Abstract
Sacrococcygeal teratoma (SCT) is a rare congenital tumor typically diagnosed in neonates, with management challenges arising from the size of the tumor and associated delivery complications. In this case, a 32-year-old gravida 5 para 5 woman with a history of three prior cesarean sections was diagnosed with a giant type I SCT at 30 weeks of gestation through prenatal ultrasound, confirmed by fetal MRI. At 34 weeks, an emergency cesarean section was performed due to acute fetal distress, resulting in a newborn with transient respiratory distress. Postnatal imaging classified the tumor as type I SCT, and it was successfully excised on the third day of life without complications. The patient recovered well and was discharged on day fifteen. This case highlights the importance of early prenatal diagnosis, surgical intervention, and multidisciplinary care in managing large SCTs.
Keywords: Teratoma, Sacrococcygeal, Foetus
Introduction
Sacrococcygeal teratoma (SCT) is the most common tumor in neonates, with an incidence of 1 in 20,000 to 40,000 live births. Prenatal diagnosis should systematically include an MRI. Typically, outcomes following surgery are favorable, especially when cases are identified and treated early, with recurrence rates after surgery estimated at 10-15% [1]. However, managing large tumors, as in our case, presents significant challenges. There is a high risk of rupture, particularly during delivery and neonatal care. Surgical management in such cases is complex, requiring intricate procedures to achieve successful tumor resection [2]. Here, we present our experience with a giant sacrococcygeal teratoma in a newborn girl, diagnosed prenatally using fetal MRI. This report follows the SCARE guidelines [3].
Presentation of case
A 32-year-old multiparous woman (gravida 5, para 5) with a history of three cesarean sections and one vaginal delivery presented at 30 weeks of gestation with polyhydramnios. Her pregnancy was unplanned, poorly monitored, and complicated by undiagnosed gestational diabetes. Ultrasound revealed a type I sacrococcygeal teratoma without fetal anemia or hydrops (Fig. 1). Fetal MRI was performed to assess intra-abdominal extension (Fig. 2). A multidisciplinary team decided on a cesarean delivery at 37 weeks. However, emergency cesarean delivery was required at 36 weeks due to acute fetal distress. The newborn experienced transient respiratory distress, which resolved within two hours. After stabilization, the infant was transferred to pediatric surgery. Physical examination revealed a sizeable sacrococcygeal tumor measuring approximately 35 × 40 × 20 cm with a lobulated surface and variable consistency. Abdominal ultrasound and CT imaging confirmed a solid-cystic mass with minimal intrapelvic extension (1 cm) and no involvement of critical structures such as the rectum, bladder, spinal cord, or significant vessels. The tumor was classified as type I SCT according to the AAPSS classification. Laboratory results were within normal limits, except for a slightly elevated alpha-fetoprotein. On the third day of life, the tumor was excised, including the coccyx, with careful attention to avoid rupture. The infant recovered well and was discharged on day fifteen postoperatively Fig. 3, Fig. 4.
Fig. 1.
An ultrasound scan of a 30-week fetus showing a huge solid echogenic buttock mass with internal cystic changes (white arrow).
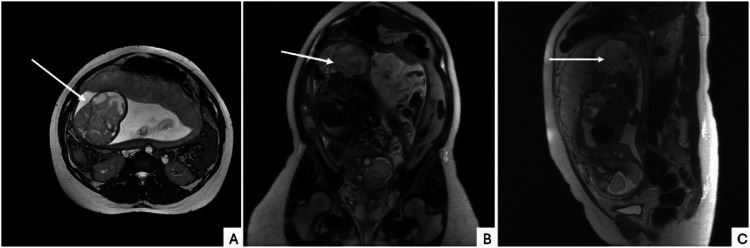
Fig. 2.
(A) Axial FIESTA (B) CORONAL T2 weighted (C) SAGITAL T2 weighted magnetic resonance images show a heterogenous solid mass in the sacrococcygeal region with cystic components. The mass mainly develops outside the fetus and has a small pre-sacral component. No intraspinal extension or ureteric dilatation are noted.
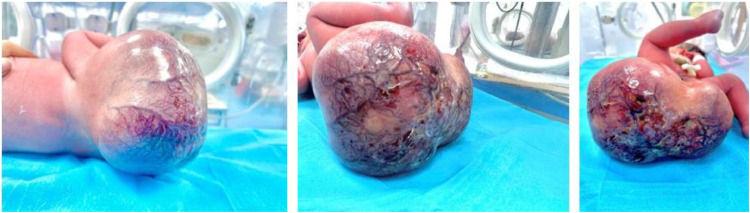
Fig. 3.
Photos showing a substantial sacrococcygeal teratoma in a newborn female immediately postnatally and preoperatively with signs of pre-rupture. The mass is hypervascularized with signs of fistulization.
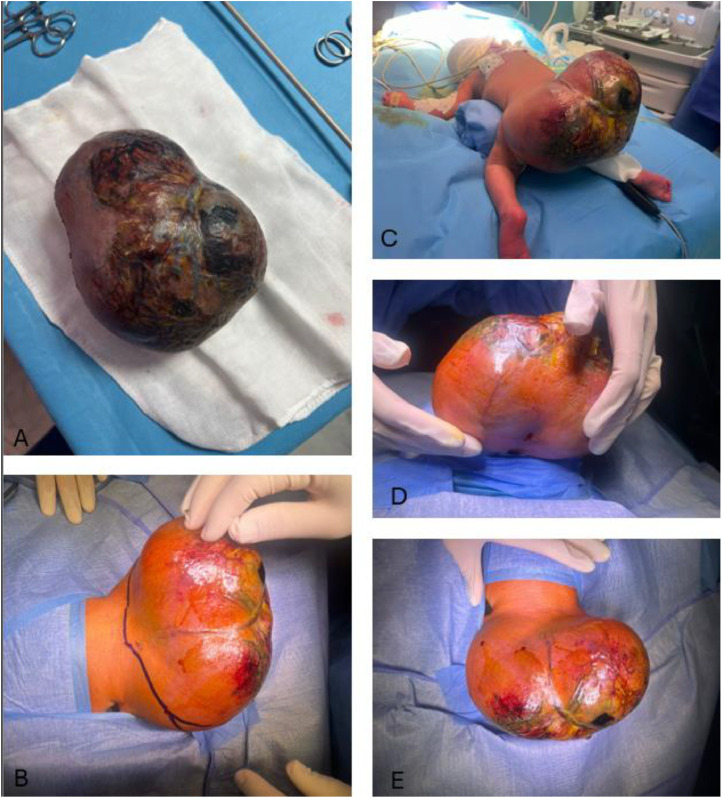
Fig. 4.
(A) Teratoma after excision. (B) Delimitation of the incision line. (C) Positioning of the newborn. (D) Caudal view of the teratoma. (E) Frontal view of the teratoma.
Discussion
SCT, predominantly affecting female neonates, is an extragonadal germ cell tumor (GCT) that arises during fetal and neonatal stages. Diagnosing SCT during pregnancy is challenging and can lead to obstetrical complications [2,4]. Management requires a multidisciplinary team involving obstetricians, radiologists, and pediatric surgeons. While fetal interventions such as devascularization and debulking are being explored for high-risk cases, they remain experimental [4]. Postnatal surgical excision is the primary treatment, and complete resection is crucial to prevent recurrence, which occurs in 10%-15% of cases, particularly with incomplete resection or malignant histology [1,4]. Long-term follow-up with alpha-fetoprotein monitoring and regular imaging is essential for early detection of recurrence, metastasis, or malignancy [4]. Survivors may experience late complications, underscoring the importance of comprehensive follow-up care.
Conclusion
This case highlights the utility of prenatal MRI in diagnosing type I SCT and guiding neonatal management and surgical planning. Managing SCT requires a multidisciplinary approach, from prenatal diagnosis to surgical intervention and long-term follow-up. Further research into fetal interventions and surgical techniques is crucial for improving outcomes and patient quality of life.
Ethical approval
The local Ethical Committee of Maternity and Neonatology Center of Tunis, Tunis, Tunisia, approved this study on 11 May 2024 (Approval Number: 45/2024).
Patient consent
Written informed consent was obtained from the patient's parents/legal guardians for publication and accompanying images. The editor-in-chief of this journal can review a copy of the written consent upon request.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Phi JH. Sacrococcygeal teratoma: a tumor at the center of embryogenesis. J Korean Neurosurg Soc. 2021;64(3):406–413. doi: 10.3340/jkns.2021.0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shrestha HK, Shrestha RG. Sacrococcygeal teratoma: a case report. JNMA J Nepal Med Assoc. 2020;58(227):508–511. doi: 10.31729/jnma.5230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sohrabi C, Mathew G, Maria N, Kerwan A, Franchi T, Agha RA. The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kornete A, Bokucava D, Vedmedovska N. Fetal sacrococcygeal teratoma: a case report of a giant tumor withan excellent outcome. Acta Med Litu. 2023;30(2):206–215. doi: 10.15388/Amed.2023.30.2.13. [DOI] [PMC free article] [PubMed] [Google Scholar]