Abstract
Introduction and importance:
Odontoid fractures of the second cervical vertebra (C2) are categorized into three types, with type III extending into the body of the axis. These fractures, often resulting from high-energy trauma, can cause significant instability and neurological issues. This case report discusses a 43-year-old male with a type III odontoid fracture and C1–C2 fracture dislocation, demonstrating the effectiveness of traditional neurosurgical techniques in managing such complex injuries.
Case presentation:
A 43-year-old male presented with upper cervical pain and right upper limb weakness following a road traffic accident. Imaging revealed a type III odontoid fracture with posterior displacement and atlanto-axial (C1–C2) joint dislocation. The patient underwent a two-stage surgical procedure. The first stage involved transoral decompression to address the retropulsed odontoid fragment and relieve spinal cord compression. The second stage involved posterior craniocervical fixation using an autologous iliac bone graft for stabilization. The patient showed postoperative improvement and was discharged on the third day, with a stable condition at a one-month follow-up.
Clinical discussion:
Managing type III odontoid fractures with C1–C2 dislocation is challenging, requiring a strategic approach to ensure spinal stability and neurological recovery. Transoral decompression provides direct access for effective decompression, while posterior fixation ensures robust stabilization. The use of an autologous iliac bone graft enhances fusion and long-term stability. This case illustrates the successful integration of traditional neurosurgical techniques with modern surgical principles.
Conclusion:
This case underscores the importance of traditional neurosurgical techniques in managing complex odontoid fractures. The two-stage approach of transoral decompression followed by posterior craniocervical fixation proved effective, highlighting the relevance of these techniques in achieving positive outcomes in contemporary neurosurgical practice.
Keywords: C1–C2 fracture dislocation, odontoid fracture, posterior craniocervical fixation, traditional neurosurgical techniques, transoral decompression
Introduction
Highlights
-
Case overview:
A 43-year-old male with a type III odontoid fracture and C1–C2 fracture dislocation following a road traffic accident.
-
Symptoms and initial findings:
Presented with upper cervical pain and right upper limb weakness.
Imaging revealed posterior displacement of the odontoid process and atlanto-axial joint dislocation.
-
Surgical approach:
A two-stage procedure: transoral decompression followed by posterior craniocervical fixation using an autologous iliac bone graft.
-
Postoperative results:
Significant postoperative improvement with the patient discharged on the third day.
Follow-up at one month showed a stable condition with normal limb power.
-
Clinical significance:
Emphasizes the effectiveness of traditional neurosurgical techniques in managing complex spinal injuries.
Highlights the continued relevance of these techniques, particularly in resource-limited settings.
-
Educational value:
Provides a detailed account of the surgical procedure and decision-making process, offering valuable insights for neurosurgeons and spine surgeons.
The odontoid process, also known as the dens, is a superior projecting bony element that originates from the second cervical vertebrae (C2, or the axis). The first cervical vertebrae (atlas) rotate around the odontoid process to produce the most significant single component of cervical spine lateral rotation. Odontoid process fractures are categorized into three categories according to their location and morphology: type I—Avulsion fracture of the tip of the dens (usually stable), type II—Fracture of the base of the dens (considered unstable), and type III—Fracture at the junction of the dens and the body of C21. Odontoid fractures develop because of cervical spine trauma. They are usually the outcome of high-energy trauma, such as road traffic accidents. Nevertheless, low-energy impacts, such as falls from a standing posture, can cause trauma in the geriatric population2. The most prevalent mechanism of injury is cervical spine hyperextension, which pushes the head and C1 vertebrae backward. If the energy mechanism and associated force are strong enough (or the patient’s bone density is weakened due to osteopenia/osteoporosis), the odontoid will fracture with different degrees of displacement and comminution. Odontoid fractures can also occur because of cervical spine hyperflexion. The transverse ligament attaches to the lateral mass of C1 on either side and travels dorsal to (behind) the odontoid process. When the cervical spine is too flexed, the transverse ligament can transmit excessive anterior stresses to the odontoid process, resulting in an odotoid fracture1. Odontoid fractures are managed conservatively if stable and surgically if unstable. Different types of surgery used for the management of odontoid fractures depend on the type of fracture, such as anterior odontoid screw fixation, posterior C1–C2 fusion, and transarticular screw fixation. In this paper, we present a case report of two-stage surgical management for type III odontoid fracture with C1–C2 fracture dislocation.
Potential risks and complications, include neurological injury, infection, non-union, hardware failure, vascular injury, dysphagia, respiratory issues.
Case report
A 43-year-old male patient arrived at the neurotrauma unit after being involved in a road traffic accident, reporting pain in the upper cervical region and weakness in the right upper limb. With no significant past medical or surgical history, the patient’s vital signs were stable upon examination. Tenderness was noted in the upper cervical spine, and his Glasgow Coma Scale (GCS) score was 15/15. While the power of the right upper limb measured 4/5 BMRC, the power in the lower limb and left upper limb was 5/5 BMRC. Given these findings, a Philadelphia cervical collar was promptly applied, and a CT scan of the cervical spine, including the craniocervical junction, was recommended. The subsequent CT scan revealed a fracture of the odontoid of the axis with retropulsion (Figs. 1–3). Further evaluation through MRI of the cervical spine exhibited compression of the thecal sac and cord at the C2 level (Fig. 4).
Figure 1.
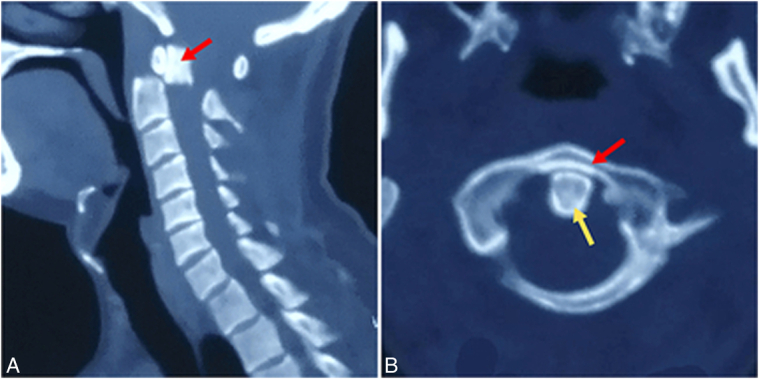
(A) Sagittal view of the cervical spine computed tomography scan with craniocervical junction showing a fracture of the odontoid process (red arrow) with retropulsion. (B) Axial view of the atlas vertebra (red arrow) with the odontoid (yellow arrow) showing the odontoid process in place in relation to the C2 vertebral arch.
Figure 3.
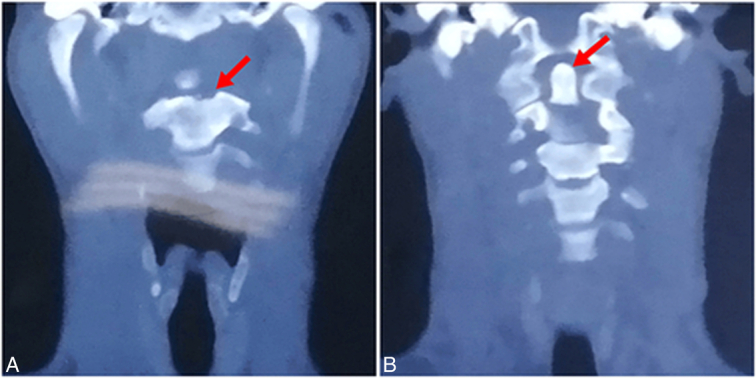
Coronal view of the computed tomography scan showing fracture of the body of the axis indicated by the red arrow (A) and retropulsion of the odontoid fracture indicated by the red arrow (B).
Figure 4.
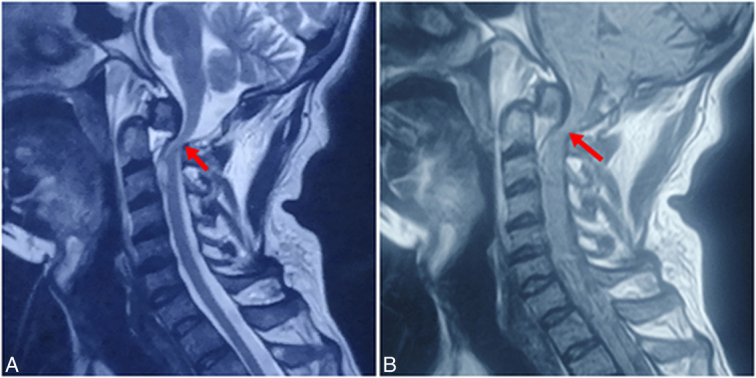
Sagittal view of the cervical spine MRI with the craniocervical junction, T2-weighted image (T2WI) (A), and T1-weighted image (T1WI) (B) showing compression of the spinal cord (red arrows) at the level of C1 and C2 vertebrae.
Figure 2.
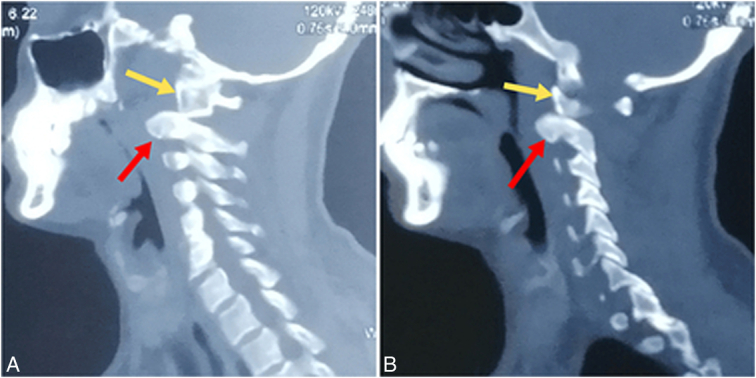
Sagittal view of the computed tomography scan showing dislocation of the atlanto-axial joint on the right side (A) and on the left side (B). The red arrow indicates the axis, while the yellow arrow indicates the atlas, both displaying the dislocation of the joint.
Differential diagnosis:
Traumatic cervical spine injury with odontoid fracture and cord compression.
C1–C2 fracture dislocation.
Investigations:
CT scan of the cervical spine with craniocervical junction.
MRI of the cervical spine.
Treatment: The decision was made to proceed with a transoral approach. A Boyle Davis mouth gag with a tongue plate was employed to open the mouth, and the level was confirmed using a C-arm fluoroscope. A midline linear incision was made using monopolar diathermy. Decompression of the C1–C2 level spinal cord began with the removal of the atlas arch ~1.5 mm from the midline (total 3 mm). Subsequently, an odontoidectomy was performed, successfully removing free bony pieces. The wound was meticulously closed with 2.0 Vicryl. Postoperatively, mild cervical traction of 1.5 kg with Gardner Wells tong was applied. On the subsequent day, the patient’s right upper limb showed improvement from 4/5 to 4+/5. Following this progress, surgery was performed on the second postoperative day to fixate the occipital bone to the spinous process of the axis. This involved utilizing an autologous bone graft from the patient’s iliac crest, secured with surgical wire of 20 (gauge) L arch size (refers to the wire’s shape, designed to fit the lower dental or jaw arch) (Fig. 5). The wound was closed in layers, a drain was placed, and the skull traction was removed at the end of the surgery. An X-ray was performed on the second postoperative day (Fig. 6).
Figure 5.
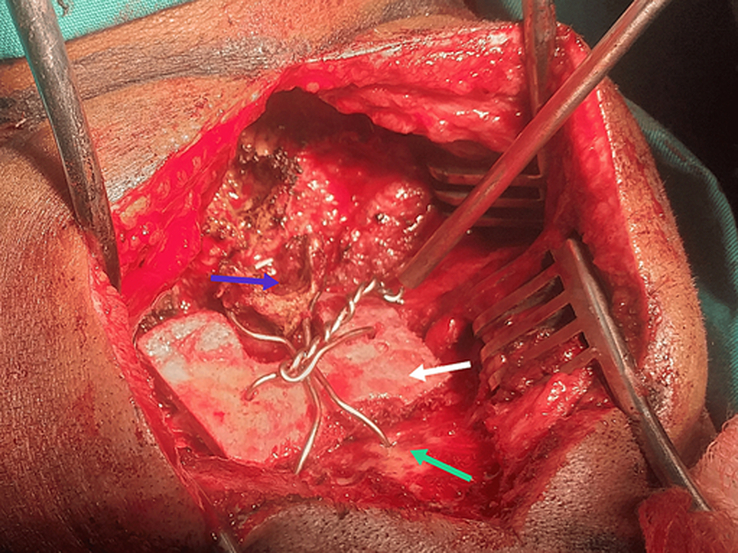
Intraoperative image depicting fixation of the C2 spinous process (blue arrow) to the occipital bone (green arrow) achieved through the utilization of an autologous iliac bone graft (white arrow) and surgical wire.
Figure 6.
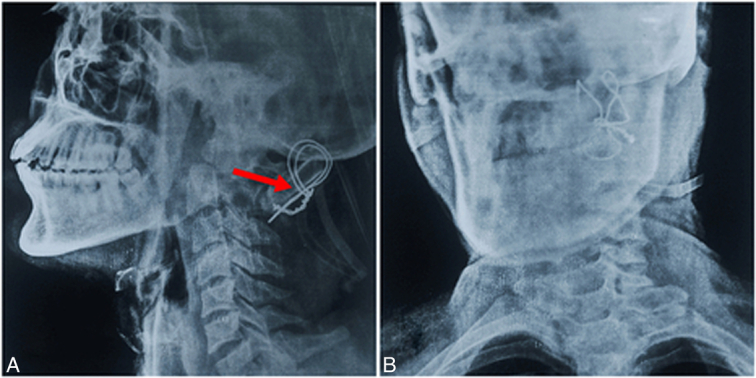
Postoperative X-ray, lateral view (A) and anterior-posterior view (B), displaying the iliac bone graft (red arrow) and the surgical wire in place.
Outcome
The patient was discharged on the third postoperative day with 4+/5 power in the right upper limb.
Follow-up: At the 1-month follow-up, the patient remained vitally stable with normal power (5/5) in all four limbs. A CT scan of the cervical spine with craniocervical junction was advised for further evaluation (Fig. 7). After the 6-month follow-up, the patient was fine. The work has been reported in line with the SCARE 2023 criteria3.
Figure 7.
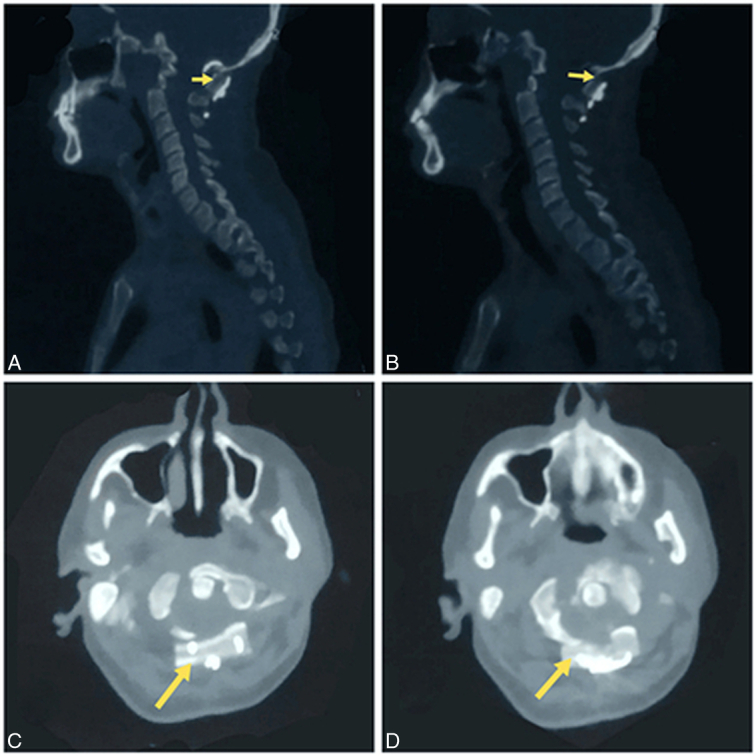
One-month postoperative follow-up computed tomography scan of the cervical spine with craniocervical junction (A, B), along with axial views (C, D), revealing an autologous iliac bone graft (yellow arrows) and demonstrating complete decompression of the spinal canal.
Discussion and results
Injuries to the upper cervical spine are often associated with high-energy trauma and are more prevalent in the elderly population, commonly resulting from incidents like sports accidents, car crashes, and falls4,5. These fractures frequently occur in the atlanto-axial joint, which is particularly vulnerable. Acute dislocation of the C1–C2 joint is rare in adults but poses a significant risk to life when it does occur. The injury typically involves damage to numerous ligaments at the junction, which can be compounded if adjacent non-vital tissues such as bones or muscles are also injured. The complex anatomy of the occipitocervical junction, housing delicate structures like nerve tissue, the spinal cord, lower cranial nerves, and major blood vessels, adds further complexity and concern to these injuries. Type III odontoid fractures, characterized by a fracture at the junction of the dens and the body of C2, are believed to have a high healing potential due to the extensive fracture surface area through cancellous bone. Recent research suggests nonsurgical treatment for Type III odontoid fractures6. However, our case presented a unique fracture pattern not typically described within the classical type III odontoid fracture classification. Various classifications of atlanto-axial joint dislocation have been proposed, typically based on the disrupted anatomical structures, including bone fractures of the atlas and axis, the odontoid process, the C1 arch, and occasionally the articular facets. However, the combination of atlanto-axial and atlantooccipital dislocations is rare, with only two descriptions reported in the literature, both from the same medical center7.
Our case highlights a rare injury in a healthy young adult male following trauma, a presentation more commonly observed in older individuals or those with pre-existing bone pathologies. While surgical management using newer techniques is often reported, resource limitations in low to middle-income countries may necessitate alternative approaches. In our case, surgical treatment involved transoral decompression of comminuted fractured odontoid pieces followed by posterior fixation using the modified Gallie technique in a two-staged procedure. The modified Gallie technique, although described in textbooks, has seen little practical application in young adults in the literature. However, our patient tolerated the procedure well, with favorable fusion outcomes observed immediately post-surgery and at 1-month follow-up. Comparative studies have shown similar fusion rates between the modified Gallie technique and newer screw placement techniques8. It’s crucial for neurosurgeons and spine surgeons to be proficient in both traditional and newer surgical techniques. While advancements in technology continue to shape modern surgical practices, maintaining proficiency in traditional methods, upon which modifications are built, remains invaluable. Passing down these methods to future generations of doctors ensures continuity and familiarity with both traditional and evolving surgical approaches. In conclusion, while we embrace advancements in neurosurgical and spine techniques, it’s imperative not to overlook traditional methods that may still hold relevance, especially in resource-limited settings. Keeping abreast of both traditional and newer techniques ensures versatility and adaptability in addressing the diverse array of clinical scenarios encountered in practice.
This study emphasizes the crucial role of traditional upper cervical spine neurosurgical techniques, particularly in addressing complex cases such as type III odontoid fracture with C1–C2 fracture dislocation. The two-stage surgical approach utilized in this case, involving transoral decompression of the fractured odontoid followed by posterior craniocervical fixation using an autologous iliac bone graft, demonstrated efficacy, and resulted in a successful outcome with positive fusion results. The successful outcome underscores the life-saving potential of these traditional techniques, especially in critical situations where advanced resources may be limited. This case serves as a reminder of the importance for neurosurgeons and spine surgeons to maintain proficiency in both traditional and contemporary surgical methods. While newer techniques often receive attention, this case highlights the enduring value of traditional approaches, which serve as the foundation upon which modifications and advancements are built, particularly in managing complex spinal injuries.
Ethical approval
This case report was compiled after obtaining informed consent from the patient for the disclosure of clinical history and management with the intention of publication. All attached imaging and clinical materials were de-identified to ensure patient anonymity.
Consent
Informed consent was taken from the patient, including permission of printing his images.
Source of funding
This manuscript did not receive any funds.
Author contribution
K.H. and S.A.: conceptualization, data curation, methodology; M.A.W., A.E.A. and A.A.H.: investigation, methodology, resources; B.C.: supervision, validation, visualization, writing—review and editing.
Conflicts of interest disclosure
The authors declare no conflicts of interest disclosure.
Research registration unique identifying number (UIN)
Not applicable.
Guarantor
Bipin Chaurasia.
Data availability statement
Data sharing not applicable—no new data generated, or the article describes entirely theoretical research.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this articles.
Contributor Information
Khitamul Haq, Email: khitam13401@gmail.com.
Saleem Akhter, Email: slimrazasim@gmail.com.
Muhammad A. Waqas, Email: dralisheikh@gmail.com.
Adedoyin E. Alao, Email: alaoadedoyin14@gmail.com.
Abhik Halder, Email: dr.abhikhalder@gmail.com.
Bipin Chaurasia, Email: trozexa@gmail.com.
References
- 1. Robinson AL, Möller A, Robinson Y, et al. C2 fracture subtypes, incidence, and treatment allocation change with age: a retrospective cohort study of 233 consecutive cases. BioMed Res Int 2017;2017:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tenny S, Munakomi S, Varacallo M. Odontoid Fractures In. StatPearls Publishing; 2023. [PubMed] [Google Scholar]
- 3. Sohrabi C, Mathew G, Maria N, et al. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl 2023;109:1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pryputniewicz DM, Hadley MN. Axis fractures. Neurosurgery 2010;66:68. [DOI] [PubMed] [Google Scholar]
- 5. Umana GE, Visocchi M, Scalia G, et al. Minimally invasive percutaneous anterior odontoid screw fixation: institutional experience with a simple and effective technique. J Neurosurg Sci 2022;66:571–575. [DOI] [PubMed] [Google Scholar]
- 6. Silbergeld DL, Laohaprasit V, Grady MS, et al. Two cases of fatal atlantoaxial distraction injury without fracture or rotation. Surg Neurol 1991;35:54–56. [DOI] [PubMed] [Google Scholar]
- 7. Farey ID, Nadkarni S, Smith N. Modified Gallie technique versus transarticular screw fixation in C1-C2 fusion. Clin Orthop 1999;359:126–135. [DOI] [PubMed] [Google Scholar]
- 8. Sebastian RF, Tobing SDAL. Sonntag procedure in Atlanto-odontoid fractures type III in restoring Atlanto-axial complex stability: a case report. Int J Surg Case Rep 2023;110:108545. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable—no new data generated, or the article describes entirely theoretical research.


