longobardi Y, et al. Voice telerehabilitation in iatrogenic unilateral vocal fold paralysis: from necessity to opportunity in the COVID-19 time. J Voice. Published online May 28, 2022:S0892-1997(22)00108-4. [DOI] [PubMed]
- 23. Liu J, Zhao R, Wang S, et al. Efficacy of voice training on voice quality in patients with vocal cord paralysis after thyroid surgery. Chin Archiv Otolaryngol Head Neck Surg 2021;28:41–44. [Google Scholar]
- 24. Batista D, de J, da Silva RD, et al. Internal consistency of the voice handicap index in individuals with dysphonia: a systematic review and meta-analysis. J Voice. Published online September 29, 2023:S0892-1997(23)00253-9. [DOI] [PubMed]
- 25. Kempster GB, Gerratt BR, Verdolini Abbott K, et al. Consensus auditory-perceptual evaluation of voice: development of a standardized clinical protocol. Am J Speech Lang Pathol 2009;18:124–132. [DOI] [PubMed] [Google Scholar]
- 26. Desuter G, Dedry M, Schaar B, et al. Voice outcome indicators for unilateral vocal fold paralysis surgery: a review of the literature. Eur Arch Otorhinolaryngol 2018;275:459–468. [DOI] [PubMed] [Google Scholar]
- 27. Żurek M, Jasak K, Niemczyk K, et al. Artificial intelligence in laryngeal endoscopy: systematic review and meta-analysis. JCM 2022;11:2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yao P, Usman M, Chen YH, et al. Applications of artificial intelligence to office laryngoscopy: a scoping review. Laryngoscope 2022;132:1993–2016. [DOI] [PubMed] [Google Scholar]
- 29. Ruoppolo G, Mariani L, Quaglieri S, et al. Unilateral vocal fold paralysis post-thyroidectomy: does early intervention allow for better voice recovery? Eur Rev Med Pharmacol Sci 2021;25:1177–1184. [DOI] [PubMed] [Google Scholar]
- 30. Mattioli F, Menichetti M, Bergamini G, et al. Results of early versus intermediate or delayed voice therapy in patients with unilateral vocal fold paralysis: our experience in 171 patients. J Voice 2015;29:455–458. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are publicly available.