Abstract
Cortical desmoid is an uncommon benign bony lesion that can typically be diagnosed through conventional radiographic methods. However, here we present an atypical case of a 14-year-old male who presented with a history of trauma, and the initial X-ray showed a right femur suspicious bony lesion. Still, the subsequent use of CT and MRI confirmed the diagnosis of cortical desmoid, so conservative management and follow-up imaging was recommended. This case highlights the importance of proper identification of this entity can prevent unnecessary biopsy and surgical intervention.
Keywords: Cortical desmoid, Bone tumors, “Do not touch” lesions, Femoral cortical irregularity, Fibrous cortical defect
Introduction
Cortical desmoids are benign, self-limiting conditions often accidentally discovered on various radiological examinations, e.g., conventional radiography, CT scan, and MRI. Different terms can be used to describe this condition, such as cortical avulsive injuries, Bufkin lesions, periosteal desmoids, or distal femoral cortical irregularities. Regarded as a ``do not touch'' lesion, it's crucial not to mistake them for an aggressive cortical or periosteal pathology, such as osteosarcoma [1].
Although this lesion is termed a ``cortical desmoid,'' it does not accurately reflect the histological nature of true desmoid tumors. These lesions are also known in the literature as distal femoral cortical irregularities [1]. Histologically, they resemble fibrous cortical defects or non-ossifying fibromas [2]. Given their benign, often asymptomatic, and self-limiting nature, invasive diagnostic methods like biopsies are generally discouraged. Nonetheless, MRI follow-up may be recommended in rare instances where symptoms are present [2].
Case presentation
A 14-year-old male visited the emergency department after experiencing painful right knee trauma and difficulty flexing his knee following a stairway fall at school. Examination revealed tenderness in the right knee, worsening upon stressing the knee. The patient has no significant medical history or previous surgical intervention history. Initial X-rays did not show any fractures but did raise suspicion of potential neoplastic processes due to observed distal medial femoral diaphyseal cortical irregularities (Fig. 1). Further evaluations using CT scan and enhanced MRI were performed, revealing an irregular cortical sclerotic lining on the distal third of the femur's posteromedial aspect, particularly where the medial gastrocnemius muscle and adductor magnus tendon attach (Fig. 2, Fig. 3). MRI identified slight edema in the cortical irregularity zone and tendon attachment points, with minimal contrast enhancement seen in these areas (Fig. 4, Fig. 5). The final diagnosis of medial distal femoral metaphyseal cortical desmoid was based on imaging findings. Conservative management and imaging follow-up were recommended. The patient has 2 visits in the hospital records, one for shoulder pain after trauma and the other for upper respiratory tract infection; no complaints regarding the previously diagnosed right femur cortical desmoid.
Fig. 1.
Right knee x-ray (A) AP (Frontal) view, (B) lateral view. The X-ray displays a poorly defined radiolucent zone on the distal femur's medial metaphysis with a thickened cortical lining of the medial femoral condyle (white arrow), with no adjacent soft tissue mass or aggressive periosteal response, indicating a benign condition.
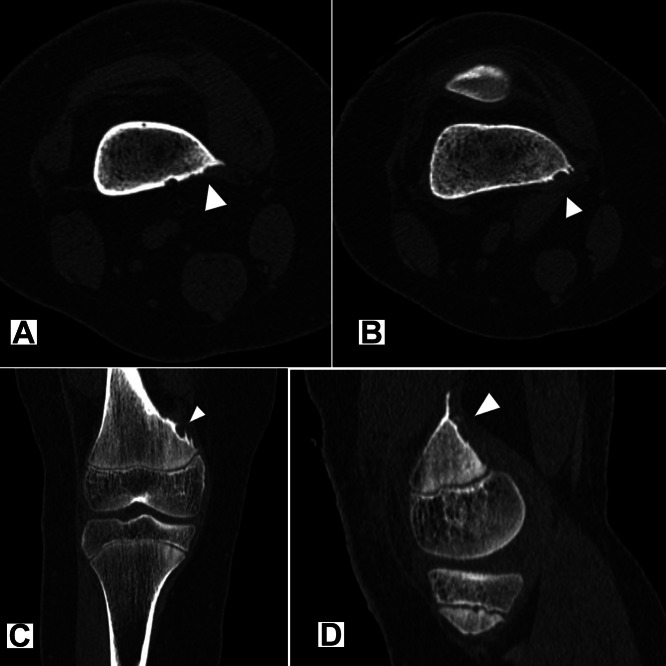
Fig. 2.
Computed tomography (CT) scan with axial cuts (A and B), coronal (C), and sagittal (D) reconstructions in bone window through different levels of the cortical lesion. CT images reveal a conspicuously irregular sclerotic cortical layer near the medial femur condyle (arrowhead), specifically at the gastrocnemius muscle (medial head) and adductor magnus tendon attachment sites. No soft tissue mass or aggressive periosteal reaction indicates a benign condition.
Fig. 3.
3D reconstructions of the CT images (A) anterior and (B) lateral. 3D reconstructions of the CT images showing the irregular posteromedial supracondylar cortex.
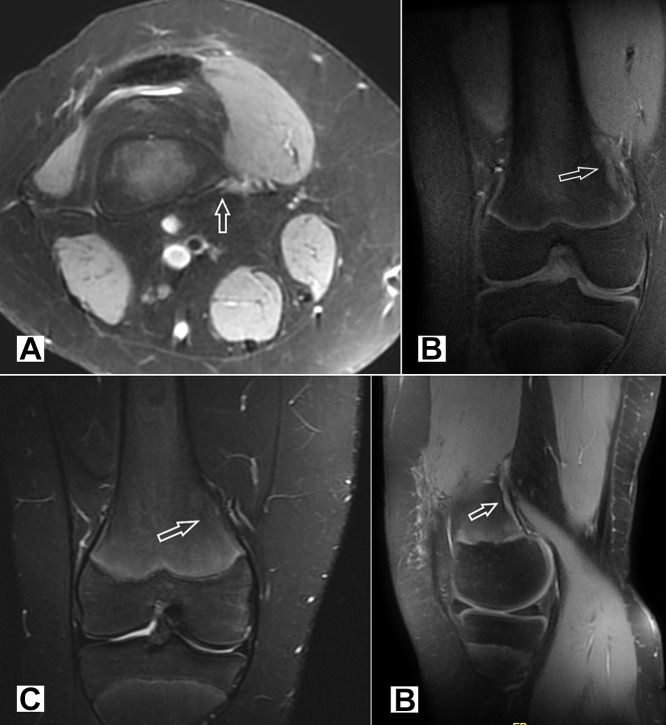
Fig. 4.
RT knee Magnetic resonance imaging (MRI) scan with (A) PD axial, (B) coronal T1 Fat Sat, (C) coronal STIR, (D) sagittal PD. A slight edema is seen in the cortical irregularity area and, to a lesser extent, at the attachment sites of the gastrocnemius muscle (medial head) and adductor magnus' tendon (arrow). There is no sign of underlying bone marrow edema, lesions, or adjacent soft tissue mass.
Fig. 5.
Post-contrast magnetic resonance imaging (MRI) scan (A) axial T1 Fat Sat, (B) coronal T1 Fat Sat, and (C) sagittal T1 Fat Sat. Minimal contrast enhancement was observed at the gastrocnemius (medial head) and adductor magnus tendon attachment sites (arrow).
Discussion
Clinical perspective
Cortical desmoid cases are usually detected incidentally, with a few instances that may present with localized pain or discomfort. In scarce situations, the lesion exhibits unusual characteristics or suspicious periosteal reactions on X-ray, prompting further review with CT or MRI to exclude malignant and infectious possibilities [3,4].
Patients typically don't show symptoms and are often discovered incidentally. Pain can occur occasionally. These lesions are mainly found in adolescents with males affected more than females [1,3].
Cortical desmoids usually appear on the posteromedial aspect of the distal femur and may be bilateral in approximately 33% of cases [1,3]. The repetitive stress on the attachment sites of the gastrocnemius' medial head, or less frequently, the gastrocnemius' lateral head or adductor magnus, is thought to contribute to their pathophysiology [[1], [2], [3]].
In rare cases, similar lesions have been reported on the humerus, either medially at the insertion of the pectoralis major or laterally at the insertion of the deltoid muscle [3].
These lesions are benign, and the diagnosis should consider the imaging findings interpreted with the patient's clinical context to prevent unnecessary diagnostic and therapeutic measures [4].
Imaging
Using conventional radiography, an oblique femur view with external rotation optimally shows the lesion [4]. Cortical desmoids look like small, radiolucent, saucer-like lesions or show cortically rough areas (Fig 1A) in their usual location on the posteromedial cortex of the medial femoral condyle [1,3]. These lesions often feature cortical erosion or irregularity atop a sclerotic base. When classic symptoms and radiographic signs align with a benign clinical course of the patient, the diagnosis is straightforward, so further work-ups or biopsies can be avoided. In cases where radiographic results aren't clear or when lesions appear atypical, CT scans can offer a more accurate assessment by identifying lytic areas or cortical thickening (Fig. 2) and any slight fragmentation [5]. CT scan is useful in ruling out more aggressive neoplastic conditions [3,5].
MRI can identify cortically-based lesions not visible on X-rays, displaying low to intermediate T1-weighted imaging signal intensity and intermediate to high T2-weighted signal intensity. A rim of low signal intensity on T2-weighted images, presumably indicating sclerosis, is commonly observed in addition to post-contrast enhancement of the fibrous lesion (Fig 4 & 5) [2,6]. MRI is also instrumental in pinpointing the lesion's exact location at the tendon attachment sites and ruling out associated soft-tissue masses [1,3,6].
On 99mTc methylene diphosphonate (99 mTc MDP) bone scintigraphy, the appearance of cortical desmoid varies with the lesion's maturity phase. Lesions in active or healing stages may show normal or slightly increased uptake in delayed-phase images due to chronic stress, whereas inactive lesions typically exhibit no uptake [1,4].
FDG-PET scans can detect mild to intense 18F-FDG uptake even in cases where MDP bone scans yield negative results. This intense uptake could be mistakenly attributed to bone metastasis in children with concurrent malignancies, making it essential to correlate these findings with CT or MRI results to confirm the lesion's benign nature [4].
When considering imaging differential diagnoses, options include:
-
-
Medial distal femoral metaphyseal cortical desmoid.
-
-
Fibrous cortical defect (FCD).
-
-
Non-ossifying fibroma (NOF).
-
-
Osteosarcoma.
-
-
Ewing Sarcoma.
Conclusion
Cortical desmoids are classic benign, self-limiting ``do not touch'' lesions; it is crucial not to mistake these for more aggressive cortical or periosteal conditions like osteosarcoma. Recognizing these lesions as benign can eliminate the need for unnecessary invasive diagnostic and therapeutic procedures, as shown in this case study. MRI and CT scans should be reserved for situations with suspicion of malignancy, atypical conventional radiography, or when it is necessary to confirm the benign nature of the lesion for the peace of mind of both patients and healthcare providers.
Declaration of generative AI and AI-assisted technologies in the writing process
During the preparation of this work, the authors used Grammarly software to check grammar, spelling, and punctuation and to improve readability and language. After using this tool, the authors reviewed and edited the content as needed and took full responsibility for the publication's content.
Author contributions
Khalid Ibrahim: Writing and reviewing the paper draft, interpreting and reporting the imaging studies.
Osama Elhag: Writing and reviewing the paper draft, interpreting the imaging studies.
Reem AlKtebi: Reviewing the paper draft, interpreting the imaging studies.
Amna AlKtebi: Reviewing the paper draft, interpreting the imaging studies.
Loai Ali: Reviewing the paper draft, interpreting the imaging studies.
Ethical statement
None.
Ethical approval
None.
Data sharing statement
Data described in this study will be publicly available post-publication.
Patient consent
This is to declare that a written consent was obtained from the patient's guardian for this case report.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments: No sponsor.
References
- 1.Dang D, Hacking C, Campos A, et al. Cortical desmoid. Reference article, Radiopaedia.org (Accessed August 7, 2024). doi: 10.53347/rID-5198 (RID: 5198).
- 2.Stern Christoph, Galley Julien, Fröhlich Stefan, Peterhans Loris, Spörri Jörg, Sutter Reto. Distal femoral cortical irregularity at knee MRI: increased prevalence in youth competitive alpine skiers. Radiology. 2020;296:411–419. doi: 10.1148/radiol.2020192589. [DOI] [PubMed] [Google Scholar]
- 3.Gould CF, Ly JQ, Lattin GE, Beall DP, Sutcliffe JB. Bone tumor mimics: avoiding misdiagnosis. Curr Probl Diagn Radiol. 2007;36:124–141. doi: 10.1067/j.cpradiol.2007.01.001. https://pubmed.ncbi.nlm.nih.gov/17484955/ [DOI] [PubMed] [Google Scholar]
- 4.Kontogeorgakos VA, Xenakis T, Papachristou D, Korompilias A, Kanellopoulos A, Beris A, et al. Cortical desmoid and the four clinical scenarios. Arch Orthop Trauma Surg. 2009;129:779–785. doi: 10.1007/s00402-008-0687-6. https://pubmed.ncbi.nlm.nih.gov/18612646/ [DOI] [PubMed] [Google Scholar]
- 5.Pennes DR, Braunstein EM, Glazer GM. Computed tomography of cortical desmoid. Skeletal Radiol. 1984;12:40–42. doi: 10.1007/BF00373175. https://pubmed.ncbi.nlm.nih.gov/6474218/ [DOI] [PubMed] [Google Scholar]
- 6.Gould Frank, Ly Justin Q., Lattin Grant E., Jr, Beall Douglas P., Sutcliffe Joseph B., III Bone tumor mimics: avoiding misdiagnosis. Curr Prob Diagn Radiol. 2007;36(3):97–142. doi: 10.1067/j.cpradiol.2007.01.001. [DOI] [PubMed] [Google Scholar]