Abstract
Objective:
To examine the association between family cohesion and behaviors linked to health or overweight in adolescents.
Method:
Cross-sectional analyses of family cohesion and eating behaviors of 2,379 girls (followed from ages 9–19) who participated in the National Heart, Lung, and Blood Institute Growth and Health Study (NGHS). Height and weight measurements were obtained on an annual basis. Family cohesion was measured by the Family Adaptability and Cohesion Evaluation Scale (FACES) III. Food diaries were used to assess frequency of breakfast consumption and intake of milk, soda, fruits, and vegetables.
Results:
Family cohesion was significantly associated with less soda intake and higher rates of breakfast consumption. Ingestion of milk, fruits, and vegetables was predicted by family cohesion at the trend level.
Conclusion:
Understanding the role of familial factors in adolescent eating behaviors is an important research priority. Strengthening family cohesion may be a valuable goal toward promoting the health of adolescents, increasing breakfast eating and decreasing soda consumption.
Keywords: family, nutrition, breakfast, adolescents, adolescent health
Introduction
Familial variables are known to influence child and adolescent eating behaviors.1 Beyond conferring biological predispositions for body weight, parents provide the environmental context for children’s eating behaviors, including the types and amount of food available, frequency of meals or snacks, the social context of meals (e.g., eating alone versus as a family), modeling healthful or unhealthful eating, and instructing children about or reinforcing them for healthy eating behaviors.2-5 Much of the literature on familial influences has looked at specific parental behaviors (e.g., modeling healthy eating or providing healthy foods, see Refs. 6 and 7) or parental attitudes (e.g., belief that it is important to eat breakfast; see Ref. 8 for review). In a number of studies,9-12 Birch and coworkers have found that parental modeling of fruit, vegetable, and milk consumption was positively associated with children’s consumption of these foods. Similarly, Zabinski et al.13 reported that family influence, defined as parental encouragement to eat fruits and vegetables and making them available, was the only psychosocial variable associated with number of daily servings of fruits and vegetables in a sample of adolescent girls (aged 11–15 years). While studies have provided both direct and indirect support for the influence of parental attitudes and behaviors on children’s eating habits, few have explored psychological aspects of the overall family climate or the extent to which children’s views of the familial environment may play a role in developing healthy eating behaviors.
Family cohesion has been defined as the emotional connection between family members and is known to be important for children’s development and functioning,14,15 including affecting adolescents’ feeling of control over their own health.16 Ogden and Steward17 determined that interactions between mothers and daughters were associated with weight concerns and dieting in young girls and others have reported that girls who perceived their family relationships as negative were more likely to engage in restrictive eating and skipping meals in the subsequent year.18 Moreover, family climate has been related to unhealthy weight control practices (e.g., extreme dieting, vomiting). One such study found that family connectedness, positive family communication, parental supervision, and maternal presence protected against the onset of these behaviors.19 Beato-Fernandez et al. (2004) reported that negative feelings toward mother predicted the onset of an eating disorder 2 years later.20 Higher parental educational attainment, a stronger perception that parents care about them and stronger self-esteem were found to reduce female adolescents’ risk for excessive weight as young adults.21 This work suggests that not only are familial attitudes and behaviors associated with dietary habits, but also that interactional patterns within families may be an important influence in the development of eating behaviors.
Perceived family cohesion might be linked to healthy eating behaviors in a number of ways. A cohesive family might be one that promotes healthy behaviors directly; parents may encourage such behaviors and children who feel connected with their parents might be more inclined to follow their suggestions. Alternatively, cohesion is likely linked to psychological health,15 which may directly affect the development of healthy attitudes and behaviors in children. Young and Fors22 reported that high school students who consumed healthy breakfasts and lunches and ate more fruits and vegetables were better able to communicate with parents on serious issues and were more closely monitored by their parents, suggesting that elements of family climate may be associated with some healthy eating behaviors in adolescence. From the perspective of both the adolescent and parent, family meals create a sense of togetherness and provide an opportunity for role modeling of healthful eating habits.23
Two recent studies argue for the association between family cohesion and positive eating behaviors as a way of understanding more specifically the way familial variables may play an influential role. Using a Belgian sample of 7th and 8th graders, hierarchical regression analyses indicated that home environmental factors, including family cohesion, influenced the consumption of fruit in both boys and girls.24 Moore and Harre25 found that both parental monitoring and family cohesion were significantly positively related to adolescents’ consumption of breakfast and eating healthy foods, and negatively associated with eating unhealthy foods. While we would not necessarily expect family cohesion to be differentially linked to eating behaviors, there are likely additional influences (e.g., peers, availability) that are also relevant. Because family cohesion has been shown to be important and has not been examined in a large sample over the period of middle childhood through adolescence, we sought to explore the relationship between family cohesion and several eating behaviors in the 10-year National Heart, Lung, and Blood Institute Growth and Health Study (NGHS; 26), a study of 2,379 black and white girls. We investigated the extent to which ratings of family cohesion by the participants were associated with four eating behaviors that have been linked to health or overweight in children and adolescents: breakfast consumption and the intake of milk, soda, and fruits and vegetables. We predicted that higher family cohesion would be associated with higher frequency of breakfast eating, greater consumption of milk, fruits, and vegetables, and lower soda intake.
Method
The National Heart Lung and Blood Institute Growth and Health Study (NGHS) was a 10-year longitudinal study of 2,379 black and white girls who were 9 or 10 years old at study entry (NHLBI, 1992).26 NGHS was specifically designed to investigate the development of overweight and cardiovascular disease risk factors in girls; boys were not studied. Girls were recruited from three study sites: University of California at Berkeley, University of Cincinnati/Cincinnati Children’s Hospital Medical Center, and Westat/Group Health in Rockville, MD. Girls were interviewed annually between study year 1 and study year 10. For the current study, data from years 1, 3, 5, and 7 were used, as these were the visits when the measure of family cohesion was administered. Girls’ mean ages at these visits were 9.5, 11.5, 13.5, and 15.5 years, respectively. Eligibility criteria to participate in NGHS included: (1) racial concordance of parents and child; (2) girls were within 2 weeks of age 9 or 10 years; (3) child gave assent; (4) parents gave consent and completed a household demographic sheet. The study protocol was approved by the Institutional Review Boards of all participating sites. Data from all participants (n = 2,379) were included in the current study. Most psychosocial measures were given in alternating years (years 1, 3, 5, 7) to reduce subject burden.
Measures
Demographics.
At study entry, demographic information was obtained including race/ethnicity (non-Hispanic black or white, self-reported using United States census categories), parental education (completed 4+ years of college vs. less education) and number of parents in the household (two parents vs. one parent).
Adiposity.
Annually, centrally trained examiners obtained height and weight measurements. Body mass index was calculated as weight in kilogram divided by height in meters squared. For the present analyses, BMI-for-age z-scores were used as a covariate. BMI-for-age z-scores indicate girls’ BMI relative to other girls of the same age. Thompson et al.27 indicated that BMI z-score provides an indirect age and gender-specific measure of relative adiposity. Because the body composition of adolescent girls’ changes dramatically with pubertal growth, a relative measure of BMI changes is more sensitive and useful than is absolute BMI. Note that a positive change in BMI z-score indicates an increase in relative BMI, whereas the reverse is true for a negative z-score.
Family Cohesion.
To measure the girls’ perceptions of family cohesion, the Cohesion scale from the Family Adaptability and Cohesion Evaluation Scale (FACES) III28 was administered in study years 1, 3, 5, and 7. Questions were re-worded slightly to be appropriate for children and included questions in the areas of emotional bonding, supportiveness, family boundaries, and spending time together. Examples of items are “In my family we feel very close to each other,” “In my family we ask other family members about our decisions,” and “Family members like to spend free time with each other.” Each item was rated by NGHS participants and items were summed to create a “cohesion score,” with higher scores indicating greater family cohesion. Responses were scored on a 4-point scale, from 1 to 4 (i.e., almost never, once in a while, often, or almost always) and could range from 9 to 36 at each visit. Psychometric data presented by Olson et al.28 indicated test–retest reliability of 0.93 at a 5-week interval and evidence of discriminate validity has been shown by low correlations between cohesion and adaptability (r = .03) and cohesion and social desirability (r = .35). In the NGHS sample, internal consistency, as measured by Cronbach’s α, was 0.82 in study year 3 and 0.89 in study year 7.
Eating Behaviors.
Information about four eating behaviors was extracted from girls’ food diaries: breakfast consumption, soda intake, milk intake, and the consumption of fruits and vegetables. Specifically, 3-day food records that had been validated previously29 were collected annually for visits 1–5 and then again at visits 7. However, uniform recording of food amounts for fruits and vegetables was introduced only at visit 3. Therefore, the present analyses for fruits and vegetables are based on visits 3, 5, and 7, whereas the other three eating behaviors (breakfast, soda, and milk consumption) utilize data from visits 1, 3, 5, and 7. Dietitians trained and certified by the University of Minnesota Nutrition Coordinating Center (NCC) and retrained in later years by staff at the Dietary Data Entry Center in Cincinnati, used age-appropriate materials to instruct girls to record all food and drink for three consecutive days (2 weekdays and 1 weekend day). Dietitians reviewed the completed food records individually with the girls, using standard probes to answer girls’ questions or clarify incomplete responses. Default values adapted from NCC were used for missing information on food amounts or preparation methods. To minimize the use of defaults, staff had a notebook of labels and label pictures to help girls describe foods. Food records were coded and analyzed for nutrients using Food Table Version 19 of the NCC nutrient database30 initially, with updated versions being used as the study progressed.
Dietitians instructed girls to record type of meal (e.g., breakfast, lunch) and time of intake for three consecutive days. Breakfast was defined as any eating that occurred between 5:00 am and 10:00 am weekdays or between 5:00 am and 11:00 am during weekends. The amount and type of beverages consumed also were recorded in the food diaries. For the present analysis, the following beverages were analyzed: (1) “Milk” (all kinds of cow’s milk, including flavored varieties) and (2) “Regular soda” (all nondiet carbonated beverages, except water). At each visit, for each beverage category, average grams consumed per day were determined by adding the daily amounts and dividing the total by the number of days associated with a visit.
Finally, each item recorded in the food diaries was coded as fruit, vegetable, or neither fruit nor vegetable. Food quantities were measured in grams. Gram measures were converted to food-specific volumetric or portion measures (either cups or proportion of a piece of fruit/vegetable), which were in turn converted to servings, based on guidelines from the USDA food pyramid.31 For each girl, daily total servings of fruits and vegetables (all kinds) were computed. Mean daily servings were computed by averaging across the 3 days.
Data Analysis
Mixed models (PROC MIXED in SAS version 9.1) were used to model the relationship between FACES scores (predictor variable) and nutrition outcomes (dependent variables) across visits. All models were adjusted for race. To adjust for the potentially confounding influence of other demographic factors, models also were adjusted for level of parental education, number of parents in household, BMI z-score, and study site; all variables were appropriately centered for the analysis. Only results pertaining to the main study question are reported, namely, is family cohesion associated with eating behaviors and does the relationship between family cohesion and eating behaviors change as girls get older (using study visit as a proxy for age).
Nonlinearity was explored by adding spline terms at tertile cut points into the model, so that the slope of the relationship could vary from bottom to middle to top thirds of the sample. Likelihood ratio tests comparing models with and without splines indicated that for consumption of milk and soda, models with spline terms had a significantly better fit; however, for fruit and vegetable servings and for days of breakfast, models without splines were better. Therefore, spline terms were retained for soda and milk consumption only.
Results
Sample Characteristics
On the basis of data from year 1, there were slightly more black girls (51%) than white girls in the NGHS sample; a majority of girls (68.5%) lived in a two-parent household and about one-third of girls (31.5%) had at least one parent with a college education. As shown in Table 1, FACES scores tended to decline with increasing visits. Relative to early visits, frequency of eating breakfast and consumption of milk decreased over time; in contrast, intake of soda and fruit/vegetables increased at later visits.
TABLE 1.
Sample characteristics and values by visit for FACES scores and nutrition measures
| Visit | 1 | 3 | 5 | 7 |
|---|---|---|---|---|
| Age | 9.52 (0.52) n = 2,379 |
11.54 (0.60) n = 2,228 |
13.52 (0.61) n = 2,055 |
15.54 (0.61) n = 1,902 |
| Body mass index (BMI) | 18.57 (3.85) n = 2,359 |
20.63 (4.67) n = 2,228 |
22.68 (5.26) n = 2,056 |
23.98 (5.73) n = 1,902 |
| FACES | 26.96 (4.79) n = 2,343 |
25.28 (5.33) n = 2,211 |
23.22 (6.00) n = 2,031 |
22.41 (5.93) n = 1,882 |
| Breakfast consumption (days per visit) | 2.53 (0.73) n = 2,085 |
2.26 (0.91) n = 1,977 |
2.01 (1.01) n = 1,790 |
1.92 (1.06) n = 1,568 |
| Sweetened soda intake (g/day) | 139.03 (160.02) n = 2,085 |
207.39 (214.74) n = 1,978 |
272.48 (258.65) n = 1,790 |
302.42 (303.33) n = 1,568 |
| Milk intake (g/day) | 298.81 (200.42) n = 2,085 |
281.70 (219.50) n = 1,978 |
232.25 (220.27) n = 1,790 |
219.97 (239.33) n = 1,568 |
| Fruit/vegetable servings per day | NA | 3.05 (1.95) n = 1,978 |
2.96 (1.97) n = 1,790 |
3.39 (2.15) n = 1,568 |
Family Cohesion and Girls’ Food Intake
For each eating behavior, Table 2 shows the parameter estimates and statistical significance associated with each variable in the model. As predicted, higher FACES scores were associated with more days of breakfast consumption (p < .01); the interaction with visit was nonsignificant (p > .05). Also as predicted, higher FACES scores were associated with lower soda intake (p < .05); the interaction and spline terms (see Fig. 1) were not individually significant (p > .05). They were included in the model because the overall model fit was significantly better when these terms were included.
TABLE 2.
Mixed model parameter estimates of FACES scores and nutrition outcomesa
| Predictor Variables | Outcome Variables | |||
|---|---|---|---|---|
| Days Eating Breakfast |
Daily Grams of Soda |
Daily Grams of Milk |
Daily Servings of Fruits/Vegetables |
|
| Race = Af. American | −0.33 (0.03)*** | 12.69 (7.29)† | −121.11 (7.02)*** | 0.17 (0.07)* |
| Parental education 4+ years of college | 0.15 (0.03)*** | −37.52 (7.62)*** | 15.40 (7.36)* | 0.47 (0.07)*** |
| 2-parent household | 0.03 (0.03) | 9.76 (7.73) | −8.19 (7.44) | 0.07 (0.08) |
| Site 1 | 0.17 (0.03)*** | 14.07 (8.64) | 9.32 (8.34) | −0.17 (0.08)† |
| Site 2 | 0.18 (0.03)*** | 56.34 (8.66)*** | 7.30 (8.36) | −0.36 (0.08)*** |
| Visit | −0.24 (0.04)*** | 65.75 (10.86)*** | −31.00 (9.36)*** | 0.19 (0.13) |
| BMI z-score | −0.04 (0.01)*** | 7.51 (3.13)* | −7.05 (2.94)* | −0.04 (0.03) |
| FACES | 0.008 (0.003)** | −2.66 (1.34)* | 1.49 (1.16) | 0.022 (0.012)† |
| Spline 1 | NA | 2.71 (2.58) | −1.21 (2.22) | NA |
| Spline 2 | NA | −1.18 (2.73) | 1.69 (2.36) | NA |
| FACES* visit | 0.002 (0.002) | −0.70 (0.44) | 0.31 (0.38) | 0.000 (0.005) |
Note: †.05 < p < .10, *p < .05, **p < .01, ***p < .001.
Estimates are interpreted as the predicted change in an outcome variable (days eating breakfast, daily consumption of soda, milk or fruits/vegetables), assuming a 1-unit increase in a given predictor variable while the other predictor variables are held constant. FACES was broken into three segments, representing non-linear effects. The first term (“FACES”) represents the first tertile of FACES score, “Spline 1” the second tertile and “Spline 2” represents the third tertile. For example, in the lowest or first tertile of FACES score, a 1-unit increase in FACES predicts a significant decrease (−2.66 g) in soda consumed; in the second tertile of FACES, a 1-unit increase in FACES predicts a non-significant increase (−2.66 + 2.71 = 0.05 g) in soda consumed; and in the third tertile of FACES, a 1-unit increase in FACES predicts a non-significant decrease (−2.66 + 2.71 − 1.18 = −1.13 g) in soda consumed.
FIGURE 1.
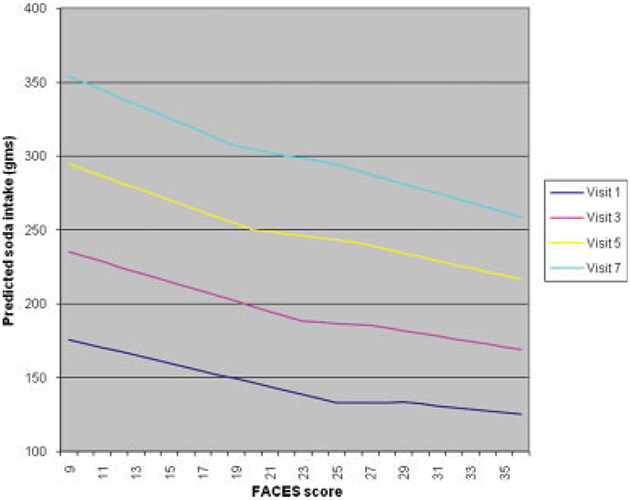
Model estimate of soda consumption by FACES score, by visit.
The association between FACES scores and milk consumption was in the expected direction, but the relationship failed to reach the .05 level of statistical significance (p = .08). In addition, the interaction between visit and FACES score suggested that the FACES effect increased at later visits, but this term was also just short of significance (p = .06). The spline terms were not individually significant (p > .05). The hypothesis that higher FACES scores would be associated with more fruit and vegetable servings was supported only at the trend level (p = .07); the interaction with visit was nonsignificant (p > .05).
Conclusion
This study examined the relationship between family cohesion and four eating behaviors that have been shown to contribute to health: frequency of breakfast, milk and fruit/vegetable consumption, and lower daily intake of soda. Previous studies have shown marked racial and age differences in these eating behaviors.32-35 In models that adjusted for the effects of race and age (using visit as a proxy for age) as well as adjusting for the potentially confounding influences of parental socioeconomic status, BMI, and study site, we found that girls who reported greater family cohesion, compared with girls who reported less family cohesion, had more days of eating breakfast; consumed less soda; and showed a trend toward greater consumption of fruits, vegetables, and milk consumption. Although the effect of family cohesion on these eating behaviors is not large (e.g., for a 1-point increase on the family cohesion measure, there was a decrease of 2.66 of soda consumed), the association is noteworthy because even after adjusting for a variety of demographic variables and BMI, family cohesion did exert some effect.
One explanation for these results is that breakfast may be the meal most likely to be eaten at home.36 Cohesive families may be more likely to have children who comply with parental communication about the importance of breakfast, or potentially, more cohesive families may be more likely to be together in the morning at meal time. A twin study indicated that family environmental factors predicted the likelihood of breakfast eating in a large sample of adolescents.37 In light of well documented decreases in breakfast consumption over the course of adolescence,38 our data suggest that a strong connection with family may enhance breakfast eating behavior.
Decreased soda consumption was also associated with levels of family cohesion. This may indicate that families high in cohesion have been successful at conveying the potential negative effects of soda intake39 and those girls from cohesive families may be more likely to act on that information. Girls who feel emotionally connected to their families may be more likely to listen to health messages from their parents. Alternatively, based on the inverse relationship between family cohesion scores and soda intake, it is possible that family cohesion serves as a proxy measure for time spent with family (vs. time spent with peers). Girls who are with their family more may feel a stronger connection, whereas lower family cohesion scores may mean that girls are spending more time with friends, during which time they may be more likely to be consuming soda than with family. Thus soda consumption may be more strongly related to the social context of snacking rather than to health beliefs or health information provided by the family. Bere et al.40 reported that modeling, both by parents and by peers, was one of the strongest determinants of soda consumption in a large study of Norwegian adolescents. Future studies will need to separate the influence of peers from family in order to better understand the role of each group in soda consumption. As soda consumption has been linked to obesity39,41 and dental caries,42 determining the relative influences on soda intake will be important in order to develop intervention studies.
It is somewhat puzzling that although soda consumption was associated with levels of cohesion, milk intake was not more strongly associated with family cohesion. Possible explanations for this include that milk consumption is a relatively low frequency event as girls grow older and therefore we did not have the power to detect the association34,43 but a clearer understanding of the relationship between milk drinking and familial variables, particularly in older children, awaits further research.
Similarly, fruit and vegetable consumption was not strongly associated with family cohesion, a finding that may be explained by the low intake of fruits and vegetables in this sample. Interestingly, Befort et al.44 recently reported that compared with restaurant use and eating while watching television, home availability had a relatively small impact on fruit, vegetable, and fat consumption for both black and white adolescents. On the other hand, Neumark-Sztainer et al.45 reported that the strongest correlates of fruit/vegetable intake were home availability of fruits/vegetables and taste preferences of fruits/vegetables and Zabinski et al.13 found that parental encouragement to eat fruits and vegetables was the only predictor of consumption. Still others have shown that in addition to home availability of fruits/vegetables and perceived parental modeling, perceived parent support and self-efficacy were significant predictors of fruit and vegetable consumption among middle school students.46 Thus it appears that no clear consensus has emerged on the relative influences of home/familial variables on fruit and vegetable consumption. Researchers need to learn more about the influences on fruit and vegetable intake in order to develop successful programs to promote greater consumption by adolescents.47,48
Recent work by Croll et al.49 found that family connectedness served as a protective factor against disordered eating in adolescents. A second study20 conducted in Spain sought to identify psychosocial and familial variables measured at ages 12–13 that would be predictive of eating disorders measured 2 years later. Participants with eating disorders reported more negative feelings toward the family, greater depression and body dissatisfaction, and lower self-esteem relative to those with no eating disorder. Time 1 predictors of the development of eating disorders at time 2 included only body dissatisfaction and feelings of being “ignored or not loved enough by mother.” These studies, in addition to our findings, raise the question of whether connection within a family is inversely related to disordered eating (e.g., binge eating, unhealthy weight loss methods) via its influence on healthy eating behaviors. Families that are higher in cohesion may encourage the adoption of healthy eating behaviors, which in turn may discourage the development of problematic eating behaviors. Studies are needed to characterize the exact path(s) by which such associations develop over time.
Overall, we found that a cohesive family environment was associated with two health behaviors, breakfast consumption and decreased soda intake, in black and white adolescent girls. Familial influences for milk consumption and fruit and vegetable intake require future research, but in our sample cohesion was not found to be as significant an influence. Limitations of our study include somewhat variable annual participation rates, so that data were not available for all girls through the entire study period. Self-reported food intake data are open to reporting biases and errors. Moreover, we did not have information about parental eating behaviors or attitudes toward healthy eating, which likely overlap with family cohesion. The site differences obtained suggest that there may be some regional variability in our findings and thus our results should be generalized with caution.
These weaknesses are off-set, however, by several strengths, including a high retention rate, a large and diverse sample, and the use of a three-day food intake record, which may lead to more reliable estimates of intake dietary intake than 24-h recalls or food frequency methodologies.50
Strengthening family cohesion may be a valuable goal toward increasing the overall health of adolescents and in particular, may be helpful in increasing breakfast eating and decreasing soda consumption. Understanding the role of familial factors in adolescent eating behaviors is an important research priority for the development of prevention programs and public health.
Acknowledgments
Supported by HL/DK71122 from National Heart, Lung, and Blood Institute (NHLBI) and by HC55023-26 and Cooperative Agreements U01-HL-48941-44
Footnotes
Earn CE credit for this article!
Visit: http://www.ce-credit.com for additional information. There may be a delay in the posting of the article, so continue to check back and look for the section on Eating Disorders. Additional information about the program is available at www.aedweb.org
References
- 1.Zeller M, Daniels S. The obesity epidemic: Family matters. J Pediatr 2004;145:3–4. [DOI] [PubMed] [Google Scholar]
- 2.Brown R, Ogden J. Children’s eating attitudes and behavior: A study of the modeling and control theories of parental influence. Health Educ Res 2004;19:261–271. [DOI] [PubMed] [Google Scholar]
- 3.Golan M, Crow S. Parents are key players in the prevention and treatment of weight-related problems. Nutr Rev 2004;62:39–50. [DOI] [PubMed] [Google Scholar]
- 4.Patrick H, Nicklas TA. A review of family and social determinants of children’s eating patterns and diet quality. J Am Coll Nutr 2001;24:83–92. [DOI] [PubMed] [Google Scholar]
- 5.Ritchie LD, Welk G, Styne D, Gerstein DE, Crawford PB. Family, environment and pediatric overweight: What is a parent to do? J Am Diet Assoc 2005;105(5, Suppl 1):S70–S90. [DOI] [PubMed] [Google Scholar]
- 6.Blanchette L, Brug J. Determinants of fruit and vegetable consumption among 6–12-year-old children and effective interventions to increase consumption. J Hum Nutr Diet 2005;18:431–443. [DOI] [PubMed] [Google Scholar]
- 7.Hanson NI, Neumark-Sztainer D, Eisenberg ME, Story M, Wall M. Associations between parental report of the home food environment and adolescent intakes of fruits, vegetables and dairy foods. Public Health Nutr 2005;8:77–85. [DOI] [PubMed] [Google Scholar]
- 8.Jenkins S, Horner SD. Barriers that influence eating behaviors in adolescents. J Pediatr Nurs 2005;20:258–267. [DOI] [PubMed] [Google Scholar]
- 9.Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics 1998;101:539–549. [PubMed] [Google Scholar]
- 10.Fisher JO, Mitchell DC, Smiciklas-Wright H, Birch LL. Parental influences on girls’ fruit and vegetable, micronutrient, and fat intakes. J Am Diet Assoc 2002;102:58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fisher JO, Mitchell DC, Smiciklas-Wright H, Mannino ML, Birch LL. Meeting calcium recommendations during middle childhood reflects mother-daughter beverage choice and predicts bone mineral status. Am J Clin Nutr 2004;79:698–706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Savage JS, Fisher JO, Birch LL. Parental influence on eating behavior: Conception to adolescence. J Law Med Ethics 2007;35:22–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zabinski MF, Daly T, Norman GJ, Rupp JW, Calfas KJ, Sallis JF, et al. Psychosocial correlates of fruit, vegetable, and dietary fat intake among adolescent boys and girls. J Am Diet Assoc 2006;106:814–821. [DOI] [PubMed] [Google Scholar]
- 14.Ackard DM, Neumark-Sztainer D, Story M, Perry C. Parent-child connectedness and behavioral and emotional health among adolescents. Am J Prev Med 2006;30:59–66. [DOI] [PubMed] [Google Scholar]
- 15.Lucia VC, Breslau N. Family cohesion and children’s behavior problems: A longitudinal investigation. Psychiatry Res 2006;141:141–149. [DOI] [PubMed] [Google Scholar]
- 16.Zdanowicz N, Janne P, Reynaert C. Family, health, and adolescence. Psychosomatics 2004;45:500–507. [DOI] [PubMed] [Google Scholar]
- 17.Ogden J, Steward J. The role of the mother-daughter relationship in explaining weight concern. Int J Eat Disord 2000;28:78–83. [DOI] [PubMed] [Google Scholar]
- 18.Byely L, Archibald AB, Graber J, Brooks-Gunn J. A prospective study of familial and social influences on girls’ body image and dieting. Int J Eat Disord 2000;28:155–164. [DOI] [PubMed] [Google Scholar]
- 19.Fonseca H, Ireland M, Resnick MD. Familial correlates of extreme weight control behaviors among adolescents. Int J Eat Disord 2004;32:441–448. [DOI] [PubMed] [Google Scholar]
- 20.Beato-Fernandez L, Rodriguez-Cano T, Belmonte-Llario A, Martinez-Delgado C. Risk factors for eating disorders in adolescents a Spanish community-based longitudinal study. Eur Child Adolesc Psychiatry 2004;13:287–294. [DOI] [PubMed] [Google Scholar]
- 21.Crossman A, Anne Sullivan D, Benin M. The family environment and American adolescents’ risk of obesity as young adults. Soc Sci Med 2006;63:2255–2267. [DOI] [PubMed] [Google Scholar]
- 22.Young EM, Fors SW. Factors related to the eating habits of students in grades 9–12. J Sch Health 2001;71:483–488. [DOI] [PubMed] [Google Scholar]
- 23.Fulkerson JA, Neumark-Sztainer D, Story M. Adolescent and parent views of family meals. J Am Diet Assoc 2006;106:526–532. [DOI] [PubMed] [Google Scholar]
- 24.Haerens L, Craeynest M, Deforche B, Maes L, Carbon G, De Bourdeaudhuij I. The contribution of psychosocial and home environmental factors in explaining eating behaviors in adolescents. Eur J Clin Nut 2008;62:51–59. [DOI] [PubMed] [Google Scholar]
- 25.Moore J, Harre N. Eating and activity: The importance of family and environment. Health Promot J Austr 2007;18:143–148. [DOI] [PubMed] [Google Scholar]
- 26.National Heart, Lung, and Blood Institute Growth and Health Study Research Group. Obesity and cardiovascular disease risk factors in black and white girls: The NHLBI Growth and Health Study. Am J Public Health 1992:82:1613–1620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thompson OM, Ballew C, Resnicow K, Gillespie C, Must A, Bandini LG, et al. Dietary patterns as a predictor of change in BMI z-score among girls. Int J Obes (London) 2006;30:176–182. [DOI] [PubMed] [Google Scholar]
- 28.Olson DH, Portner J, Lavee Y. FACES III. Family Social Science. St. Paul, MN: University of Minnesota, 1985. [Google Scholar]
- 29.Crawford PB, Obarzanek E, Morrison J, Sabry ZI. Comparative advantage of 3-day food records over 24-hour recall and 5-day food frequency validated by observation of 9- and 10-year-old girls. J Am Diet Assoc 1994;94:626–630. [DOI] [PubMed] [Google Scholar]
- 30.Schakel SF, Sievert YA, Buzzard IM. Sources of data for developing and maintaining a nutrient database. J Am Diet Assoc 1988;88:1268–1271. [PubMed] [Google Scholar]
- 31.U.S. Department of Agriculture. USDA food pyramid. US: Center for Nutrition Policy and Promotion, 2005. [Google Scholar]
- 32.Affenito SG, Thompson D, Barton BA, Franko DL, Daniels SR, Obarzanek E, et al. Breakfast consumption in African-American and white adolescent girls correlates positively with calcium and fiber intake and negatively with body mass index: The National Heart, Lung, and Blood Institute growth and health study. J Am Diet Assoc 2005;105:938–945. [DOI] [PubMed] [Google Scholar]
- 33.Striegel-Moore RH, Thompson DR, Affenito SG, Franko DL, Barton BA, Schreiber GB, et al. Fruit and vegetable intake: Few adolescent girls meet national guidelines: The National Heart, Lung, and Blood Institute (NHLBI) growth and health study. Prev Med 2006;42:223–228. [DOI] [PubMed] [Google Scholar]
- 34.Striegel-Moore RH, Thompson D, Affenito SG, Franko DL, Obarzanek E, Barton BA, et al. Correlates of beverage intake in adolescent girls: The National Heart, Lung, and Blood Institute growth and health study. J Pediatr 2006;148:183–187. [DOI] [PubMed] [Google Scholar]
- 35.Novotny R, Daida YG, Acharya S, Grove JS, Vogt TM. Dairy intake is associated with lower body fat and soda intake with greater weight in adolescent girls. J Nutr 2004;134:1905–1909. [DOI] [PubMed] [Google Scholar]
- 36.Nicklas TA, Baranowski T, Cullen KW, Berenson G. Eating patterns, dietary quality and obesity. J Am Coll Nutr 2001;20:599–608. [DOI] [PubMed] [Google Scholar]
- 37.Keski-Rahkonen A, Viken RJ, Kaprio J, Rissanen A, Rose RJ. Genetic and environmental factors in breakfast eating patterns. Behav Genet 2004;34:503–514. [DOI] [PubMed] [Google Scholar]
- 38.Miech RA, Kumanyika SK, Stettler N, Link BG, Phelan JC, Chang VW. Trends in the association of poverty with overweight among U.S. adolescents, 1971–2004. JAMA 2006;295:2385–2393. [DOI] [PubMed] [Google Scholar]
- 39.Ludwig DS, Ebbeling CB, Peterson KE, Gortmaker SL. Hard facts about soft drinks. Arch Pediatr Adolesc Med 2004;158:290. [DOI] [PubMed] [Google Scholar]
- 40.Bere E, Glomnes ES, Velde SJ, Klepp KI. Determinants of adolescents’ soft drink consumption. Public Health Nutr 2008;11:49–56. [DOI] [PubMed] [Google Scholar]
- 41.Giammattei J, Blix G, Marshak HH, Wollitzer AO, Pettitt DJ. Television watching and soft drink consumption: Associations with obesity in 11-to 13-year-old schoolchildren. Arch Pediatr Adolesc Med 2003;158:882–886. [DOI] [PubMed] [Google Scholar]
- 42.Mobley CC. Nutrition and dental caries. Dent Clin North Am 2003;47:319–336. [DOI] [PubMed] [Google Scholar]
- 43.Demory-Luce D, Morales M, Nicklas T, Baranowski T, Zakeri I, Berenson G. Changes in food group consumption patterns from childhood to young adulthood: The Bogalusa Heart Study. J Am Diet Assoc 2004;104:1684–1691. [DOI] [PubMed] [Google Scholar]
- 44.Befort C, Kaur H, Nollen N, Sullivan NK, Nazir N, Choi WS, et al. Fruit, vegetable, and fat intake among non-Hispanic black and non-Hispanic white adolescents: Associations with home availability and food consumption settings. J Am Diet Assoc 2006;106:367–373. [DOI] [PubMed] [Google Scholar]
- 45.Neumark-Sztainer D, Wall M, Perry C, Story M. Correlates of fruit and vegetable intake among adolescents. Findings from Project EAT. Prev Med 2003;37:198–208. [DOI] [PubMed] [Google Scholar]
- 46.Young EM, Fors SW, Hayes DM. Associations between perceived parent behaviors and middle school student fruit and vegetable consumption. J Nutr Educ Behav 2004;36:2–8. [DOI] [PubMed] [Google Scholar]
- 47.Baranowski T, Baranowski J, Cullen KW, Marsh T, Islam N, Zakeri I, et al. Squire’s quest: Dietary outcome evaluation of a multimedia game. Am J Prev Med 2003;24:52–61. [DOI] [PubMed] [Google Scholar]
- 48.Nicklas TA, O’Neil CE. Process of conducting a 5 a day intervention with high school students: Gimme 5 (Louisiana). Health Educ Behav 2000;27:201–212. [DOI] [PubMed] [Google Scholar]
- 49.Croll J, Neumark-Sztainer D, Story M, Ireland M. Prevalence and risk and protective factors related to disordered eating behaviors among adolescents: Relationship to gender and ethnicity. J Adolesc Health 2002;31:166–175. [DOI] [PubMed] [Google Scholar]
- 50.Institute of Medicine. Dietary reference intakes: Applications for dietary assessment. Washington, DC: National Academy Press, 2001. [Google Scholar]


