Abstract
Purpose
To compare the anatomical and functional outcomes of pars plana vitrectomy (PPV) alone versus PPV with the addition of a scleral buckle in treating inferior rhegmatogenous retinal detachments (RRDs).
Methods
Comparative, retrospective cohort study including patients who were diagnosed with primary inferior RRD, defined as RRD with one or more retinal tears located between 4 and 8 hours, and divided into two treatment groups. Group 1 patients were treated with PPV and gas tamponade alone, whereas group 2 patients were treated with PPV, gas tamponade and the addition of an encirclement band. Demographic and clinical features were collected, and surgical outcomes of both groups were analysed. A univariable logistic regression model evaluated the factors influencing surgical success.
Results
A total of 161 eyes were included in the study. The average age at diagnosis was 64.1 years. There was a male predominance (66.5%), and most patients had macula-off detachments (54%). Group 1 included 75 eyes (43.1%), whereas group 2 included 86 eyes (56.9%). Baseline best-corrected visual acuity was 1.00 logMAR, improving to 0.62 logMAR at the last visit (p=0.003). No significant difference in primary success rate was observed between the two groups (86.0% with encirclement band vs 80.0% without; p=0.3). The mean follow-up period was 29 weeks (SD 39).
Conclusions
PPV alone may be as effective as PPV with an encirclement band when treating inferior RRDs. The choice of tamponade does not appear to significantly influence anatomical success, and short-acting gas can be considered sufficient for favourable outcomes.
Keywords: retina, vitreous, tears, treatment surgery
WHAT IS ALREADY KNOWN ON THIS TOPIC
Rhegmatogenous retinal detachments secondary to inferior retinal breaks are known to be particularly insidious to repair, generally showing a lower attachment rate after one operation compared with other retinal detachments. There are currently no established guidelines or consensus for their management, but it has been postulated that the incorporation of an encirclement band into the vitrectomy procedure may increase the success rate.
WHAT THIS STUDY ADDS
Our study shows that vitrectomy alone might be as effective in the treatment of inferior retinal detachments, without the need for the addition of an encirclement band. Short-acting gas proved furthermore to be a sufficiently effective tamponade for inferior retinal detachments.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This findings could help vitreoretinal surgeons in their choice of procedure and tamponade when treating patients with inferior retinal detachments, but more research is needed to reach a widespread consensus on the topic.
Introduction
Rhegmatogenous retinal detachments (RRDs) with inferior retinal breaks still represent a challenge with increased risk of primary surgical failure and recurrent RRDs.1 2 In fact, success rate after one operation for inferior RRD varies greatly, from 60% to 97%.3,5 In this regard, the two most common reasons contributing to surgical failure in RRDs with inferior breaks are the presence of inadequate gas or oil tamponade and the development of proliferative vitreoretinopathy (PVR). In addressing the first issue, the anatomical challenge lies in tamponing inferior retinal breaks right after surgery due to their specific location. As for the second point, PVR typically develops in the inferior region, influenced by gravitational forces. PVR development may furthermore lead to reopening of previously closed breaks or the formation of new stretch holes, while insufficient tamponade could result in unsealed breaks or recurrent RRD.6
Despite the recognised challenges and poorer postoperative outcomes associated with this type of RRD compared with those with breaks in other areas, there are currently no established guidelines or consensus for its management.3 It has been postulated that the incorporation of a scleral buckle (SB) or encirclement band into the vitrectomy procedure may counteract the tractional forces of PVR and reduce the reliance on an internal tamponade, potentially minimising the risk of persistent or recurrent RRD.17,9
In this study, we evaluated the demographic and clinical characteristics and compare two different surgical techniques to assess the primary success rates (PSRs) of different surgical procedures and complications associated with the management of inferior primary uncomplicated RRD.
Materials and methods
Comparative, retrospective, clinical series of patients diagnosed with primary uncomplicated inferior RRD, defined as RRD with one or more retinal tears located between 4 and 8 hours in the detached retina. Inclusion criteria were inferior RRD repaired with vitrectomy (pars plana vitrectomy (PPV)) in combination or not with encircling band and gas. Exclusion criteria include PVR at presentation, previous retinal surgery and RRD secondary to ocular trauma.
Variables analysed included age, gender, clinical features, including lens status, vitreous status, macula status, tear location, number of retinal tears, extension of detachment, incidence and grade of PVR, rate of success of surgery and follow-up, initial and final best-corrected visual acuity (BCVA). All surgeries were performed by experienced vitreoretinal consultants between March 2017 and March 2023 at the ophthalmology department of Inselspital, University Hospital of Bern, Switzerland. In relation to surgical management, the cohort was divided into two groups according to the type of operation they received. In the first group, patients underwent PPV with the addition of a encirclement band and gas (either SF6 or C3F8) as tamponade, while in the second group patients received PPV alone, without the addition of a band and gas (either SF6 or C3F8) as a tamponade. All statistical analyses were performed using GraphPad Prism V.10.0.3 and Python 3.9.6. A p value of 0.05 was considered statistically significant.
Institutional review board approval was obtained and all the aspects of this study adhered to the tenets of the Declaration of Helsinki.
Results
Clinical and demographical features
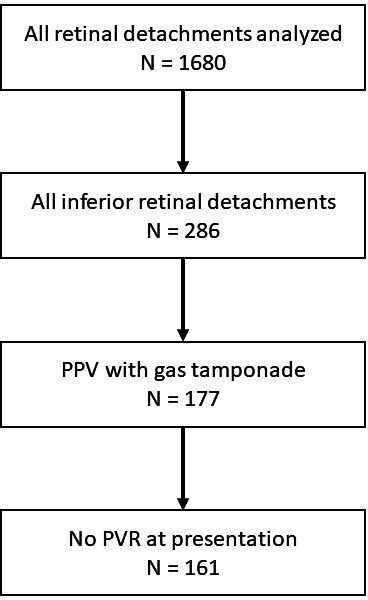
A total of 1680 eyes with retinal detachments were analysed, of these, 286 eye underwent vitrectomy for RRDs secondary to inferior retinal breaks during the study period. Out of this cohort, 161 were included for meeting the inclusion criteria. (figure 1)
Figure 1. Flow diagram of patients selection. PPV, pars plana vitrectomy; PVR, proliferative vitreoretinopathy.
The average age at diagnosis was 64.1 years (SD 11.0, range 28.7–92.0 years). A total of 107 patients (66.5%) were men and 54 (33.5%) were women. Regarding lens status, 77 eyes (47.8%) were phakic and 84 (52.2%) were pseudophakic. In 140 (87%) eyes, a posterior vitreous detachment (PVD) was present, and in 21 (13%) eyes, a partial PVD was observed. The mean number of retinal tears was 3.27 (SD 1.81, range 1–7).
Visual acuity data available for the patients showed the initial mean BCVA was 1.00 logMAR (SD 0.89) and the final mean BCVA had improved significantly to 0.62 logMAR (Snellen 0.41) (SD 0.72; p=0.003). Table 1 outlines the demographical and clinical characteristics of the two distinct subgroups
Table 1. Clinical and surgical features of both groups.
| Vitrectomy+encirclement band+gas | Vitrectomy alone and gas | P value | |
| Number of patients | 86 | 75 | – |
| Success rate | 86.0% | 80.0% | 0.3 |
| Age (mean) (SD) | 61.5 (10.9) | 67.0 (10.3) | 0.001 |
| Gender (male) | 60.7% | 68.1% | 0.7 |
| Lens status (phakic) | 68.6% | 24.0% | <0.0001 |
| Vitreous status (full PVD) | 83.7% | 90.7% | 0.19 |
| Macula status (on) | 46.5% | 45.3% | 0.88 |
| PVR at presentation | 0% | 0% | – |
| Number of retinal tears (SD) | 3.1 (1.7) | 3.5 (1.9) | 0.19 |
| Extension of RD (SD) | 3.9 (1.9) | 4.5 (1.7) | 0.28 |
| Type of gas | C3F8 4.8%SF6 95.2% | C3F8 15.5%SF6 84.5% | 0.03 |
| Cause of failure (PVR) | PVR 66.7%New hole 33.3% | PVR 93.4%New hole 6.6% | 0.08 |
| logMAR Initial BCVA (SD) | 0.91 (0.9) | 1.06 (0.9) | 0.38 |
| Final BCVA (logMAR) | 0.61 (0.7) | 0.62 (0.7) | 0.91 |
| Follow-up (mean) (SD) | 29.8 (45.9) | 28.5 (34.6) | 0.88 |
BCVAbest-corrected visual acuityPVDposterior vitreous detachmentPVRproliferative vitreoretinopathy
Surgical outcomes
In our study 134 of 161 eyes had complete retinal reattachment with one single surgery, resulting in an overall PSR of 83.2% for the whole cohort. Overall 86 (56.9%) eyes underwent PPV with the addition of an encirclement band and gas as tamponade and 75 (43.1%) eyes PPV alone (without the addition of an encirclement band) and gas as tamponade. In subgroup analysis, vitrectomy with encirclement band had a PSR of 86.0% and vitrectomy alone 80.0% (p=0.3). The main cause of failure of our cohort was PVR, accounting for 85.2% of total failures. In the remaining 14.8% of cases, the cause of failure was a new retinal break or a break missed by the surgeon intraoperatively. This showed a difference in the subgroup analysis, where group 1 had 66.7% of failure caused by PVR and group 2 had 93.4%; this showed no statistically significant difference (p=0.08). The average final follow-up was at 29.8 weeks (SD 45.9) or patients treated with combination between vitrectomy and encirclement band and 28.5 (SD 34.6) weeks for vitrectomy alone.
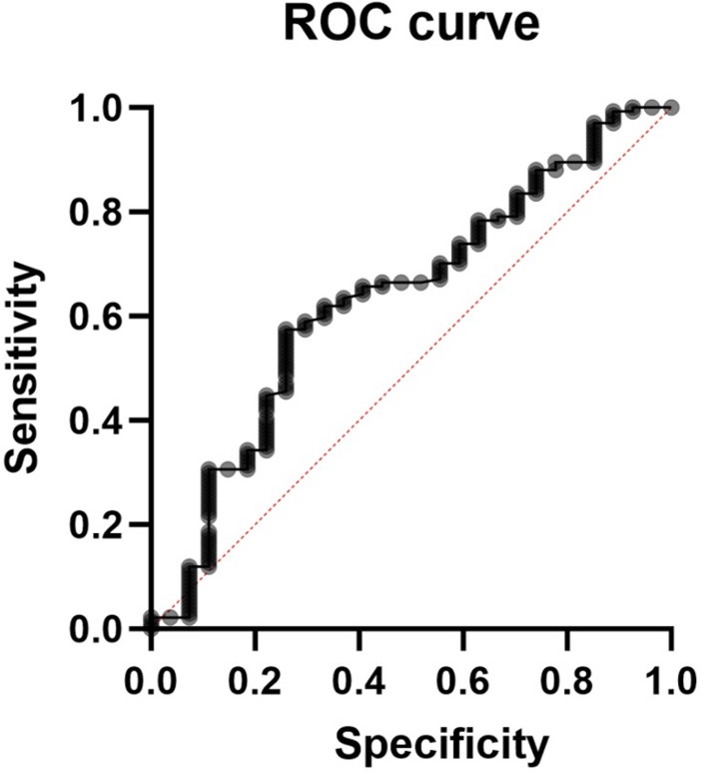
The simple logistic regression model revealed that age has a statistically significant impact on the likelihood of patients being attached after one surgery, with a p value of 0.03. Specifically, for each one-unit increase in age, the odds of being attached after surgery decrease by approximately 4.38%. The area under the ROC curve (AUC) was 0.6346 (figure 2). However, when applying a Bonferroni correction to account for multiple comparisons, the new significance threshold became 0.01. Under this more stringent criterion, the effect of age was no longer statistically significant. Other factors examined, including gender, macula status, number of retinal tears and type of tamponade, showed no statistically significant association with surgical failure.
Figure 2. ROC curve of a simple logistic regression analysis for age and failure, showing an area under the curve of 0.6346.
Discussion
Inferior retinal detachment is a significant risk factor for surgical failure,10 which has led to ongoing discussions among vitreoretinal surgeons regarding the most effective ways to treat this condition. In this context, vitreoretinal specialists can choose from various surgical methods to address primary RRD, with their choice influenced by their own expertise and experience, as well as their evaluation of existing research findings.11 It has been hypothesised that adding an encircling band could provide numerous benefits, including supporting any unseen breaks and the whole vitreous base, reducing vitreous traction and acting as a prophylaxis against future break development specially in inferior RRD, where the addition of SB may be more beneficial due to the lack of support from intraocular tamponade agents.12 However, the real benefit of the combination of vitrectomy plus encircling band or SB has not been clearly established and despite earlier research indicating that PPV alone achieves acceptable success rates for inferior RRD,313,17 this is not universally accepted.7 10 Similarly, we report that the use of vitrectomy alone is as effective as the combination of a PPV with an encircling band for repairing inferior RRD in a cohort of 161 eye (80% vs 86% p=0.3), as has been reported in other clinical series and metanalysis.313 14 16,18Although our study showed a trend favouring the combination of PPV with encircling band for repairing inferior RRD (86% success rate), this did not reach statistical significance. Two factors may explain this outcome: first, our sample size may have been insufficient to detect a statistically significant difference; second, the mean age was significantly higher in the PPV-alone group, and increasing age is a known risk factor for PVR and surgical failure.19,21 These factors could account for the observed trend in success rates and explain the higher incidence of post-operative PVR in the vitrectomy-alone subgroup (93.4%) compared with the combined group (66.7%).
The PRO study,1 a multicentric retrospective study which analysed 238 eyes, found that inferior RRD had a higher single-surgery success rate if treated with PPV/SB compared with PPV alone (87.4% vs 76.8%, p=0.0), a difference which was observed especially in phakic patients (85.2% vs 68.6%, p=0.046). It was hypothesised that phakic eyes may benefit the most, especially considering the challenges associated with performing an extensive anterior vitrectomy in these eyes and that incomplete removal of the vitreous might not fully relieve the anterior traction of the retinal tears. SBs are effective in counteracting this tension and any additional traction caused by PVR.1 However, there is no evidence in the literature to suggest that shaving of the vitreous base prevents or reduces the incidence of PVR and clinical series have demonstrated good surgical results using PPV without vitreous base shaving and also with limited vitrectomy,22,24 showing that the key elements of successful outcomes are repairing all retinal tears and sealing the responsible breaks using a gas tamponade. It has also been postulated that vitrectomy without the addition of SBs does not allow us to perform a full vitrectomy having this as an impact in the gas filling and potentially leading to a suboptimal gas fill, which may lead to less effective tamponade.1 Nevertheless, better gas fill has not shown better outcome in inferior RRD.25 Tamponade agents cannot be expected to achieve total reattachments by acting as space fillers, due to the difficulty in filling completely the eye. The success of RRD surgery depends on the effective repair of the break, which should be tamponade for only a short time in the early postoperative hours. This time is essential for the initial chorioretinal adhesion.26 Break closure can occur independently of direct contact of gas with the retina, as demonstrated by a computational fluid dynamic software.27 This is in line with our findings, where the majority of patients in both groups were repaired using SF6, achieving similar results to cases repaired with long-acting gas.
Our study presents some limitations, including the retrospective design and the relative moderate sample size. While randomised controlled trials remain the gold standard of clinical research, they are often resource-intensive in terms of both time and cost, making them impractical for every research endeavour. As such, real-world data studies play a crucial role in complementing trials by providing insights into how treatments perform in diverse patient populations and real-life settings, efficiently guiding the development of new treatment strategies.11
This study demonstrated that PPV alone is as effective as the combination of PPV with an encircling band for repairing inferior RRD, consistent with previous clinical series and meta-analysis. Overall, we believe that still there is improvement in the anatomical outcome of inferior RRD. As it has been extensively showed in the literature, there are different alternatives to successfully treat retinal detachments. As more data emerge, it is important to maintain a clear and logical structure privileging outcome with less invasive therapy without need to add extra possible complications to our patients
Summary statement
The study analysed the PSR of PPV with and without the addition of an encirclement band in 161 patients with inferior retinal detachments. The results showed comparable efficacy in both groups, suggesting that PPV alone may be sufficient for treating inferior retinal detachments. Additionally, short-acting gas may be enough as a tamponade for the treatment of inferior retinal detachments.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Patient consent for publication: Not applicable.
Ethics approval: Not applicable.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Contributor Information
Enrico Bernardi, Email: enrico.bernardi.pv@gmail.com.
Lorenzo Ferro Desideri, Email: lorenzoferrodes@gmail.com.
Dmitri Artemiev, Email: d.artemiev@gmx.ch.
Martin Zinkernagel, Email: martin.zinkernagel@insel.ch.
Rodrigo Anguita, Email: rodrigoanguita@gmail.com.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Starr MR, Obeid A, Ryan EH, et al. RETINAL DETACHMENT WITH INFERIOR RETINAL BREAKS: Primary Vitrectomy Versus Vitrectomy With Scleral Buckle (PRO Study Report No. 9) Retina (Philadelphia, Pa) 2021;41:525–30. doi: 10.1097/IAE.0000000000002917. [DOI] [PubMed] [Google Scholar]
- 2.Wang A, Snead MP. Scleral buckling-a brief historical overview and current indications. Graefes Arch Clin Exp Ophthalmol. 2020;258:467–78. doi: 10.1007/s00417-019-04562-1. [DOI] [PubMed] [Google Scholar]
- 3.Bonnar J, Tan CH, McCullough P, et al. Scleral Buckle, Vitrectomy, or Combined Surgery for Inferior Break Retinal Detachment: Systematic Review and Meta-Analysis. Ophthalmol Retina. 2023;7:837–47. doi: 10.1016/j.oret.2023.05.006. [DOI] [PubMed] [Google Scholar]
- 4.Mehboob M, Ghani MU, Khan A, et al. Scleral buckling and pars plana vitrectomy versus pars plana vitrectomy alone in the treatment of rhegmatogenous retinal detachment with inferior break. Pakistan Journal of Medical &Amp; Health Sciences. 2018 [Google Scholar]
- 5.Romano MR, Angi M, Valldeperas X, et al. Twenty-three-gauge pars plana vitrectomy, Densiron-68, and 360° endolaser versus combined 20-gauge pars plana vitrectomy, scleral buckle, and SF6 for pseudophakic retinal detachment with inferior retinal breaks. Retina . 2011;31:686–91. doi: 10.1097/IAE.0b013e3181f0d249. [DOI] [PubMed] [Google Scholar]
- 6.Wickham L, Ho-Yen GO, Bunce C, et al. Surgical failure following primary retinal detachment surgery by vitrectomy: risk factors and functional outcomes. Br J Ophthalmol. 2011;95:1234–8. doi: 10.1136/bjo.2010.190306. [DOI] [PubMed] [Google Scholar]
- 7.Alexander P, Ang A, Poulson A, et al. Scleral buckling combined with vitrectomy for the management of rhegmatogenous retinal detachment associated with inferior retinal breaks. Eye (Lond) 2008;22:200–3. doi: 10.1038/sj.eye.6702555. [DOI] [PubMed] [Google Scholar]
- 8.Ferro Desideri L, Artemiev D, Zandi S, et al. Proliferative vitreoretinopathy: an update on the current and emerging treatment options. Graefes Arch Clin Exp Ophthalmol. 2024;262:679–87. doi: 10.1007/s00417-023-06264-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferro Desideri L, Zandi S, Zinkernagel MS, et al. Challenges in proliferative vitreoretinopathy: is biological therapy a solution? Expert Opin Biol Ther. 2023;23:937–9. doi: 10.1080/14712598.2023.2248881. [DOI] [PubMed] [Google Scholar]
- 10.Yorston D, Donachie PHJ, Laidlaw DA, et al. Stratifying the risk of re-detachment: variables associated with outcome of vitrectomy for rhegmatogenous retinal detachment in a large UK cohort study. Eye (Lond) 2023;37:1527–37. doi: 10.1038/s41433-023-02388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anguita R, Charteris D. Could real-world data replace evidence from clinical trials in surgical retinal conditions? Br J Ophthalmol. 2022;106:1037–8. doi: 10.1136/bjophthalmol-2022-321759. [DOI] [PubMed] [Google Scholar]
- 12.Smith BTB. Buckle, Vitrectomy, or Both for Retinal Detachments with Inferior Breaks. Ophthalmol Retina. 2023;7:835–6. doi: 10.1016/j.oret.2023.05.018. [DOI] [PubMed] [Google Scholar]
- 13.Wickham L, Connor M, Aylward GW. Vitrectomy and gas for inferior break retinal detachments: are the results comparable to vitrectomy, gas, and scleral buckle? Br J Ophthalmol. 2004;88:1376–9. doi: 10.1136/bjo.2004.043687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharma A, Grigoropoulos V, Williamson TH. Management of primary rhegmatogenous retinal detachment with inferior breaks. Br J Ophthalmol. 2004;88:1372–5. doi: 10.1136/bjo.2003.041350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martínez-Castillo VJ, García-Arumí J, Boixadera A. Pars Plana Vitrectomy Alone for the Management of Pseudophakic Rhegmatogenous Retinal Detachment with Only Inferior Breaks. Ophthalmology. 2016;123:1563–9. doi: 10.1016/j.ophtha.2016.03.032. [DOI] [PubMed] [Google Scholar]
- 16.Tanner V, Minihan M, Williamson TH. Management of inferior retinal breaks during pars plana vitrectomy for retinal detachment. Br J Ophthalmol. 2001;85:480–2. doi: 10.1136/bjo.85.4.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baumgarten S, Schiller P, Hellmich M, et al. Vitrectomy with and without encircling band for pseudophakic retinal detachment with inferior breaks: VIPER Study Report No. 3. Graefes Arch Clin Exp Ophthalmol. 2018;256:2069–73. doi: 10.1007/s00417-018-4106-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stavrakas P, Tranos P, Androu A, et al. Anatomical and Functional Results Following 23-Gauge Primary Pars Plana Vitrectomy for Rhegmatogenous Retinal Detachment: Superior versus Inferior Breaks. J Ophthalmol. 2017;2017:2565249. doi: 10.1155/2017/2565249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xiang J, Fan J, Wang J. Risk factors for proliferative vitreoretinopathy after retinal detachment surgery: A systematic review and meta-analysis. PLoS One. 2023;18:e0292698. doi: 10.1371/journal.pone.0292698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferrara M, Al-Zubaidy M, Song A, et al. The effect of age on phenotype of primary rhegmatogenous retinal detachment. Eye (Lond) 2023;37:1114–22. doi: 10.1038/s41433-022-02061-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pastor JC, de la Rúa ER, Aragón J, et al. Interaction Between Surgical Procedure for Repairing Retinal Detachment and Clinical Risk Factors for Proliferative Vitreoretinopathy. Curr Eye Res. 2005;30:147–53. doi: 10.1080/02713680490904142. [DOI] [PubMed] [Google Scholar]
- 22.Tabandeh H, London NJS, Boyer DS, et al. Outcomes of small-gauge vitreoretinal surgery without scleral-depressed shaving of the vitreous base in the era of wide-angle viewing systems. Br J Ophthalmol. 2019;103:1765–8. doi: 10.1136/bjophthalmol-2018-313626. [DOI] [PubMed] [Google Scholar]
- 23.Wibbelsman TD, Xu D, Levin H, et al. Limited Vitrectomy for Pseudophakic Rhegmatogenous Retinal Detachment. Retina . 2022;42:2411–3. doi: 10.1097/IAE.0000000000002690. [DOI] [PubMed] [Google Scholar]
- 24.Anguita R, Makuloluwa A, Sim SY, et al. LATE RECURRENCE OF RETINAL DETACHMENT: Incidence, Clinical Features, and Surgical Outcomes. Retina . 2024;44:83–7. doi: 10.1097/IAE.0000000000003924. [DOI] [PubMed] [Google Scholar]
- 25.Young BA, Heath Jeffery RC, Atkins WK, et al. The effect of day-1 postoperative gas fill on the outcome of vitrectomy for retinal detachment. Eye (Lond) 2021;35:682–3. doi: 10.1038/s41433-020-0846-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martínez-Castillo V, Verdugo A, Boixadera A, et al. Management of inferior breaks in pseudophakic rhegmatogenous retinal detachment with pars plana vitrectomy and air. Arch Ophthalmol. 2005;123:1078–81. doi: 10.1001/archopht.123.8.1078. [DOI] [PubMed] [Google Scholar]
- 27.Angunawela RI, Azarbadegan A, Aylward GW, et al. Intraocular fluid dynamics and retinal shear stress after vitrectomy and gas tamponade. Invest Ophthalmol Vis Sci. 2011;52:7046–51. doi: 10.1167/iovs.10-6872. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.


