Abstract
Introduction and importance:
A carotid-cavernous sinus fistula is an abnormal connection between the internal or external carotid artery and the venous system of the cavernous sinus. It represents a rare entity, and it is often misdiagnosed due to its overlapping symptoms with other conditions such as cavernous sinus thrombosis or orbital inflammation. Cerebral angiography continues to be the gold standard for diagnosis and surgical planning in patients with CCF, and the endovascular trans-venous approach still represents the primary line of treatment. Trans-arterial technique has become an excellent treatment option since the advent of embolic agents.
Case presentation:
Here, the authors report the case of a 42-year-old male with a one-week history of impaired visual acuity, bilateral eye edema, eye redness, and ophthalmoplegia. A neuro-ophthalmological examination found proptosis, conjunctival chemosis, and sclera injection. Examination using MR venography and digital subtraction angiography (DSA) revealed an abnormal connection between the meningeal branch of the ICA, the ECA, and the cavernous sinus. The patient received endovascular treatment with Onyx injection into the facial vein with thrombosis of the anterior cavernous sinus. The patient presented an uneventful postoperative period and was symptoms-free on postoperative day 1.
Clinical discussion:
CCF are rare and challenging conditions that require a multidisciplinary approach.
Conclusion:
The endovascular treatment represents the gold standard and usually allows an effective interruption of the abnormal vascular connection with an almost immediate resolution of the preoperative signs and symptoms.
Keywords: carotid-cavernous fistula, cavernous sinus, proptosis
Introduction
Highlights
A 42-year-old patient had impaired vision and proptosis, conjunctival chemosis, and sclera injection.
Digital subtraction angiography (DSA) revealed an abnormal connection between the meningeal branch of the ICA, the ECA, and the cavernous sinus.
The patient received endovascular treatment with Onyx injection into the facial vein with thrombosis of the anterior cavernous sinus. The patient presented an uneventful postoperative period and was symptoms-free on postoperative day 1.
Carotid-cavernous sinus fistulas (CCFs) are rare conditions based on an abnormal vascular connection between the carotid artery and the cavernous sinus1.
They clinically present with a classic triad: proptosis, eye congestion, and signs of turbulent flow into the cavernous sinus. Treatment is crucial to interrupt the abnormal communication decreasing the venous pressure and restoring the normal venous outflow from the orbit2–6.
Here, we report a rare case of bilateral carotid-cavernous fistula, and we review the classification, clinical presentation, pathophysiology, diagnosis and treatment of CCFs. We followed the SCARE 2023 criteria7 to present our case. We report this case because indirect fistulas, particularly Barrow type D, are quite uncommon.
Case report
A 42-year-old male was admitted to our Institution with a 1-week history of impaired visual acuity, bilateral eye edema, eye redness, and ophthalmoplegia. A full neuro-ophthalmological examination was completed showing proptosis, conjunctival chemosis, and sclera injection (Fig. 1).
Figure 1.

Neuro-ophthalmic assessment of the patient.
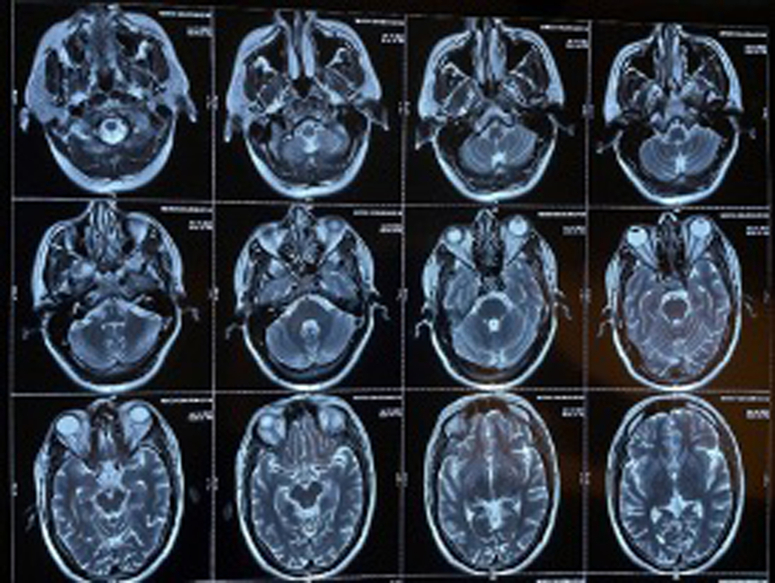
As further investigation, the patient underwent a brain MRI/MRA (Fig. 2), that showed an absence of flow into the left cavernous, which was suggestive of thrombosis. As a result, it was presumed that the patient had cavernous sinus thrombosis.
Figure 2.
MRI showing thrombosis of cavernous sinus.
The symptoms persisted despite the medication. Further examination using MR venography (Fig. 3) and digital subtraction angiography (DSA) (Fig. 4) revealed an abnormal connection between the meningeal branch of the ICA, the ECA, and the cavernous sinus.
Figure 3.
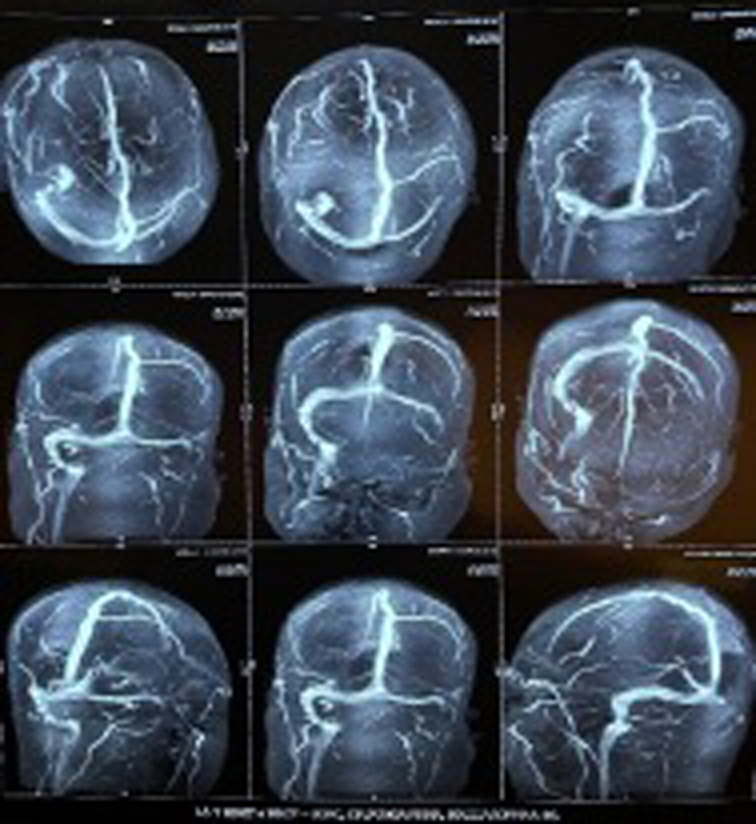
MR venography.
Figure 4.
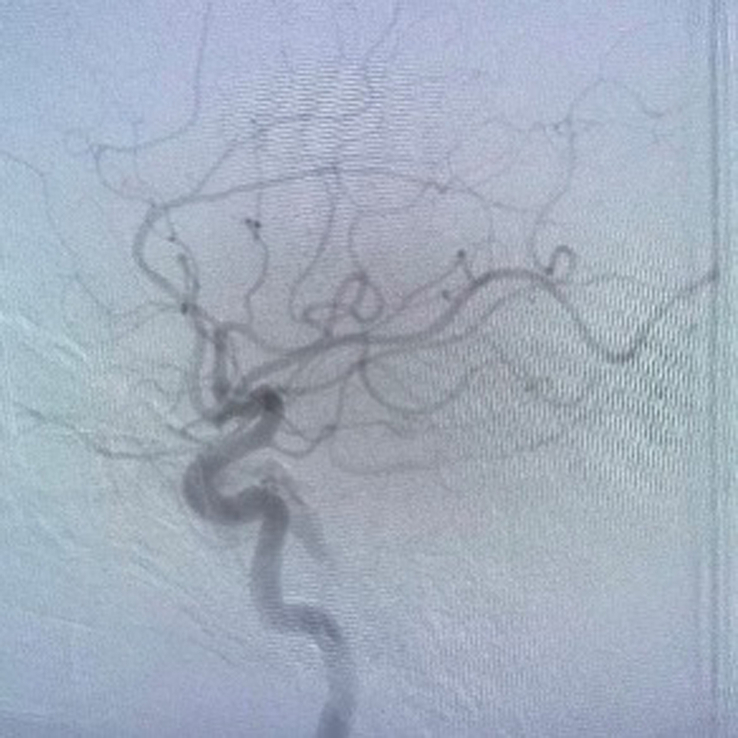
Digital subtraction angiography.
After case review at the neuroendovascular meeting, the patient was brought into the operating room for embolization (Fig. 5). Using a trans-venous approach through the left facial vein, Onyx was injected into the anterior cavernous sinus and thrombosis was achieved. The patient well tolerated the procedure and was symptom-free on postoperative day 1 (Fig. 6). The work has been reported in line with the SCARE 2023 criteria7.
Figure 5.

Preoperative assessment.
Figure 6.

Postoperative result.
Discussion
Anatomy
The dural venous sinus (Fig. 7) includes the cavernous sinus, which is home to a number of neuro-vascular structures. It is located symmetrically lateral to the sella turcica, it measures about 1 cm in width and 2 cm in length, and it runs from the superior orbital fissure to the petrous part of the temporal bone.
Figure 7.

Cavernous sinus anatomy.
The superficial middle cerebral vein, the superior and anterior ophthalmic veins, and the sphenoparietal sinus all supply the cavernous sinus with venous blood; the intercavernous sinuses, anterior and posterior, provide communication between the left and right cavernous sinuses8,9.
Arterial anatomy
Throughout its path through the CS, the ICA gives rise to a number of arterial branches, the largest of which is the meningo-hypophyseal trunk. This vessel emerges from the dorsal perimeter of the C5 segment of the ICA, just before the vertical part turns into the horizontal one.
The inferior hypophysial artery was initially described by Luschka in 1860 and it supplies the anterior hypophyseal artery, the tentorial artery, and the lateral clival artery. The tentorium’s dura is also supplied by the artery of Bernasconi–Cassinari (lateral clival artery or dorsal meningeal artery).
The infero-lateral trunk, which supplies the portion of the cranial nerves going into the lateral sellar compartment, and the capsular artery of McDonnel are two more rather constant branches. The ICA and ECA’s branches are constantly anastomosed even if it is not always angiographically evident.
Knowledge of these anastomotic channels is crucial in preventing complications during endovascular approaches10.
Venous anatomy
For the understanding of the angiographical anatomy of cavernous sinus dural arteriovenous fistulas (CSDAVFs), it is essential to understand how the venous channels related to the cavernous sinus (Fig. 8).
Figure 8.

Superior ophthalmic vein, cavernous sinus, and inferior ophthalmic vein.
The anterior part of the CS receives regular venous drainage from the orbit through the superior and inferior ophthalmic veins. Additionally, the sphenoparietal sinus serves as the typical entry point for the superficial middle cerebral veins into the CS. The circular sinus is created when the two separated CSs interact via the anterior and posterior intercavernous sinuses. To reach the jugular bulb, posterior drainage passes through the basilar plexus, the superior petrosal sinuses, and the inferior petrosal sinuses. Connections can be found inferolaterally through the dural veins that drain into the pterigoid plexus.
Classification
CCFs are usually classified according anatomy, origin, and hemodynamic features.
Based on their hemodynamic characteristics we are able to identify high-flow and low-flow CCFs. Etiologically we can classify CCF as spontaneous or traumatic11.
According to their angio-architecture, CCFs can be divided into 4 groups (Fig. 9) (Table 1):
Direct fistulas (Barrow type A)
Indirect or dural fistulas (Barrow types B, C, and D).
Figure 9.
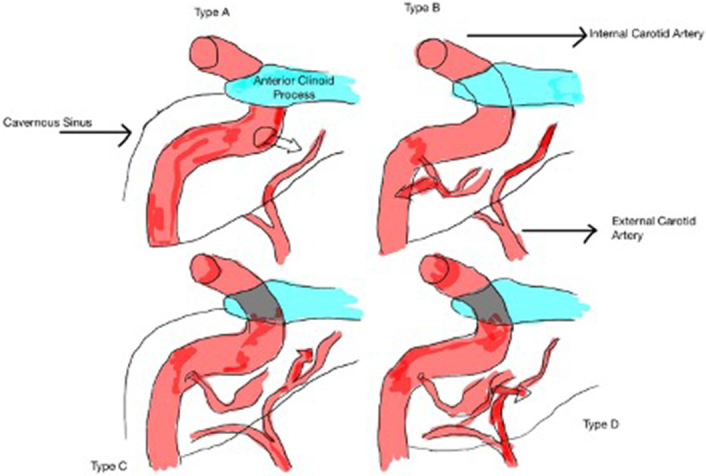
Classification of carotid-cavernous fistula.
Table 1.
Barrow classifications for types of carotid-cavernous fistula.
| Type | Direct vs. indirect | Description |
|---|---|---|
| A | Direct | Direct connection between ICA and cavernous sinus. |
| B | Direct | Connection between dural branches of ICA and cavernous sinus |
| C | Indirect | Connection between dural branches of ECA and cavernous sinus |
| D | Indirect | Connection between dural branches of both ICA and ECA and cavernous sinus |
ECA, external carotid artery; ICA, internal carotid artery.
The internal carotid artery (ICA) and the cavernous sinus are directly connected in direct fistulas. Typically, they are high-flow fistulas12–27.
On the contrary, indirect or dural CCFs are low-flow fistulas that connect the cavernous sinus and cavernous artery branches. Specifically, meningeal branches of the ICA are involved in Barrow type B fistulas, ECA branches are in Barrow type C fistulas, and meningeal branches from both the ICA and ECA are involved in Barrow type D fistulas. Type D spontaneous dural CCFs are the most common28.
The inferior cavernous sinus artery is the ICA trunk that is most usually implicated; however, dural fistulas can also affect the meningo-hypophyseal trunk and its branches. The internal maxillary artery, middle and accessory meningeal arteries, ascending pharyngeal artery, anterior deep temporal artery, and posterior auricular artery are the branches of the external carotid artery that are most frequently affected29.
Etiology
Traumatic CCFs are usually type A direct fistulas and frequently show a single direct contact between the ICA and the cavernous sinus. Nonetheless, the cavernous sinus wall typically contains several micro-fistulas and various dural feeders in spontaneous fistulas30. Because a type A shunt with high-flow characteristics might emerge after spontaneous rupture of an intracavernous ICA aneurysm, spontaneous CCFs may fit into any of the four angiographic classifications established by Barrow31.
The most frequent cause of direct CCFs is traumatic disruption of the vessel wall. Direct CCFs may result from blunt and penetrating head trauma as well as iatrogenic harm32,33.
Around 20% of type A CCFs are thought to be spontaneous and unrelated to any history of trauma5,34. They typically result from the rupture of an atherosclerotic artery or a cavernous segment aneurysm5,36. Ehlers-Danlos syndrome, fibromuscular dysplasia, and pseudoxanthoma elasticum are also risk factors linked to spontaneous type A, CCFs5,37,38.
Pathophysiology and clinical features
The presence of important neuro-vascular structures into the cavernous sinus affects the symptomatology of CCFs. They comprise cranial nerves III (oculomotor nerve), IV (trochlear nerve), V1 (ophthalmic nerve), V2 (maxillary nerve), and VI (abducens nerve)41.
Venous hypertension results from the direct transmission of extremely pressured arterial blood into the cavernous sinus and the draining veins via a CCF. The clinical manifestation of CCF is a direct result of increased intracavernous pressure and altered flow patterns. The size, as well as the exact position, duration, sufficiency, and route of venous drainage, along with the existence of arterial/venous collaterals, are all factors that affect the clinical characteristics of CCFs33.
Exophthalmos, bruit, and conjunctival chemosis are the classic Dandy’s triad symptoms that signify a direct, high-flow CCF. Although the full clinical trial is not always present, the majority of patients have proptosis (90%), chemosis (90%), diplopia (50%), cephalic bruit (25%), pain (25%), trigeminal nerve dysfunction, high intraocular pressure, and vision loss (up to 50%) upon presentation35.
Elevated pressure in the veins that drain the orbit may result in secondary glaucoma, orbital venous congestion. Increased intraocular pressure and intravenous pressure can compromise retinal perfusion, which will drastically reduce visual acuity33. One of the most concerning CCF complications is visual loss, which requires urgent medical attention. Subconjunctival hemorrhages can be noticed as a result of dilated arterialized veins rupturing, and increased corneal exposure can also harm the cornea. In about 5% of patients, intracranial hemorrhage occurs; this is likely caused by altered venous drainage into the sphenoparietal sinus with obstruction of other drainage channels, which leads to cerebral cortical venous hypertension5,35.
Indirect CCFs frequently lack the traditional triad of symptoms. Indirect CCFs do not present with symptoms as abruptly as do direct CCFs. Insidiously developing symptoms and indicators of indirect CCFs include proptosis, conjunctival injection, or progressive glaucoma in the majority of patients5,29,35,39,40,42. The hallmark of dural CCFs is exacerbation and remission of signs and symptoms, which may be caused by cavernous sinus thromboses and rerouting of venous flow in different directions35.
Diagnosis
In the initial work-up of a potential CCF, noninvasive imaging techniques such computed tomography (CT), magnetic resonance (MR), CT angiography, MR angiography, and Doppler are frequently employed.
A CT scan of the orbit typically shows the afflicted eyeball proptosed, the extraocular muscles enlarged, the superior ophthalmic vein (SOV) dilated and tortuously twisted, and the ipsilateral cavernous sinus enlarged. With ocular edema and aberrant flow voids in the afflicted cavernous sinus, MR imaging results in CCFs are comparable to those seen on CT5,32,35.
The gold standard for endovascular intervention planning, classification, and conclusive diagnosis of CCFs is cerebral angiography (Fig. 10). It does allow a detailed identification of the size and location of the fistula, the distinction between direct and indirect lesions, the presence of any associated cavernous carotid aneurysms, the presence of complete or partial stealing phenomena, as well as the assessment of the global cortical arterial circulation and collateral flow through the circle of Willis.
Figure 10.

Carotid cavernous fistula on digital subtraction angiography.
Color Doppler study can measure flow direction and velocity, identifying the arterial flow in the orbital veins in CCF instances43. The SOV’s flow reversal suggests a CCF.
Treatment
Conservative management
Due to additional thrombosis of the affected cavernous sinus segment, spontaneous resolution of dural fistulas can occasionally take place within days to months following clinical presentation. As a result, it is standard practice to treat the patient’s ocular symptoms medically. This includes prism therapy or patching for diplopia, topical beta-blockers and acetazolamide for elevated intraocular pressure, lubrication for proptosis-related keratosis, and/or systemic corticosteroids as necessary.
As a further noninvasive treatment for indirect CCFs, manual external carotid-jugular compression therapy may be started5. By reducing arterial intake while concurrently increasing outlet venous pressure and encouraging spontaneous thrombosis within the fistula, compression therapy seeks to temporarily reduce arteriovenous shunting44.
Surgical intervention
Surgery interventions can include stereotactic radiosurgery and endovascular therapy.
Stereotactic radiosurgery
For the treatment of CCFs, stereotactic radiosurgery has become a viable alternative therapy option and has been studied in numerous institutions. Gamma knife radiosurgery can be utilized as a stand-alone procedure or as a follow-up treatment after endovascular intervention45,46 The 22 months average delay between treatment and full symptom relief is a significant downside, even if preliminary results indicate that radiosurgery is a safe and effective alternative treatment for indirect CCFs42. Moreover, the use of radiosurgery as a first-line treatment is hindered by the inability to manage crises and traumatic fistulae35.
Endovascular approach
There are two routes for the endovascular approach.
Arterial route
Indirect low-flow CCF trans-arterial embolization is typically difficult due to the small size, intricate architecture, and numerous artery feeders. Also, the decision to use the trans-arterial method as the major therapy of spontaneous indirect CCFs is constrained by potential side effects (such as thromboembolic stroke, cranial nerve palsies, etc.). Thus, for high-flow indirect CCFs, trans-arterial embolization is normally only utilized to decrease arterial inflow prior to trans-venous occlusion and as a workable alternative when trans-venous attempts fail5,35.
Indirect CCFs that are traumatic are managed differently than those that are spontaneous. Trans-arterial embolization may be chosen for traumatic lesions because the single artery supply is large enough to provide microcatheter access to the feeder and cavernous sinus. The trans-venous technique is only used when the fistula fails or recurs and arterial access to the site of the fistula cannot be achieved47.
The tiny meningeal branches supplying the fistula are distally catheterized using trans-arterial methods (Fig. 11). The microcatheter tip should be positioned as close to the point of fistulous communication as is practical when inserting the super selective microcatheter. In order to occlude the fistulous connections and penetrate the cavernous sinus, liquid embolic agents (n-BCA, EVOH) are injected under fluoroscopic supervision once a suitable microcatheter position has been attained. Coils and particle agents have been utilized, but by themselves, they are unable to permanently occlude the fistula5.
Figure 11.
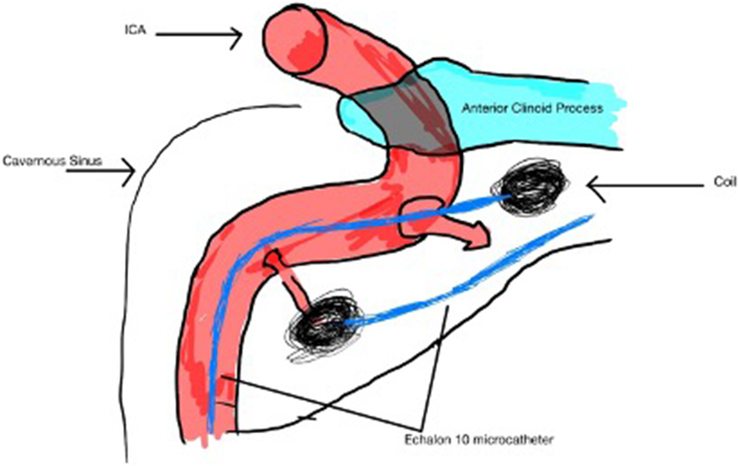
Trans arterial embolization of carotid-cavernous sinus fistula.
Venous route
Via inferior petrosal sinus
Because the IPS is directly connected to the internal jugular vein (IJV) through the petro-occipital fissure, access to the CS through the ipsilateral IPS is typically favored. It is typically viable to maneuver a microcatheter into the anterior region of the CS to approach the junction between the SOV and CS after securely inserting it into the posterior part of the CS.
Via superior ophthalmic vein
The attempt to approach by SOV can be taken into consideration if the ipsilateral or contralateral IPS approach fails. There are typically two ways to access the CS through the SOV: a direct per-cutaneous SOV approach and a trans-femoral SOV technique using the facial vein48.
Other trans-venous approaches
Other accesses may also be taken into consideration if all of the aforementioned methods prove unsuccessful. The frontal vein, superficial temporal vein, and facial vein have all been directly cannulated, according to some publications49. Rare cases of direct cannulation of the superficial middle cerebral vein following endovascular and open craniotomy surgery have been documented50.
Prognosis
Although ocular symptoms subside quickly after successful treatment, patients may experience a brief increase in symptoms as a result of thrombus spreading across the cavernous sinus and into the SOV. With trans-arterial embolization, gamma knife radiosurgery, or conservative treatment, patients may experience what is known as the “paradoxical worsening phenomena.” Although troubling to the patient, such symptoms typically go away on their own with time. Inflammation linked to sinus thrombosis may be reduced with a brief course of corticosteroids29,51.
Conclusion
A carotid-cavernous fistula is a rare entity and often misdiagnosed due to its overlapping symptoms with modalities such as cavernous sinus thrombosis. In order to diagnose and treat such CCF situations, a thorough approach is necessary. For the diagnosis and categorization of CCF, cerebral angiography continues to be the gold standard. The primary line of treatment is still trans-venous endovascular therapy. The trans-arterial technique is another excellent choice with the development of emboli agents. After receiving neuro-vascular treatment for CCF, there is a higher success rate and full symptom remission.
Ethical approval
Not applicable.
Consent
Consent was obtained by the patient in this study. The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Source of funding
Not applicable.
Author contribution
All authors have equal contribution.
Conflicts of interest disclosure
The authors declare no conflicts of interest.
Research registration unique identifying number (UIN)
None.
Guarantor
Bipin Chaurasia.
Data availability statement
None.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Ruchit Jain, Email: ruchit.jain16@gmail.com.
Nitin Jagdhane, Email: drjagdhane@gmail.com.
Sameer Deshmukh, Email: samdeshmukh74@gmail.com.
Stefano M. Priola, Email: spriola@nosm.ca.
Vishal Chavda, Email: chavdavishal2@gmail.com.
Bipin Chaurasia, Email: trozexa@gmail.com.
References
- 1. Henderson AD, Miller NR. Carotid-cavernous fistula: current concepts in aetiology, investigation, and management. Eye Lond Engl 2018;32:164–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Al-Mufti F, Amuluru K, El-Ghanem M, et al. Spontaneous bilateral carotid-cavernous fistulas secondary to cavernous sinus thrombosis. Neurosurgery 2017;80:646–654. [DOI] [PubMed] [Google Scholar]
- 3. Khan S, Gibbon C, Johns S. A rare case of bilateral spontaneous indirect caroticocavernous fistula treated previously as a case of conjunctivitis. Ther Adv Ophthalmol 2018;10:2515841418788303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lang M, Habboub G, Mullin JP, et al. A brief history of carotid-cavernous fistula. J Neurosurg 2017;126:1995–2001. [DOI] [PubMed] [Google Scholar]
- 5. Gemmete JJ, Ansari SA, Gandhi D. Endovascular treatment of carotid cavernous fistulas. Neuroimaging Clin N Am 2009;19:241–255. [DOI] [PubMed] [Google Scholar]
- 6. Miller NR. Diagnosis and management of dural carotid-cavernous sinus fistulas. Neurosurg Focus 2007;23:E13. [DOI] [PubMed] [Google Scholar]
- 7. Sohrabi C, Mathew G, Maria N, et al. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl 2023;109:1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ngnitewe Massa R, Minutello K, Mesfin FB. Neuroanatomy, Cavernous Sinus. StatPearls [Internet]. StatPearls Publishing; 2023. [PubMed] [Google Scholar]
- 9. Graffeo CS, Perry A, Copeland WR, et al. Histology of the distal dural ring. Clin Anat N Y N 2017;30:742–746. [DOI] [PubMed] [Google Scholar]
- 10. Geibprasert S, Pongpech S, Armstrong D, et al. Dangerous extracranial-intracranial anastomoses and supply to the cranial nerves: vessels the neurointerventionalist needs to know. AJNR Am J Neuroradiol 2009;30:1459–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ellis JA, Goldstein H, Connolly ES, et al. Carotid-cavernous fistulas. Neurosurg Focus 2012;32:E9. [DOI] [PubMed] [Google Scholar]
- 12. Kashiwagi S, Tsuchida E, Goto K, et al. Balloon occlusion of a spontaneous carotid-cavernous fistula in Ehlers-Danlos syndrome type IV. Surg Neurol 1993;39:187–190. [DOI] [PubMed] [Google Scholar]
- 13. Masson-Roy J, Savard M, Mackey A. Carotid cavernous fistula in a patient with type IV Ehlers-Danlos syndrome. Can J Neurol Sci J Can Sci Neurol 2017;44:427–428. [DOI] [PubMed] [Google Scholar]
- 14. Schievink WI, Piepgras DG, Earnest F, et al. Spontaneous carotid-cavernous fistulae in Ehlers-Danlos syndrome Type IV. Case report. J Neurosurg 1991;74:991–998. [DOI] [PubMed] [Google Scholar]
- 15. Ono K, Oishi H, Tanoue S, et al. Direct carotid-cavernous fistulas occurring during neurointerventional procedures. Interv Neuroradiol J Peritherapeutic Neuroradiol Surg Proced Relat Neurosci 2016;22:91–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kupersmith MJ, Berenstein A, Flamm E, et al. Neuroophthalmologic abnormalities and intravascular therapy of traumatic carotid cavernous fistulas. Ophthalmology 1986;93:906–912. [DOI] [PubMed] [Google Scholar]
- 17. Barr JD, Mathis JM, Horton JA. Iatrogenic carotid-cavernous fistula occurring after embolization of a cavernous sinus meningioma. AJNR Am J Neuroradiol 1995;16:483–485. [PMC free article] [PubMed] [Google Scholar]
- 18. Guglielmi G, Viñuela F, Duckwiler G, et al. High-flow, small-hole arteriovenous fistulas: treatment with electrodetachable coils. AJNR Am J Neuroradiol 1995;16:325–328. [PMC free article] [PubMed] [Google Scholar]
- 19. Kuether TA, O’Neill OR, Nesbit GM, et al. Direct carotid cavernous fistula after trigeminal balloon microcompression gangliolysis: case report. Neurosurgery 1996;39:853–855. [DOI] [PubMed] [Google Scholar]
- 20. Dolenc VV, Lipovsek M, Slokan S. Traumatic aneurysm and carotid-cavernous fistula following transsphenoidal approach to a pituitary adenoma: treatment by transcranial operation. Br J Neurosurg 1999;13:185–188. [DOI] [PubMed] [Google Scholar]
- 21. Song IC, Bromberg BE. Carotid-cavernous sinus fistula occurring after a rhinoplasty. Case report. Plast Reconstr Surg 1975;55:92–96. [DOI] [PubMed] [Google Scholar]
- 22. Lister JR, Sypert GW. Traumatic false aneurysm and carotid-cavernous fistula: a complication of sphenoidotomy. Neurosurgery 1979;5:473–475. [DOI] [PubMed] [Google Scholar]
- 23. Pedersen RA, Troost BT, Schramm VL. Carotid-cavernous sinus fistula after external ethmoid-sphenoid surgery. Clinical course and management. Arch Otolaryngol Chic Ill 1960 1981;107:307–309. [DOI] [PubMed] [Google Scholar]
- 24. Reilly JJ, Caparosa RJ, Latchaw RE, et al. Aberrant carotid artery injured at myringotomy. Control of hemorrhage by a balloon catheter. JAMA 1983;249:1473–1475. [PubMed] [Google Scholar]
- 25. Feuerman TF, Hieshima GB, Bentson JR, et al. Carotid-cavernous fistula following nasopharyngeal biopsy. Arch Otolaryngol Chic Ill 1960 1984;110:412–414. [DOI] [PubMed] [Google Scholar]
- 26. Habal MB. A carotid cavernous sinus fistula after maxillary osteotomy. Plast Reconstr Surg 1986;77:981–987. [PubMed] [Google Scholar]
- 27. Miller NR, Walsh FB, Hoyt WF. Walsh and Hoyt’s Clinical Neuro-ophthalmology. Lippincott Williams & Wilkins; 2005:1190. [Google Scholar]
- 28. Debrun GM, Viñuela F, Fox AJ, et al. Indications for treatment and classification of 132 carotid-cavernous fistulas. Neurosurgery 1988;22:285–289. [DOI] [PubMed] [Google Scholar]
- 29. Meyers PM, Halbach VV, Dowd CF, et al. Dural carotid cavernous fistula: definitive endovascular management and long-term follow-up. Am J Ophthalmol 2002;134:85–92. [DOI] [PubMed] [Google Scholar]
- 30. Coskun O, Hamon M, Catroux G, et al. Carotid-cavernous fistulas: diagnosis with spiral CT angiography. AJNR Am J Neuroradiol 2000;21:712–716. [PMC free article] [PubMed] [Google Scholar]
- 31. Barrow DL, Spector RH, Braun IF, et al. Classification and treatment of spontaneous carotid-cavernous sinus fistulas. J Neurosurg 1985;62:248–256. [DOI] [PubMed] [Google Scholar]
- 32. Tjoumakaris SI, Jabbour PM, Rosenwasser RH. Neuroendovascular management of carotid cavernous fistulae. Neurosurg Clin N Am 2009;20:447–452. [DOI] [PubMed] [Google Scholar]
- 33. Connors JJ. Interventional neuroradiology: strategies and practical techniques. No Title [Internet]. [cited 2023 Aug 10]; Available from: https://cir.nii.ac.jp/crid/1130282269406885120
- 34. Tomsick TA. Type A (direct) CCF: etiology, prevalence, and natural history Tomsick TA. Carotid cavernous sinus fistula. Digital Education Publishing; 1997:35–38. [Google Scholar]
- 35. Ringer AJ, Salud L, Tomsick TA. Carotid cavernous fistulas: anatomy, classification, and treatment. Neurosurg Clin N Am 2005;16:279–295; viii. [DOI] [PubMed] [Google Scholar]
- 36. Wanke I, Doerfler A, Stolke D, et al. Carotid cavernous fistula due to a ruptured intracavernous aneurysm of the internal carotid artery: treatment with selective endovascular occlusion of the aneurysm. J Neurol Neurosurg Psychiatry 2001;71:784–787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Germain DP, Herrera-Guzman Y. Vascular Ehlers-Danlos syndrome. Ann Genet 2004;47:1–9. [DOI] [PubMed] [Google Scholar]
- 38. Debrun GM. Angiographic workup of a carotid cavernous sinus fistula (CCF) or what information does the interventionalist need for treatment? Surg Neurol 1995;44:75–79. [DOI] [PubMed] [Google Scholar]
- 39. Zhang Y, Zheng H, Zhou M, et al. Teaching neuroimages: carotid-cavernous fistula caused by fibromuscular dysplasia. Neurology 2014;82:e134–e135. [DOI] [PubMed] [Google Scholar]
- 40. Taki W, Nakahara I, Nishi S, et al. Pathogenetic and therapeutic considerations of carotid-cavernous sinus fistulas. Acta Neurochir (Wien) 1994;127:6–14. [DOI] [PubMed] [Google Scholar]
- 41. Kohli GS, Patel BC. Carotid Cavernous Fistula. StatPearls [Internet]. StatPearls Publishing; 2023. [cited 2023 Aug 10]. Available from http://www.ncbi.nlm.nih.gov/books/NBK535409/ [PubMed] [Google Scholar]
- 42. Quiñones D, Duckwiler G, Gobin PY, et al. Embolization of dural cavernous fistulas via superior ophthalmic vein approach. AJNR Am J Neuroradiol 1997;18:921–928. [PMC free article] [PubMed] [Google Scholar]
- 43. de Keizer R. Carotid-cavernous and orbital arteriovenous fistulas: ocular features, diagnostic and hemodynamic considerations in relation to visual impairment and morbidity. Orbit Amst Neth 2003;22:121–142. [DOI] [PubMed] [Google Scholar]
- 44. McConnell KA, Tjoumakaris SI, Allen J, et al. Neuroendovascular management of dural arteriovenous malformations. Neurosurg Clin N Am 2009;20:431–439. [DOI] [PubMed] [Google Scholar]
- 45. Link MJ, Coffey RJ, Nichols DA, et al. The role of radiosurgery and particulate embolization in the treatment of dural arteriovenous fistulas. J Neurosurg 1996;84:804–809. [DOI] [PubMed] [Google Scholar]
- 46. Koebbe CJ, Singhal D, Sheehan J, et al. Radiosurgery for dural arteriovenous fistulas. Surg Neurol 2005;64:392–398. [DOI] [PubMed] [Google Scholar]
- 47. Luo CB, Teng MMH, Chang FC, et al. Traumatic indirect carotid cavernous fistulas: angioarchitectures and results of transarterial embolization by liquid adhesives in 11 patients. Surg Neurol 2009;71:216–222. [DOI] [PubMed] [Google Scholar]
- 48. Lee JM, Park ES, Kwon SC. Endovascular management of cavernous sinus dural arteriovenous fistulas: overall review and considerations. J Cerebrovasc Endovasc Neurosurg 2021;23:293–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Matsumoto A, Okauchi M, Shindo A, et al. Cavernous sinus dural arteriovenous fistula treated by facial vein direct puncture: case report and review of the literature. Interv Neuroradiol 2017;23:301–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Venturi C, Bracco S, Cerase A, et al. Endovascular treatment of a cavernous sinus dural arteriovenous fistula by transvenous embolisation through the superior ophthalmic vein via cannulation of a frontal vein. Neuroradiology 2003;45:574–578. [DOI] [PubMed] [Google Scholar]
- 51. Akamatsu Y, Sato K, Endo H, et al. Single-session hematoma removal and transcranial coil embolization for a cavernous sinus dural arteriovenous fistula: a technical case report. World Neurosurg 2017;104:1046.e7–1046.e12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
None.