Abstract
Background
Prior work evaluated clinician work-related physical activity and found it does not meet recommended requirements. We aimed to assess more fully daily surgeon physical activity and compare it to self-reported activity.
Methods
This multispecialty prospective cohort study included attending surgeons from 14 surgical departments within four French university hospitals. Over a 14-month period (11/01/2020-12/31/2021), surgeons were continuously monitored 24/7 for their daily physical activity by wearing an accelerometer on their ankle. For each surgeon, measured parameters included the daily average of step counts and sedentary time, as well as the total weekly time of physical activity within the 30 days preceding surgeries. Surgeons self-reported the validated Global Physical Activity Questionnaire from the World Health Organization (WHO). The self-reported and measured physical activity of surgeons were described, and their correlation was assessed using Spearman rank correlation.
Results
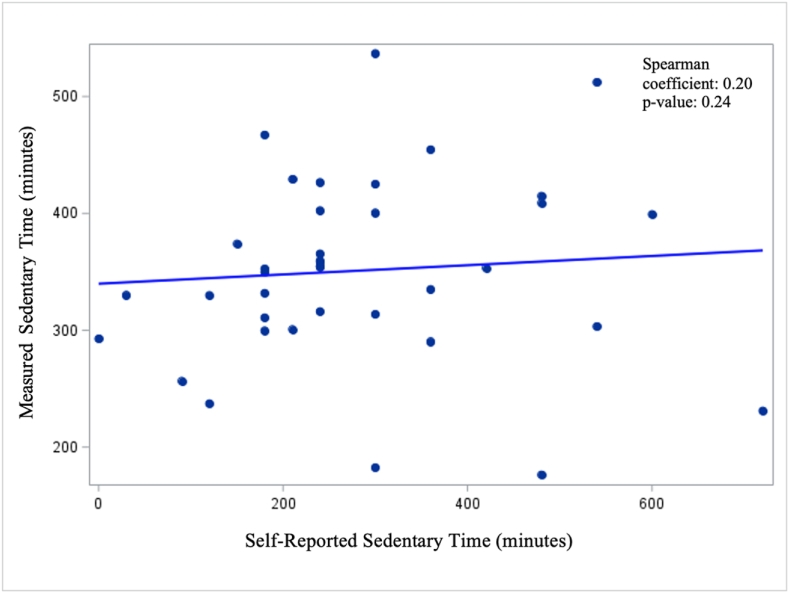
Overall, there were 38 surgeons in the cohort and 8810 surgeries performed. Surgeons were 78.9 % male, median age was 46.1, and median BMI was 24.5. Median measured daily step count was 9439 (IQR: 7238–9918). The measured weekly total time of physical activity was 918 min (95 % CI: 767–990), while the corresponding self-reported median time was 1940 min (95 % CI: 1120–3600) (Spearman coefficient = 0.14, p = 0.41). The measured median daily sedentary time was 353 min (95 % CI: 316–374), compared to a self-reported median of 240 min (95 % CI: 210–300) (Spearman coefficient = 0.20, p = 0.24).
Conclusions
Surgeons may overestimate the sufficiency of their physical activity and underestimate their sedentary time. Increased awareness is needed to improve surgeon wellness.
Keywords: Physical activity, Sedentary time, Surgeon self-report, Measured, Correlation
Highlights
-
•
Evaluated surgeon self-reported physical activity and sedentary time.
-
•
Compared self-report with corresponding objective measurement from an accelerometer.
-
•
Surgeons overestimated physical activity and underestimated sedentary time.
-
•
Increased awareness is needed to improve surgeon wellness.
1. Introduction
Physical activity is important for general health and prevention of disease [1]. Clinicians spend a significant amount of their time working and previous research has evaluated occupational physical activity among clinicians to determine if they perform substantial physical activity while at work [[2], [3], [4], [5]]. Abd et al. found that work-related physical activity among cardiovascular specialists did not meet recommended American Heart Association guidelines (at least 10,000 steps daily) [2]. When looking more generally at clinicians, it was found that both attending physicians and trainees do not meet their 10,000 step goal during working hours [3]. The low levels of occupational physical activity were also confirmed within other physician groups [4,5].
Adequate levels of physical activity are important, but evaluating physical activity can be difficult. It requires the use of either self-reported questionnaires or device-measure of physical activity. In the general population, it has been found that the correlation between self-reported physical activity and measured physical activity is weak [6]. Self-reporting of physical activity suggested that 25–33 % of individuals met physical activity guidelines, but when measured with devices, less than 5 % of the population actually met recommendations [7]. This shows that within the general populations, individuals tend to over-report their physical activity level.
However, it has been found that individuals with higher education have better correlation between their self-reported physical activity time and measured physical activity [8]. Surgeons inherently fall within the high education level group given the extensive schooling required to obtain a medical degree. To date, no studies have evaluated surgeon ability to accurately report their own physical activity and sedentary time and whether this group demonstrates better correlation with measured physical activity. Therefore, we primarily aimed to compare surgeon self-reported physical activity and sedentary time with their device-measured physical activity and sedentary time to evaluate correlation.
2. Methods
2.1. Study population
The cohort of this multicenter, observational study was composed of surgeons operating in fourteen cardiac, endocrine, digestive, gynecologic, orthopedic, thoracic, and urologic surgical departments of four university hospitals in Lyon, France. Surgeons were excluded from the cohort if they were still in training (i.e. assistant specialists, residents, medical students, visiting interns, etc.), conducted less than 50 surgeries per year, or refused to share personal data for the study purpose. All the surgeries conducted by those attending surgeons between November 1, 2020 and 12/31/2021 were considered in analysis.
The study used pseudonymized data in accordance with European General Data Protection Regulation No. 2016/679. The French National Data Protection Authority (DR-2020-055 CNIL) and the European Research Council Executive Agency (801660 ERCEA) approved the study protocol. It was deemed exempt from formal oversight by the Mass General Brigham Institutional Review Board (Protocol 2023P002266). Surgeons gave written informed consent to participate in the study, and for the use of their data.
2.2. Data collection and physical activity assessment
The surgeons completed a survey including demographics questions (gender, BMI, professional status, specialty, commuting methods, monitoring of physical activity parameters) and the validated Global Physical Activity Questionnaire (GPAQ) from the WHO [[9], [10], [11]]. This included questions regarding physical activity and sedentary time. The GPAQ considers vigorous physical activity to be “activities that require hard physical effort and cause large increases in breathing or heart rate”, and moderate physical activity to be “activities that require moderate physical effort and cause small increases in breathing or heart rate”. Total physical activity on the GPAQ is the sum of work-related and recreational moderate and vigorous physical activity, as well as time spent walking or biking as the method of travel to and from places. Sedentary time in minutes per day is defined as time spent sitting or reclining, but not sleeping [12].
To quantify their physical activity, surgeons continuously wore Actigraph wGT3X-BT accelerometers (ActiGraph, Pensacola, FL, USA) on the ankle 24 h a day throughout the entire study period. Accelerometer data was analyzed using ActiLife software (version 6.13.3). A sampling frequency of 30 Hz and an epoch length of 60 s were used. The measured parameters included daily step counts and sedentary time, as well as weekly total physical activity in minutes within the 30 days prior to each of their surgeries during the study period.
Only 30-day periods prior to surgery with ≥17 days of valid accelerometer data were included in the analyses. Non-wear periods were defined as zero counts per minute during ≥180 min. Sedentary time was defined as 0–100 activity counts per minute, and sedentary bouts were defined as periods of uninterrupted sedentary time ≥10 min. Daily sedentary time was calculated as the sum of all sedentary bouts each day. Sleep was not assessed in the current study and we excluded periods either when the surgeon was not consistently wearing the sensor or it was nighttime [13]. Standing time was not explicitly excluded from the analysis, but was likely recorded as light activity by the accelerometer.
2.3. Statistical analysis
Surgeon measured physical activity and sedentary time were recorded daily and then 30-day averages were generated with each operation as the ending point of the 30-day average measure for each surgeon. Mean measured metrics were generated for each surgeon by taking the average of all the 30-day metrics for each operation. Overall, there were 8810 patient operations for the 38 surgeons included in the cohort. The mean metrics were generated for each of the 38 surgeons based on their proportion of the 8810 operations conducted during the study period. This was meant to generate the true average activity and sedentary time for each surgeon, taking into account any potential outlier periods where they may have been more or less active or had more or less sedentary time than their typical.
Descriptive analysis was performed for surgeon demographics, measured and self-reported physical activity and sedentary time. Measured versus self-reported metrics were compared using Spearman rank correlation with weak correlation considered less than 0.4. For all analyses, a two-sided p-value of <0.05 defined statistical significance. All data analyses were conducted using SAS V.9.4 (SAS Institute, Cary, North Carolina, USA).
3. Results
3.1. Surgeon demographics
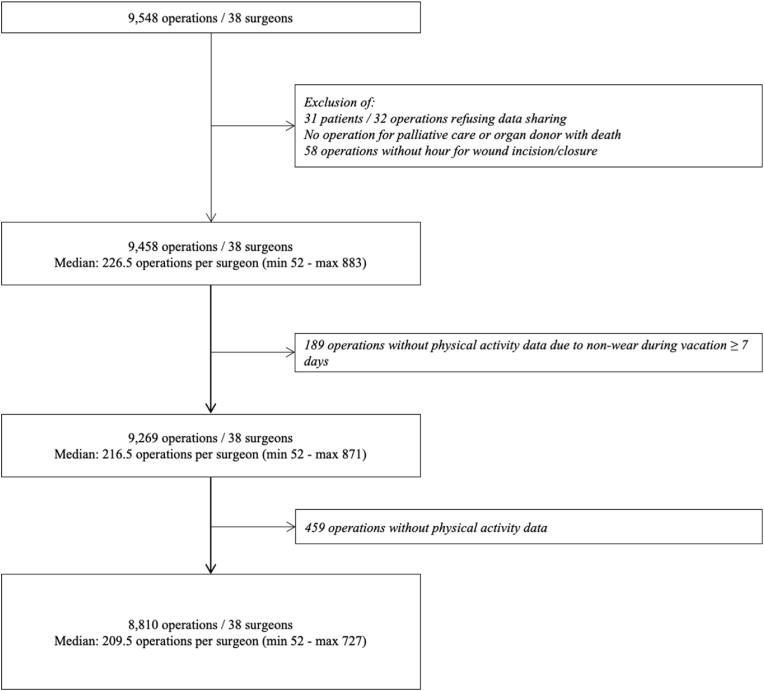
There were 38 surgeons included in the cohort who had measured physical activity metrics Table 1, Fig. 1. Surgeons were predominantly male (78.9 %) and the median age was 46.1. Median BMI was normal at 24.5. Most surgeons were associate-full professors (60.5 %). Surgical specialties were digestive (28.9 %), gynecologic (21.1 %), orthopedic (18.4 %), urologic (13.2 %), cardiac (10.5 %), endocrine (5.3 %), and thoracic (2.6 %). In terms of commuting methods, 33 (86.8 %) surgeons commuted via a motorized vehicle and 10 (26.3 %) via active mobility, such as biking or walking. Ten (26.3 %) surgeons wore smartwatches or smartbands and 9 (23.7 %) surgeons regularly monitored their physical activity parameters.
Table 1.
Surgeon demographics.
| Characteristic (N = 38) | Median (IQR) or N (%) |
|---|---|
| Surgeon Age | 46.1 (39.7–52.5) |
| Gender | |
| Male | 30 (78.9 %) |
| Female | 8 (21.1 %) |
| Surgeon BMI (kg/m2) | 24.5 (22.2–26.4) |
| Professional Status | |
| Associate/Full Professor | 23 (60.5 %) |
| Non-Professor | 15 (39.5 %) |
| Surgeon Specialty | |
| Digestive | 11 (28.9 %) |
| Gynecologic | 8 (21.1 %) |
| Orthopedic | 7 (18.4 %) |
| Urologic | 5 (13.2 %) |
| Cardiac | 4 (10.5 %) |
| Endocrine | 2 (5.3 %) |
| Thoracic | 1 (2.6 %) |
| Commute home/work via motorized vehicle | 33 (86.8 %) |
| Commute home/work via active mobility (bike/walk) | 10 (26.3 %) |
| Daily commute time (minutes), missing = 2 | 40 (27.5–67.5) |
| Wear smartwatch/smartband | 10 (26.3 %) |
| Regularly monitors physical activity parameters | 9 (23.7 %) |
| Self-reported weekly physical activity time (minutes) | 1940 (960–4320) |
| Self-reported daily sedentary time (minutes) | 240 (180–360) |
Fig. 1.
Flow chart of Included Patients.
3.2. Self-Reported and measured metrics
Surgeons reported a median time of physical activity per week as 1940 min. Thirty (78.9 %) surgeons reported that their level of physical activity was sufficient. When considering sedentary time, surgeons reported a median time of 240 min per day. Similarly, 30 (78.9 %) surgeons reported that their daily amount of sedentary time was appropriate, with only 8 surgeons reporting it was excessive [Table 1].
The median measured average daily step counts over the 30-day period for each surgeon were 9439 steps (IQR: 7238–9918). Median average total physical activity over the 30-day period was 918 min (IQR: 721–1048). The median average daily sedentary time over the 30-day period was 353 min (IQR: 303–403).
3.3. Comparison between surgeon Self-Report versus measured metrics
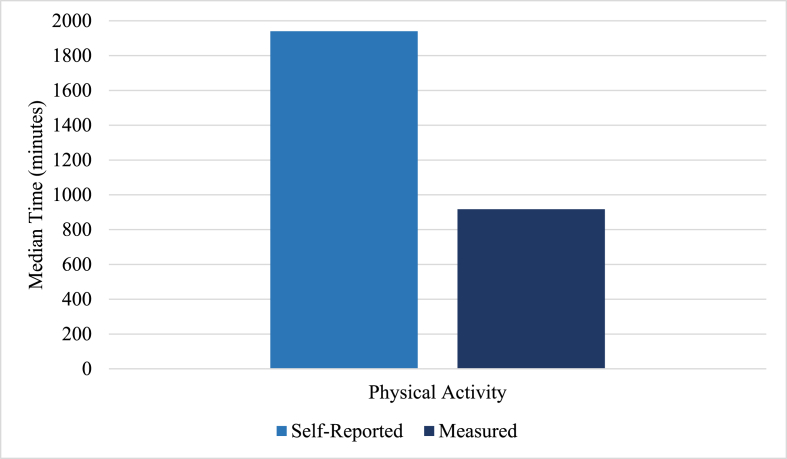
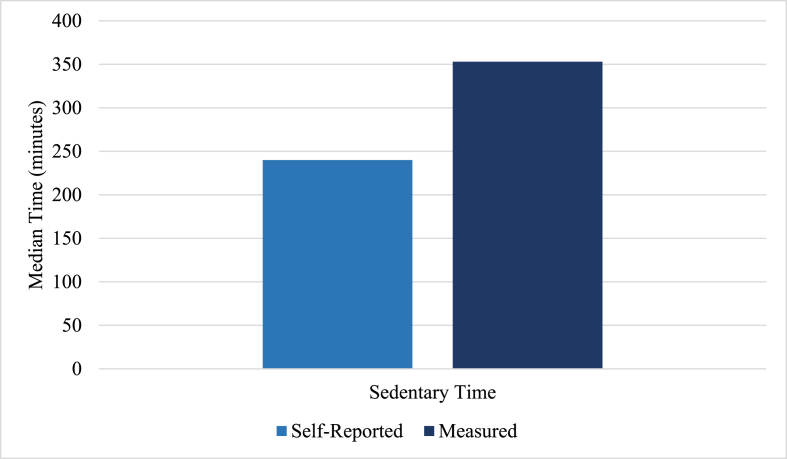
When comparing median self-reported physical activity time versus measured, surgeons overestimated their amount of physical activity. Surgeons self-reported a median of 1940 (95 % CI: 1120–3600) minutes of physical activity, as compared to their median measured physical activity of 918 (95 % CI: 767–990) minutes [Fig. 2a]. However, when comparing the median self-reported versus measured sedentary time, surgeons underestimated their amount of sedentary time. They reported a median sedentary time of 240 (95 % CI: 210–300) minutes, as compared to their median measured sedentary time of 353 (95 % CI: 316–374) minutes [Fig. 2b].
Fig. 2a.
Comparison of surgeon self-reported weekly physical activity to measured.
Fig. 2b.
Comparison of surgeon self-reported daily sedentary time to measured.
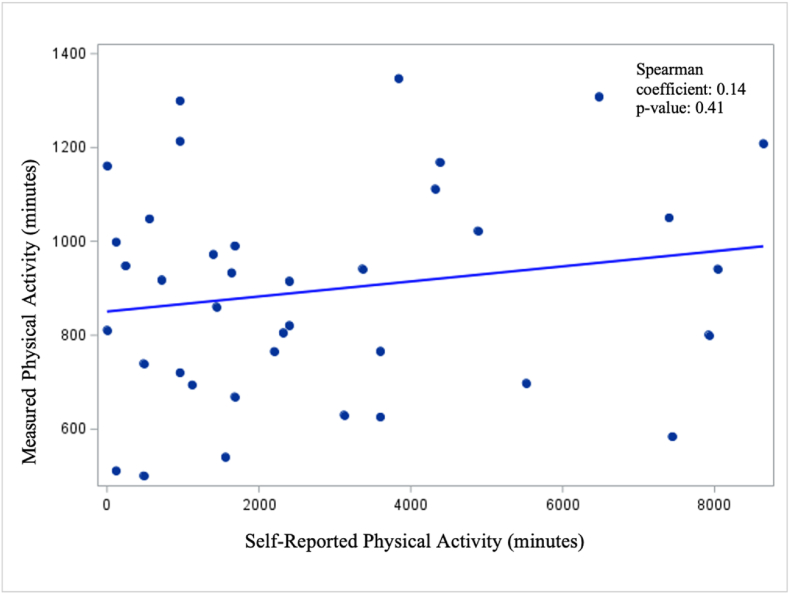
The correlation between surgeon self-report of their sedentary and physical activity time with their actual measured time are shown in Fig. 3a, Fig. 3b. There was no significant correlation between surgeon self-reported and measured physical activity time (Spearman coefficient = 0.1, p-value = 0.4) [Fig. 3a], nor between surgeon self-reported and measured sedentary time (Spearman coefficient = 0.2, p-value = 0.2) [Fig. 3b].
Fig. 3a.
Correlation between surgeon self-reported weekly physical activity and measured physical activity.
Fig. 3b.
Correlation between surgeon self-reported daily sedentary time and measured sedentary time.
4. Discussion
Surgeons overestimated the amount of physical activity they completed compared to measured physical activity. They also underestimated their daily sedentary time compared to measured amounts. Despite this, the majority of surgeons self-reported that their physical activity was sufficient and their sedentary time was appropriate. There was no correlation found between their self-reported and measured physical activity or sedentary time.
Though surgeons underestimated their amount of sedentary time, the median measured sedentary time (5 h and 53 min) was less than that of a more general French population with habitually low physical activity, who were found to have an average sedentary time of 7 h and 17 min [6]. The increased level of activity and reduced length of sedentary time in surgeons is also true when compared to a Norwegian population who had an average daily step count of 8206 (compared to 9439 steps in our cohort) and average daily sedentary time of 9 h and 11 min [14]. The reportedly higher completed physical activity compared to measured physical activity is also consistent with studies in the general population [6,15,16]. Correlation between self-reported and measured physical activity has been found to range from 0.14 to 0.58, with only one third of studies finding a correlation coefficient above 0.4 [16]. This is consistent with our findings that surgeon self-reported physical activity was not correlated with measured physical activity.
This study had several limitations. First, the actigraph was worn on the surgeon’s ankle, rather than at their hip. This location may have overestimated how vigorous the level of physical activity was and, therefore, inappropriately increased the amount of measured physical activity. However, despite this potential for overestimation, surgeon measured physical activity was still much lower than self-reported physical activity. Secondly, measured physical activity was based on an average weekly for a 30-day period that was calculated for each operation performed by the surgeon during the study period. This was also done for sedentary time which was measured daily and then averaged for the 30-day period prior to the operation. This generated multiple 30-day measured weekly physical activity and daily sedentary time results for each surgeon in the cohort, but these were averaged to provide an estimate of the typical physical activity and sedentary time for each surgeon. Some periods would have overlapped, but the goal was to determine the typical weekly physical activity for each surgeon. Despite this, bias may have been introduced into the measured physical activity and sedentary time through the use of this method. Lastly, the generalizability of our findings is limited by the French context within a specific geographical area.
Surgeons demonstrate overestimation of their physical activity and underestimation of their sedentary time with self-reporting compared to measured findings. There is no correlation between their self-reports and measured findings. This demonstrates that even within a cohort of practicing surgeons, increased awareness is needed to promote surgeon wellness through intentional physical activity completion and reducing sedentary time. This is particularly important as prior research has found that sedentary time tends to be higher outside of work [17]. Physical activity has also been associated with reduced cognitive weariness when stress is high, meaning that those completing more physical activity have less cognitive weariness than those who completed less physical activity [18]. Given the high stress nature of surgeons’ practices, increasing physical activity and reducing sedentary time could be particularly beneficial to stress management and mitigating burnout. These, in turn, could improve patient outcomes by enhancing surgeon performance in the operating room. Further work should explore associations between surgeon physical activity and its relation to intraoperative stress and patient outcomes.
5. Conclusions
Surgeons tend to overestimate the sufficiency of their physical activity and underestimate their sedentary time when self-reporting activity compared to device-measured activity. There was no correlation between surgeon self-reported versus measured physical activity and sedentary time, further demonstrating the difficulty with self-assessing personal physical activity. Increased awareness regarding physical activity and targeted interventions are needed to promote surgeon health and wellness.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Antoine Duclos reports financial support was provided by European Research Council. Antoine Duclos reports financial support was provided by French Ministry of Health. If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Handling editor:D.G. Healy
Footnotes
Support: This project was supported by a European Research Council (ERC) Starting Grant under the European Union’s Horizon 2020 research and innovation program (Grant agreement No. 801660 - TopSurgeons - ERC-2018-STG). This study was also supported by a public grant from the French Ministry of Health (Programme de Recherche sur la Performance du Système des Soins [PREPS-17-0008]).
References
- 1.World Health Organization. Physical Activity. Geneva, Switzerland. Available at: https://www.who.int/news-room/fact-sheets/detail/physical-activity. Accessed June 7, 2024.
- 2.Abd T.T., Kobylivker A., Perry A., Miller Iii J., Sperling L. Work-related physical activity among cardiovascular specialists. Clin Cardiol. 2012 Feb;35(2):78–82. doi: 10.1002/clc.21954. Epub 2012 Jan 23. PMID: 22271102; PMCID: PMC6652291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jatkinson J., Goody R.B., Walker C.A. Walking at work: a pedometer study assessing the activity levels of doctors. Scot Med J. 2005 May;50(2):73–74. doi: 10.1177/003693300505000210. PMID: 15981342. [DOI] [PubMed] [Google Scholar]
- 4.Murphy I.G., Murphy C.G., Heffernan E.J. A comparative analysis of the occupational energy expenditure of radiologists versus clinicians. Ir J Med Sci. 2015 Dec;184(4):889–892. doi: 10.1007/s11845-014-1215-z. Epub 2014 Oct 24. PMID: 25342162. [DOI] [PubMed] [Google Scholar]
- 5.Assayag E., Wiener R., Gelman E., Abulafia A., Wasser L.M., Hanhart J., Zadok D., Weill Y. The physical activity level of ophthalmologists at work: a pedometer-based study. Workplace Health & Saf. 2023 Jan;71(1):6–12. doi: 10.1177/21650799221099039. Epub 2022 Jun 7. PMID: 35673758. [DOI] [PubMed] [Google Scholar]
- 6.Jacobi D., Charles M.A., Tafflet M., Lommez A., Borys J.M., Oppert J.M. Relationships of self-reported physical activity domains with accelerometry recordings in French adults. Eur J Epidemiol. 2009;24(4):171–179. doi: 10.1007/s10654-009-9329-8. Epub 2009 Mar 13. PMID: 19283494. [DOI] [PubMed] [Google Scholar]
- 7.Troiano R.P., Berrigan D., Dodd K.W., Mâsse L.C., Tilert T., McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008 Jan;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. PMID: 18091006. [DOI] [PubMed] [Google Scholar]
- 8.Gorzelitz J., Peppard P.E., Malecki K., Gennuso K., Nieto F.J., Cadmus-Bertram L. Predictors of discordance in self-report versus device-measured physical activity measurement. Ann Epidemiol. 2018 Jul;28(7):427–431. doi: 10.1016/j.annepidem.2018.03.016. Epub 2018 Mar 30. PMID: 29681429; PMCID: PMC6500726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cleland C.L., Hunter R.F., Kee F., Cupples M.E., Sallis J.F., Tully M.A. Validity of the global physical activity questionnaire (GPAQ) in assessing levels and change in moderate-vigorous physical activity and sedentary behaviour. BMC Publ Health. 2014 Dec 10;14:1255. doi: 10.1186/1471-2458-14-1255. PMID: 25492375; PMCID: PMC4295403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bull F.C., Maslin T.S., Armstrong T. Global physical activity questionnaire (GPAQ): nine country reliability and validity study. J Phys Activ Health. 2009 Nov;6(6):790–804. doi: 10.1123/jpah.6.6.790. PMID: 20101923. [DOI] [PubMed] [Google Scholar]
- 11.Keating X.D., Zhou K., Liu X., Hodges M., Liu J., Guan J., Phelps A., Castro-Piñero J. Reliability and concurrent validity of global physical activity questionnaire (GPAQ): a systematic review. Int J Environ Res Publ Health. 2019 Oct 26;16(21):4128. doi: 10.3390/ijerph16214128. PMID: 31717742; PMCID: PMC6862218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Global physical activity questionnaire (GPAQ). Geneva, Switzerland. Available at: https://www.who.int/publications/m/item/global-physical-activity-questionnaire. Accessed June 7, 2024.
- 13.Choi L., Liu Z., Matthews C.E., Buchowski M.S. Validation of accelerometer wear and nonwear time classification algorithm. Med Sci Sports Exerc. 2011 Feb;43(2):357–364. doi: 10.1249/MSS.0b013e3181ed61a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dyrstad S.M., Hansen B.H., Holme I.M., Anderssen S.A. Comparison of self-reported versus accelerometer-measured physical activity. Med Sci Sports Exerc. 2014 Jan;46(1):99–106. doi: 10.1249/MSS.0b013e3182a0595f. PMID: 23793232. [DOI] [PubMed] [Google Scholar]
- 15.Gudnadottir U., Cadmus-Bertram L., Spicer A., Gorzelitz J., Malecki K. The relationship between occupational physical activity and self-reported vs measured total physical activity. Prev Med Rep. 2019 Jun 10;15 doi: 10.1016/j.pmedr.2019.100908. PMID: 31297308; PMCID: PMC6598033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Skender S., Ose J., Chang-Claude J., Paskow M., Brühmann B., Siegel E.M., Steindorf K., Ulrich C.M. Accelerometry and physical activity questionnaires - a systematic review. BMC Publ Health. 2016 Jun 16;16:515. doi: 10.1186/s12889-016-3172-0. PMID: 27306667; PMCID: PMC4910242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tudor-Locke C., Leonardi C., Johnson W.D., Katzmarzyk P.T. Time spent in physical activity and sedentary behaviors on the working day: the American time use survey. J Occup Environ Med. 2011 Dec;53(12):1382–1387. doi: 10.1097/JOM.0b013e31823c1402. PMID: 22104979. [DOI] [PubMed] [Google Scholar]
- 18.Isoard-Gautheur S., Ginoux C., Gerber M., Sarrazin P. The stress-burnout relationship: examining the moderating effect of physical activity and intrinsic motivation for off-job physical activity. Workplace Health & Saf. 2019 Jul;67(7):350–360. doi: 10.1177/2165079919829497. Epub 2019 Mar 15. PMID: 30873913. [DOI] [PubMed] [Google Scholar]